Abstract
Allergic diseases are prevalent chronic conditions among children and can lead to significant health and economic issues. It is hypothesized that healthy and high quality diet during pregnancy can prevent the onset of allergic diseases in offspring. This study aimed to investigate the potential relationship between major dietary patterns during pregnancy and allergies in children under one year of age. This case–control study was conducted involving 244 participants (122 mothers of allergic children and 122 healthy controls) who visited pediatricians and allergy outpatient clinics in Khuzestan Province, Iran, between June 2022 and March 2023. Demographic information was recorded using a socio-demographic questionnaire. A food frequency questionnaire was used to identify the foods consumed during pregnancy. Major dietary patterns were extracted using principal component analysis, and the potential relationship between these patterns and childhood allergies was investigated using multivariable logistic regression models. The crude odds ratio (OR) analysis showed that the fourth quartile of "Nut, vegetables, fruits, and protein" dietary pattern was associated with lower occurrence of childhood allergies (OR: 0.214, 95% CI = 0.068–0.679; P trend = 0.211). After adjusting for cofactors in Model 3, this association was still observed in the fourth quartile (OR = 0.108, 95% CI = 0.019–0.613; P trend, 0.001). However, no significant association was observed between "Carbohydrate and cereals" and "Salty" dietary patterns and childhood allergies. The study findings suggest that a maternal dietary pattern rich in nuts, vegetables, and fruits during pregnancy may reduce the risk of allergic diseases in offspring.
Similar content being viewed by others
Introduction
Allergic conditions are prevalent in children and can lead to significant health and economic issues. Childhood eczema, asthma, food allergies and allergic rhinitis are among the most common allergic diseases1. Food allergies affect approximately 5% of young children, significantly affecting their quality of life2. Severe food allergy reactions occur at least once in the lifetime of 42% of children with food allergies in the United States3. In Europe, approximately 15%, 16%, and 34% of children reported incidences of asthma, allergic rhinitis, and eczema, respectively4.
Unfortunately, to date, no study has assessed the prevalence of asthma, wheezing, atopic dermatitis, eczema, or food allergies in children under one year of age in Iran. However, some studies have reported the prevalence of these conditions in school-aged children from different regions of Iran. In North Iran, the prevalence rates of wheezing, allergic rhinitis symptoms, and atopic dermatitis symptoms were 16.8%, 14.5%, and 4.5%, respectively, for children aged 6–7 years, respectively5. In 2020, the prevalence rate of eczema in the Zanjan province of Iran was 4.1% among 6- to 7-year-old schoolchildren6. In 2022, the prevalence of ever and current wheeze in Khuzestan province among children aged 6–7 years was 4.5% and 3.8%, respectively7. The general prevalence of atopic dermatitis and current eczema among elementary school Iranian children is 4.9% and 10.4%, respectively8.
Some studies have suggested that exclusive breastfeeding for the first six months of life can reduce the risk of allergic diseases9. Moreover, consuming a healthy diet during childhood, which includes vegetables, fruits, grains, and fish oil rich in unsaturated fatty acids, olive oil, and low-fat dairy products, while reducing the consumption of red meat and poultry can decrease the risk of allergic diseases10.
Adopting a healthy diet and lifestyle during pregnancy can prevent the onset of various diseases in infants and minimize their symptoms and complications. Several researchers have investigated the association between macro-and/or micronutrient intake during pregnancy and the development of childhood allergic diseases11,12. Some studies have suggested that consuming allergenic foods, such as peanuts, during pregnancy may increase the occurrence of allergies in newborns13. Another study reported that a higher maternal intake of milk, peanuts, and wheat during the first and second trimesters was associated with a decrease in mid-childhood allergy and asthma14.
Other researches have investigated the effects of supplementing the maternal diet during pregnancy with individual nutrients like vitamins A or D, fish oil, and probiotics, on allergy prevention15,16,17,18,19. Dietary patterns reflect the types of foods and diets that people regularly consume. Therefore, it is a useful index for epidemiological research to investigate the association between diet and diseases20,21.
A recent study conducted in the United States in 2022 reported that consuming more vegetables and yogurt during pregnancy is associated with the prevention of allergic diseases in offspring22.
It is hypothesized that healthy and high-quality diet during pregnancy can prevent the onset of allergic diseases in offspring. Dietary patterns reflect the habitual consumption of various foods and the type of diet related to cultural and social factors. To date, no research has been conducted on this topic among the Iranian population. As part of this study, we examined the relationship between major dietary patterns during pregnancy and allergies in children under one year of age in the cities of Ahvaz, Dezful, and Shoushtar in Khouzestan Province, Southwest Iran. Furthermore, we compared macro-and some micronutrient intake from foods during pregnancy between mothers of healthy children and mothers whose children exhibited symptoms of allergies during childhood.
Participants, materials, and methods
Participants
Between June 2022 and March 2023, a case–control study was conducted on 244 participants (122 mothers of allergic children and 122 healthy controls) who were referred to pediatricians and allergy outpatient clinics in Ahvaz, Dezful, and Shoushtar cities in Khuzestan Province. The collaborating doctors in this project were pediatricians and allergy sub-specialists. Allergists, diagnosed allergies of the children. The definitions and criteria for the diagnosis of allergic disease are shown in Table 1. The subjects in the control group were selected from among the mothers of children referred to the same outpatient clinic with no history of allergies. The case and control groups were similar in terms of age and ethnicity after group matching. The research plan received ethical clearance from the Medical Ethics Committee at Shoushtar Faculty of Medical Sciences in accordance with the Helsinki ethical guidelines of 2013 (registration number: IR.SHOUSHTAR.REC.1401.005). The research protocol was explained to the subjects, and they signed a consent form before participating in the research.
To be eligible for the study, women had to meet several inclusion criteria, such as being between the ages of 18 and 45 years and having a child under one year of age who exclusively consumed breast milk. Additionally, they had to be married, have a primary school or higher education level, and have no chronic conditions such as diabetes, hypothyroidism or hyperthyroidism, high blood pressure, heart disease, kidney disease, or cancer. They did not have a history of depression or were taking antidepressants, painkillers, or anti-obesity medications. Finally, they were willing to participate in the study. In the case group, the child was diagnosed with an allergy by an allergy specialist physician. Exclusion criteria for both the case and control groups were incomplete questionnaires, and consumption of formula by the child.
The sample size for the case–control study was calculated using an online OpenEPI calculator and the Fleiss method11. A 1:1 ratio was used between the case and control groups, and with 90% power and 95% confidence interval (CI), 122 participants were included in each group. The exposure rates were estimated to be 4% in the control group and 16% in the case group27.
General data collection
A questionnaire designed to gather general information was utilized to obtain demographic data from the participants, such as their age, marital status, medical history, usage of medications and nutritional supplements during pregnancy, financial status, ethnicity, and educational background. Allergy diagnosis in children (atopic dermatitis, eczema, asthma, wheezing, food allergy) was made by a pediatrician and allergy specialist based on clinical symptoms, such as respiratory wheezing, dry cough, and skin inflammation. The mothers' pre-pregnancy weight and height were obtained from their health records, which were routinely updated every time they visited a health center. A digital scale with a precision of 100 g was used to measure weight, with the person wearing minimal clothing and no shoes. To measure the height, a tape measure with a precision of one centimeter was used while the person stood next to a wall without shoes.
Body mass index (BMI) was calculated by dividing a person's weight in kilograms by the square of their height in meters. Participants who did not have pre-pregnancy weight in their health records were excluded from the study.
A short form of The International Physical Activity Questionnaire (IPAQ) was used to investigate physical activity levels28, which was previously validated in an Iranian study29. This study measured the total metabolic equivalent (MET) of the participants and categorized them into three levels: low, medium, and high.
Dietary intake investigation
Three trained nutritionists collected data on participants' food intake frequency by conducting face-to-face interviews and using a food frequency questionnaire (FFQ) consisting of 148 food items. The FFQ was specifically designed for the Iranian and has been previously validated30. To ensure accuracy, a booklet was provided to show the portion sizes of each food group, and participants were asked to explain household measures31. The participants were asked about their food intake frequency during pregnancy, using options such as daily, weekly, monthly, annual, or never. In the first stage of analysis, the frequency of intake for each food item was converted into grams per day using Nutrient 4 software (version 3.5). The macro- and micronutrients of the subjects were then calculated using this software. To extract major dietary patterns, SPSS Statistics for Windows (Version 15.0) was employed.
Dietary pattern extraction
Foods were classified into 20 groups based on their similarity in nutrients (Table 1). Although there was no significant difference in energy intake between the case and control groups, the residual method was used to adjust for total energy intake32. The major dietary patterns identified using Principal component analysis (PCA). The maximum number of factors was determined by this method33, and the sampling adequacy and suitability of the factor analysis were assessed using Kaiser–Meyer–Olkin (KMO) and Bartlett's test of sphericity. The KMO index ranges from 0 to 1, with 0.6 being the minimum value for good factor analysis, and Bartlett's test of sphericity (p < 0.05) was required34. In our study, the adequacy of sampling was confirmed using Bartlett's test (KMO values more than 0.63 with P = 0.02 Bartlett's).
The eigenvalue rule was used to determine the number of factors to be retained, and a scree plot was examined for each value. The maximum number of major dietary patterns was determined using a graph in which the points appeared to lie on the same surface. We considered the scree plot investigation and eigenvalue of more than 1.3 to characterize the number of dietary patterns. Orthogonal rotation (varimax) was used to simplify the data interpretation. To analyze and assess the relationships between food groups and dietary patterns, the study focused on selected food groups that had factor loadings greater than │0.3│. Factor loadings are measures of how strongly a particular food group is associated with a given dietary pattern. By selecting food groups with high factor loadings, the study was able to identify the specific foods that were most strongly associated with each dietary pattern, and to explore the potential health implications of these dietary patterns. By using this analytical approach, the study aimed to gain a more detailed understanding of the complex relationships between diet and health outcomes. Three dietary patterns were identified by analyzing the food groups with the highest factor loadings and then determining a score for each participant based on their adherence to these patterns, which was shown in quartiles. The fourth and first quartiles indicated high adherence to and low intake of dietary patterns, respectively.
Statistical analysis
The Kolmogorov–Smirnov test was used to assess the normality of the distribution of all variables.
Data that follow a normal distribution are presented as the mean and standard deviation, expressed as "mean ± SD". Non-normal variables were reported as medians (25th and 75th percentiles). Categorical variables were compared between cases and controls using the chi-square test. The independent sample t test and Mann–Whitney U test were used to compare quantitative variables between the case and control groups with normal and non-normal distributions, respectively.
Multivariate logistic regression was used to examine the association between the quartiles of the three major dietary patterns during pregnancy and the occurrence of childhood allergies. The Hosmer–Lemeshow test included in regression. Odds ratios (OR) and 95% confidence intervals (CIs) were also calculated. The first model showed a crude OR. In the second model, we adjusted for cofactor effects including mother and father allergy history, physical activity of the mother during pregnancy, and history of smoking during pregnancy. The effects of additional cofactors, including mother weight, mother age, mother educational levels, nutritional supplement intake, birth weight, and type of delivery, were removed from the third model. Statistical analyses were performed using SPSS Statistics software (version 15.0) for Windows, which was developed by SPSS Inc. and is based in Chicago. In this study, a P value less than 0.05, calculated for a two-sided test was deemed to be statistically significant.
Ethical approval and consent to participate
The study protocol was approved by the Medical Ethics Committee of the Shoushtar Faculty of Medical Sciences in accordance with the 2013 Declaration of Helsinki guidelines (registration number: IR.SHOUSHTAR.REC.1401.005). All the participants provided written informed consent.
Results
The participants' dietary intake was analyzed u, and three major dietary patterns were identified, accounting for a cumulative variance of 33.25%. The factor loadings for each food group in the dietary patterns are presented in Table 2.
The first dietary pattern was named "Nuts and seeds, vegetables, fruits, and protein" and accounted for 15.09% of the variance. It was characterized by high intakes of raw and cooked vegetables (including leek, lettuce, basil, parsley, black and red pepper, bell pepper, carrot, raw spinach, stewed vegetables, celery, squash, z zucchini, mushroom, eggplant, turnip, and cooked spinach), summer vegetables (including tomato, cucumber, cantaloupe, melon, and watermelon), fresh and dried fruits (including peach, apricot, fig, pear, apple, plum, nectarine, grape, kiwi, strawberry, persimmon, and date), high-fat and creamy dairies (including high-fat milk, high-fat yogurt, creamy cheese, strained yogurt, cream, and butter) and low and medium-fat dairies (including low-fat milk, and yogurt, skim milk, traditional whey (Kashk), and doogh (a yogurt drink).
The second dietary pattern was named as "Carbohydrate and cereals" and accounted for 9.17% of the variance. It was characterized by a high intake of rice, pasta, potato, breads, and other cereals (such as Barbari, Sangak, Lavash, vermicelli, noodles, whole cereals (oatmeal, barley, and corn), cakes, biscuits, high-fat and creamy dairies (including high-fat milk, high-fat yogurt, creamy cheese, strained yogurt, cream, and butter), and fast food (including pizza, sausage, and hamburger).
"Salt and salty snack" accounted for 8.99% of the variance named as the third dietary pattern. It was characterized by a high intake of salt and salty snacks, sauces, and pickles (including salt, chips, salty popcorn, pickled cucumbers, pickles, and ketchup sauce), citrus fruits (including sweet lemon, lemon, orange, grapefruit, and sour orange), organ meats (including sheep's tongue, liver, and broth of lamb), and a low intake of vegetables (including leek, lettuce, basil, parsley, black and red and bell pepper, carrot, stewed vegetables, celery, squash, zucchini, mushroom, eggplant, turnip, and cooked spinach), bread and other cereals (such as Barbari, Sangak, Lavash, Vermicelli, noodles, whole cereals (oatmeal, barley, and corn), low and medium-fat dairies (including low-fat milk, low-fat yogurt, skim milk, traditional whey (Kashk), and doogh (a yogurt drink)), and legumes (including lentil, broad bean, mung bean, pinto bean, soybean, and pigeon pea).
This study assessed the dietary intake history of 224 participants (112 mothers of healthy children and 112 mothers of children with allergies) during pregnancy. Table 3 presents the demographic characteristics. The average energy intake (measured in kilocalories per day) for both groups was calculated to be 3065.45 ± 1286.69 and 2970.036 ± 1106.43, respectively, and there was no significant difference between the two groups in terms of energy intake.
The mean age of the mothers in the study was 30.20 ± 5.93 years, and the mean BMI was 26.62 ± 5.47. Mothers in the allergy group had a significantly higher level of education than those in the control group (P = 0.047). There were no significant differences between case and control groups in terms of age, pre-pregnancy BMI, maternal physical activity during pregnancy, economic status, and birth weight.
Table 4 presents the association between the quartiles of the three major dietary patterns during pregnancy and the occurrence of childhood allergies using three logistic regression models. The results of crude OR indicated that the fourth quartile of the "Nuts, vegetables, fruits, and protein" dietary pattern was associated with a decreased occurrence of childhood allergy (OR: 0.214, 95% CI = 0.068–0.679; P trend = 0.211). This result was also observed in the fourth quartile after eliminating all cofactors in Model 3 (OR: 0.108, 95% CI = 0.019–0.613, P trend = 0.001).
The crude OR and third adjusted model of the fourth quartile of "carbohydrate and cereals" showed that this dietary pattern was not associated with the occurrence of allergies in children (model 1: OR: 0.671, 95% CI = 0.306–1.472, P trend = 0.381; model 3: OR: 1.217, 95% CI = 0.210–7.045, P trend = 0.460). The quartiles of the "Salt and salty snack" dietary patterns were not associated with the occurrence of childhood allergy in the crude model. After adjusting for cofactors in Model 3, no significant association was observed (Table 4).
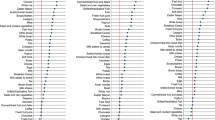
Figures 1 and 2, illustrate a comparison of the mean of macronutrients, some vitamins, and sugar intakes during pregnancy between mothers of children with allergies and mothers of healthy children. According to Fig. 1 the dietary intake of omega-3 fatty acids and folic acid was significantly higher in mothers who gave birth to healthy children during pregnancy. The two groups did not show a statistically significant difference in terms of their intake of simple sugars (Fig. 2).
The dietary intake of omega-3 fatty acids and folic acid was significantly higher in mothers who gave birth to healthy children during pregnancy. (A) Comparison intake of macronutrients between case and control groups, (B) Comparison intake of fatty acids between case and control groups, (C, D) Comparison of intake of vitamins between case and control groups. The data are presented as mean ± SD, and an independent t-test was utilized to compare quantitative variables between case and control groups. *P < 0.05, and **P < 0.01 considered as significant.
The two groups did not show a statistically significant difference in terms of their intake of simple sugars. Comparison intake of sugars between case and control groups. The data are presented as mean ± SD, and an independent t-test was utilized to compare quantitative variables between case and control groups. Total sugar, in addition to the simple sugars shown in the figure, includes alcoholic and other simple sugars. *P < 0.05, and ** P < 0.01 considered as significant.
Discussion
We observed a significant association between the "Nuts and seeds, vegetables, fruits, and protein" dietary patterns during pregnancy, and a decrease in the risk of allergic disease in offspring at one year of age. This dietary pattern is thought to be beneficial due to its high content of nutrients and anti-inflammatory compounds. Nuts and seeds are rich in a variety of nutrients such as vitamin E, magnesium, and fiber, which have been shown to have anti-inflammatory properties. In addition, it suggested that omega-3 fatty acids found in fish and seafood have been shown to have anti-inflammatory properties and may be beneficial for reducing the risk of allergic disease. Maternal diet during pregnancy may affect the nutrient content of breast milk, which can influence the development of the immune system in offspring35,36.
Results of our research have shown that a maternal diet rich in vegetables and fruits during pregnancy can have a significant impact on reducing the risk of allergic disease in offspring.
This result is consistent with the findings of previous studies. Ogawa et al. conducted a study in Tokyo, which found that a higher maternal dietary intake of vegetables during early pregnancy (defined as the first trimester) was associated with a decreased occurrence of wheezing in offspring at the age of 2 years. This association remained significant after adjusting for potential confounding factors such as maternal age, smoking status, and level of education37.
Similarly, Erkkola et al. conducted a study in Finland that found that a lower intake of leafy vegetables during pregnancy was associated with an increased risk of wheezing in children at 5 years of age. The researchers found that children of mothers who consumed less than 1.5 servings of leafy vegetables per day had a higher risk of wheezing compared to children of mothers who consumed more than 1.5 servings per day. This association was independent of other factors such as maternal smoking during pregnancy, family history of asthma, and birth weight38. Vegetables and fruits are rich in antioxidants and other anti-inflammatory compounds that may help to reduce the risk of allergic disease in offspring.
In addition, as a secondary objective, we compared the intake of macronutrients, some vitamins, and sugars between the case and control groups. Our observations showed that mothers of healthy children consumed more dietary folate equivalents (DFE) and omega-3 fatty acids during pregnancy.
Bekkhus et al. also investigated the association between maternal folate intake during pregnancy and childhood asthma in a large population-based cohort in Norway. The results of this study indicated that increased maternal folate intake during pregnancy was linked to a decrease in the risk of childhood asthma39. Sufficient dietary folate intake during pregnancy may alter the expression of genes in the developing fetus through epigenetic modifications, such as DNA methylation. This may affect the development of the immune system in offspring and increase or decrease the risk of allergies40,41.
Omega-3 fatty acids, particularly EPA and DHA, have also been studied for their potential roles in preventing allergic diseases in children. Some studies suggest that maternal intake of omega-3 fatty acids during pregnancy may be associated with a decreased risk of allergic diseases in the offspring42. Sufficient dietary omega-3 intake during pregnancy may affect the mother's immune function, which in turn may influence the development of the immune system in the offspring. A healthy maternal immune system may promote the development of a healthy immune system in offspring, reducing the risk of allergic diseases43,44. Therefore, it is reasonable to recommend that pregnant women consume a diet that includes a variety of folate-rich vegetables and sources of omega-3 fatty acids.
Alpha-linolenic acid (ALA), a type of omega-3 fatty acid found in plants, has anti-inflammatory effects and may play a role in preventing allergic diseases. Green leafy vegetables are a particularly good source of ALA, with approximately 50% of their fatty acid composition comprising ALA. Other sources of ALA include flaxseed, linseed, and chia seeds, which contain a high amount of ALA, accounting for 45–55% of their composition. Walnuts, rapeseed oil, and soybeans are also good sources of ALA, with almost 10% ALA. Encouraging pregnant women to include these foods in their diet can help ensure a sufficient intake of important nutrients during pregnancy45,46,47.
Additionally, studies have demonstrated that omega-3 fatty acids and their metabolites can modulate neutrophil function by augmenting migration, phagocytic capacity, and production of reactive oxygen species (ROS) and cytokines46,47,48,49. The role of the Dietary Inflammatory Index (DII)50,51, the Healthy Eating Index (HEI), 52 and the Mediterranean diet score53,54,55,56, in pregnancy on offspring allergy assessed in previous studies, a total of eight studies were reviewed, but only three of them reported a significant association between maternal diet during pregnancy and offspring allergy.
These researchers reported that higher scores on the Mediterranean diet index and lower maternal DII scores during pregnancy were associated with a lower risk of asthma and wheezing in offspring. However, no significant association was observed between HEI or modified HEI during pregnancy and any allergic diseases in childhood.
In a recent systematic review conducted by the European Academy in 2020, the association between maternal diet during pregnancy and the risk of allergic outcomes in the offspring was evaluated. The authors did not find any reliable evidence to indicate that particular macronutrients, micronutrients, food groups, or dietary patterns should be either avoided or consumed during pregnancy to lower the risk of childhood allergies57. They noted that the included studies had several limitations, such as variations in dietary assessment methods, small sample sizes, and a lack of adjustment for confounding factors. Therefore, they recommended that more studies be conducted to better understand the relationship between maternal diet during pregnancy and allergic outcomes in the offspring.
In a 2022 study, Venter et al. investigated data from the Healthy Start pre-birth cohort in Colorado, including information on mothers and offspring. The researchers calculated a diet index that weighed the intake of several food groups, including fried potatoes, rice/grains, cold cereals, vegetables, yogurt, red meats, and pure fruit juice. The study results showed that maternal intake of yogurt and vegetables during pregnancy was associated with a decreased risk of the offspring developing any type of allergy. However, the intake of red meats, fried potatoes, cold cereals, fruit juice, and rice/grains during pregnancy is associated with an increased risk of allergies in offspring22. The authors propose that future research should investigate the mechanisms underlying these associations.
Earlier investigations in this field assessed how a mother's dietary intake during pregnancy was related to her child's allergies, employing measures such as HEI and DII. Our study, however, utilized the FFQ to identify the major dietary patterns. The major dietary patterns are a prevalent instrument in nutritional epidemiology research, encompassing various types of food based on cultural and geographical factors. By identifying dietary patterns, nutritional researchers can better understand the relationship between a chronic illness and a typical diet.
Strength and limitation
Previous research on this topic has primarily focused on European and American populations, with a limited number of studies conducted in Asian countries. We did not find any published studies that investigated the association between major dietary patterns during pregnancy and the likelihood of allergies in the offspring of Iranian women. In addition, logistic regression models were used to minimize the impact of potential confounding factors. However, this study has some limitations. First, since it was a case–control study, we were unable to establish a definitive causal relationship between dietary patterns during pregnancy and the risk of allergies in the offspring. Second, although we employed a validated questionnaire with 148 food items, recall bias was possible because of the retrospective nature of the questionnaire. In our study, mothers had to recall their diet more than a year ago. Considering that pregnancy is one of the most important periods in women's lives, they usually remember their food intake during this period. However, we did not include women who did not remember details of their food intake during pregnancy. Participants who answered more than 10% of the questions on the food intake frequency questionnaire with doubts were excluded from the study.
Lastly, despite our efforts to consider the effects of certain potential confounding factors, there may be some unmeasured factors that were not considered.
Conclusions
This research showed that “Nuts and seeds, vegetables, fruits, and protein” dietary patterns during pregnancy can decrease the occurrence of childhood allergies. Overall, maintaining a healthy diet that is rich in nutrients and anti-inflammatory compounds may be beneficial for decreasing allergy disease in offspring. Prospective research and clinical trials are needed to provide additional support for these findings. As Asia is a diverse continent with various cultures, it is recommended that future research investigate the risk of childhood allergies associated with cultural and dietary patterns using well-designed prospective studies.
Data availability
The data supporting the findings of this study are available upon request from the corresponding author.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- DII:
-
Dietary Inflammatory Index
- E-DII:
-
Energy-adjusted Dietary Inflammatory Index
- FFQ:
-
Food frequency questionnaire
- HEI:
-
Healthy Eating Index
- HEI-P:
-
Healthy Eating Index for Pregnancy
- KMO test:
-
Kaiser–Meyer–Olkin test
- OR:
-
Odds ratio
- PCA:
-
Principal component analysis
- Q:
-
Quartile
References
Secord, E. Pediatric allergy and immunology revisited. Immunol. Allergy Clin. N. Am. 41(4), 9. https://doi.org/10.1016/j.iac.2021.07.001 (2021).
Paparo, L. et al. Butyrate as a bioactive human milk protective component against food allergy. Nutrients 13(4), 1398–1415. https://doi.org/10.1111/all.14625 (2021).
Gupta, R. S. et al. The public health impact of parent-reported childhood food allergies in the United States. Pediatrics 142(6), e20181235. https://doi.org/10.1542/peds.2018-1235 (2018).
Garcia-Aymerich, J. et al. Phenotyping asthma, rhinitis and eczema in MeDALL population-based birth cohorts: An allergic comorbidity cluster. Allergy 70(8), 973–984. https://doi.org/10.1111/all.12640 (2015).
Mohammadzadeh, I., Ghafari, J., Barari, S. K., Tamadoni, A., Esmaeili, D. M. & Alizadeh, N. R. The prevalence of asthma, allergic rhinitis and eczema in north of Iran: The international study of asthma and allergies in childhood (ISAAC). Iran J. Pediatr. 18(2), 117–122 (2008).
Ahmadiafshar, A., Nourollahi, S., Arminpour, A. & Faghihzadeh, S. The prevalence and risk factors of asthma, allergic rhinitis, and eczema in primary school children, Zanjan, Iran. J. Adv. Med. Biomed. Res. 28(130), 230–236 (2020).
Dastoorpoor, M. et al. Assessing the prevalence and severity of asthma, rhinitis, and eczema among schoolchildren (6–7 and 13–14 years old) in Khuzestan, Iran: A cross-sectional survey. BMC Pediatr. 22, 463. https://doi.org/10.1186/s12887-022-03520-x (2022).
Ghalenoei, A. A. et al. Prevalence and determinants of eczema among elementary school children, Southeast of Iran, 2019. J. Arak. Univ. Med. Sci. 24(3), 438–449. https://doi.org/10.32598/jams.24.3.6370.1 (2021).
Dogaru, C. M., Nyffenegger, D., Pescatore, A. M., Spycher, B. D. & Kuehni, C. E. Breastfeeding and childhood asthma: Systematic review and meta-analysis. Am. J. Epidemiol. 179(10), 1153–1167. https://doi.org/10.1093/aje/kwu072 (2014).
de Silva, D. et al. Preventing food allergy in infancy and childhood: Systematic review of randomised controlled trials. Pediatr. Allergy Immunol. 31(7), 813–826. https://doi.org/10.1111/pai.13273 (2020).
Venter, C. et al. The maternal diet index in pregnancy is associated with offspring allergic diseases: The Healthy Start study. Allergy 77(1), 162–172. https://doi.org/10.1111/all.14949 (2022).
Garcia-Larsen, V. et al. Diet during pregnancy and infancy and risk of allergic or autoimmune disease: A systematic review and meta-analysis. PLoS Med 15(2), e1002507. https://doi.org/10.1371/journal.pmed.1002507 (2018).
Anagnostou, K. & Clark, A. The management of peanut allergy. Arch Dis. Child. 100(1), 68–72. https://doi.org/10.1136/archdischild-2014-306152 (2015).
Wolsk, H. M. et al. Prenatal vitamin D supplementation reduces risk of asthma/recurrent wheeze in early childhood: A combined analysis of two randomized controlled trials. PLoS ONE 12(10), e0186657. https://doi.org/10.1371/journal.pone.0186657 (2017).
Bunyavanich, S. et al. Peanut, milk, and wheat intake during pregnancy is associated with reduced allergy and asthma in children. J. Allergy Clin. Immunol. 133(5), 1373–1382. https://doi.org/10.1016/j.jaci.2013.11.040 (2014).
Yepes-Nuñez, J. J. et al. Vitamin D supplementation in primary allergy prevention: Systematic review of randomized and non-randomized studies. Allergy 73(1), 37–49. https://doi.org/10.1111/all.13241 (2018).
Gunaratne Anoja, W., Makrides, M. & Collins, C. T. Maternal prenatal and/or postnatal n-3 long chain polyunsaturated fatty acids (LCPUFA) supplementation for preventing allergies in early childhood. Cochrane Database Syst. Rev. 7, CD010085. https://doi.org/10.1002/14651858.CD010085.pub2 (2015).
Checkley, W. et al. Maternal vitamin A supplementation and lung function in offspring. New Engl. J. Med. 362(19), 1784–1794. https://doi.org/10.1056/NEJMoa0907441 (2010).
Cuello-Garcia, C. et al. Prebiotics for the prevention of allergies: A systematic review and meta-analysis of randomized controlled trials. Clin. Exp. Allergy 47(11), 1468–1477. https://doi.org/10.1111/cea.13042 (2017).
Hu, F. B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 13, 3–9. https://doi.org/10.1097/00041433-200202000-00002 (2002).
Cespedes, E. M. & Hu, F. B. Dietary patterns: From nutritional epidemiologic analysis to national guidelines. Am. J. Clin. Nutr. 101(5), 899–900. https://doi.org/10.3945/ajcn.115.110213 (2015).
Venter, C. et al. Different measures of diet diversity during infancy and the association with childhood food allergy in a UK birth cohort study. J. Allergy Clin. Immunol. Pract. 8(6), 2017–2026. https://doi.org/10.1016/j.jaip.2020.01.029 (2020).
Venter, C. et al. Dietary factors during pregnancy and atopic outcomes in childhood: A systematic review from the European Academy of Allergy and Clinical Immunology. Pediatr. Allergy Immunol. 31(6), 889–912. https://doi.org/10.1111/pai.13303 (2020).
Al-Shamrani, A., Bagais, K., Alenazi, A., Alqwaiee, M. & Al-Harbi, A. S. Wheezing in children: Approaches to diagnosis and management. Int. J. Pediatr. Adolesc. Med. 6(2), 68–73. https://doi.org/10.1016/j.ijpam.2019.02.003 (2019).
Castro-Rodriguez, J. A. The Asthma Predictive Index: Early diagnosis of asthma. Curr. Opin. Allergy Clin. Immunol. 11(3), 157–161 (2011).
Endre, K. M. et al. Diagnosing atopic dermatitis in infancy using established diagnostic criteria: A cohort study. Br. J. Dermatol. 186(1), 50–58 (2022).
Dean, A. G., Sullivan, K. M. & Soe, M. M. OpenEpi. Open Source Epidemiologic Statistics for Public Health, Version. www.OpenEpi.com. Accessed 15 Sep 2021.
Estrada-Reyes, E. et al. A case–control study of food hyper-sensitivity, timing of weaning and family history of allergies in young children with atopic dermatitis. Allergol. Immunopathol. 35(3), 101–104. https://doi.org/10.1157/13106777 (2007).
Tomioka, K., Iwamoto, J., Saeki, K. & Okamoto, N. Reliability and validity of the International Physical Activity Questionnaire (IPAQ) in elderly adults: The Fujiwara-kyo Study. J. Epidemiol. 21, 459–465. https://doi.org/10.2188/jea.je20110003 (2011).
Vasheghani-Farahani, A. et al. The Persian, last 7-day, long form of the International Physical Activity Questionnaire: translation and validation study. Asian J. Sports Med. 2(2), 106. https://doi.org/10.5812/asjsm.34781 (2011).
Mirmiran, P., Esfahani, F. H., Mehrabi, Y., Hedayati, M. & Azizi, F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 13(5), 654–662. https://doi.org/10.1017/S1368980009991698 (2010).
Ghaffarpour, M., Houshiar-Rad, A. & Kianfar, H. The manual for household measures, cooking yields factors and edible portion of foods. Tehran Nashre Olume Keshavarzy. 7(213), 42–58 (1999).
Willett, W. C., Howe, G. R. & Kushi, L. H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 65, 1220S-S1228. https://doi.org/10.1093/ajcn/65.4.1220S (1997).
Jolliffe, I. T. & Cadima, J. Principal component analysis: A review and recent developments. Philos. Trans. Math. Phys. Eng. Sci. 374, 20150202. https://doi.org/10.1098/rsta.2015.0202 (2016).
Pallant, J. SPSS Survival Manual (McGraw-hill Education, London, 2013).
Palmer, D. J., Metcalfe, J., Prescott, S. L. & Makrides, M. Supplementation with n-3 fatty acid during pregnancy and lactation reduces the incidence of allergic diseases in childhood: A randomized, double-blind, placebo-controlled trial. J. Nutr. 142, 661–668. https://doi.org/10.3945/jn.111.151086 (2012).
Kull, I. et al. Fish consumption during the first year of life and development of allergic diseases during childhood. Allergy 61, 1009–1015. https://doi.org/10.1111/j.1398-9995.2006.01121.x (2006).
Ogawa, K. et al. Association between maternal vegetable intake during pregnancy and allergy in offspring: Japan Environment and Children’s Study. PLoS One 16(1), e0245782. https://doi.org/10.1371/journal.pone.0245782 (2021).
Erkkola, M. et al. Risk of asthma and allergic outcomes in the offspring in relation to maternal food consumption during pregnancy: A Finnish birth cohort study. Pediatr. Allergy Immunol. 23, 186–194. https://doi.org/10.1111/j.1399-3038.2012.01272.x (2012).
Bekkhus, M., Skjærven, R. & Júlíusson, P. B. Folate intake during pregnancy and childhood asthma in a population-based cohort. Allergy 66(8), 1134–1141. https://doi.org/10.1111/j.1398-9995.2011.02614.x (2011).
Hollingsworth, J. W. & Bisgaard, H. Epigenetic mechanisms in asthma and allergy: The role of maternal nutrition. Am. J. Respir. Crit. Care Med. 180(26), 630–636. https://doi.org/10.1164/rccm.200903-0349PP (2009).
Martino, D. J., Prescott, S. L. & Epigenetics, A. Can we develop effective dietary interventions for allergy prevention?. EMBO Rep. 12(3), 197–205. https://doi.org/10.1038/embor.2011.10 (2011).
Bisgaard, H. et al. Fish oil-derived fatty acids in pregnancy and wheeze and asthma in offspring. N. Engl. J. Med. 375, 2530–2539. https://doi.org/10.1056/NEJMoa1503734 (2016).
Prescott, S. L. & Clifton, V. L. Asthma and pregnancy: Emerging evidence of epigenetic interactions in utero. Curr. Opin. Allergy Clin. Immunol. 9(5), 417–426. https://doi.org/10.1097/ACI.0b013e32832e68f5 (2009).
Murphy, V. E. & Gibson, P. G. Asthma in pregnancy. Clin. Chest Med. 32(1), 93–110. https://doi.org/10.1016/j.ccm.2010.11.002 (2011).
Rajaram, S. Health benefits of plant-derived α-linolenic acid. Am. J. Clin. Nutr. 100, 443S-S448. https://doi.org/10.3945/ajcn.113.071514 (2014).
Takic, M., Pokimica, B., Petrovic-Oggiano, G. & Popovic, T. Effects of dietary α-linolenic acid treatment and the efficiency of its conversion to eicosapentaenoic and docosahexaenoic acids in obesity and related diseases. Molecules 27(15), 4471. https://doi.org/10.3390/molecules27144471 (2022).
Calder, P. C. n-3 polyunsaturated fatty acids, inflammation, and inflammatory diseases. Am. J. Clin. Nutr. 83(6 Suppl), 1505S-1519S. https://doi.org/10.1093/ajcn/83.6.1505S (2006).
Kim, J. Y. et al. N-3 polyunsaturated fatty acids restore Th17 and Treg balance in collagen antibody-induced arthritis. PLoS One 13(3), e0194331. https://doi.org/10.1371/journal.pone.0194331 (2018).
Lange, N. E. et al. Maternal dietary pattern during pregnancy is not associated with recurrent wheeze in children. J. Allergy Clin. Immunol. 126(2), 250-255.e1–4. https://doi.org/10.1016/j.jaci.2010.05.011 (2010).
Moonesinghe, H. et al. Association between healthy eating in pregnancy and allergic status of the offspring in childhood. Ann. Allergy Asthma Immunol. 116(2), 163–165. https://doi.org/10.1016/j.anai.2015.11.016 (2016).
Chen, L. W. et al. Maternal dietary inflammatory potential and quality are associated with offspring asthma risk over 10-year follow-up: The Lifeways Cross-Generation Cohort Study. Am. J. Clin. Nutr. 111(2), 440–447. https://doi.org/10.1093/ajcn/nqz291 (2020).
Hanson, C. et al. Associations of prenatal dietary inflammatory potential with childhood respiratory outcomes in project viva. J. Allergy Clin. Immunol. Pract. 8(3), 945–52.e8. https://doi.org/10.1016/j.jaip.2019.09.017 (2020).
Castro-Rodriguez, J. A. et al. Effect of foods and Mediterranean diet during pregnancy and first years of life on wheezing, rhinitis and dermatitis in preschoolers. Allergol. Immunopathol. 44(5), 400–409. https://doi.org/10.1016/j.aller.2016.02.001 (2016).
Chatzi, L. et al. Mediterranean diet adherence during pregnancy and risk of wheeze and eczema in the first year of life: INMA (Spain) and RHEA (Greece) mother–child cohort studies. Br. J. Nutr. 110(11), 2058–68. https://doi.org/10.1017/S0007114513001426 (2013).
Chatzi, L. et al. Mediterranean diet in pregnancy is protective for wheeze and atopy in childhood. Thorax 63(6), 507–513. https://doi.org/10.1136/thx.2007.081745 (2008).
de Batlle, J., Garcia-Aymerich, J., Barraza-Villarreal, A., Anto, J. M. & Romieu, I. Mediterranean diet is associated with reduced asthma and rhinitis in Mexican children. Allergy 63(10), 1310–1316. https://doi.org/10.1111/j.1398-9995.2008.01716.x (2008).
Acknowledgements
The authors have no acknowledgments to declare.
Funding
This research was financially supported by the Vice-Chancellor for Research Affairs of the Shoushtar Faculty of Medical Sciences, Shoushtar City, Iran (grant number: 400000040).
Author information
Authors and Affiliations
Contributions
S.A. conceived and designed the study, analyzed and interpreted the data, and wrote the manuscript. F.A. contributed to the diagnosis and confirmation of the disease. P.A., F.J., and N.A. contributed to data collection. All authors have reviewed and approved the final version of the manuscript prior to submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Adineh, P., Amini, S., Abolnezhadian, F. et al. Nuts, vegetables, fruits, and protein dietary pattern during pregnancy is inversely associated with risk of childhood allergies: a case–control study. Sci Rep 14, 842 (2024). https://doi.org/10.1038/s41598-024-51488-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-51488-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.