Abstract
In Mongolia, there is limited data on the prevalence and correlates of common mental health conditions. This study addresses this data gap by exploring anxiety, depression, and brain overwork. The aim of this study was to determine normative data on these conditions in the general population of Mongolia. This nationwide, population-based, cross-sectional study was conducted in 48 sampling centers across Mongolia in 2020. A total of 613 participants (190 men and 423 women) with a mean age of 41.8 ± 12.4 years were recruited. The participants completed the Hospital Anxiety and Depression Scale (HADS) and the Brain Overwork Scale (BOS-10). Vital signs, body measurements, and lifestyle determinants were also assessed. The prevalence of anxiety was 9.9%, depression was 4.9%, and brain overwork was 18.3% among the participants. Anxiety and depression were correlated with brain overwork symptoms. Brain overwork was associated with young age, unemployment, low income, and alcohol use. These findings suggest that anxiety, depression, and brain overwork are a significant problem in the general population of Mongolia. Further research is needed to develop effective interventions to reduce the prevalence and risk factors of anxiety, depression, and brain overwork.
Similar content being viewed by others
Introduction
Mental disorders are a significant worldwide public health problem, with a high prevalence in many countries1. One in eight people in the world are affected by a mental disorder2. However, understanding the complexities of mental well-being requires a nuanced approach that avoids confusion between overlapping concepts. While mental disorders represent specific diagnoses with defined criteria, mental distress often serves as a precursor or even a symptom of these conditions. Mental distress can decrease quality of life, cause disability, and increase mortality. Consequently, it poses substantial challenges to the mental well-being of individuals3. Anxiety and depression, characterized by distinct emotional and cognitive symptoms, are undoubtedly central to mental well-being. Anxiety manifests as excessive worry, fear, and physical tension, while depression casts low mood, hopelessness, and diminished energy. However, the experience of mental distress often goes beyond these classic presentations. Individuals may exhibit somatic symptoms like fatigue, unexplained pain, or sleep disturbances, masking their underlying emotional burden4. These presentations often lead to diagnoses of medically unexplained symptoms or functional somatic syndromes, further complicating the understanding and treatment of their distress5,6. These patients often respond well to treatment with antidepressants and anxiolytics, suggesting that the cause of mental distress may be linked to chronic stress-induced brain activity dysfunction7. It is within this context that we propose the concept of brain overwork as a potential bridge between emotional and physical manifestations of mental distress. Drawing on Selye's General Adaptation Syndrome8, we hypothesize that chronic stress triggers an overactive stress response, leading to an "unrelenting workload" on the brain. This heightened activity, mediated by the hypothalamic–pituitary–adrenal axis and other stress-related pathways, may manifest in various ways, including: (i) excessive cognitive activity, characterized by constant rumination, intrusive thoughts, and difficulty "switching off.", (ii) emotional hypervigilance leading to heightened sensitivity to perceived threats and emotional reactivity, (iii) restless behavior, including physical agitation, difficulty relaxing, and sleep disturbances. These subjective experiences, collectively termed brain overwork syndrome, may not align with existing diagnoses of anxiety or depression but could represent an underlying contributor to these conditions. Furthermore, physical characteristics, such as age, sex, and obesity may influence individual vulnerability to stress and exacerbate its potential consequences, including both mental and physical health problems9,10,11. Chronic stress activates the sympathetic nervous system, leading to increased heart rate, blood pressure, and changes in body temperature12,13,14. Furthermore, anxiety and depression are associated with alterations in breathing patterns and oxygen consumption, potentially impacting oxygen saturation levels15. While a cross-sectional design cannot establish causal direction, examining these physiological markers may provide valuable insights for early identification and intervention. To investigate our hypothesis, we employed a combination of self-report questionnaires and objective physical assessments in a representative sample of the Mongolian general population.
Mongolia is a landlocked country in East Asia, located between Russia and China. The most recent study on the epidemiology of mental disorders in the general population of Mongolia was conducted between 1976 and 1984, and it indicated that a population-wide prevalence of mental disorders was 1.8%16. Since the democratic revolution in 1990, numerous factors such as the political transition from communism to democracy, rapid urbanization, air pollution, lifestyle changes, shifts in disease burden, and economic turbulence over the past three decades have likely significantly impacted the mental health of the Mongolian population. However, no studies have more recently assessed the mental well-being of the general population in Mongolia.
Several mental distress assessment instruments, such as the Generalized Anxiety Disorder-7, Beck Depression Inventory, and Hospital Anxiety and Depression Scale (HADS), have been investigated for their validity and reliability across different cultures. These questionnaires generally possess robust psychometric properties with a focus on emotional symptoms. Notably, the HADS is a concise self-report questionnaire used to assess health-related mental distress in both general and clinical populations17. It comprises of 14 Likert-scale items that represent two latent domains: anxiety and depression. In a previous study, we translated and evaluated the psychometric properties of the Mongolian version of the HADS in the general population, demonstrating good validity and reliability for assessing mental distress18.
To evaluate brain overwork, we utilized the Brain Overwork Scale (BOS-10), which we developed and validated for the Mongolian population. The BOS-10 assesses three core symptoms: excessive thinking, hypersensitivity, and restless behavior. The scale demonstrated excellent internal consistency (McDonald's ω = 0.861) and moderate external reliability (intraclass correlation coefficient = 0.75), indicating its accuracy and consistency in measuring brain overwork in this population. Moreover, the BOS-10's brevity and focus on specific symptoms not fully captured by other measures make it a valuable tool for research and clinical use19.
This study aimed to establish normative data and assess the screening ability of the HADS and BOS-10 for identifying anxiety, depression, and brain overwork in the general Mongolian population. Furthermore, we extensively investigated the sociodemographic and physical characteristics of the Mongolian population to determine factors associated with these conditions.
Materials and methods
Study participants
This cross-sectional study was part of a nationwide, multicenter, interdisciplinary, prospective, population-based cohort study that aimed to examine brain-related disorders in the general population of Mongolia. To ensure our study reflects the Mongolian population aged 18–65, we calculated an initial sample size of 385. This was determined using a 95% confidence level and a 5% margin of error, considering an estimated prevalence of 50% for the characteristic of interest and a population size of 2,028,035 individuals20. Taking into account the lifestyle differences between nomadic herders in rural areas and urban dwellers in urban areas, we included two residency locations, resulting in a target sample size of 770. Considering an 80% response rate, the final sample size required was 924. The inclusion criteria require: (i) participants be Mongolian citizens who have resided in geopolitical units for at least 6 months, (ii) be aged between 18 and 65, and (iii) have not been admitted to any clinical setting during the study. Participants with cognitive deficiencies were excluded from the study. We aimed to create a sample that matched the age and sex distribution of the population. To achieve this, six age-sex groups (18–29, 30–44, 45–65 years; men and women) were used (Supplementary Table S1).
A multi-stage sampling method was employed. In the first stage, we selected representative geological units within each region of the country. Mongolia has four geographical regions, each with 5–6 prefectures. Geopolitical units studied were the capital city, Ulaanbaatar, and the following eight prefectures: Gobi-Altai, Khovd (Western region), Uvurkhangai, Arkhangai (Mountain region), Tuv, Dornogobi (Central region), Dornod and Sukhbaatar (Eastern region). In the second stage, the participants were recruited from 48 sampling centers, including 24 centers in 8 districts of Ulaanbaatar and 24 centers in 8 prefectures of the four rural regions. In the final stage, two or three individuals from each age-sex group were randomly selected from each sampling center depending on the population density. If selected participants were unavailable at the center, they were replaced by the following available participants regardless of age and sex category.
Figure 1 shows the flowchart of the study.
Of the 924 invited individuals, 118 did not attend the sampling center, leaving 806 participants to be approached for the study. 126 of those approached were ineligible due to exceeding the age limit, and 67 were excluded due to missing data on key demographic variables. The remaining 613 participants were included in the final analysis.
Data collection
The data collection for this study commenced on September 7, 2020 and concluded on December 22, 2020. The investigation was conducted in Mongolian, the official language of Mongolia. Trained research personnel or medical doctors delivered in-person explanations of the study instruments to the participants, and assisted them in providing responses via tablet devices. Additionally, comprehensive data encompassing participants' demographic characteristics and lifestyle factors were gathered. Moreover, to evaluate the effect of obesity, anthropometric measurements comprising height, weight, waist circumference, and neck circumference were obtained21. To assess the prevailing physical health status, four primary vital signs were noninvasively examined by adept research personnel or medical doctors: body temperature measured at the forehead or wrist with an electronic infrared thermometer (Tida, TD-133, China), blood pressure and heart rate assessed using an advanced blood pressure monitor (BP A6 PC, Microlife, Switzerland), and arterial oxygen saturation (SpO2) determined via pulse oximetry (PO40, Beurer, Germany). Blood pressure, heart rate, and arterial oxygen saturation were assessed in accordance with the WHO’s guidelines on the measurement of these vital signs22,23.
Instruments
The Hospital Anxiety and Depression Scale (HADS)
The 14-item HADS was used as a reliable and valid measure of anxiety (HADS-A, 7 items) and depression (HADS-D, 7 items). It was developed to identify mental health symptoms in the past week in nonclinical and clinical settings17. Each item is evaluated on a 4-point scale, resulting in a total score ranging from 0 to 21 for each subscale. Scores falling within the range of 0–7 are classified as normal, scores between 8 and 10 indicate a mild abnormality, scores ranging from 11 to 14 denote a moderate abnormality, and scores from 15 to 21 represent severe abnormality for each subscale. We determined the psychometric properties of the HADS in the general population in our previous study, which demonstrated that the Mongolian version of HADS has good validity and reliability for assessing anxiety and depression18.
The Brain Overwork Scale (BOS-10)
The BOS-10 is a 10-item self-report questionnaire that was developed to assess brain overwork in the general population. The BOS-10 measures three dimensions of brain overwork: excessive thinking, hypersensitivity, and restless behavior (Supplementary Table S2). To score the BOS-10, participants are asked to rate how often they have experienced each of the 10 symptoms in the past week on a scale of 0 (never) to 3 (very often). The total score is the sum of the ratings for all 10 items. Higher scores indicate greater levels of brain overwork. The scale has been shown to have good psychometric properties, including high internal consistency, test–retest reliability, and construct validity. The BOS-10 is a tool for screening for brain overwork in the general population and can be used to identify individuals who may need further assessment or treatment19.
Statistical analysis
Data were presented as mean ± standard deviation (SD). Differences between the two groups were examined using the χ2 test for categorical data and one-way ANOVA or t-test for continuous data, as appropriate. To estimate the prevalence of anxiety and depression, cut-off points of 8 and 11 were used for the HADS-A and HADS-D, respectively. The cut-off points for each subscale and total score of the BOS-10 were established by dichotomizing the scores at 1 SD above the mean of each score in the participants of this study24. Correlation analyses between continuous variables were performed using Pearson’s bivariate test. Multiple linear regression analyses were used to determine if risk factors (independent variables: all variables, including sociodemographic characteristics, body measurements, vital function indexes, and the HADS scores) were associated with the mean scores of the BOS-10 (dependent variables: excessive thinking, hypersensitivity, restless behavior, and the total scores of BOS-10). Multicollinearity was examined using variance inflation factor (VIF) and tolerance (1 < VIF < 2.5; tolerance < 10). Homoscedasticity was assessed using scatter plots of residuals by predicted values. No outliers were detected (Cook’s distance < 1; standard residuals < ± 3.3). The independence assumption was tested using the Durbin–Watson coefficient (satisfied if 1.5 < Durbin–Watson < 2.5). To construct a receiver operating characteristic (ROC) curve, the dichotomized variable at the HADS total score with a cut-off point of 13 was used for BOS-10, whereas the dichotomized variable at the BOS-10 total score with a cut-off point of 28 was used for HADS. Using the new nominal variables, we evaluated the screening ability of the HADS and BOS-10 at a range of cut-off points (Supplementary Table S3). All statistical tests were two-tailed with a statistical significance set at p < 0.05. Data were analyzed using SPSS v26.0 and JAMOVI v2.2.5.
Ethical considerations
All procedures performed in this study were done so in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments. The design and methods were reviewed and approved by the Institutional Review Board and Ethics Committee at the Mongolian National University of Medical Sciences, Ulaanbaatar, Mongolia (number: 20/03-05). Written informed consent was obtained from all participants.
Results
There were 613 participants (190 men and 423 women) aged 18–65 years, with a mean ± SD of 41.8 ± 12.4 years. The details of the sociodemographic characteristics are described in Table 1.
There were no differences in marital status, education, income, living condition, residency location, alcohol use, body temperature, heart rate, oxygen saturation, and body mass index (BMI) between men and women. Women were younger, more unemployed, smoked less, and had less blood pressure and neck circumference. Of the participants, 64.1% earned less than ₮500,000 (low income), 34.7% received ₮500,000–1,000,000 (middle income), and 1.1% received more than ₮1,000,000 (high income). 33.6% of the sample population lived in traditional gers or houses that were not connected with water, sanitation, and heating system. More than half (55.6%) of the sample population lived in rural areas.
Table 2 shows the mean and SD of each domain of the HADS and BOS-10 by sociodemographic characteristics among the participants.
The age- and sex-adjusted mean scores of HADS were 9.2 for anxiety, 8.2 for depression, and 17.3 for the total score. The age- and sex-adjusted mean scores of BOS were 10.7 for excessive thinking, 8.4 for hypersensitivity, 12.6 for restless behavior, and 31.0 for the total score. There were no differences in the HADS scores between sex, education, employment, income, alcohol use, tobacco use, and BMI ranges among the participants. In contrast, there were significant differences in the BOS-10 scores between all variables, except sex (p < 0.001, one-way ANOVA or t-test). Both in HADS and BOS-10, younger participants had higher scores than older participants and participants living in urban areas had higher scores than those living in rural areas (both p < 0.001, t-test). Participants living in apartments had higher scores than the other participants in the HADS depression (p = 0.007, t-test). Furthermore, subgroup analyses revealed that as age decreased, all the HADS and BOS-10 scores dropped among the male participants (all p < 0.05 or p < 0.001, one-way ANOVA), and all scores excluding depression decreased among female participants (p = 0.060, one-way ANOVA).
The prevalence of anxiety, depression, and brain overwork were described as percentages of participants above the cut-off scores of the HADS and BOS-10 (Table 3).
The cut-off scores of the HADS were 8 (including mild, moderate, and severe levels) and 11 (including moderate and severe levels) for both anxiety and depression. The cut-off scores of the BOS-10, using a criterion of 1 standard deviation above the mean, were 9 for ET, 8 for H, 12 for RB, and 28 for the total score. The prevalence was 9.9–34.5% for anxiety, 4.9–20% for depression, and 18.3% for brain overwork (the total score of the BOS-10). There was no difference in the prevalence of the HADS and BOS-10 scores between the sexes. In contrast, the prevalence of the HADS and BOS-10 scores differed between age groups. Younger participants had higher anxiety, depression, and brain overwork than older participants.
Table 4 shows the Pearson’s correlation coefficients between the HADS and BOS-10 scores and selected continuous variables.
The HADS and BOS-10 scores showed significant positive correlations to each other and the coefficients ranged from 0.194 to to 0.420. Age was inversely correlated with both HADS and BOS-10 scores. Anxiety was correlated with heart rate. In contrast, depression was inversely correlated with arterial systolic pressure. The BOS-10 scores were inversely correlated to all risk factors, with the exception of heart rate.
Table 5 shows the coefficients of multiple linear regression for the BOS-10.
To investigate how brain overwork was associated with the sociodemographic characteristics, independent variables were selected for each subscale and the total score of the BOS-10, using a stepwise method. This method demonstrates that brain overwork (the total score of the BOS-10) was associated by decreased age, unemployment (student), less income, residency location (apartment), alcohol use, anxiety, and depression (R2 = 0.429, p < 0.001). No multicollinearity was detected between the tested variables; the independence assumption was satisfied; the distribution of the residuals satisfied the normality assumptions. The variance of the model was constant, and homoscedasticity was not violated.
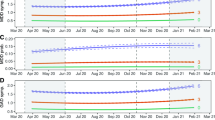
Figure 2 shows the ROC curves of the HADS and BOS-10.
ROC curves of the HADS and BOS-10. (a) The true-positive rates of the HADS subscales against the false-positive rates were plotted at a variety of thresholds for a single variable created by dichotomizing the BOS-10 total score with the cut-off score of 28. (b) The true-positive rates of the BOS-10 scores against the false-positive rates were plotted at a variety of thresholds for a single variable created by dichotomizing the HADS total score with the cut-off score of 17.
The area under the ROC curve (AUC) values of the HADS were 0.73, 0.65, and 0.73 for anxiety, depression, and the total score, respectively. AUC values of the BOS-10 were 0.75, 0.74, 0.69, and 0.76 for ET, H, RB, and the total score, respectively. The AUC indicates performance; the greater the AUC, the better the performance. Two cut-off points were set to calculated sensitivity, specificity, positive predictive value, negative predictive value, and Youden’s index for the HADS and BOS-10 (Supplementary Table S3).
Discussion
The present study aimed to investigate the prevalence, risk factors, and interrelationships of anxiety, depression, and brain overwork among the Mongolian adult population. This is the first report on the normative data on anxiety, depression, and brain overwork in Mongolia, shedding light on the sociodemographic characteristics associated with these mental health conditions and providing insights into potential risk factors. The study sample was chosen to represent the target population which is composed of urban and rural residents. To measure anxiety and depression, we employed the HADS, whereas to assess brain overwork, we used the BOS-10 for excessive thinking, hypersensitivity, and restless behavior. In our previous studies, we validated the Mongolian versions of both the HADS and BOS-10, which showed good validity and reliability for assessing brain overwork in the general population. Therefore, the current results provide valuable information on mental health in the general population of Mongolia.
The prevalence of anxiety, depression, and brain overwork in the study population was significant, with prevalence rates ranging from 9.9 to 34.5% for anxiety, 4.9 to 20% for depression, and 18.3% for brain overwork. The normative scores were higher or similar compared with those of other countries25,26,27,28,29,30 (Supplementary Table S4). These findings highlight the substantial burden of these mental health conditions within the population and emphasize the need for targeted interventions and support services.
The study also explored the relationship between sociodemographic characteristics and mental health outcomes. The results indicated that there were no significant differences in marital status, education, income, living condition, residency location, alcohol use, body temperature, heart rate, oxygen saturation, and BMI between men and women. However, notable distinctions were observed in age, employment status, smoking habits, blood pressure, and neck circumference. These differences suggest that certain factors, such as age and employment, may contribute to variations in mental health outcomes. While no significant differences were observed between the sexes in terms of prevalence rates, variations were evident across different age groups. Younger participants consistently displayed higher levels of anxiety, depression, and brain overwork compared to older individuals. This finding suggests that specific age-related factors, such as life stressors, social pressures, and changes in social roles, may contribute to higher brain overwork in younger age groups. Younger individuals, particularly women, exhibited higher levels of anxiety, depression, and brain overwork, which may be attributed to the challenges associated with transitions and societal expectations. Additionally, the inverse correlations between age and both HADS and BOS-10 scores highlight the potential protective effect of age against the development of anxiety, depression, and brain overwork. This finding may be attributed to increased coping skills, resilience, and adaptive strategies developed over the lifespan.
We found that residency location plays an important role in mental health conditions. The urban residents showed higher scores in anxiety, depression, and brain overwork compared to the rural residents. Initially, we anticipated that individuals residing in rural areas would experience higher levels of anxiety and depression compared to those living in urban areas due to the harsh living conditions, as suggested by previous studies31,32,33. However, our findings were contrary to our initial expectations. The environmental difference might be related to the climate and living conditions. The climate in Mongolia is harsh, with long, cold winters and short, hot summers. The average temperature in January is -30 °C, and the average temperature in July is 20 °C. Over half of the population, approximately 3 million people, resides in rural areas, engaging in nomadic herding and living in traditional dwellings known as gers. Gers lack essential amenities such as centralized electricity, water, sanitation, and heating systems. In contrast, urban residents, mainly concentrated in the capital city of Ulaanbaatar, reside in apartments that are connected to centralized utilities, including heating systems for the harsh winter months. Since the democratic revolution in 1990, the rural population has migrated to Ulaanbaatar, resulting in a population surpassing one million residents. Consequently, this migration has led to the expansion of ger areas in Ulaanbaatar, contributing to its notoriety as one of the most air-polluted cities in the world34. While some households within Ulaanbaatar's ger areas have transitioned to conventional houses, comprehensive central utility systems, apart from electricity, remain lacking. Our previous study found that urban dwellers, particularly those in ger areas, experience lower physical quality of life compared to their rural counterparts35. These findings emphasize the need for targeted interventions and support services for urban dwellers, particularly who live in ger areas.
The study also revealed significant correlations between the HADS and BOS-10 scores. The positive correlations observed between the two scales suggest that individuals experiencing higher levels of anxiety and depression may also exhibit brain overwork and vice versa. This finding suggests potential shared underlying mechanisms and supports the notion of a transdiagnostic approach to mental health assessment and treatment. Also, anxiety was found to be positively correlated with heart rate, while depression demonstrated an inverse correlation with arterial systolic pressure. However, these findings are not generalizable and emphasize the need for further research on the complex relationship between mental and physical health in diverse populations and longitudinal designs.
Moreover, the study identified several sociodemographic factors associated with an increased risk of brain overwork, reflecting the multifaceted nature of this construct. Young age has emerged as a significant risk factor, possibly due to emerging technology-related health concerns. Unemployment/student status and lower income were found to increase risk, suggesting the potential impact of and financial strain on brain function and mental well-being in young adulthood. This aligns with research on the impact of chronic stress and social determinants of health on mental health9,10. Interestingly, residency in apartments was also associated with a higher risk, which may be due to factors such as environmental pollution, limited green space, or lack of privacy. In addition, alcohol use was found to be a risk factor of brain overwork, highlighting the complex relationship between substance use and mental health. This result is consistent with our previous findings that an increased risk of alcohol dependence was associated with being unemployed, and having lower levels of education36. Notably, both anxiety and depression were also associated with brain overwork, raising questions about the complex interplay between these conditions. While the cross-sectional study cannot establish causation, these findings suggest a need for targeted interventions and support systems for vulnerable groups, such as young people, unemployed individuals, and those facing financial hardship. Future research with longitudinal designs should further explore the complex interplay between sociodemographic factors, emotional dysregulation, and brain overwork to inform more effective prevention and intervention strategies.
The cut-off scores established for the HADS and BOS-10 provide valuable clinical thresholds for identifying individuals with clinically significant levels of anxiety, depression, and brain overwork. These cut-off scores can serve as practical screening tools in various healthcare settings, facilitating early detection and intervention.
Mongolia's mental health service system provides a three-level service. Primary care includes 334 general practice clinics distributed throughout the country, which provide basic mental health services for common disorders and act as gatekeepers. Severe cases are referred to secondary healthcare, which is comprised of general hospitals. For complex diagnoses and non-conventional treatments, patients are further directed to tertiary healthcare. The National Center of Mental Health (NCMH), established in 1961, has 450 beds dedicated to inpatient care and provides a wide range of mental health services, including prevention, early detection, diagnosis, and treatment for the entire population. This structure ensures initial support for common disorders, specialized interventions for complex cases, and dedicated inpatient care at the NCMH. However, the system faces potential resource limitations in budget and service delivery capacity, as there are only 0.6 psychiatrists and 0.5 nurses per 10,000 population, which is lower than the global average37,38. Our research provides valuable insights into the prevalence and risk factors of mental health problems, including anxiety, depression, and brain overwork, in Mongolia. Given the high prevalence of mental health problems, the resource limitations of the Mongolian system, and the specific needs identified by our study, it is crucial to advocate for increased funding for mental health services. Such investments should prioritize interventions tailored to the Mongolian context, addressing both psychological and physical aspects of mental well-being. Further research is also warranted to explore the longitudinal trajectories of these mental health conditions and their impact on overall well-being.
Limitations of the study include the reliance on self-report measures, which may be subject to recall bias and social desirability bias. Furthermore, the study was cross-sectional, which means that it cannot establish causality. Additionally, the study had a limited sample size, with a disproportionate number of younger adults and a high attrition rate. Future research should aim to include a broader age range and utilize more objective measures to complement self-report data. Although the findings suggest that the prevalence of anxiety and depression may be high in other developing countries that are undergoing rapid social and economic change such as Mongolia, the study may not be generalizable to other populations.
In conclusion, this study provides valuable insights into the prevalence, risk factors, and interrelationships of anxiety, depression, and brain overwork in a diverse population. The findings underscore the importance of considering sociodemographic factors, including age and employment status, in mental health research and interventions. The observed associations between psychological symptoms and physiological measures highlight the complex interactions between mental and physical health. The identified risk factors and cut-off scores can inform clinical practice and support the development of targeted interventions. Overall, the findings suggest the need for increased funding for mental health services in Mongolia, and interventions that target cognitive processes and emotional reactivity may be effective in reducing mental distress. Further research is warranted to explore the longitudinal trajectories of these mental health conditions and their impact on overall well-being.
Conclusion
This is the first report on normative data on anxiety, depression, and brain overwork in the general population of Mongolia. The findings of this study suggest that these conditions are a significant problem in the general population of Mongolia. Further research is needed to develop effective interventions to reduce the prevalence and risk factors of anxiety, depression, and brain overwork.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Access GBDH, Quality Collaborators. Electronic address cue, Access GBDH, Quality C. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990-2015: A novel analysis from the Global Burden of Disease Study 2015. Lancet 390(10091), 231–266 (2017).
IHME. Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx). https://vizhub.healthdata.org/gbd-results/ (accessed Nov 25 2023).
Schneiderman, N., Ironson, G. & Siegel, S. D. Stress and health: Psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol. 1, 607–628 (2005).
Barsky, A. J., Orav, E. J. & Bates, D. W. Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Arch. Gen. Psychiatry 62(8), 903 (2005).
Wessely, S., Nimnuan, C. & Sharpe, M. Functional somatic syndromes: One or many?. The Lancet 354(9182), 936–939 (1999).
Graver, C. J. Functional somatic syndrome: Assessment and management. J. Osteop. Med. 117(8), 511–519 (2017).
Hiramoto, T., Oka, T., Yoshihara, K. & Kubo, C. Pyrogenic cytokines did not mediate a stress interview-induced hyperthermic response in a patient with psychogenic fever: A case report. Psychosom. Med. 71(9), 932–936 (2009).
Selye, H. Confusion and controversy in the stress field. J. Hum. Stress 1(2), 37–44 (1975).
Akil, H. & Nestler, E. J. The neurobiology of stress: Vulnerability, resilience, and major depression. Proc. Natl. Acad. Sci. USA 120(49), 62120 (2023).
Hodes, G. E. & Epperson, C. N. Sex differences in vulnerability and resilience to stress across the life span. Biol. Psychiatry 86(6), 421–432 (2019).
Tomiyama, A. J. Stress and obesity. Annu. Rev. Psychol. 70(1), 703–718 (2019).
Ginty, A. T., Kraynak, T. E., Fisher, J. P. & Gianaros, P. J. Cardiovascular and autonomic reactivity to psychological stress: Neurophysiological substrates and links to cardiovascular disease. Auton. Neurosci. 207, 2–9 (2017).
Oka T. Stress-Induced Hyperthermia and Hypothermia. Thermoregulation: From Basic Neuroscience to Clinical Neurology, Part II. Handbook of Clinical Neurology 599–621 (Elsevier, 2018).
Lkhagvasuren, B. et al. Increased prevalence of postural orthostatic tachycardia syndrome in psychogenic fever patients. Psychother. Psychosom. 82(4), 269–270 (2013).
Burtscher, J. et al. The interplay of hypoxic and mental stress: Implications for anxiety and depressive disorders. Neurosci. Biobehav. Rev. 138, 104718 (2022).
Byambasuren, S. & Tsetsegdary, G. Mental health in Mongolia. Int. Psychiatry 2(8), 9–12 (2005).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67(6), 361–370 (1983).
Tumurbaatar, E. et al. Translation, reliability, and structural validity of the Hospital Anxiety and Depression Scale (HADS) in the general population of Mongolia. Neurosci. Res. Notes 43(3Suppl), 30–39 (2021).
Lkhagvasuren, B. et al. The brain overwork scale: A population-based cross-sectional study on the psychometric properties of a new 10-item scale to assess mental distress in Mongolia. Healthcare (Basel) 11(7), 1003 (2023).
National Statistical Office of Mongolia. 2019 Population and Housing By-Census of Mongolia. https://www.en.nso.mn/ (Accessed: December 15, 2020); 2020 [updated December 15, 2020December 15, 2020]. https://www.en.nso.mn/.
Kroll, C. et al. The accuracy of neck circumference for assessing overweight and obesity: A systematic review and meta-analysis. Annals of Human Biology. 44(8), 667–677 (2017).
WHO (World Health Organization). WHO Technical Specifications for Automated Non-invasive Blood Pressure Measuring Devices with Cuff 2020. https://www.who.int/publications/i/item/9789240002654.
WHO (World Health Organization). WHO-UNICEF Technical Specifications and Guidance for Oxygen Therapy Devices 2019. https://www.who.int/publications/i/item/9789241516914.
Bat-Erdene, E. et al. Validation of the abbreviated version of the World Health Organization Quality of Life in Mongolia: A population-based cross-sectional study among adults in Ulaanbaatar, Nagoya. J. Med. Sci. 85(1), 79–92 (2023).
Crawford, J. R., Henry, J. D., Crombie, C. & Taylor, E. P. Normative data for the HADS from a large non-clinical sample. Br. J. Clin. Psychol. 40(4), 429–434 (2001).
Hinz, A. & Brahler, E. Normative values for the hospital anxiety and depression scale (HADS) in the general German population. J. Psychosom. Res. 71(2), 74–78 (2011).
Iani, L., Lauriola, M. & Costantini, M. A confirmatory bifactor analysis of the Hospital Anxiety and Depression Scale in an Italian community sample. Health Qual. Life Outcomes 12, 84 (2014).
Hinz, A. et al. Anxiety and depression in the general population in Colombia: Reference values of the Hospital Anxiety and Depression Scale (HADS). Soc. Psychiatry Psychiatr. Epidemiol. 49(1), 41–49 (2014).
Breeman, S., Cotton, S., Fielding, S. & Jones, G. T. Normative data for the Hospital Anxiety and Depression Scale. Qual. Life Res. 24(2), 391–398 (2015).
Kibitov, A. A. et al. Screening of depressive symptoms in a Russian general population sample: A web-based cross-sectional study. Clin. Pract. Epidemiol. Ment. Health 17, 205–211 (2021).
Cianconi, P., Betro, S. & Janiri, L. The impact of climate change on mental health: A systematic descriptive review. Front. Psychiatry 11, 74 (2020).
Kaiser, N., Sjölander, P., Liljegren, A. E., Jacobsson, L. & Renberg, E. S. Depression and anxiety in the reindeer-herding Sami population of Sweden. Int. J. Circumpolar Health 69(4), 383–393 (2016).
Oguzturk, O. Differences in quality of life in rural and urban populations. Clin. Investig. Med. 31(6), 346 (2008).
WHO. Air pollution in Mongolia. Bull. World Health Organ. 97(2), 79–80 (2019).
Bat-Erdene, E. et al. Quality of life in the general population of Mongolia: Normative data on WHOQOL-BREF. PLoS ONE 18(9), e0291427 (2023).
Tumur-Ochir, G. et al. Prevalence of alcohol dependence in Mongolia: A nationwide population-based, cross-sectional study. Neurosci. Res. Notes 6(2), 181 (2023).
HDC. Health Development Center (HDC). Health Indicators 2022. http://hdc.gov.mn/media/files/2022.pdf (accessed Nov 25 2023).
Burvill, P. W. Looking beyond the 1:10,000 ratio of psychiatrists to population. Aust. N. Z. J. Psychiatry 26(2), 265–269 (1992).
Acknowledgements
The authors acknowledge the assistance of the Mon-Timeline cohort study team of the Brain Science Institute at the Mongolian National University of Medical Sciences. We greatly appreciate those who participated in our study and 48 sampling center coordinators who supported for collecting data.
Funding
Funding was provided by Mongolian Coro-Heart Society for Health and Education, Grant no. 2020MN2.
Author information
Authors and Affiliations
Contributions
T.H. conceived the concept. B.L. and T.H. completed the interpretation of data, data analysis, drafting the manuscript, and revision of the manuscript. E.B., E.T., G.T., T.A., and M.D. contributed to data collection and interpretation of data. E.L. and V.V. contributed to developing items and drafting the manuscript. T.O. and T.J. contributed to the revision of the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lkhagvasuren, B., Hiramoto, T., Bat-Erdene, E. et al. Anxiety, depression, and brain overwork in the general population of Mongolia. Sci Rep 14, 2484 (2024). https://doi.org/10.1038/s41598-024-52779-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52779-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.