Abstract
Hepatitis C virus (HCV) infection may cause chronic liver disease, liver cirrhosis, and liver cancer. It has been reported to associate with habits including alcohol, betel nut and cigarette use. We aimed to investigate the association between alcohol, betel nut, and cigarette use with HCV infection in Taiwan and to explore their effects. A total of 121,421 participants were enrolled from the Taiwan Biobank. They were stratified into two groups according to whether they had (n = 2750; 2.3%) or did not have (n = 118,671; 97.7%) HCV infection. All participants were also classified into four groups according to the number of habits, including a history of alcohol drinking, betel nut chewing, and cigarette smoking. There were 85,406 (no habit), 24,299 (one habit), 8659 (two habits), and 3057 (three habits) participants in the four groups, respectively. Multivariable analysis showed that the participants who had an alcohol drinking history (odds ratio [OR] 1.568; 95% confidence interval [CI] 1.388–1.773; p < 0.001), betel nut chewing history (OR 1.664; 95% CI 1.445–1.917; p < 0.001), cigarette smoking history (OR 1.387; 95% CI 1.254–1.535; p < 0.001), were significantly associated with HCV infection. Furthermore, the participants were classified into four groups according to the number of habits as follows: 85,406 (no habit), 24,299 (one habit), 8659 (two habits), and 3057 (three habits). The HCV infection rates in these four groups were 2.11%, 2.14%, 3.23%, and 4.78%, respectively. Compared to the participants with no or one habit, those with two habits had a higher HCV infection rate (all p < 0.001). In addition, compared to the participants who had no, one or two habits, those who had three habits also had higher HCV infection rates (all p < 0.001). The participants who had three habits had the highest prevalence of HCV infection. In an era when most HCV can be cured, understanding the epidemiology link between habits and HCV may help the case finding.
Similar content being viewed by others
Introduction
Taiwan has a high prevalence of hepatitis C virus (HCV) infection, with an estimated prevalence of 2.09% (95% CI, 1.60–2.77%) in the general population, which is higher than the global prevalence1. In 2020, the incidence of HCV infection was around 2.55 per 100,000 population in Taiwan2. The main risk factors for the transmission of HCV are intravenous drug use, blood transfusion, and sexual behavior3,4,5,6. HCV infection is a significant cause of hepatic fibrosis, cirrhosis, and hepatocellular carcinoma (HCC)7,8,9. In recent years, antiviral therapies for HCV infection have led to very high cure rates and few side effects10. Direct-acting antiviral agents for hepatitis C-related liver cirrhosis have proved to be an excellent treatment, with high tolerability and relatively low rates of serious adverse events11. In addition, attaining a treatment-related sustained virologic response among persons with HCV is associated with a reduction in the relative risk for HCC12. Therefore, identifying risk factors for HCV as early as possible is crucial to identify cases and for subsequent treatment.
Cigarette smoking, alcohol consumption, and betel nut chewing are common habits in Taiwan13,14,15. These behaviors may contribute to the development of oral cancer, esophageal cancer, stomach cancer, and liver cancer16,17,18,19. Moreover, a synergistic risk effect of these behaviors on oral cancer, esophageal cancer and HCC has been reported16,19,20. HCV infection is linked to blood exposure and injecting drug users, which were more common among cigarette smokers. Furthermore, a high proportion of cigarette smokers were habitual drinkers and betel nut chewers14,21,22. The use of these different substances was found to cluster. Previous studies have also reported that alcohol drinking, betel nut chewing, and cigarette smoking were independently associated with HCV infection23,24,25,26,27. However, the association between these three habits and HCV infection remains poorly defined.
Therefore, the aim of this study was to investigate the associations between alcohol drinking, betel nut chewing and cigarette smoking with HCV infection in around 120,000 participants in the Taiwan Biobank (TWB). We further investigated the effect between alcohol, betel nut and cigarette use on HCV infection.
Materials and methods
TWB
To enhance biomedical and epidemiological research in Taiwan, the TWB was launched by the government in 2012 as an ongoing prospective study of men and women aged 30–70 years recruited from approximately 30 centers around the country. Comprehensive genomic and phenotypic data are collected and recorded for each participant at enrollment and during follow-up visits through structured questionnaires, physical examinations, and urine and blood tests28,29. We used first enrolled data of TWB for further analysis. All participants in the TWB provided written informed consent before enrollment.
Demographic, lifestyle, laboratory and medical data
Information obtained through the TWB structured questionnaires included sex and age, and habits for alcohol drinking, betel nut chewing, and cigarette smoking. None of the enrollees in the TWB have a history of cancer. A history of other diseases such as diabetes mellitus (DM) and hypertension was recorded. Weight and height were measured during the physical examinations, and the body mass index (BMI; kg/m2) was recorded. In addition, analysis of the urine and blood samples provided data on: hemoglobin, fasting glucose, triglycerides, total cholesterol, uric acid, aspartate aminotransferase (AST), alanine aminotransferase (ALT) and estimated glomerular filtration rate (eGFR), calculated using the Modification of Diet in Renal Disease equation30. Chemiluminescence was used to test for anti-HCV antibodies (ADVIA Centaur, Siemens).
Assessment of alcohol drinking, betel nut chewing, and cigarette smoking history
The definitions of habits for alcohol drinking, betel nut chewing, and cigarette smoking history were as follows. For betel nut, those who had chewed ≥ 1 betel nut/per week for at least 1 year were defined as ever chewers, and those who had smoked ≥ 1 cigarette per day for at least 1 year were defined as ever smokers. For alcohol drinking, those who had consumed any alcoholic beverage > 4 times a week for at least 1 year were defined as ever drinkers.
The frequency of betel nut chewing in the ever chewers was recorded as follows: 1–3 days/month (1 point); 1–2 days/week (2 points); 3–5 days/week (3 points); 6–7 days (4 points). The daily amount of betel nut chewing was then recorded as follows: < 10 quids (1 point); 10–20 quids (2 points); 21–30 quids (3 points); ≥ 31 quids (4 points). Finally, the cumulative dose was calculated as: years of chewing betel nut × frequency score × daily amount score.
Study participants
Of 121,423 individuals in the TWB, 2 did not have data on HCV and were excluded. The remaining 121,421 individuals (males: 43,636; females: 77,785; mean age: 49.9 ± 11.0 years) were enrolled, and divided into two groups according to whether they had (n = 2750; 2.3%) or did not have (n = 118,671; 97.7%) HCV infection (Fig. 1).
Ethics statement
The study was conducted according to the Declaration of Helsinki, and it was granted approval by the Institutional Review Board of Kaohsiung Medical University Hospital (KMUHIRB-E(I)-20,210,058), and the TWB was granted approval by the IRB on Biomedical Science Research, Academia Sinica, Taiwan and the Ethics and Governance Council of the TWB.
Statistical analysis
Data are presented as n (%) or as mean ± SD. Continuous variables were compared using the independent t test, and categorical variables were compared using the chi-square test. Associations between alcohol drinking, betel nut chewing, cigarette smoking, and their characteristics with HCV infection were evaluated using multivariable logistic regression analysis. To avoid bias of demographic and characteristic differences between HCV (−) and HCV (+) groups, we further performed 1:10 matching using propensity score matching. In order to exclude the possibility that habit was associated with different sex and age group, we further performed subgroup analysis (male and female participants, and participants aged ≥ 50 and < 50 years). Besides, subgroup analysis of the associations between the number of habits and HCV infection were evaluated using multivariable logistic regression analysis. A p value of < 0.05 was considered to indicate a statistically significant difference. Statistical analysis was performed using SPSS version 26.0 for Windows (SPSS Inc., Armonk, NY, USA).
Ethics approval and consent to participate
The study was conducted according to the Declaration of Helsinki, and it was granted approval by the Institutional Review Board of Kaohsiung Medical University Hospital (KMUHIRB-E(I)-20,210,058), and the TWB was granted approval by the IRB on Biomedical Science Research, Academia Sinica, Taiwan and the Ethics and Governance Council of the TWB. All participants in the TWB provide written informed consent before enrollment.
Results
Comparisons of clinical characteristics between the with and without HCV groups
The group with HCV infection group were older and had more males than the without HCV infection group. In addition, those with HCV infection had higher rates of DM, hypertension, alcohol drinking, betel nut chewing, and cigarette smoking, lower rates of education higher than senior high schools, and higher levels of fasting glucose, hemoglobin, AST, ALT, and uric acid, and lower total cholesterol and eGFR than those without HCV infection (Table 1).
Determinants of HCV infection
The results of multivariable logistic regression analysis for the factors associated with HCV infection in the whole cohort (n = 121,421) are shown in Table 2. We performed five models to show the factors associated with HCV infection. Model 1: Adjusted alcohol drinking history and covariates of age, sex, diabetes, hypertension, fasting glucose, hemoglobin, total cholesterol, AST, ALT, eGFR and uric acid (significant variables in Table 1). Model 2: Adjusted betel nut chewing history and covariates. Model 3: Adjusted cigarette smoking history and covariates. Model 4: Adjusted alcohol drinking, betel nut chewing, and cigarette smoking history and covariates. Model 5: Interaction test was conducted by including multiplicative interaction terms in the multiple logistic regression model. After adjusting for age, sex, DM, hypertension, alcohol drinking, betel nut chewing, and cigarette smoking, education status, fasting glucose, hemoglobin, total cholesterol, AST, ALT, eGFR and uric acid (significant variables in Table 1), alcohol drinking history (odds ratio [OR] 1.568; 95% confidence interval [CI] 1.388–1.773; p < 0.001) in model 1, betel nut chewing history (OR 1.664; 95% CI 1.445–1.917; p < 0.001) in model 2, cigarette smoking history (OR 1.387; 95% CI 1.254–1.535; p < 0.001) in model 3 were significantly associated with HCV infection.
We then performed a sub-analysis of the determinants of HCV infection in the participants who chewed betel nut (n = 7355). Multivariable logistic regression analysis showed that a high cumulative dose (per 1 year × frequency × daily score; OR = 1.001; 95% CI 1.000–1.003; p = 0.042) was significantly associated with HCV infection.
Association of subgroup of habits combination associated with HCV infection
The results of multivariable logistic regression analysis for subgroup of habits combination associated with HCV infection in the whole cohort (n = 121,421) are shown in Table 3. After multiple adjustment, compared to the group of alcohol (−) betel nut (−) cigarette (−), the group of alcohol (−) betel nut (−) cigarette (+) (OR 1.212; 95% CI 1.077–1.365; p = 0.001), the group of alcohol (+) betel nut (+) cigarette (−) (OR 2.337; 95% CI 1.019–5.360; p = 0.045), the group of alcohol (+) betel nut (−) cigarette (+) (OR 1.770; 95% CI 1.473–2.127; p < 0.001), the group of alcohol (−) betel nut (+) cigarette (+) (OR 1.898; 95% CI 1.546–2.331; p < 0.001), and the group of alcohol (+) betel nut (+) cigarette (+) (OR 2.677; 95% CI 2.201–3.256; p < 0.001) were significantly associated with HCV infection.
We have further performed the synergy index. The synergy index was calculated as (odds ratio for Alcohol and Betel nut − 1) ÷ ([odds ratio for Alcohol or Betel nut] − 2). Synergy index (Alcohol and Betel nut) = \(\frac{1.988 - 1}{{\left( {1.237 + 1.397} \right) - 2}} =\) 1.56. The synergy index was calculated as (odds ratio for Alcohol and Cigarette − 1) ÷ ([odds ratio for Alcohol or Cigarette] − 2). Synergy index (Alcohol and Cigarette) = \(\frac{1.731 - 1}{{\left( {1.237 + 1.216} \right) - 2}} =\) 1.61. The synergy index was calculated as (odds ratio for Betel nut and Cigarette − 1) ÷ ([odds ratio for Betel nut or Cigarette] − 2). Synergy index (Betel nut and Cigarette) = \(\frac{1.685 - 1}{{\left( {1.397 + 1.216} \right) - 2}} =\) 1.12. The values of synergy index are all greater than 1. Our results revealed that alcohol drinking, betel nut chewing, and cigarette smoking history had an additive interaction associated with hepatitis C virus infection.
To avoid bias of demographic and characteristic differences between HCV (−) and HCV (+) groups, we have added 1:10 matching using propensity score matching (Table S1). Compared to the group of alcohol (−) betel nut (−) cigarette (−), the group of alcohol (+) betel nut (−) cigarette (+) (OR 1.426; 95% CI 1.191–1.707; p < 0.001), the group of alcohol (−) betel nut (+) cigarette (+) (OR 1.299; 95% CI 1.066–1.582; p = 0.009), and the group of alcohol (+) betel nut (+) cigarette (+) (OR 1.697; 95% CI 1.405–2.050; p < 0.001) were significantly associated with HCV infection (Table S2).
Association of the number of habits with HCV infection
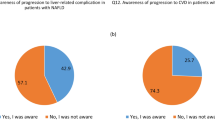
The participants were classified into four groups according to the number of habits as follows: 85,406 (no habit), 24,299 (one habit), 8659 (two habits), and 3057 (three habits). The HCV infection rates in these four groups were 2.11%, 2.14%, 3.23%, and 4.78%, respectively (Fig. 2). Compared to the participants who had no or one habit, those who had two habits had higher HCV infection rate (all p < 0.001). In addition, compared to the participants who had no, one or two habits, those who had three habits also had higher HCV infection rates (all p < 0.001). The participants who had three habits had the highest prevalence of HCV infection.
Subgroup analysis of the associations between the number of habits and HCV infection of different sex
Table 4 shows the subgroup analysis of associations between the number of habits and HCV infection using multivariable logistic regression analysis. The male participants (n = 42,636) who had two habits (vs. no habit; OR 1.599; 95% CI 1.338–1.911; p < 0.001), and three habits (vs. no habit; OR 2.313; 95% CI 1.870–2.862; p < 0.001) were significantly associated with HCV infection. However, the male participants had one habit was not (p = 0.068). The female participants (n = 77,785) who had one habit (vs. no habit; OR 1.312; 95% CI 1.120–1.535; p < 0.001), two habits (vs. no habit; OR 2.334; 95% CI 1.721–3.167; p < 0.001), and three habits (vs. no habit; OR 3.371; 95% CI 1.189–9.557; p < 0.001) were significantly associated with HCV infection.
Subgroup analysis of the associations between the number of habits and HCV infection of different age groups
Table 5 shows the subgroup analysis of associations between the number of habits and HCV infection of different age groups using multivariable logistic regression analysis. The participants aged ≥ 50 years (n = 64,818), and those who had two habits (vs. no habit; OR 2.143; 95% CI 1.670–2.749; p < 0.001), and three habits (vs. no habit; OR 3.452; 95% CI 2.518–4.732; p < 0.001) were also significantly associated with HCV infection. However, the participants aged ≥ 50 years had one habit was not (p = 0.156). In addition, the participants aged < 50 years (n = 56,603), and those who had one habit (vs. no habit; OR 1.439; 95% CI 1.201–1.724; p < 0.001), two habits (vs. no habit; OR 1.983; 95% CI 1.544–2.548; p < 0.001), and three habits (vs. no habit; OR 2.979; 95% CI 2.162–4.103; p < 0.001) were also significantly associated with HCV infection.
Discussion
In this study, we investigated the associations between HCV infection and its characteristics among 121,421 Taiwanese participants. The results showed that alcohol drinking, betel nut chewing, and cigarette smoking were significantly associated with HCV infection. Furthermore, the more habits had, the greater the rate of HCV infection. We also found an effect of alcohol, betel nut, and cigarette use on HCV infection.
The first important finding of this study is that alcohol drinking was associated with HCV infection. A previous cross-sectional study reported a highly significant correlation between self-reported alcohol consumption and serum HCV ribonucleic acid levels (r = 0.26, p < 0.0001), suggesting that greater alcohol consumption was associated with higher virus levels in the blood31. There are several potential mechanisms for this association. First, alcohol may impair cellular immunity and inhibit the efficacy of antiviral therapy32. Thus, impaired immune function may contribute to the ability of the virus to enter and remain inside the body rather than be eliminated by immune cells. The second mechanism may be due to oxidative stress. Larrea et al. reported that HCV infection itself can lead to oxidative stress, which induces viral genome heterogeneity and influences HCV propagation in the organism33. The mechanism of oxidative stress facilitates viral escape during treatment34, and escape from the immune system35. Alcohol is metabolized predominantly in the liver and can generate free radicals that contribute to oxidative stress, which may aggravate this virus-induced oxidative stress36. Therefore, impaired immune function and oxidative stress may play important roles in the association between alcohol drinking and HCV infection. Furthermore, Charles et al. found that people with alcohol abuse disorder had higher rates of HCV infection than controls, even in those with no other classical risk factors for HCV infection such as intravenous drug abuse or blood transfusions37. Taken together, we suggest that excessive alcohol consumption may increase the risk of acquiring HCV.
The second important finding of this study is that betel nut chewing was associated with HCV infection. We further analyzed the frequency, daily amount, and cumulative dose of betel nut chewing, and found that a high cumulative dose was correlated with HCV infection. A community-based study conducted in central Taiwan was the first to show that betel nut chewing was an independent risk factor for HCV infection, with an adjusted OR of 9.1225. Other studies have found that the habit of betel nut chewing was an independent risk factor for HCC, and that an increased risk of HCC was associated with seropositivity for anti-HCV in Taiwan38,39. Taken together, these findings indirectly support that betel nut chewing is an independent risk factor for anti-HCV25. Further investigations are needed to elucidate the precise mechanism underlying the association between betel nut chewing and HCV infection.
Another interesting finding of this study is that cigarette smoking was associated with HCV infection. Kim et al. reported that the prevalence of smoking in individuals with HCV infection was nearly three times higher than in individuals without HCV infection (62.4% vs. 22.9%, p < 0.001) in the United States from 1999 to 2014, and that heroin use was more common in individuals with HCV infection who smoked than in individuals without HCV infection who smoked22. In addition, Chen et al. founded that the prevalence of illicit drug use ranged from 0.3% among those using no other substance to 7.1% among those using tobacco, betel quid, and alcohol among 13-to 35-year-old persons in I-Lan County, a rural area of Taiwan, supporting that tobacco smoking may have a large effect on illicit drug use21. Heroin users are more likely to smoke. A possible explanation is that HCV infection is linked to blood exposure, and injection drug use may increase the risk of acquiring HCV. The association between smoking and HCV may be because of the higher rate of heroin use in smokers. Another population-based study reported an association between the initiation and intensity of habits and the number of sexual partners, and suggested that the severity of alcohol and cigarette use was an indicator of a higher number of sexual partners40. The risk of sexually transmitted diseases and hepatitis B or C virus infection increases as the number of sexual partners increases41. In addition, Chuang et al. proposed a synergistic effect between smoking and hepatitis B or C virus infection on the risk of HCC27. Therefore, further investigations are needed to study the influence of cigarette smoking on HCV infection.
Lastly, we found that the more habit had, the greater the rate of HCV infection, and that there was an effect of alcohol, betel nut, and cigarette use on HCV infection. The prevalence of males and older age was significantly higher in the participants with HCV infection. To exclude the possibility that habit was associated with these groups, we further performed subgroup analysis of female participants and participants aged < 50 years, and found similar results of an effect of alcohol, betel nut and cigarette use on HCV infection. Prior studies have identified the synergistic risk effects of alcohol drinking, tobacco smoking and betel nut chewing on various cancers. Ko et al. reported that betel quid chewing, cigarette smoking and alcohol consumption were significantly related to oral cancer, which they suggested could be due to the carcinogenicity of alcoholic beverages, tobacco smoke and betel quid, with target organs including the oral cavity, pharynx, larynx and esophagus16. Wu et al. reported an interaction between these three habits on the risk of esophageal cancer in Taiwan, and suggested that betel nut plays a role in adding to the carcinogenetic effect of cigarette smoke and alcohol20. In addition, Wang et al. suggested that there are combined effects of habitual alcohol drinking, betel quid chewing and cigarette smoking on an increased risk of HCC19. Cigarette smoke contains several chemicals that are metabolized and activated as carcinogens in the liver42. Alcohol is a hepatotoxin which accelerates fibrosis progression and increases the risk of cirrhosis, a primary clinical predictor of HCC43,44,45. The mechanism underlying the association between betel nut chewing and HCC may also be related to safrole, which may be the reactive agent responsible for hepatocarcinogenesis46.
At present, alcohol drinking, betel nut chewing, and cigarette smoking history independently predicts HCV in Table 2, but it is not easy to distinguish whether independent influence is indeed on HCV. To avoid Table 2 fallacy47, we performed further analysis of 8 subgroups of habits combination (Table 3) to clarify that he effect of habit combinations on the association with HCV appears consistent with the results in Fig. 2 that the group of alcohol (+) betel nut (+) cigarette (+) being the highest. When any two habit factors co-exist, statistically significant effect are retained to associate with HCV. Therefore, the results revealed that the three factors do jointly affect the risk of HCV. The group of alcohol (+) betel nut (−) cigarette (−), and the group of alcohol (−) betel nut (+) cigarette (−) did not have a significant association but with a trend with HCV (Table 3). It could be caused by the number of the two groups is relatively small.
This work is the first study to show the association between alcohol, betel nut, and cigarette on the risk of HCV infection, as they were independent risk factors for HCV infection. Ko et al. reported that a high proportion of betel nut chewers in Taiwan were also habitual smokers and drinkers14. The current investigation also indicated that smoking and alcohol drinking were also independently associated with the progression of HCV infection23,27. In addition, we found evidence of the combined effects of chronic hepatitis virus infection and habits on chronic liver disease, and that there was a biological gradient in the risk of developing chronic liver disease, with multivariable-adjusted ORs of 4.7 and 7.9 for subjects who had 1–2 and 3 habits, respectively, compared to those who did not have the habit48. Betel nut chewing was recently found to be associated with HCC, esophageal cancer and gastric cancer in Taiwan39,49,50, and HCV infection has been considered as an important cause of advanced hepatic fibrosis and cirrhosis, with a significantly increased risk of developing HCC51. Thus, taken together, these findings suggest that lifestyle factors such as alcohol consumption, cigarette smoking and betel nut chewing are related to liver damage and indirectly support our findings that these three habits has effects on HCV infection. Further studies are necessary to investigate the exact mechanism by which betel nut chewing increases the risk of HCV infection in drinkers and smokers.
Our findings are strengthened by the inclusion of a large number of healthy participants enrolled from a national biobank, and controlling for confounding factors including alcohol, betel nut and cigarette use in our analyses. Nevertheless, several limitations should also be mentioned. First, as this was a cross-sectional study, it was not possible to determine the duration of HCV infection, and consequently causal relationships could not be established. Longitudinal studies are needed to clarify the association between habits and HCV infection. Second, the genotype and severity of HCV infection could not be ascertained. Third, some data associated with HCV infection was lacking, such as socioeconomic status of participants, which may influence HCV infection rate. Fourth, the alcohol history, betel nut chewing history, and smoking history were collected by questionnaire, which may result in the possibility of misclassification, and then lead to wrong analysis results. Besides, the participants of TWB may not represent the general population in Taiwan, which may result in selection bias, and then lead to underestimated or overestimated the OR. Finally, our findings may be limited by the single ethnicity of the enrolled participants. Further studies on other ethnic groups are warranted.
In conclusion, this study suggests the association between HCV infection and alcohol drinking, betel quid chewing, and cigarette smoking. Cessation programs for habits are important to prevent chronic HCV infection in Taiwan.
Data availability
The data underlying this study are from the Taiwan Biobank Database. Due to restrictions placed on the data by the Personal Information Protection Act of Taiwan, the minimal data set cannot be made publicly available. Data may be available upon request to interested researchers. Please send data requests to: Szu-Chia Chen, PhD, MD. Division of Nephrology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University.
References
Chen, G. J. et al. Hepatitis C microelimination among people living with HIV in Taiwan. Emerg. Microb. Infect. 11, 1664–1671. https://doi.org/10.1080/22221751.2022.2081620 (2022).
Centers for Disease Control, M. o. H. a. W., R.O.C.(Taiwan). Statistics of Communicable Diseases and Surveillance Report 2020.
Nelson, P. K. et al. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: Results of systematic reviews. Lancet 378, 571–583. https://doi.org/10.1016/S0140-6736(11)61097-0 (2011).
Alter, H. J. et al. Detection of antibody to hepatitis C virus in prospectively followed transfusion recipients with acute and chronic non-A, non-B hepatitis. N. Engl. J. Med. 321, 1494–1500. https://doi.org/10.1056/NEJM198911303212202 (1989).
Tohme, R. A. & Holmberg, S. D. Is sexual contact a major mode of hepatitis C virus transmission?. Hepatology 52, 1497–1505. https://doi.org/10.1002/hep.23808 (2010).
Lissen, E. et al. Hepatitis C virus infection among sexually promiscuous groups and the heterosexual partners of hepatitis C virus infected index cases. Eur. J. Clin. Microbiol. Infect. Dis. 12, 827–831. https://doi.org/10.1007/BF02000402 (1993).
Khatun, M. & Ray, R. B. Mechanisms underlying hepatitis C virus-associated hepatic fibrosis. Cells https://doi.org/10.3390/cells8101249 (2019).
Khullar, V. & Firpi, R. J. Hepatitis C cirrhosis: New perspectives for diagnosis and treatment. World J. Hepatol. 7, 1843–1855. https://doi.org/10.4254/wjh.v7.i14.1843 (2015).
Goto, K., Roca Suarez, A. A., Wrensch, F., Baumert, T. F. & Lupberger, J. Hepatitis C virus and hepatocellular carcinoma: When the host loses its grip. Int. J. Mol. Sci. https://doi.org/10.3390/ijms21093057 (2020).
Manns, M. P. et al. Hepatitis C virus infection. Nat. Rev. Dis. Prim. 3, 17006. https://doi.org/10.1038/nrdp.2017.6 (2017).
Toshikuni, N. Therapy with direct-acting antiviral agents for hepatitis C-related liver cirrhosis. Gut Liver 11, 335–348. https://doi.org/10.5009/gnl15458 (2017).
Morgan, R. L. et al. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: A meta-analysis of observational studies. Ann. Intern. Med. 158, 329–337. https://doi.org/10.7326/0003-4819-158-5-201303050-00005 (2013).
Liang, W. M., Kuo, H. W. & Wang, C. B. Prevalence of Tobacco Smoking, Drinking and Betel Nut Chewing Among Taiwanese Workers in 1999, https://www.airitilibrary.com/Publication/alDetailedMesh?DocID=10293507-200209-7-3-146-154-a. (2002).
Ko, Y. C., Chiang, T. A., Chang, S. J. & Hsieh, S. F. Prevalence of betel quid chewing habit in Taiwan and related sociodemographic factors. J. Oral Pathol. Med. 21, 261–264. https://doi.org/10.1111/j.1600-0714.1992.tb01007.x (1992).
National Health Research Institutes & Health Promotion Administration, Ministry of Health and Welfare. National Health Interview Survey in 2013.
Ko, Y. C. et al. Betel quid chewing, cigarette smoking and alcohol consumption related to oral cancer in Taiwan. J. Oral Pathol Med. 24, 450–453. https://doi.org/10.1111/j.1600-0714.1995.tb01132.x (1995).
Chung, C. S. et al. Secondary prevention of esophageal squamous cell carcinoma in areas where smoking, alcohol, and betel quid chewing are prevalent. J. Formos. Med. Assoc. 109, 408–421. https://doi.org/10.1016/S0929-6646(10)60072-1 (2010).
Chuang, Y. S. et al. Effects of alcohol consumption, cigarette smoking, and betel quid chewing on upper digestive diseases: A large cross-sectional study and meta-analysis. Oncotarget 8, 78011–78022. https://doi.org/10.18632/oncotarget.20831 (2017).
Wang, L. Y. et al. Risk of hepatocellular carcinoma and habits of alcohol drinking, betel quid chewing and cigarette smoking: A cohort of 2416 HBsAg-seropositive and 9421 HBsAg-seronegative male residents in Taiwan. Cancer Causes Control 14, 241–250. https://doi.org/10.1023/a:1023636619477 (2003).
Wu, I. C. et al. Interaction between cigarette, alcohol and betel nut use on esophageal cancer risk in Taiwan. Eur. J. Clin. Invest. 36, 236–241. https://doi.org/10.1111/j.1365-2362.2006.01621.x (2006).
Chen, K. T., Chen, C. J., Fagot-Campagna, A. & Narayan, K. M. Tobacco, betel quid, alcohol, and illicit drug use among 13–35-year-olds in I-Lan, rural Taiwan: Prevalence and risk factors. Am. J. Public Health 91, 1130–1134. https://doi.org/10.2105/ajph.91.7.1130 (2001).
Kim, R. S. et al. Cigarette smoking in persons living with hepatitis C: The national health and nutrition examination survey (NHANES), 1999–2014. Am. J. Med. 131, 669–675. https://doi.org/10.1016/j.amjmed.2018.01.011 (2018).
Hutchinson, S. J., Bird, S. M. & Goldberg, D. J. Influence of alcohol on the progression of hepatitis C virus infection: A meta-analysis. Clin. Gastroenterol. Hepatol. 3, 1150–1159. https://doi.org/10.1016/s1542-3565(05)00407-6 (2005).
Corrao, G. & Arico, S. Independent and combined action of hepatitis C virus infection and alcohol consumption on the risk of symptomatic liver cirrhosis. Hepatology 27, 914–919. https://doi.org/10.1002/hep.510270404 (1998).
Lin, C. H., Lin, C. C. & Liu, C. S. Betel nut chewing as a risk factor for hepatitis C infection in Taiwan: A community-based study. Ann. Saudi Med. 31, 204–205. https://doi.org/10.4103/0256-4947.78211 (2011).
Pessione, F. et al. Cigarette smoking and hepatic lesions in patients with chronic hepatitis C. Hepatology 34, 121–125. https://doi.org/10.1053/jhep.2001.25385 (2001).
Chuang, S. C. et al. Interaction between cigarette smoking and hepatitis B and C virus infection on the risk of liver cancer: A meta-analysis. Cancer Epidemiol. Biomark. Prev. 19, 1261–1268. https://doi.org/10.1158/1055-9965.EPI-09-1297 (2010).
Chen, C. H. et al. Population structure of Han Chinese in the modern Taiwanese population based on 10,000 participants in the Taiwan Biobank project. Hum. Mol. Genet. 25, 5321–5331. https://doi.org/10.1093/hmg/ddw346 (2016).
Fan, C. T., Hung, T. H. & Yeh, C. K. Taiwan regulation of biobanks. J. Law Med. Eth. 43, 816–826. https://doi.org/10.1111/jlme.12322 (2015).
Levey, A. S. et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann. Intern. Med. 130, 461–470. https://doi.org/10.7326/0003-4819-130-6-199903160-00002 (1999).
Pessione, F. et al. Effect of alcohol consumption on serum hepatitis C virus RNA and histological lesions in chronic hepatitis C. Hepatology 27, 1717–1722. https://doi.org/10.1002/hep.510270635 (1998).
Ince, N. & Wands, J. R. The increasing incidence of hepatocellular carcinoma. N. Engl. J. Med. 340, 798–799. https://doi.org/10.1056/NEJM199903113401009 (1999).
Larrea, E., Beloqui, O., Munoz-Navas, M. A., Civeira, M. P. & Prieto, J. Superoxide dismutase in patients with chronic hepatitis C virus infection. Free Radic. Biol. Med. 24, 1235–1241. https://doi.org/10.1016/s0891-5849(97)00437-1 (1998).
Seronello, S. et al. Ethanol and reactive species increase basal sequence heterogeneity of hepatitis C virus and produce variants with reduced susceptibility to antivirals. PLoS One 6, e27436. https://doi.org/10.1371/journal.pone.0027436 (2011).
Forns, X., Purcell, R. H. & Bukh, J. Quasispecies in viral persistence and pathogenesis of hepatitis C virus. Trends Microbiol. 7, 402–410. https://doi.org/10.1016/s0966-842x(99)01590-5 (1999).
Lieber, C. S. Role of oxidative stress and antioxidant therapy in alcoholic and nonalcoholic liver diseases. Adv. Pharmacol. 38, 601–628. https://doi.org/10.1016/s1054-3589(08)61001-7 (1997).
Lieber, C. S. Alcohol and hepatitis C. Alcohol. Res. Health 25, 245–254 (2001).
Tsai, J. F. et al. Betel quid chewing as a risk factor for hepatocellular carcinoma: A case-control study. Br. J. Cancer 84, 709–713. https://doi.org/10.1054/bjoc.1999.1597 (2001).
Tsai, J. F. et al. Habitual betel quid chewing and risk for hepatocellular carcinoma complicating cirrhosis. Medicine (Baltimore) 83, 176–187. https://doi.org/10.1097/01.md.0000126971.80227.a4 (2004).
Cavazos-Rehg, P. A. et al. Number of sexual partners and associations with initiation and intensity of substance use. AIDS Behav. 15, 869–874. https://doi.org/10.1007/s10461-010-9669-0 (2011).
Rich, J. D., Anderson, B. J., Schwartzapfel, B. & Stein, M. D. Sexual risk for hepatitis B virus infection among hepatitis C virus-negative heroin and cocaine users. Epidemiol. Infect. 134, 478–484. https://doi.org/10.1017/S0950268805005248 (2006).
Hoffmann, D., Rivenson, A., Chung, F. L. & Wynder, E. L. Potential inhibitors of tobacco carcinogenesis. Ann. N. Y. Acad. Sci. 686, 140–160. https://doi.org/10.1111/j.1749-6632.1993.tb39169.x (1993).
Yu, M. C., Tong, M. J., Govindarajan, S. & Henderson, B. E. Nonviral risk factors for hepatocellular carcinoma in a low-risk population, the non-Asians of Los Angeles County, California. J. Natl. Cancer Inst. 83, 1820–1826. https://doi.org/10.1093/jnci/83.24.1820 (1991).
Donato, F. et al. Hepatitis B and C virus infection, alcohol drinking, and hepatocellular carcinoma: A case-control study in Italy. Brescia HCC Study. Hepatology 26, 579–584. https://doi.org/10.1002/hep.510260308 (1997).
Kuper, H. et al. Tobacco smoking, alcohol consumption and their interaction in the causation of hepatocellular carcinoma. Int. J. Cancer 85, 498–502 (2000).
Liu, C. J., Chen, C. L., Chang, K. W., Chu, C. H. & Liu, T. Y. Safrole in betel quid may be a risk factor for hepatocellular carcinoma: Case report. CMAJ 162, 359–360 (2000).
Westreich, D. & Greenland, S. The table 2 fallacy: Presenting and interpreting confounder and modifier coefficients. Am. J. Epidemiol. 177, 292–298. https://doi.org/10.1093/aje/kws412 (2013).
Lin, H. H. et al. Combined effects of chronic hepatitis virus infections and substance-use habits on chronic liver diseases in Taiwanese aborigines. J. Formos. Med. Assoc. 101, 826–834 (2002).
Wu, M. T. et al. Risk of betel chewing for oesophageal cancer in Taiwan. Br. J. Cancer 85, 658–660. https://doi.org/10.1054/bjoc.2001.1927 (2001).
Wu, M. T., Chen, M. C. & Wu, D. C. Influences of lifestyle habits and p53 codon 72 and p21 codon 31 polymorphisms on gastric cancer risk in Taiwan. Cancer Lett. 205, 61–68. https://doi.org/10.1016/j.canlet.2003.11.026 (2004).
Axley, P., Ahmed, Z., Ravi, S. & Singal, A. K. Hepatitis C virus and hepatocellular carcinoma: A narrative review. J. Clin. Transl. Hepatol. 6, 79–84. https://doi.org/10.14218/JCTH.2017.00067 (2018).
Funding
This work was supported partially by the Research Center for Precision Environmental Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan and by Kaohsiung Medical University Research Center Grant (KMU-TC111A01 and KMUTC111IFSP01).
Author information
Authors and Affiliations
Contributions
Conceptualization, methodology, validation, formal analysis, writing—review and editing, and supervision: S.-C.C. and P.-L.L. Software and investigation: S.-C.C. Resources, project administration, and funding acquisition: S.-C.C. Data curation: Y.-A.T., Y.-L.O., J.-H.G., C.-W.W., D.-W.W., S.-C.C. and P.-L.L. Writing—original draft preparation: Y.-A.T. and Y.-L.O. Visualization: Y.-A.T., Y.-L.O., J.-H.G., C.-W.W., D.-W.W., S.-C.C. and P.-L.L. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tseng, YA., Ou, YL., Geng, JH. et al. The association between alcohol, betel nut, and cigarette use with hepatitis C virus infection in Taiwan. Sci Rep 13, 23082 (2023). https://doi.org/10.1038/s41598-023-50588-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-50588-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.