Abstract
Subjective cognitive complaints (SCC) is a self-reported experience of persistently impaired cognitive functions which could be the earliest red flag of neurocognitive disorders. The COVID-19 pandemic and related restriction measures changed the lifestyle and behaviour of older adults. The aim of this study was to assess the relation of these changes and SCC status in Hungary. This cross-sectional study analysed the data of 359 elderly Hungarians who filled out the WW-FINGERS-SARS-CoV2 survey. A quarter of the respondents (n:88) reported SCC in connection with the pandemic. We compared sociodemographic features, health status, lifestyle, and social life parameters between subjects with reported SCC and without. To eliminate the potential interrelation across group differences, stepwise logistic regression was applied. Participants with SCC showed the following characteristics, compared to individuals without: (1) they were older; (2) they were more likely to be women; (3) they had a higher number of chronic disorders; (4) showed more prominent impairment in physical mobility; (5) had worse sleep quality; (6) spent less time with family; and (7) used internet more frequently during the pandemic (all p’s < 0.001). Logistic regression highlighted that only two parameters were related to SCC status independently, the physical mobility (ability to walk 500 m without difficulties; OR = 1.186; p < 0.001; 95%CI = 1.101, 1.270) and changes in time spent with grandchildren (OR = 1.04; p = 0.015; 95%CI = 1.008, 1.073). Our study draws attention to the importance of physical mobility and quality time with family as key factors in the cognitive well-being of elderly people.
Similar content being viewed by others
Introduction
With an aging population cognitive impairment due to major neurocognitive disorders such as Alzheimer’s disease (AD) is a growing public health concern. According to the estimations, over 55 million people are living with AD and other dementias worldwide, and this number is expected to reach 139 million by 20501. Dementia is characterized by cognitive and functional impairment that leads to loss of daily functioning and independence2. It is often preceded by mild cognitive impairment (MCI), which is an early stage of cognitive decline in individuals who maintain the ability to independently perform most activities of daily living. This condition is also characterised by objective cognitive deterioration3.
Subjective cognitive complaints (SCC) represent a self-reported experience of persistently impaired cognitive functions (e.g., memory, visuo-spatial skills, language functions). The condition is an integral component of the diagnostic criteria of MCI4 and also a key hallmark of subjective cognitive decline (SCD), where individuals show a normal performance on standardised cognitive tests5. The utility of SCC in the prediction of cognitive decline shows ambiguous results in a short-interval period due to (1) the possible overreporting of SCC in individuals with higher level of anxiety or mood problems6, or (2) the anosognosia/reduced awareness of their cognitive symptoms in patients with neurocognitive disorders7. However, a large meta-analysis of 28 studies8 demonstrated that SCC was associated with a relative risk of 2.07 for the development of dementia after 4 years follow-up. Furthermore, a hallmark longitudinal autopsy study confirmed the long-term predictive value of SCC showing that subjective complaints precede the diagnosis of MCI by over 9-years9. These findings have been confirmed by further studies, particularly in SCC population with chronic cardiovascular disease10.
In March 2020, the World Health Organization declared COVID-19 a pandemic11. In many countries around the world severe restrictions have been introduced during peaks of infection. To slow down the spread of infections, countries introduced general mobility restrictions, limitation of social gathering and strict infection control measures in the healthcare system12. In addition to the negative health consequences of COVID-19 infection, the introduction of strict quarantine and lockdown measures has disrupted social networks and damaged the global economy. As a result, there is growing concern that the pandemic has been affecting the mental health and the quality of life of the population13. One of the most vulnerable groups in the COVID-19 pandemic is the population over 60 years of age, as they had the highest morbidity and mortality. They often must deal with significant health and economic challenges by themselves as persons living with chronic diseases and being both isolated and with limited access or ability to use digital technology14.
In Hungary, the third wave of the COVID-19 pandemic began from February 2021. An increasingly significant number of illnesses were caused by mutations that spread faster than before, especially the so-called British (alpha) virus variant. The symptoms were more severe, and the daily number of new deaths linked to the coronavirus has gradually increased from below 100 in the second half of January 2021; by the end of March, it repeatedly exceeded 300 cases a day. In Hungary, the total number of deaths linked to the coronavirus increased from ten thousand to thirty thousand during the third wave, and the total number of people infected with the COVID-19 virus also doubled during this period. Radical restrictions were also introduced in Hungary: in addition to the closure of kindergartens and primary schools, non-essential shops and services were suspended, and the use of masks was required in public areas. The health sector also mainly focused on the treatment of cases related to the coronavirus and those that cannot be postponed. Mass vaccinations against COVID-19 also took place during this period; for the first time, at the end of December 2020. Healthcare workers were the first to be vaccinated, and later the oldest residents and patients with certain chronic diseases. From April 2021, in accordance with the increase in the number of vaccinated people, the restrictions were gradually eased; by the beginning of June 2021—after the number of daily new cases and deaths had significantly decreased—the end of the third wave was announced. Taking into account the previous description, the Hungarian population of older adults was also socially isolated during the pandemic, which had a significant negative impact on their lifestyle and health15.
In the current cross-sectional study, we aimed to analyse the social and the lifestyle changes during the third wave of the pandemic in an elderly population. Our special aim was to characterize the most relevant predisposing factors for SCC in relation of the COVID-19 pandemic and following life-style changes.
Methods
Participants and data acquisition
The study was conducted within the framework of the World-Wide (WW)-FINGERS network of multidomain clinical trials for dementia risk reduction (led by Prof. Miia Kivipelto, Karolinska Institute, Sweden)16. Within the network, the WW-FINGERS-SARS-CoV-2 initiative was launched in response to the COVID-19 pandemic, under the aegis of the World Health Organization (WHO) Neurology and COVID-19 Global Forum, to assess direct and indirect effects of the pandemic in midlife and older age17,18. The survey focused on changes in lifestyle factors, management of chronic noncommunicable diseases, as well as psychosocial factors, all of which are relevant to cognition and are expected to be affected by the pandemic. Local results in some countries are already available18,19,20.
In Hungary, the study was led by the consortium of the National Institute of Mental Health, Neurology and Neurosurgery and by the Department of Psychiatry and Psychotherapy, Semmelweis University. We collected data using the Hungarian translation of the „World-Wide Fingers SARS-CoV-2 Survey” (Hungarian WW-Fingers SARS CoV2 Survey) between 1st of February and 1st of June 2021, covering the third wave of the COVID-19 pandemic in Hungary (Budapest and neighbouring suburban area). Inclusion criteria were the followings: (1) age 60 + years; (2) living in Hungary; (3) being fluent in Hungarian language; (4) the absence of previous diagnosis of major neurocognitive disorders based on the available medical records. Participation was on a voluntary base and included patients from GP practices, residents of nursing homes, and residents from inpatient institutions. The above categories included healthy elderly participants and patients with various types of chronic diseases. For obtaining the data, a paper-based, self-administered questionnaire was used. Data were recorded in uniform format defined by the WW-FINGERS Network, the standardized modules allow later international comparisons. The Research Ethics Committee of the National Institute of Mental Health, Neurology and Neurosurgery authorized our ethical protocol (reference number: IKEB 17/2020). All respondents agreed to participate in the survey with their informed written consent. All methods were carried out in accordance with relevant guidelines and regulations.
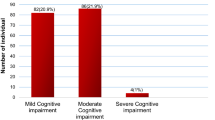
In total 431 participants answered the Hungarian WW-Fingers SARS CoV2 survey. The vast majority of respondents were patients in GP practices. A small number of respondents, only 7%, (30/431) lived in a nursing homes. Since we did not aim to analyze the direct impact of COVID-19 infection, we excluded persons self-reported previous COVID-19 virus infection (n = 26). We also excluded participants having possible cognitive impairment at the time of data acquisition [existing diagnosis of minor neurocognitive disorders (n = 8) and subjects who preferred not to disclose their pandemic cognitive status (n = 4)]. Those participants who reported better subjective memory performance since the start of COVID-19 pandemic (n = 4) or subjects preferred not to report their subjective memory changes (n = 30) were also excluded.
For statistical analysis the answers of 359 participants (age: 73.6 ± 7.9, 223 females) were processed. Those 271 (75.5%) participants who had intact cognitive performance before the pandemic and did not experience any change in their cognitive functions were included in the SCC− group. The remaining 88 (24.5%) who had normal cognitive performance preceding the pandemic but reported worsening cognitive performance (affecting mostly the memory functions) since the outbreak were selected in the SCC+ cohort. In SCC+ group 45 participants worried about the memory worsening. Figure 1 displays the flowchart of the participant selection for the SCC prediction.
Survey
The questionnaire was built up by 46 questions, focusing on six main domains, which are presented in more detail in Table 1.
Data extraction and statistical analysis
From 4 question groups, 5–5 parameters were selected that were consistent with the previously reported cognitive risk parameters21,22,23,24. As a major selection criterion, only statistically independent parameters were included for further analysis, where the risk that one variable directs the changes of the others is enough low. Independence was checked with a correlation matrix where r was set as < 0.35 in significant correlations (p < 0.05) or p was not significant (p > 0.05) (Table S1 in Supplementary Material). The thresholds are defined based on traditional medical statistical opinions25. From the sociodemographic category age (in years), sex (possible answers- 1: female, 2: male, 3: prefer not to say), educational attainment (in years), family status (possible answers- 1: single, 2: married, 3: living with partner, 4: in relationship, living separately, 5: divorced, 6: widowed, 7: prefer not to say) and employment status (possible answers:- 1: employed, 2: temporally unemployed due to pandemic, 3: unemployed, 4: pensioner, 5: working as a pensioner, 6: prefer not to say) were selected. From information regarding lifestyle, medical conditions and biometric data, pre-pandemic smoking status (scale- 1: no, 2: sometimes 3: daily), pre-pandemic alcohol consumption (scale- 1: 1–2 international unit (IU), 2: 3–4 IU, 3: 5–6 IU, 4: 7–9 IU, 5: > 10 IU/day), pre-pandemic body mass index (BMI), current number of chronic disorders and physical independence measured as the capability of independent walking of 500 m (possible answers- 1: easily able, 2: able but with difficulties, 3: barely able, 4: not able) were selected. From the lifestyle changes, the followings were selected measured with a 5-point scale (1: significantly decreased, 2: decreased, 3: same, 4: increased, 5: significantly increased): time spent with family, time spent doing physical activity, presence of sleep problems, time spent on remote working, time spent with internet use. From the social engagement response pool, the followings were selected measured on a 7-point scale (1: daily, 2: few times per week, 3: once per week, 4: few times per month, 5: once per month, 6: less than once per month, 7: never): time for grandchildren, time for voluntary work, time for educational activity, time for sport and social clubs, time for patient organizations. Pre- and post-pandemic responses were compared, and changes were highlighted on a scale ranging from − 6 (maximum increase) to + 6 (maximum decrease).
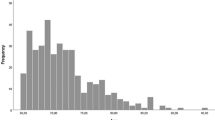
Distribution of the numeric variables was analysed with Kolmogorov–Smirnov test. Continuous variables were analysed with independent samples t-test or Mann–Whitney U-test as appropriate. Categoric variables were compared with Chi-squared tests. The frequency of missing responses was analysed in all questions and its difference across the two study groups was compared with Chi-square tests. Statistical significance (p < 0.05) was considered only in variables without significant differences in the distribution of missing responses. Since in independent component multivariate analysis, finding the most influential driver factors are critical, we applied the stepwise logistic regression to find potential predictive models for subjective memory complaints with the inclusion of the 20 analysed variables (predictor variables)26,27. Where participants preferred not to say, responses were considered as missing variables. The response variable was set as the grouping variable (SCC). Predictor variables were continuous variables (age, educational attainment, BMI), categoric variables (sex) or directly generated as categorical variables from scale-based answers. Significance of p was set at < 0.05. Results of logistic regression were reported with significance levels, odds ratios (ORs) and 95% confidence intervals (CIs).
Results
Sociodemographic factors
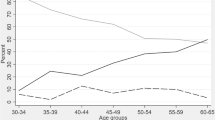
The SCC+ cohort was significantly older than the SCC− (MD = 3.6 years; p < 0.001) and there were more women in the SCC+ group (Chi = 21.1; p < 0.001). The missing response rate was not statistically different in the above mentioned two parameters. The average educational years in the SCC+ cohort was higher than in the SCC− but the difference was non-significant. The “married” marital status was the most common in both measured groups, but there were more married participants in the SCC− than in the SCC+ group (54.2% vs. 44.6%). Parallel to this, the divorced (10.8% vs. 7.2%) and the widowed (30.1% vs. 25.4%) subjects were overrepresented in the SCC+ population. Pensioner was the most common work status in the population (72.1% in SCC− and 72.6% in SCC+ groups), while 15.5% of the subjects in the SCC− and 18.6% in the SCC+ group were working after retirement. Only 8% of the whole study population was actively working. Statistical results of between group comparisons are presented in Table 2.
Pre-pandemic physical condition
While the majority of the participants were non-smoker (88.6% in the SCC− and 85.1% in the SCC+ group), daily smoking was higher in the SCC+ population (12.6% vs. 8.9%). Most of the responders were mild drinkers consuming 1–2 international units/day (80.4% in the SCC− and 86.21% in the SCC+ group). Moderate alcohol consumption (3–4 IU/day) was more common in the SCC− group (16.9% vs. 6.9%). People in both groups were characterized by mild overweight with an average BMI of 26.6 in the SCC− and 27.4 in the SCC+ group. Chronic disorders were frequently reported: only 16.7% of the SCC− and 6.9% of the SCC+ patients indicated the absence of any chronic condition. Fifty-eight percent of SCC− subjects had at least 2 chronic disorders and it was even more frequent in the SCC+ group (76.4%). Based on these data, the measured population was characterized by polymorbid chronic medical conditions; however, the number of concomitant disorders was significantly higher in the SCC+ population (U = 8354.5; p < 0.001). This might be in line with the physical mobility measurements, since less patients reported the ability to walk 500 m without difficulties in the SCC+ than in the SCC− group (58.6% vs .86.9%). Ten percent of the SCC+ participants were not able to walk independently, and it was less characteristic in the SCC− group (3%). The reported difference was significant. The missing response rate was not statistically different in physical independence and the number of chronic illness categories. The results of between group comparison statistics are presented in Table 2.
Changes in lifestyle
The time dedicated to family was greatly reduced in both groups, 78% of the participants irrespective of which group they were in, reported significant reduction, while only 7% indicated increase in this activity. The frequency of physical activity also decreased in a large proportion of subjects (significant reduction was detected in 20% of the SCC+ and in 11.5% of the SCC− group, while slight reduction was present in 32.9% of the SCC+ and 29.5% of the SCC− patients). Only 13% reported at least slightly increased sport activities without significant intergroup differences. Sleep problems were more frequent in the SCC+ than in the SCC− group (70.5% vs. 33.1% respectively). Improvement in subjective sleep quality was reported by less than 3% of the responders. Remote working was increased in 76.9% of SCC+ and 53.4% of SCC− subjects. Reduction was indicated in less than 2% of the participants. While SCC+ patients showed higher decrease in physical activity and increase in sleep problems and remote working, compared to SCC− subjects, the only parameter without dominant missing response differences is the internet use. Seventy-six percent of SCC+ patients versus 55.9% of the SCC− patients reported more intensive use with statistical significance (p’s < 0.001). Furthermore, constant internet use was demonstrated less frequently in the SCC+ group (24.7% vs. 42.2%). Statistical results of between group comparisons are presented in Table 2.
Changes in social engagement
Most of responders spent less time with grandchildren. Consistency was less frequently reported in the SCC+ group (54.6% vs. 62.7%). A 1-point decrease was the most common in both groups (15.9% in the SCC+ and 12.6% in the SCC− group); however, a large 4-point decrease was also frequently found among the SCC+ population (10.23% in SCC+ vs. 3.3% in SCC− group). Changes in voluntary work (11%) and educational activities (10%) were barely reported. A slight reduction was visible in the time spent in social and sport clubs as 17% reported reduction (3.2-point change in average). Only 10.5% of responders indicated less time in patient organizations, but the change was mild (1.1-point change in average). Significant missing response differences were presented between the study groups in all categories. Statistical results of between group comparisons are presented in Table 2.
Factors associated with SCC
Stepwise logistic regression was used to analyse the factors associated with SCC (Table S2 in Supplementary Material). The applied model highlighted that only two parameters defined the outcome of the responders, the physical mobility and independence (ability to walk 500 m without difficulties; OR = 1.186; p < 0.001; 95%CI = 1.101, 1.270) and changes in time spent with grandchildren (OR = 1.04; p = 0.015; 95%CI = 1.008, 1.073). The reported model included only the physical mobility reached 0.082 R square, while the model including both parameters reached 0.108 R square. The improvement of R square values between the two models was significant (p = 0.026). Intergroup differences are presented with error bars in Fig. 2.
Differences in physical mobility and time with family across healthy participants and responders developing subjective cognitive complaints (SCC) during the 3rd wave of COVID pandemic in Hungary. Logistic regression revealed that the key parameter indicating the development of SCC is the reduced physical mobility. Physical mobility was assessed on a 4-point scale where higher scale indicates poor performance. The second important contributor of SCC in our sample is the time spent with grandchildren. Responses were compared on a 7-point scale assessing the estimated time before and during the pandemic. Positive change indicates less time with family. Key: SCC subjective cognitive complaints.
Discussion
In this study, after exclusion, we analysed the data of 359 elderly Hungarians who filled out the WW-Fingers SARS-CoV2 survey. The majority of questionnaires (83%) were completed in February and March 2021, in the first part of the third wave of COVID-19 pandemic in Hungary. Our participants typically live in the capital city and its suburban area, they have a higher-than-average level of education, are mostly retired, and have more than one chronic disease. An important observation was that a quarter of the respondents (n:88) reported subjective cognitive complaints affecting their memory functions that could be related to the COVID-19 pandemic. Our goal was to analyse the sociodemographic features, health status, lifestyle, and social life parameters (altogether 20 features) to characterize the most significant contributors associated with SCC within our cohort. Noticeably, the two measured groups demonstrated significant differences in many parameters regarding the number of missing responses, making the data analysis more complicated. However, participants with SCC showed special characteristics compared to individuals without SCC: (1) they were older; (2) they were more likely to be women; (3) they had on average a higher number of chronic disorders; (4) showed more prominent impairment in physical mobility; (5) had worse sleep quality; (6) spent less time with family; and (7) used internet more frequently during the pandemic (all p’s < 0.001). To eliminate the potential interrelation across these group differences, stepwise logistic regression was applied. As a major finding of this model, impaired pre-pandemic physical mobility and reduced time spent with family during the pandemic were the most characteristic associated with SCC.
Noticeably, even though no memory tests have been carried out, our cohort represented an SCD plus category since: (1) they reported dominantly memory impairment; (2) symptoms developed within the last 5 years; (3) the age of the responders was > 60 years21. The analysed population lends special importance to our findings in the light of studies showing that SCD plus individuals have the highest risk to convert into MCI21.
Our results show that older age is associated with increased likelihood of SCC. This is not surprising, as several studies have confirmed an aging-related increase in the incidence of dementia and MCI28. The higher likelihood for the development of cognitive complaints in women is also in line with the current literature. Recent evidence shows that women have a higher chance to show cognitive symptoms in the presence of Alzheimer brain pathology even in the preclinical stages29,30; they show higher conversion from MCI to AD31; and have a higher risk for AD32. In our analysis, marital status, education, and labour market position were not associated with the presence of SCC; however, our data acquisition follows a special set-up making generalization of these features complicated due to the significant differences between the study groups in regard of the missing responses. Impact of work status is barely measurable in our cohort since the age > 60 years was an inclusion criterion. While low educational years associate with higher dementia risk33, a possible explanation for our results is the high level of education in the entire subject population. Some results reported that living alone increases the risk for SCC34 and for dementia35. We distinguished numerous marital status categories which might decrease the discriminative effect compared to other studies using only strict grouping variables (living with partner or without). However, a trend was also visible in our sample showing higher proportion of divorced and widowed status in SCC+ group. Furthermore, the protective effect of family was clearly reinforced by the regression analysis pointing to the important of time spent with grandchildren as the second most important predictor of SCC.
In the sample, the number of people living with chronic diseases was remarkably high, affecting almost 90% of the respondents, most of them being diagnosed with 2 diseases. Presence of SCC was associated with higher number of concomitant chronic disorders. Since it is well known that parallel to the increase in the number of chronic diseases, the patient's immobility and vulnerability also increases in the majority of the cases, several studies have confirmed their role in the development of SCC36,37,38. Although, in order to prevent dementia, the classic cardiovascular risk factors should be prevented23. Probably the effect of alcohol and smoking is non-measurable since both populations reported only a low dose of alcohol consumption (mild drinkers) and relatively low frequency of smoking. Even if not confirmed by further statistical analyses, it is important to note that 34% of SCC+ (compared to 16% of SCC−) refused to report drinking alcohol before the epidemic, and of those who did report, nearly 7% of SCC+ drank heavily before the epidemic. SCC+ patients also smoked more than SCC− (12.6% vs. 8.9%). Both factors are much studied and have a significant role in the development and progression of cognitive decline39,40. Reduced physical activity and immobility is considered nowadays as one of the most important risk factors of cognitive deterioration24,41,42 and our results also highlighted its crucial and leading predictive value in the development of SCC.
In our study, among the changes in lifestyle factors, the increase in internet use should be highlighted. More than 60% of respondents reported an increase in internet usage and daily use of digital devices. Increased internet use can reduce time spent on physical activities, which can cause anxiety43 and increase feelings of loneliness44, each of these factors may have been independently significantly affected by pandemic-related restrictions. Based on our data, the more frequent use of digital services did not lead to the strengthening of social relations, even though this method of contact would have made it possible. Another important point is that for the elderly, increased digital living space can reduce isolation45, but increased use results in a drastic decrease in satisfaction in this population based on large samples46. Based on previous research data, increased internet use is often accompanied by reduced sleep time, later bedtimes and earlier waking up47. This factor is also significant in our research, since sleep disorders became more pronounced in almost half of the respondents, which was found in several studies to be related to the deterioration of subjective memory48,49,50. One of the most promiment differences between the groups is how greatly the sleep quality decreased in SCC+ vs. SCC−. Sleep disorders may be a prodrome to dementia and sleep has an active role in information processing, with non-rapid eye movement (NREM) being predominantly responsible for processing declarative content and rapid eye movement (REM) sleep for processing non-declarative content51,52. During NREM sleep, acquired information is reactivated and integrated into long-term memory, which is stabilized by a synaptic consolidation process during REM sleep53. Furthermore, higher frequency of sleep disorders and impaired sleep quality in relation to pandemic was observed with the same survey in the United Kingdom in 37% of the responders20, so the increase in sleep problems seems to be general across the various geographical regions.
Based on our results, it can be concluded that although the use of digital services has increased significantly, the time spent with family and close friends has decreased drastically. Among the social activities, volunteering, participation in education, sports, visiting social and other clubs were characteristic in only small ratio of the respondents, even in the period before the pandemic. Furthermore, the ratio of missing responses in social engagement characteristic showed large variety across the study groups. It should be noted that the low engagement in these activities in the Hungarian population might have a negative effect in general, since these are well-known preventive factors of cognitive functions24. The most significant predictive factor in the development of subjective cognitive complaints is the decrease in the frequency of meetings with grandchildren. The lack of that as a source of joy can also greatly affect the emotional life. Almost 80% of the respondents reported that the time spent with family members and friends decreased significantly. This is in line with observations using the same survey in other countries: 55% of the participants reported less contact with friends and 33% with family in a Finnish observation18. The connection between social isolation and the increase in the number of affective disorders was also described as a possible indirect effect of the Covid-19 pandemic54 and it should be carefully considered as a possible long-term change in social behaviour.
In our sample, after performing the regression analysis, two clear risk factors could be highlighted: (1) Physical immobility is the greatest risk and we need to pay special attention to the patient population with low mobility to lessen dementia risk following the pandemic; (2) The time spent with grandchildren is the second most dominant predictor for developing SCC. Reduced physical activity and immobility are currently regarded as a significant risk factor of cognitive deterioration24,41,42. The role of family and social contacts in the prevention and the progression of cognitive decline has long been investigated55,56. These findings highlight the importance of physical activity and close social relationships as a key aspect of healthy brain ageing that is usually overlooked, although many studies have demonstrated their importance24,57,58. This must be also considered on a broad social level since pandemics might change our social relationships on a more consistent way than the short-term restrictions.
To our knowledge, this study was the first in our region that examines the factors predisposing to subjective memory disorder in a larger number of cases. In addition, our research has several important limiting factors. Firstly, due to the characteristics of the international questionnaire, a self-completion cross-sectional test was used, health data on the participants' previous physical and mental health status were only partially known and their assessment was based on the subjective opinion of the respondent. Our results may have been influenced by the fact that some respondents may have been unaware of their COVID-19 infection or denied it. We could not control the changes in the living situation, these were also self-reported changes. It can be assumed that in most cases these changes were caused by the pandemic and related restrictions. The data collection follows a specific design, which makes it difficult to generalise these characteristics. No memory screening test was performed. Secondly, the sample reflects a specific, highly educated, well-cooperating population. Due to the uncertainty surrounding the pandemic, our survey was not representative, we used convenience sampling. Our results are based primarily on data from people living in the Hungarian capital or its suburbs and are therefore not generalisable. Finally, the large variety in the missing responses in numerous parameters complicate the comparisons. This fact also draws attention to a common problem of dementia research analysing the impact of sociodemographic factors. However, it can be assumed that in terms of the main findings, similar changes can be expected in populations belonging to other geographical areas, although their extent cannot be estimated based on the present data. Further joint-analyses are needed within the framework of the World-Wide Finger network.
Data availability
Raw data are available upon request to the corresponding author.
References
WHO. Global status report on the public health response to dementia. 2021. https://apps.who.int/iris/bitstream/handle/10665/344701/9789240033245-eng.pdf.
McKhann, G. M. et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 7, 263–269 (2011).
Petersen, R. C. Mild cognitive impairment as a diagnostic entity. J. Intern. Med. 256, 183–194 (2004).
Petersen, R. C. et al. Alzheimer’s disease neuroimaging initiative (ADNI): Clinical characterization. Neurology 74, 201–209 (2010).
Jessen, F. et al. A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer’s disease. Alzheimers Dement. 10, 844–852 (2014).
Buckley, R. et al. Factors affecting subjective memory complaints in the AIBL aging study: Biomarkers, memory, affect, and age. Int. Psychogeriatr. 25, 1307–1315 (2013).
Galeone, F., Pappalardo, S., Chieffi, S., Iavarone, A. & Carlomagno, S. Anosognosia for memory deficit in amnestic mild cognitive impairment and Alzheimer’s disease. Int. J. Geriatr. Psychiatry 26, 695–701 (2011).
Mitchell, A. J., Beaumont, H., Ferguson, D., Yadegarfar, M. & Stubbs, B. Risk of dementia and mild cognitive impairment in older people with subjective memory complaints: meta-analysis. Acta Psychiatr. Scand. 130, 439–451 (2014).
Kryscio, R. J. et al. Self-reported memory complaints: Implications from a longitudinal cohort with autopsies. Neurology 83, 1359–1365 (2014).
Peters, R. et al. Subjective memory complaints and incident dementia in a high risk older adult hypertensive population. Age Ageing 48, 253–259 (2019).
Ghebreyesus, T. A. 2020. WHO director-general’s opening remarks at the media briefing on COVID-19. WHO director general’s speeches, https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed 11 March 2020.
Heymann, D. L. & Shindo, N. COVID-19: What is next for public health?. Lancet 395, 542–545 (2020).
Kim, Y.-J. & Cho, J.-H. Correlation between preventive health behaviors and psycho-social health based on the leisure activities of South Koreans in the COVID-19 crisis. Int. J. Environ. Res. Public Health 17, 4066 (2020).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 395, 1054–1062 (2020).
Zsuffa, J. A. et al. Impact of the third wave of the COVID-19 pandemic on the lifestyle, mental and physical health of the Hungarian population over 60. Orv. Hetil. 163, 1215–1223 (2022).
Kivipelto, M. et al. World-wide FINGERS network: A global approach to risk reduction and prevention of dementia. Alzheimers Dement. 16, 1078–1094 (2020).
Mangialasche, F. et al. The WW-FINGERS-SARS-CoV2 initiative: Impact of the COVID-19 pandemic on brain health and prevention strategies. Alzheimers Dement. 17, e056732 (2021).
Lehtisalo, J. et al. Changes in lifestyle, behaviors, and risk factors for cognitive impairment in older persons during the first wave of the coronavirus disease 2019 pandemic in Finland: Results from the FINGER study. Front. Psychiatry 12, 624125 (2021).
Udeh-Momoh, C. T. et al. Health, lifestyle, and psycho-social determinants of poor sleep quality during the early phase of the COVID-19 pandemic: A focus on UK older adults deemed clinically extremely vulnerable. Front. Public Health 9, 753964 (2021).
Waterink, L. et al. Changes in brain-health related modifiable risk factors in older adults after one year of COVID-19-restrictions. Front. Psychiatry 13, 877460 (2022).
Jessen, F. et al. The characterisation of subjective cognitive decline. Lancet Neurol. 19, 271–278 (2020).
Kivipelto, M. et al. Risk score for the prediction of dementia risk in 20 years among middle aged people: A longitudinal, population-based study. Lancet Neurol. 5, 735–741 (2006).
Kivipelto, M. et al. The finnish geriatric intervention study to prevent cognitive impairment and disability (FINGER): Study design and progress. Alzheimers Dement. 9, 657–665 (2013).
Livingston, G. et al. Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet 396, 413–446 (2020).
Mukaka, M. M. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 24, 69–71 (2012).
O’gormanWoolson, T. W. R. F. Variable selection to discriminate between two groups: Stepwise logistic regression or stepwise discriminant analysis?. Am. Stat. 45(3), 187–193 (1991).
Merlo, J., Wagner, P., Ghith, N. & Leckie, G. An original stepwise multilevel logistic regression analysis of discriminatory accuracy: The case of neighbourhoods and health. PLoS One 11, e0153778 (2016).
Pike, K. E., Cavuoto, M. G., Li, L., Wright, B. J. & Kinsella, G. J. Subjective cognitive decline: Level of risk for future dementia and mild cognitive impairment, a meta-analysis of longitudinal studies. Neuropsychol. Rev. 32, 703–735 (2022).
Koran, M. E. I., Wagener, M. & Hohman, T. J. Sex differences in the association between AD biomarkers and cognitive decline. Brain Imaging Behav. 11, 205–213 (2017).
Buckley, R. F. et al. Sex, amyloid, and APOE ε4 and risk of cognitive decline in preclinical Alzheimer’s disease: Findings from three well-characterized cohorts. Alzheimers Dement. 14, 1193–1203 (2018).
Sohn, D. et al. Sex differences in cognitive decline in subjects with high likelihood of mild cognitive impairment due to Alzheimer’s disease. Sci. Rep. 8, 1–9 (2018).
Laws, K. R., Irvine, K. & Gale, T. M. Sex differences in Alzheimer’s disease. Curr. Opin. Psychiatry 31, 133–139 (2018).
Xu, W. et al. Education and risk of dementia: Dose-response meta-analysis of prospective cohort studies. Mol. Neurobiol. 53, 3113–3123 (2016).
Wen, C. et al. Risk factors for subjective cognitive decline: The CABLE study. Transl. Psychiatry 11, 1–9 (2021).
Sundström, A., Westerlund, O. & Kotyrlo, E. Marital status and risk of dementia: a nationwide population-based prospective study from Sweden. BMJ open 6, e008565 (2016).
Vassilaki, M. et al. Multimorbidity and risk of mild cognitive impairment. J. Am. Geriatr. Soc. 63, 1783–1790 (2015).
Cordier, R., Chen, Y. W., Clemson, L., Byles, J. & Mahoney, N. Subjective memory complaints and difficulty performing activities of daily living among older women in Australia. Aust. Occup. Ther. J. 66, 227–238 (2019).
Jacob, L., Haro, J. M. & Koyanagi, A. Physical multimorbidity and subjective cognitive complaints among adults in the United Kingdom: A cross-sectional community-based study. Sci. Rep. 9, 12417 (2019).
Kalmijn, S., Van Boxtel, M. P., Verschuren, M. W., Jolles, J. & Launer, L. J. Cigarette smoking and alcohol consumption in relation to cognitive performance in middle age. Am. J. Epidemiol. 156, 936–944 (2002).
Hagger-Johnson, G. et al. Combined impact of smoking and heavy alcohol use on cognitive decline in early old age: Whitehall II prospective cohort study. Br. J. Psychiatry 203, 120–125 (2013).
Tan, Z. S. et al. Physical activity, brain volume, and dementia risk: the Framingham study. J. Gerontol. Ser. A 72, 789–795 (2017).
Podewils, L. J. et al. Physical activity, APOE genotype, and dementia risk: Findings from the cardiovascular health cognition study. Am. J. Epidemiol. 161, 639–651 (2005).
Lee, B. W. & Stapinski, L. A. Seeking safety on the internet: relationship between social anxiety and problematic internet use. J. Anxiety Disord. 26, 197–205 (2012).
Caplan, S. E. Relations among loneliness, social anxiety, and problematic Internet use. Cyberpsychol. Behav. 10, 234–242 (2007).
Şar, A. H., Göktürk, G. Y., Tura, G. & Kazaz, N. Is the internet use an effective method to cope with elderly loneliness and decrease loneliness symptom?. Procedia-Soc. 55, 1053–1059 (2012).
Yang, H. L. et al. Internet use, life satisfaction, and subjective well-being among the elderly: Evidence from 2017 China general social survey. Front. Public Health 9, 677643 (2021).
Sonnega, J. & Sonnega, A. Internet use and sleep among older adults in the United States. Innov. Aging 2, 962 (2018).
Lee, S. H., Kang, Y. & Cho, S. J. Subjective cognitive decline in patients with migraine and its relationship with depression, anxiety, and sleep quality. J. Headache Pain 18, 77 (2017).
Tardy, M., Gonthier, R., Barthelemy, J. C., Roche, F. & Crawford-Achour, E. Subjective sleep and cognitive complaints in 65 year old subjects: a significant association. The PROOF cohort. J. Nutr. Health Aging 19, 424–430 (2015).
Spira, A. P., Chen-Edinboro, L. P., Wu, M. N. & Yaffe, K. Impact of sleep on the risk of cognitive decline and dementia. Curr. Opin. Psychiatry 27, 478–483 (2014).
Rasch, B. & Born, J. About sleep’s role in memory. Physiol. Rev. https://doi.org/10.1152/physrev.00032.2012 (2013).
Stickgold, R. Sleep-dependent memory consolidation. Nature 437, 1272–1278 (2005).
Wang, G., Grone, B., Colas, D., Appelbaum, L. & Mourrain, P. Synaptic plasticity in sleep: Learning, homeostasis and disease. Trends Neurosci. 34, 452–463 (2011).
Pancani, L., Marinucci, M., Aureli, N. & Riva, P. Forced social isolation and mental health: A study on 1,006 Italians under COVID-19 lockdown. Front. Psychol. 12, 663799 (2021).
Glei, D. A. et al. Participating in social activities helps preserve cognitive function: an analysis of a longitudinal, population-based study of the elderly. Int. J. Epidemiol. 34, 864–871 (2005).
Sharifian, N., Kraal, A. Z., Zaheed, A. B., Sol, K. & Zahodne, L. B. Longitudinal associations between contact frequency with friends and with family, activity engagement, and cognitive functioning. J. Int. Neuropsychol. Soc. 26, 815–824 (2020).
Blondell, S. J., Hammersley-Mather, R. & Veerman, J. L. Does physical activity prevent cognitive decline and dementia?: A systematic review and meta-analysis of longitudinal studies. BMC Public Health 14, 1–12 (2014).
Marioni, R. E. et al. Social activity, cognitive decline and dementia risk: a 20-year prospective cohort study. BMC Public Health 15, 1–8 (2015).
Acknowledgements
Our study was supported by National Brain Research Program II and III (2017-1.2.1-NKP-2017-00002; NAP2022-I-9/2022), Janos Bolyai Research Scholarship of the Hungarian Academy of Sciences (bo_78_20_2020) and Momentum Research Grant of the Hungarian Academy of Sciences (Lendulet-2023_94). This is an EU Joint Programme- Neurodegenerative Disease Research (JPND) project: EU-FINGERS: multimodal precision prevention toolbox for dementia in Alzheimer’s disease. The EU-FINGERS project is supported through the following funding organization under the aegis of JPND- www.jpnd.eu (National Research, Development and Innovation, Hungary, 2019-2.1.7-ERA-NET-2020-00006; Swedish Research Council, Sweden). The World-Wide-FINGERS-SARS-CoV-2 survey has been developed by Prof. Kivipelto´s team (FINGERS Brain Health Institute, Karolinska Institute, Sweden; University of Eastern Finland; Finnish National Institute for Health and Welfare and Imperial College London, UK). The FINGERS Brain Health Institute is supported by the Alzheimer’s disease Data Initiative.
Funding
Open access funding provided by Semmelweis University.
Author information
Authors and Affiliations
Contributions
J.A.Z.S. performed the data acquisition, evaluated the results, and concluded the major findings. S.K. was responsible for literature overview. V.K. was responsible for the data extraction and recording. D.B.B. was responsible for the data extraction and recording. A.K. was responsible for the quality control of the manuscript and the concept of the study. G.C.S. was responsible for the control of statistical procedures. A.S.L.R. was responsible for the development of the survey and study protocol. F.M. was responsible for the development of the survey and study protocol. M.K. was responsible for the development of the survey and study concept. She had a leading role in the initiation of the study. A.A.H.was involved in the recruitment of patients, general concept and the design of the study protocol. All authors contributed to the writing of the manuscript and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zsuffa, J.A., Katz, S., Koszovacz, V. et al. Lifestyle and behavioural changes in older adults during the Covid-19 pandemic are associated with subjective cognitive complaints. Sci Rep 14, 2502 (2024). https://doi.org/10.1038/s41598-024-52856-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52856-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.