Abstract
The growing occurrence of novel recombinants, such as XBB.1.16, has emerged and become predominant, raising concerns about the impact of genomic recombination on the evolution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This study investigated the molecular epidemiological trends and evolution of the Omicron XBB.1.16 epidemic in Bangkok between December 2022 and August 2023. Partial spike and complete genome sequencing of SARS-CoV-2 samples collected from collaborating hospitals were performed. The analysis of 491 partial spike sequences identified 15 distinct lineages, with XBB.1.16 dominating the lineages beginning in March 2023. Phylogenetic analysis revealed at least four distinct XBB.1.16 lineages, suggesting multiple independent introductions into Bangkok. The estimated emergence of XBB.1.16 occurred approximately in January 2022, with an evolutionary rate of 0.79 × 10–3 substitutions per site per year. Monitoring the genomic epidemiology and evolution of XBB.1.16 is vital for the early detection of new strains or emerging variants, which may guide vaccine design and the inclusion of new vaccine strains.
Similar content being viewed by others
Introduction
Since its first emergence at the Huanan Seafood Wholesale Market in December 2019 in Wuhan, China, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused over 6 million confirmed deaths in over 3 years1,2. In early 2022, there was a notable surge in the global incidence of COVID-19 cases, marking a peak in case numbers3,4. In January 2022, over 63.5 million confirmed cases have been reported globally3,4,5,6. Subsequently, from the end of January to early March 2022, a consistent decline in new COVID-19 cases was reported5,7. As of 2023, the current patterns in globally reported COVID-19 cases suggest an underestimation of the actual number of global infections and reinfections8,9. In January 2023, there were nearly 20 million confirmed cases, followed by a decline to 4.8 million in February and a further decrease to 3.6 million patients in March10,11,12. From June to August, the reported number of COVID-19 cases remained consistently at one million each month13,14,15.
In Thailand, during early 2022, the number of reported COVID-19 patients with the omicron variant surged significantly, but it has continuously decreased since July 202216. After the Songkran Festival (also known as the Thai New Year Festival) in April 2023, there was a tenfold increase in COVID-19 cases, creating potential opportunities for heightened transmission. The surge in cases was likely exacerbated by many individuals traveling back to their hometowns to partake in the festive celebrations17,18,19.
In the early stages of the pandemic, one of the initial SARS-CoV-2 mutations that rapidly spread worldwide was the D614G mutation (PANGO lineage B.1) in the spike (S) gene, which was first identified in Europe in January 202020. As of now, the World Health Organization, along with national public health agencies, has designated five SARS-CoV-2 variants as variants of concern (VOCs) due to their significantly altered transmissibility or immune escape capabilities: Alpha (lineage B.1.1.7), Beta (B.1.351), Gamma (P.1), Delta (B.1.617.), and Omicron (B.1.1.529). The Delta and Omicron variants have rapidly spread worldwide, whereas Alpha, Beta, and Gamma have asserted dominance in specific regions. With mutations in both the receptor-binding domain (RBD) and the N-terminal domain (NTD), all these VOCs share a common N501Y mutation situated on the RBD, except for the Delta variant. This specific mutation increases the spike protein's affinity to angiotensin-converting enzyme 2 (ACE2) receptors, thereby strengthening the high infectivity21. The L452R mutation within Delta variants enhances spike stability, viral infectivity and fusogenicity, ultimately promoting viral replication22. With over 60 mutations, the Omicron variant possesses 15 mutations within the RBD23. The mutations in the NTD region, such as T76I, L141F, G142Y, 156–167 deletion, and R158G, have been observed to impact antibody binding efficiency, contributing to immune evasion24. The development of vaccines against SARS-CoV-2 represents a significant milestone in mitigating the effects of COVID-19. Nevertheless, the pandemic continues to persist, facilitating the accumulation of mutations throughout the entire SARS-CoV-2 genome due to ongoing viral transmission.
The XBB.1.16 subvariant has accounted for the substantial upsurge in COVID-19 cases in India in January 202325. Its global prevalence has been steadily rising, marked by weekly increases, and the WHO has identified XBB.1.16 in at least 33 countries26. As a result of this surge in cases, the WHO officially categorized XBB.1.16 as a variant under monitoring status on 22 March 2023, following its initial designation as a variant of interest on 17 April 202327. Nonetheless, there is currently no evidence indicating that it causes more severe illness.
In Thailand, six lineages were identified in the first quarter of 2020, including A, A.6, B, B.1, B.1.8, and B.5828. The B.1.36.16 variant was responsible for the predominant outbreak during the second wave (December 2020–January 2021), while the Alpha variant led the third wave (April–June 2021), Delta characterized the fourth wave (July–December 2021), and Omicron emerged during the fifth wave (January–March 2022)29. In July 2023, the new SARS-CoV-2 variant BA.2.86 was identified in the community through wastewater surveillance in Bangkok30. Since the emergence of the XBB.1.16 variant in March, the Ministry of Public Health (MoPH) has recorded a cumulative total of 24,292 confirmed cases16,17,18,19. During the period dominated by XBB.1.16, the number of infections was less than half of the outbreak attributed to the BA.2.75 variant in late 2022 (Figure S1).
The emergence and dominance of novel recombinants, like XBB.1.16, have raised concerns regarding the influence of genomic recombination on the evolution of SARS-CoV-2. This study investigated the molecular epidemiological trends and evolution of the omicron XBB.1.16 epidemic in Bangkok, Thailand, between December 2022 and August 2023.
Results
Molecular detection of SARS-CoV-2 lineages and sub-lineages
During the study period, we collected 491 RNA-positive SARS-CoV-2 samples from Bangkok residents, submitted to collaborating hospitals in Bangkok. These samples were amenable to partial spike sequencing, with an additional 50 samples chosen randomly for complete genome sequencing. Of the collected samples, 278 (57%) were from female patients and 213 (43%) were from male patients. Ten percent of the patients were aged 2 months to 10 years, 2% were aged 11–20 years, 16% were aged 21–30 years, 22% were aged 31–40 years, 14% were aged 41–50 years, 13% were aged 51–60 years, and 23% were older than 60 years (Table 1).
The Ministry of Public Health Thailand (MoPH) report covering the SARS-CoV-2 outbreak from December 2022 to August 2023 includes 49,139 confirmed cases and 1,279 deaths. (Fig. 1a)31. In 2023, a large increase in COVID-19 outbreaks was observed during the summer period, reaching a peak between May and June. Reports of COVID-19 cases in Thailand from February to early April were consistently low, with weekly numbers below 500 cases. The number of deaths from the COVID-19 outbreak in July 2023 declined by half compared to December 2022.
(a) Cases of confirmed SARS-CoV-2 infection reported in Thailand31. (b) Timecourse of omicron variant distribution in Bangkok, Thailand, between December 2022 and August 2023.
A comprehensive analysis of the 491 SARS-CoV-2 partial spike sequences generated identified 15 distinct lineages (Fig. 1b). Among these, 33.82% were identified as BA.2.75, 28.36% as XBB.1.5, 3.99% as XBB.2, 3.57% as BA.2, 1.47% as BA.5.2, and 1.05% as XBB.2.3. Five variants showed frequencies below 1%, including BA.5 (0.84%), XBB.1 (0.84%), XBB.1.9 (0.84%), BA.5.3 (0.63%), and BA.2.3 (0.21%). Additional lineages, specifically XBC.1 (0.21%) and XBF (0.63%) were also detected in February 2023 and April 2023 respectively.
During the study period, 23.32% of patients presented with XBB.1.16 infection. A significant increase in XBB.1.16 variants have been detected in the current study, with 4% in March, 29.0% in April, 58.9% in May, and peaking at 66.7% in July 2023. XBB.1.16 persisted as the predominant variant identified in the outbreak throughout August.
Figure S2 shows the evolutionary relationships among 491 Thai SARS-CoV-2 partial spike sequences and the corresponding emergence dates in Thailand. The Bayesian time-scaled phylogenetic analysis calculated an average evolutionary rate across the genome of 4.04 × 10−3 nucleotide substitutions per site per year (sub/site/year), with a 95% highest density interval (HDI) ranging from 2.75 × 10−3 to 5.40 × 10−3.
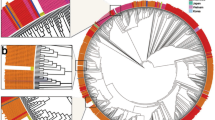
Time-scaled phylogenetic reconstruction of SARS-CoV-2
Using high-throughput sequencing technologies, an additional set of 50 complete SARS-CoV-2 genomes derived from COVID-19 patients in Thailand was successfully compiled. The time-resolved maximum likelihood tree constructed using global XBB.1.5 and XBB.1.16 sequences in comparison with the parent XBB sequences shown in Fig. 2 indicates that the emergence of the most recent common ancestor of XBB.1.5 can be traced back to approximately June 2022. Based on analysis of the time to the most recent common ancestor, the emergence of XBB.1.16 took place around October 2022. In Fig. 2 the tips are color-annotated based on the continent where the sequences were identified, and the sequences from the current study are labeled with a red triangle. The evolutionary rate was estimated to be 0.73 × 10−3 nucleotide substitutions per site per year (sub/site/year) (95% HDI 0.59 × 10−3 to 0.85 × 10−3) from the XBB.1.5, XBB.1.16, and XBB variant time-scaled phylogeny inferred with the complete genome dataset. The XBB.1.16 variant consisted of 203 sequences and exhibited substantial genetic diversity, forming two distinct subclades in October 2022. This variant also exhibited the broadest geographical distribution worldwide.
Divergence times of phylogenetic trees of global XBB.1.5, XBB.1.16, and XBB viruses using molecular clock. A time-resolved maximum-likelihood phylogenetic tree of XBB.1.5, XBB.1.16, and XBB samples sequenced worldwide and sequences from this study is shown. The scale bar indicates nucleotide substitutions per site.
SARS-CoV-2 infections have been detected in nearly all provinces across Thailand, except for Phang Nga Province in the southern region, where no cases have been reported (Fig. 3a). The three provinces with the highest numbers of SARS-CoV-2 infections, Bangkok, Chonburi, and Nonthaburi, are all located in the central region. In the northern region, Lamphun had the highest number of infections, and in the southern region, Songkhla and Surat Thani had the highest numbers of infections. In the northeastern region, the provinces with the most infections were Khon Kaen, Nakhon Ratchasima, Buri Ram, Surin, and Ubon Ratchathani (Fig. 3a).
(a) Map of the regions in Thailand most affected by the SARS-CoV-2 outbreak from December 2022 to August 202331. Administrative divisions in the northern, central, northeastern, and southern areas are differentiated by blue, brown, red, and green color respectively. These colors represent the cumulative numbers of confirmed and suspected cases reported throughout the outbreak. (b) Root-to-tip regression of genetic distances against sampling time (month) for SARS-CoV-2 XBB.1.16 variant sequences based on a maximum likelihood tree. (c) Temporal phylogeny of all publicly accessible XBB.1.16 genomes in Thailand estimated using BEAST. Each tip is color-coded based on the probable region within the country where the patient was infected.
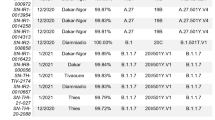
As at 13 August 2023 a total of 329 complete SARS-CoV-2 XBB.1.16 genomes identified in Thailand were accessible via GISAID32. Together with the 29 XBB.1.16 sequences acquired from Bangkok Province in the present study, the dataset includes a total of 358 genome sequences of SARS-CoV-2 XBB.1.16 collected from 58 provinces across Thailand, with sampling dates between December 2022 and August 2023. The sequences predominantly originate from Bangkok in the central region (100/358, 27.9%) and Nakhon Phanom in the northeast region (31/358, 8.7%).
Root-to-tip linear regression analyses were conducted using the best-fitting root, which minimizes the mean of the squares of the residuals, to investigate relationships between genetic divergence and sampling dates. These analyses indicated significant temporal structure in the collected dataset (R2 = 0.30, correlation coefficient 0.55), suggesting a clocklike pattern of molecular evolution, with a substitution rate of 0.86 × 10−3 sub/site/year (Fig. 3b).
Phylogenetic analysis revealed the presence of at least four distinct XBB.1.16 lineages in Thailand (Fig. 3c). The majority of XBB.1.16 genomic sequences sampled from Bangkok Province formed clusters with genomic sequences from several other Thailand provinces. This suggests that XBB.1.16 had already spread from Bangkok Province to other regions in Thailand, indicating multiple independent introductions of XBB.1.16 from various Thailand provinces into Bangkok. Based on Bayesian time-scaled phylogenetic analysis using the tip-dating method, the estimated most recent common ancestor date for XBB.1.16 was January 2022, with an evolutionary rate estimate of 0.79 × 10−3 sub/site/year (95% highest posterior density interval 0.46 × 10−3 to 1.13 × 10−3).
Discussion
Despite the WHO discontinuing COVID-19’s global emergency status, SARS-CoV-2 continues to cause substantial morbidity and epidemics worldwide, including in Thailand. The current study investigated the molecular epidemiology of SARS-CoV-2 variants and the evolution of XBB.1.16 circulating in Thailand between December 2022 and August 2023. The investigation was conducted by characterizing the weekly occurrences of SARS-CoV-2-associated outbreaks, and analyzing the distribution of circulating variants during these outbreaks. In Thailand during the first half of 2022 the predominant SARS-CoV-2 variants were the omicron subvariants BA.1 and BA.2, with subsequent months seeing an emergence of BA.4 and BA.5, as previously reported26,33. The present study revealed that in December 2022 initial identification of the XBB, XBB.1, BA.5.2, and BA.5.3 lineages indicated low prevalence. Between December 2022 and February 2023, BA.2.75 was the most dominant variant among COVID-19 cases, followed by XBB.1 and XBB.1.5. The emergence of XBB.1.5 resulted in its dominance from March to April. By mid-June 2023, XBB.1.16 had ascended as the dominant global strain, surpassing the XBB.1.5 variant in terms of prevalence28. As at 05 June 2023 a total of 19,847 sequences belonging to the omicron XBB.1.16 variant were accessible, originating from 66 different countries. A large proportion (40.7%) of these XBB.1.16 sequences were sampled in India. Sequences from other Asian nations are also noteworthy, with contributions from China (6.1%), Singapore (5.6%), Japan (4.5%), South Korea (4.3%), Malaysia (1.5%), Thailand (1.5%), Indonesia (0.7%), Brunei (0.6%), and Vietnam (0.6%)34. The present study is consistent with a report from Singapore, which found that during the first half of 2023, XBB.1.16 was the predominant strain, followed by XBB.1.5, XBB.1.9, and XBB.2.335. That report also indicated that there is a higher risk of severe outcomes when infected with XBB.1.16 compared to XBB.1.5 or XBB.1.9, there is no significant difference in the risk of hospitalization associated with different XBB variants.
A previous study investigated the global evolution rate of SARS-CoV-2 during the early stages of the pandemic and reported an estimated mean nucleotide mutation rate of approximately 6.58 × 10−3 sub/site/year36. The evolution rates for the full genome of the Gamma variant reportedly range from 1.12 × 10−3 to 4.91 × 10−3 sub/site/year, as determined via sequencing of circulating viruses37,38. The evolution rates of XBB.1 and XBB.1.5 variants exhibit a degree of similarity, at 0.63 × 10−3 and 0.69 × 10−3 sub/site/year respectively39,40. In the present study the respective rates of evolutionary change of the XBB.1.16 variant determined via Bayesian analyses with the tip-dating method and root-to-tip linear regression were 0.79 × 10−3 sub/site/year and 0.86 × 10−3 sub/site/year. Notably, these rates are slightly higher than those reported in another study that investigated XBB.1.16 variants, which documented a rate of 0.39 × 10−3 sub/site/year41.
In early 2022, Thailand experienced a surge in SARS-CoV-2 infections propelled by the BA.1 and BA.2 variants, resulting in significant outbreaks with weekly cases reaching 150,000–180,000. The following three months witnessed a sharp decline, nearly a tenfold reduction per week, credited to the emergence of the BA.5 variant. However, the recent appearance of the XBB.1.16 variant has led to a substantial increase, with weekly cases surging from 100 to 3000. There is no evidence of a difference in clinical outcomes among individuals infected with different variants in Thailand. This could be challenging to ascertain, considering that a majority of the population has been vaccinated.
The current study had several limitations, with one primary constraint being the potential for sampling bias. The genomic data used in the study were obtained from diagnosed cases, which may not comprehensively represent the entire spectrum of SARS-CoV-2 infections. Asymptomatic patients, mild infections, or cases in regions with limited testing may be underrepresented in the dataset, leading to a skewed understanding of the virus’s evolutionary dynamics. Additionally, because XBB.1.16 is a new variant, limited historical genomic data are available for comparison. While genomic data can reveal mutations and genetic changes, determining their functional implications (e.g., increased transmission, immune escape, and altered disease severity) requires additional experimental studies. Genomic data alone may not completely facilitate understanding of the consequences of specific mutations.
In conclusion, the present study contributes to the understanding of the genomic epidemiology and evolution of XBB.1.16 in Bangkok, Thailand. The dominant sub-lineage that emerged was XBB.1.16, beginning in March 2023. Phylogenetic analysis showed a minimum of four distinct lineages of XBB.1.16, indicating the multiple independent introductions into Bangkok. Our analysis shows the potential of molecular epidemiology and the evolution of XBB.1.16 to identify the most prevalent and potentially emerging strains, which may guide vaccine design to reduce the impact of COVID-19 illness.
Materials and methods
Institutional review board statement
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board of the Faculty of Medicine, Chulalongkorn University, Thailand (approval number IRB0538/66). All information and patient identifiers were anonymized to protect patient confidentiality. Due to the retrospective nature of the study, the Institutional Review Board of the Faculty of Medicine, Chulalongkorn University, Thailand (approval number IRB0538/66) waived the need to obtain informed consent.
SARS-CoV-2 sample collection and viral RNA extraction
The nasopharyngeal and pharyngeal swabs from 491 Bangkok residents used in this study were submitted to collaborating hospitals for SARS-CoV-2 testing. RNA extraction from a 200-μL aliquot of the supernatant was conducted in our laboratory using a magLEAD 12gC instrument (Precision System Science, Chiba, Japan) in accordance with the manufacturer’s instructions. From December 2022 to August 2023, a total of 491 SARS-CoV-2 RNA samples were collected, and the partial spike gene was amplified from individuals diagnosed with COVID-19. Of those, 50 samples were randomly selected and subjected to complete genome sequencing.
Partial spike gene amplification and sequencing
A total of 491 samples that tested positive for SARS-CoV-2 were subjected to variant identification via RT-PCR using primers designed based on nucleotide sequences obtained from the GenBank database. The PCR aimed to amplify the partial spike gene with an amplicon length of 1,036 bp, using the following primers:
Briefly, RT-PCR was conducted in a total volume of 25 µL, incorporating 2–3 µL of 100 ng to 1 µg of total RNA, 0.5 µM of each primer, 12.5 µL of 2X Reaction Mix (containing 0.4 mM of each dNTP and 3.2 mM MgSO4), 1 µL of SSIII RT/Platinum Taq Mix, and nuclease-free water. The Superscript III One-Step RT-PCR system with Platinum Taq High Fidelity was used in accordance with the manufacturer’s instructions (Invitrogen, Carlsbad, CA, USA). The PCR process included initial incubation at 45 °C for 40 min, followed by 40 cycles consisting of denaturation at 94 °C for 30 s, annealing at 50 °C for 30 s, and extension at 68 °C for 1 min 45 s. A final extension was performed at 68 °C for 5 min. Both forward and reverse directions were employed simultaneously for sequencing and product amplification at First BASE Laboratories Sdn Bhd (Selangor Darul Ehsan, Malaysia).
NGS
The Celemics comprehensive respiratory virus panel (Celemics Inc., Incheon, Republic of Korea) was utilized for sequencing and identifying complete SARS-CoV-2 genomes. In the RNA extraction process, 25 ng of extracted RNA was mixed with an RNA fragment buffer mix to facilitate fragmentation. Subsequently, first-strand cDNA was synthesized using a first-strand synthesis master mix. The first-strand cDNA underwent double-stranded cDNA construction through incubation at 16 °C for 60 min with a 2nd-strand synthesis-1 mix, followed by a 2nd-strand synthesis-2 mix at 25 °C for 15 min. The resulting double-stranded cDNA underwent cleaning, repair, and the addition of poly(A) tail oligomers in a 5 ERA buffer mix. Following multiple incubation steps at different temperatures, the A-tailed DNA was ligated with adaptors in a ligation reaction mix at 20 °C for 15 min. The ligated DNA was purified using CeleMag cleanup beads, amplified, and transformed into an adaptor-ligated library using CLM polymerase and UDI primers, following the manufacturer’s instructions. To assess the quantity and quality of the constructed DNA library, automated capillary gel electrophoresis (QIAxcel; Qiagen, Hilden, Germany) was employed, ensuring the presence of 200- to 400-bp DNA fragments. The DNA libraries were subsequently subjected to Next-Generation Sequencing (NGS) using the Illumina NextSeq 500 system with the mid/high-output kit v2.5 (300 cycles). The resulting FASTQ data underwent trimming, assembly, and analysis through the Celemics Virus Verifier pipeline, facilitating identifying and generating consensus sequences for the SARS-CoV-2 genome. Any nucleotide gaps identified in the assembled SARS-CoV-2 FASTQ sequences were addressed by incorporating nucleotide sequences obtained from conventional RT-PCR-derived Sanger sequencing. This was accomplished using primers specifically designed for those gaps.
Bayesian phylogenetic analysis
By 13 August 2023, a set of high-quality SARS-CoV-2 genomes had been retrieved from GISAID. These genomes met specific criteria, including having < 1% unidentified nucleotides (N) and a complete length > 29 kb. The sampled genomes represented the lineages XBB (n = 13), XBB.1.5 (n = 44), and XBB.1.16 (n = 188) globally, and there were 329 samples of lineage XBB.1.16 from Thailand from the respective lineages covering the same timeframe (December 2022–August 2023). SARS-CoV-2 XBB.1.5 and XBB.1.16 complete genome sequences from Thailand were compiled using BioEdit v.7.2.6 software42 and aligned with the global reference datasets of the corresponding lineage using MAFFT v.7.47543.
BEAST v.1.10.544 was employed for constructing Bayesian time-scaled phylogenies. These phylogenies utilized a general time-reversible substitution model with gamma-distributed rate variation among sites, a relaxed molecular clock with a log-normal prior45, and an exponential growth coalescent tree prior46. Two independent Markov Chain Monte Carlo (MCMC) chains, each comprising 200 million states, were merged using the BEAGLE package47 to enhance computational efficiency and runtime. Sampling of parameters and trees occurred every 20,000 steps, discarding the initial 20% as burn-in. To ensure an effective sample size > 200 for all estimated parameters, convergence and mixing of MCMC chains were assessed using Tracer v.1.748. Maximum clade credibility (MCC) trees were summarized using TreeAnnotator v.1.10, and visualized with FigTree v.1.4.4 (https://github.com/rambaut/figtree/releases).
Maximum likelihood phylogenetic tree and temporal signal
The XBB.1.16 dataset underwent maximum likelihood phylogenetic analysis with IQ TREE v.2.1.249. This analysis utilized a general time-reversible model of nucleotide substitution with gamma-distributed rate variation among sites (G4). It included a proportion of invariable sites (+ I) and empirical base frequencies (+ F), chosen through recommendations from ModelFinder within IQ-TREE50. Branch support was assessed using the Shimodaira-Hasegawa-like procedure (SH-aLRT) with approximately 1000 replicates for the likelihood-ratio test. To assess the temporal signal within the XBB.1.16 dataset, regression analysis of root-to-tip divergence against sampling time was performed using TempEst v.1.5.3651, based on the ML tree.
Nucleotide sequence accession IDs
The genome sequences obtained in this study have been submitted to the NCBI databases. Accession numbers are provided in Supplementary Table S1.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Wu, F. et al. A new coronavirus associated with human respiratory disease in China. Nature 579, 265–269 (2020).
Zhou, P. et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579, 270–273 (2020).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 76, published 25 January 2022.file:///C:/Users/ASUS/Downloads/20220125_Weekly_Epi_Update_76.pdf (2022).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 74, published 11 January 2022. file:///C:/Users/ASUS/Downloads/20220111_Weekly_Epi_Update_74.pdf (2022).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 73, published 6 January 2022. file:///C:/Users/ASUS/Downloads/20220106_Weekly_Epi_Update_73–1.pdf (2022).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 75, published 18 January 2022. file:///C:/Users/ASUS/Downloads/20220118_Weekly_Epi_Update_75.pdf (2022).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 85, published 29 March 2022. file:///C:/Users/ASUS/Downloads/20220329_Weekly_Epi_Update_85.pdf (2022).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 125 published 11 January 2023. file:///C:/Users/ASUS/Downloads/20230111_Weekly_Epi_Update_125.pdf (2023).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 136 published 30 March 2023. file:///C:/Users/ASUS/Downloads/20230330_Weekly_Epi_Update_136.pdf (2023).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 128 published 1 February 2023. file:///C:/Users/ASUS/Downloads/20230201_Weekly_Epi_Update_128.pdf (2023).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 132 published 1 March 2023. file:///C:/Users/ASUS/Downloads/20230301_Weekly_Epi_Update_132.pdf (2023).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 136 published 30 March 2023. file:///C:/Users/ASUS/Downloads/20230330_Weekly_Epi_Update_136–1.pdf (2023).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 149 published 29 June 2023. file:///C:/Users/ASUS/Downloads/20230629_weekly_epi_update_149.pdf (2023).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 153 published 27 July 2023. file:///C:/Users/ASUS/Downloads/20230727_weekly_epi_update_153–1.pdf (2023).
World Health Organization. COVID-19 Weekly Epidemiological Update Edition 157 published 25 August 2023. file:///C:/Users/ASUS/Downloads/20230825_weekly_epi_update_157_edited-1.pdf (2023).
World Health Organization Thailand. Weekly situation update no. 255. https://cdn.who.int/media/docs/default-source/searo/thailand/2023_01_06_tha-sitrep-255-covid-19.pdf?sfvrsn=df4cb070_3 (2023).
World Health Organization Thailand. Weekly situation update no. 261. https://cdn.who.int/media/docs/default-source/searo/thailand/2023_04_11_tha-sitrep-261-covid-19.pdf?sfvrsn=550d95e8_1 (2023).
World Health Organization Thailand. Weekly situation update no. 263. https://cdn.who.int/media/docs/default-source/searo/thailand/2023_05_09_tha-sitrep-263-covid-19.pdf?sfvrsn=e94b525_1 (2023).
World Health Organization Thailand. Weekly situation update no. 265. https://cdn.who.int/media/docs/default-source/searo/thailand/2023_06_13_tha-sitrep-265-covid-19.pdf?sfvrsn=77ab97ea_1 (2023).
Korber, B. et al. Tracking changes in SARS-CoV-2 spike: evidence that D614G increases infectivity of the COVID-19 virus. Cell 182, 812-827.e19 (2020).
Liu, Y. et al. The N501Y spike substitution enhances SARS-CoV-2 infection and transmission. Nature 602, 294–299 (2022).
Motozono, C. et al. SARS-CoV-2 spike L452R variant evades cellular immunity and increases infectivity. Cell Host Microbe 29, 1124-1136.e11 (2021).
Cui, Z. et al. Structural and functional characterizations of infectivity and immune evasion of SARS-CoV-2 Omicron. Cell 185, 1–12 (2022).
Harvey, W. T. et al. SARS-CoV-2 variants, spike mutations and immune escape. Nat. Rev. Microbiol. 19, 409–424 (2021).
World Health Organization. XBB.1.16 Initial risk assessment. https://www.who.int/docs/default-source/coronaviruse/21042023xbb.1.16ra v2.pdf?sfvrsn=84577350_1 (2023).
Looi, M. K. What do we know about the Arcturus XBB.1.16 subvariant?. BMJ 381, 1074 (2023).
World Health Organization. Tracking SARS-CoV-2 variants. https://www.who.int/en/activities/tracking-SARS-CoV-2-variants (2023).
Buathong, R. et al. Multiple clades of SARS-CoV-2 were introduced to Thailand during the first quarter of 2020. Microbiol. Immunol. 65, 405–409 (2021).
Puenpa, J. et al. Molecular characterisation and tracking of severe acute respiratory syndrome coronavirus 2 in Thailand, 2020–2022. Arch. Virol. 168, 26 (2023).
Wannigama, D. L. et al. Tracing the new SARS-CoV-2 variant BA.2.86 in the community through wastewater surveillance in Bangkok Thailand. Lancet Infect. Dis. 23(11), e464–e466 (2023).
The Ministry of Public Health. COVID-19 Situation, Thailand. https://ddc.moph.go.th/covid19-dashboard/ (2023).
Elbe, S. & Buckland-Merrett, G. Data, disease and diplomacy: GISAID’s innovative contribution to global health. Glob. Chall. 1, 33–46 (2017).
Puenpa, J. et al. Investigation of the molecular epidemiology and evolution of circulating severe acute respiratory syndrome coronavirus 2 in Thailand from 2020 to 2022 via next-generation sequencing. Viruses 15, 1394 (2023).
World Health Organization. XBB.1.16 Updated Risk Assessment. (2023). https://www.who.int/docs/defaultsource/coronaviruse/05062023xbb.1.16.pdf?sfvrsn=f1845468_3 (2023).
Pung, R. et al. Severity of SARS-CoV-2 Omicron XBB subvariants in Singapore. Lancet. Reg. Health West Pac. 37, 100849 (2023).
Benvenuto, D. et al. The global spread of 2019-nCoV: A molecular evolutionary analysis. Pathog. Glob. Health 114, 64–67 (2020).
Tay, J. H., Porter, A. F., Wirth, W. & Duchene, S. The emergence of SARS-CoV-2 variants of concern is driven by acceleration of the substitution rate. Mol. Biol. Evol. 39(2), msac013 (2022).
Gräf, T. et al. Identification of a novel SARS-CoV-2 P.1 sub-lineage in Brazil provides new insights about the mechanisms of emergence of variants of concern. Virus Evol. 7(2), 091 (2021).
Scarpa, F. et al. (2023) Molecular in-depth on the epidemiological expansion of SARS-CoV-2 XBB.1.5. Microorganisms. 11(4), 912 (2023).
Scarpa, F. et al. Genome-based comparison between the recombinant SARS-CoV-2 XBB and its parental lineages. J. Med. Virol. 95, e28625 (2023).
Scarpa, F. et al. Integrative genome-based survey of the SARS-CoV-2 omicron XBB.1.16 variant. Int. J. Mol. Sci. 24, 13573 (2023).
Hall, T. A. BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucl. Acids Symp. S. 41, 95–98 (1999).
Katoh, K. & Standley, D. M. MAFFT multiple sequence alignment software version 7: improvements in performance and usability. Mol. Biol. Evol. 30, 772–780 (2013).
Suchard, M. A. et al. Bayesian phylogenetic and phylodynamic data integration using BEAST 1.10. Virus Evol. 1, 016 (2018).
Drummond, A. J., Ho, S. Y. W., Phillips, M. J. & Rambaut, A. Relaxed phylogenetics and dating with confidence. PLOS Biol. 4, e88 (2006).
Drummond, A. J., Rambaut, A., Shapiro, B. E. T. H. & Pybus, O. G. Bayesian coalescent inference of past population dynamics from molecular sequences. Mol. Biol. Evol. 22, 1185–1192 (2005).
Ayres, D. L. et al. BEAGLE: an application programming interface and high-performance computing library for statistical phylogenetics. Syst. Biol. 61, 170–173 (2012).
Rambaut, A., Drummond, A. J., Xie, D., Baele, G. & Suchard, M. A. Posterior summarization in Bayesian phylogenetics using Tracer 1.7. Syst. Biol. 67, 901 (2018).
Nguyen, L. T., Schmidt, H. A., von Haeseler, A. & Minh, B. Q. IQ-TREE: a fast and effective stochastic algorithm for estimating maximum-likelihood phylogenies. Mol. Biol. Evol. 32, 268–274 (2015).
Kalyaanamoorthy, S., Minh, B. Q., Wong, T. K. F., von Haeseler, A. & Jermiin, L. S. ModelFinder: fast model selection for accurate phylogenetic estimates. Nat. Methods 14, 587–589 (2017).
Rambaut, A., Lam, T. T., Max Carvalho, L. & Pybus, O. G. Exploring the temporal structure of heterochronous sequences using TempEst (formerly Path-O-Gen). Virus Evol. 2(1), vew007 (2016).
Acknowledgements
We thank all staff from the Center of Excellence in Clinical Virology, Faculty of Medicine, Chulalongkorn University, for their help with the laboratory testing.
Funding
This work was supported by the Health Systems Research Institute, the National Research Council of Thailand, the Center of Excellence in Clinical Virology, Chulalongkorn University, King Chulalongkorn Memorial Hospital, the MK Restaurant Group and Aunt Thongkam Foundation, and the BJC Big C Foundation. Jiratchaya Puenpa reports that financial support was also provided by the Second Century Fund Fellowship of Chulalongkorn University.
Author information
Authors and Affiliations
Contributions
J.P. drafted the manuscript; J.P., J.C., K.S. analyzed the data, prepared figures, and interpreted the results; J.P., J.C. collected specimens and data; J.P., J.C. performed the laboratory tests; K.S., Y.P. designed the study and revised the manuscript. All authors reviewed the manuscript, provided critical feedback, and approved the final draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Puenpa, J., Chansaenroj, J., Suwannakarn, K. et al. Genomic epidemiology and evolutionary analysis during XBB.1.16-predominant periods of SARS-CoV-2 omicron variant in Bangkok, Thailand: December 2022–August 2023. Sci Rep 14, 645 (2024). https://doi.org/10.1038/s41598-023-50856-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-50856-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.