Abstract
A complete blood count (CBC) is routinely ordered for emergency department (ED) patients with infections. Certain parameters, such as the neutrophil-to-lymphocyte ratio (NLR), might have prognostic value. We aimed to evaluate the prognostic value of the presenting CBC parameters combined with clinical variables in predicting 30-day mortality in adult ED patients with infections using an artificial neural network (ANN). We conducted a retrospective study of ED patients with infections between 17 December 2021 and 16 February 2022. Clinical variables and CBC parameters were collected from patient records, with NLR, monocyte-to-lymphocyte ratio (MLR), and platelet-to-lymphocyte ratio (PLR) calculated. We determined the discriminatory performance using the area under the receiver operating characteristic curve (AUROC) and performed a 70/30 random data split and supervised ANN machine learning. We analyzed 558 patients, of whom 144 (25.8%) had sepsis and 60 (10.8%) died at 30 days. The AUROCs of NLR, MLR, PLR, and their sum were 0.644 (95% CI 0.573–0.716), 0.555 (95% CI 0.482–0.628), 0.606 (95% CI 0.529–0.682), and 0.610 (95% CI 0.534–0.686), respectively. The ANN model based on twelve variables including clinical variables, hemoglobin, red cell distribution width, NLR, and PLR achieved an AUROC of 0.811 in the testing dataset.
Similar content being viewed by others
Introduction
Sepsis is a global health burden. In 2017, an estimated 48.9 million cases and 11 million related deaths occurred worldwide, with 85% of the cases in low- or middle-income countries1. Identifying sepsis and patients who are at risk of deterioration early in the emergency department (ED) is essential for prompt intervention to prevent morbidity and mortality. The quick Sequential Organ Failure Assessment (qSOFA) score is used in many non-intensive care settings to identify high-risk patients with infections. A meta-analysis showed that it has a high pooled specificity of 83%, but its pooled sensitivity was only 51% in predicting in-hospital mortality2. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) recommend to identify organ dysfunction in septic patients by an acute change in the Sequential Organ Failure Assessment (SOFA) score of ≥ 23. However, based on the worst values within 48 h of admission and a cutoff score of > 9, the sensitivity and specificity for in-hospital mortality were only 65.8% and 75.5%, respectively4. A more reliable, fast, and affordable method is needed to identify at-risk septic patients in the ED.
The complete blood count (CBC) contains important information on the hematological system whose value in sepsis prognostication might have been overlooked5. The CBC has multiple potential advantages in identifying sepsis and predicting mortality: a low cost that enables its wider adoption in resource-poor settings, a shorter turnaround time than liver and renal function tests to support early clinical decisions, and good availability since it is often done as a routine workup for hospitalized patients. In daily practice, clinicians use elevated white blood cell (WBC) counts to gauge the severity of infection and platelet count to calculate the SOFA score. However, the CBC has not been routinely used in the ED as an objective tool in sepsis prognostication.
Previous studies have demonstrated the prognostic value of several CBC parameters in sepsis. The initial hemoglobin level on ED admission is associated with 90-day mortality6, and hematocrit in the first 24 h in the intensive care unit (ICU) is associated with increased 30-day mortality7. Increased baseline red cell distribution width (RDW), an erythrocyte index reflecting the heterogeneity in the size of circulating erythrocytes, is associated with sepsis mortality8. The lowest platelet count in the first 72 h after ICU admission is significantly lower in septic non-survivors9. Meta-analyses have shown that the neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) are significantly higher in septic non-survivors10,11. In surgical ICU settings, combining mean platelet volume to platelet count ratio (MPV/PC), NLR, monocyte-to-lymphocyte ratio (MLR), and PLR significantly improved mortality prediction12. A scoring system based on RDW, delta neutrophil index (DNI), and MPV/PC has been shown to be more useful than platelet count alone in predicting sepsis mortality13.
Literature combining patient characteristics, clinical variables, and CBC parameters in sepsis prognostication is scarce. The complex relations between these factors may require non-linear data modeling in prognostication and machine learning methods, such as artificial neural networks (ANNs). However, the use of ANNs in sepsis prognostication based on these parameters has not been evaluated. The objectives of this study were to (1) compare the patient characteristics, triage vital signs, and CBC parameters of adult ED patients with infections who did and did not survive up to 30 days and (2) evaluate the prognostic value of CBC parameters combined with patient characteristics and triage vital signs in predicting 30-day all-cause mortality for such patients using an ANN.
Methods
Study design
This was a retrospective observational study of consecutive adult patients presenting to the ED of Queen Mary Hospital (QMH) with an infection over 3 months from 17 December 2021 to 16 February 2022. QMH is a university-affiliated tertiary hospital in Hong Kong with 1,700 beds and an annual ED attendance of 100,000.
The study was approved by the Institutional Review Board of The University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB; reference number: HKWC-2023-452) and conducted in full compliance with the Declaration of Helsinki and local research ethics guidelines. Informed consent was waived by the HKU/HKW IRB because this was a retrospective study and patients remained anonymous during the data analysis. We followed the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines14 and Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD) guidelines15 in reporting the findings of this study.
Study population
All patients who were aged ≥ 18 years and presented to the QMH ED with a clinical diagnosis of infection during the study period were recruited. All clinical diagnoses and decisions on laboratory tests, including CBCs, were made by the treating clinical teams. For patients with more than one ED attendance for infections within the study period, only the first ED presentation was included as the index presentation to avoid duplication.
The exclusion criteria were (1) patients who did not have a CBC collected within 48 h of ED presentation; (2) patients younger than 18 years old because of different normal ranges of CBC parameters in children and adults16; (3) patients who were subsequently diagnosed with conditions other than an infection after hospital workup; (4) patients with pre-existing hematological malignancies or myeloproliferative disorders because these conditions affect CBC cell counts17; (5) patients who had received chemotherapy in the past 12 months, which might also affect the cell counts; and (6) patients who had received blood product transfusions in the previous 2 weeks.
Data collection
We collected the following data: (1) patient characteristics, including age, sex, old age home resident status, and Charlson Comorbidity Index (CCI); (2) ED triage vital signs, including temperature, systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), pulse rate, respiratory rate (RR), and oxygen saturation (SpO2); (3) pathogens and organ systems involved in infection, by reviewing the results of microbiology tests on patients’ blood, sputum, urine, and other specimens; (4) complications, including organ dysfunction; and (5) clinical outcomes, including ICU admission and 2-, 7-, 30-, and 90-day mortality.
We extracted nine CBC parameters at presentation, comprising the total WBC, neutrophil, lymphocyte, monocyte, basophil, and platelet counts, hemoglobin, hematocrit, and RDW, and calculated the NLR, MLR, and PLR accordingly. We calculated the SOFA score based on the worst clinical and laboratory parameters within 48 h of ED presentation18. For patients with missing partial pressure of arterial oxygen (PaO2) data, we determined the respiratory component of the SOFA score based on the method described by Grissom et al.19 that replaces PaO2 with SpO2.
The data were collected by reviewing the electronic medical records in the Clinical Management System (CMS) of the Hospital Authority (HA). The HA CMS is a central repository of all clinical records of patients attending public EDs and hospitals. It is also connected to the central death records in Hong Kong; therefore, the chance of missing mortality was very low. We reviewed the whole clinical course of each case from ED presentation to hospital discharge or death. All data was collected by trained research personnel using a standardized data collection spreadsheet and cross-checked by the first two authors.
Patient outcome
The primary outcome was 30-day all-cause mortality.
Statistical analysis
A sample size was not calculated because of the lack of similar studies to guide such a calculation. Missing data on vital signs were imputed using the vital signs documented on hospital admission, if available. We did not impute missing laboratory or outcome data.
The distribution of characteristics of the study population was analyzed using descriptive statistics, with categorical variables reported as numbers and proportions and continuous variables as mean +/− standard deviation (SD) or medians with interquartile ranges (IQR), as appropriate. We then conducted univariate analysis, with the distribution of categorical variables compared between 30-day survivors and non-survivors using Pearson’s chi-squared (χ2) test or Fisher’s exact test and continuous variables with Student’s t-test or the Mann–Whitney U test, as appropriate. The discriminatory performance of the NLR, MLR, and PLR in predicting the primary outcome was evaluated using the area under the receiver operating characteristic curve (AUROC). Using the approach of Djordjevic et al., we further evaluated the prognostic performance of the sum of NLR, MLR, and PLR to determine whether the sum would surpass the individual ratios alone12.
We then performed supervised machine learning using an ANN model with a multi-layer perceptron. The dataset was randomly split in a 70/30 ratio into a training set and a testing set. The following 12 variables were input into the model to predict the primary outcome: patient age, sex, old age home resident status, CCI, triage MAP, pulse rate, RR, SpO2, hemoglobin level, RDW, NLR, and PLR from the first CBC taken after the ED presentation, since they were significantly associated with 30-day mortality in univariate analyses. We did not input hematocrit, total WBC, neutrophil, and lymphocyte counts into the model to avoid redundancy, although they were also significantly associated with 30-day mortality in univariate analyses. All continuous variables were normalized before being entered into the model. The ANN was built with one hidden layer and seven hidden nodes and was trained using backpropagation with gradient descent. The trained ANN model was then applied to the testing dataset to evaluate its discriminatory performance. We determined the accuracy and the AUROC of the derived ANN model in the testing set.
All data were analyzed with SPSS for Windows version 27.0 (IBM Corp., Armonk, NY, USA). Statistical significance was defined as a two-sided p-value of < 0.05.
Results
Patient characteristics
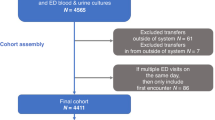
A total of 1158 adult patients met the initial screening criteria, but 501 were excluded because they did not have a CBC collected within 48 h of ED presentation, four were excluded because they were subsequently found to have a diagnosis other than an infection, 24 were excluded because of pre-existing hematological malignancies, 17 were excluded due to pre-existing hematological disorders (including four with pre-existing thrombocytopenia), and 54 were excluded because they had received chemotherapy in the past 12 months. In total, 558 patients were included and analyzed. The patient flow diagram is shown in Fig. 1.
Table 1 summarizes the patient demographic and clinical characteristics. The median age of the patients was 79.0 years (IQR 65.0–89.3), with males accounting for 49.1% and females accounting for 50.9%. The median CCI was 2 (IQR 0–3); of the 15 comorbidities included, dementia was the most common (n = 150, 26.9%), followed by diabetes mellitus with end organ damage (n = 149, 26.7%) and cerebrovascular accident or transient ischemic attack (n = 126, 22.6%). Concerning the infection, the respiratory system was the most frequently involved (n = 180, 32.3%), followed by the genitourinary system (n = 98, 17.6%) and the gastrointestinal system or intra-abdominal infections (n = 92, 16.5%). Regarding the pathogens, gram-negative bacteria were the most commonly found in bacterial cultures (n = 103, 18.5%), followed by mixed-organism infections (n = 99, 17.7%) and gram-positive bacteria (n = 43, 7.7%). Sixteen patients had COVID-19 (2.9%).
Based on the Sepsis-3 definition of sepsis, 144 (25.8%) of the patients had organ dysfunction, characterized by an increase in SOFA of ≥ 2 during the index acute hospital stay. Seven patients were admitted to the ICU. The 2- and 7-day mortality rates were 1.4% and 3.0%, respectively; 60 patients (10.8%) died by 30 days, and 113 patients (20.3%) died by 90 days.
Comparing survivors vs. non-survivors at 30 days
We compared the patient demographics, clinical characteristics, and CBC parameters between the 498 survivors and 60 non-survivors by 30 days (Table 2). The non-survivors were significantly older (median age 89.0 vs. 77.0 years, p < 0.001) and more likely to be men (p = 0.039). A significantly higher proportion of non-survivors were old age home residents (p < 0.001) and had a higher CCI (p < 0.001). Non-survivors also had a significantly higher triage RR (p < 0.001), a lower SpO2 (p < 0.001), a lower MAP (p = 0.046), and a higher pulse rate (p = 0.045). Among all CBC parameters, the presenting hemoglobin level, hematocrit, RDW, total white cell, neutrophil, and lymphocyte counts differed significantly between survivors and non-survivors. Non-survivors had a significantly higher NLR (p = 0.001) and PLR (p = 0.007). Organ dysfunction was more common in non-survivors, whose worst SOFA score within 48 h of admission was significantly higher (median 2 vs. 0, p < 0.001). Table 3 shows the distribution of individual organ dysfunction among survivors and non-survivours.
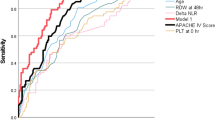
Discriminatory values of NLR, MLR, PLR, and their combination in predicting 30-day all-cause mortality
In predicting 30-day all-cause mortality, the AUROCs of NLR, MLR, and PLR were 0.644 (95% confidence interval [CI] 0.573–0.716), 0.555 (95% CI 0.482–0.628), and 0.606 (95% CI 0.529–0.682), respectively. The AUROC of the sum of NLR, MLR, and PLR in predicting 30-day all-cause mortality was modest (0.610, 95% CI 0.534–0.686; Fig. 2).
The discriminatory performance of NLR, MLR, PLR and their sum in sepsis prognostication. The AUROCs of NLR, MLR, PLR and the sum of NLR, MLR and PLR in predicting 30-day mortality in adult ED patients with infection were 0.644 (95% CI 0.573¬0.716), 0.555 (95% CI 0.482–0.628), 0.606 (95% CI 0.529–0.682), and 0.610 (95% CI 0.534–0.686), respectively.
ANN in predicting 30-day all-cause mortality
Twelve variables with a significant association with 30-day all-cause mortality in univariate analyses, including patient age, sex, old age home resident status, CCI, triage MAP, pulse rate, RR, SpO2, hemoglobin, RDW, NLR and PLR, were inputted to the ANN model. The model has 1 hidden layer and seven nodes and its architecture is shown in Fig. 3. Table 4 shows the parameters of the model. The ANN model achieved an overall accuracy of 89.0% and 87.1% in predicting 30-day mortality in the training and testing datasets, respectively. The AUROC of the ANN model in the testing dataset was 0.811 (Fig. 4). The relative contributions of individual input variables in the ANN model are shown in Fig. 5. RR was the most important input variable, followed by SpO2, hemoglobin, pulse rate, and patient age.
The discriminatory performance of the artificial neural network. The area under the receiver operating characteristic curve of the artificial neural network in predicting 30-day mortality was 0.811 in the testing dataset. CCI, Charlson Comorbidity Index; Hb, hemoglobin; MAP, mean arterial pressure; NLR, neutrophil-to-lymphocyte ratio; OAHR, old age home resident; P, pulse rate; PLR, platelet-to-lymphocyte ratio; RDW, red cell distribution width; RR, respiratory rate; SpO2, oxygen saturation.
Discussion
Our study showed that 30-day survivors and non-survivors of infection differed significantly in terms of age, sex, old age home resident status, CCI, triage RR, SpO2, MAP, pulse rate, hemoglobin, RDW, NLR, and PLR on presentation. An ANN model incorporating these twelve input variables could achieve good discriminatory performance in predicting 30-day all-cause mortality in the testing dataset, compared with the modest discriminatory performance of NLR, MLR, PLR, and their sum.
The findings on the red cell parameters, including hemoglobin, hematocrit, and RDW, in predicting sepsis mortality are consistent with published studies. Jung et al. showed that initial hemoglobin levels were an independent factor of 90-day mortality, with odds ratios of 2.35, 1.97, and 1.88 for hemoglobin levels of < 7.0 g/dL, 7.0–7.9 g/dL, and 8.0–8.9 g/dL, respectively6. A retrospective study of 2,057 patients demonstrated that a low hematocrit level was an independent risk factor for 30-day mortality in septic patients. Luo et al. divided patients into low, regular, and high hematocrit levels, and the group with low hematocrit levels had a hazard ratio (HR) of 1.369 in univariate analysis and 1.589 in multivariate analysis7. A meta-analysis that involved 11 studies and 17,961 patients showed that an increased baseline RDW was associated with mortality (hazard ratio = 1.14)8. Since hemoglobin and hematocrit levels are highly correlated with each other, we only inputted the hemoglobin level to the ANN to avoid duplication.
As for the ratios between different differential WBC counts, the NLR appeared to have a better discriminatory performance in predicting 30-day mortality in our study compared with MLR and PLR. An elevated NLR may reflect physiologic stress that increases the number of neutrophil and decreases the number of lymphocytes. Sepsis also stimulates apoptosis of lymphocytes and 90–95% of septic patients have a NLR of > 3. When using the cutoff value of NLR > 10, it has a specificity of approximately 65% across several studies20. Djordjevic et al. found the AUROC of NLR as 0.68112, which is similar to our finding of 0.644 for NLR alone. In contrast, we found that the MLR had suboptimal discriminatory performance (AUROC 0.555), which is much lower than the AUROC of 0.655 reported by Li et al. in a retrospective study of 43,174 critically ill patients. However, this might be explained by differences in the study populations. Not all the patients in our study were critically ill21.
Regarding the PLR, we found that the ratio was significantly higher in non-survivors compared with survivors at 30 days. Interestingly, a meta-analysis involving 2,403 septic patients showed that PLR levels were significantly higher in non-survivors than survivors (random effect model: standardized mean difference [SMD] = 0.72, 95% CI; 0.35–1.10, p < 0.001). However, in the subgroup analysis of 1-month mortality, a significant difference was not demonstrated (SMD = 1.03, 95% CI = 0.15–1.92, p = 0.22)11. Similarly, we found that the AUROC of the PLR in predicting 30-day mortality was 0.606, indicating that the PLR alone has limited role in sepsis mortality prediction.
To improve the discriminatory performance of CBC parameters in predicting sepsis morality, attempts have been made to develop composite scores by combining different parameters. Djordjevic et al.12 showed that a composite bio score of MPV/PC, NLR, MLR, and PLR improved the AUROC to 0.718–0.874 in subgroups of patients with bacteremia. However, we could not replicate this method in our study because MPV is not reported in the routine CBC in our hospital. Another scoring system developed by Kim et al.13 that combined RDW, DNI, and MPV/PC had an AUROC of 0.67 in predicting 28-day mortality for septic patients, which was better than solely using the platelet count. However, DNI requires neutrophil data that are spaced 24 h apart, making it less relevant in clinical decision-making in the ED setting.
Instead of combining different CBC parameters, we found that combining the hemoglobulin level, RDW, NLR, and PLR on presentation with patient characteristics and triage vital sign variables could achieve a good discriminatory performance in predicting 30-day mortality using an ANN. This finding can be compared with other existing methods in sepsis prognostication. The performance of qSOFA was modest, with a pooled AUROC of 0.694 (95% CI 0.669–0.720) in predicting 30-day mortality across 29 studies of 108,122 patients. The pooled sensitivity over 60 studies in predicting in-hospital and 30-day mortality was 56.39%, and the pooled specificity was 74.58%22. Procalcitonin (PCT) and C-reactive protein (CRP) are commonly used biomarkers for sepsis. A meta-analysis of 23 studies involving 3,994 patients demonstrated that an elevated PCT level was associated with a higher mortality risk. The pooled relative risk was 2.60 (95% CI 2.05–3.30), and the AUROC was 0.77 (95% CI 0.73–0.80)23. Another meta-analysis involving 2,477 patients with community-acquired pneumonia showed that CRP had an AUROC of 0.62 (95% CI 0.58–0.67) in predicting in-hospital or 30-day mortality24. Our ANN model showed a comparable AUROC with PCT and represented an alternative method of sepsis prognostication without the need for additional biomarker testing. This finding has implications for sepsis care in resource-poor settings where access to procalcitonin or other sepsis biomarkers is limited.
The study has several limitations. Firstly, it was a single-center retrospective study with data collected during the winter months in Hong Kong. The findings might not be generalizable to other centers or ED patients who present in other seasons. Secondly, CBCs were not available for 501 patients, most of whom had mild infections not requiring hospital admission. The included patients were sicker, and a selection bias may have occurred. However, the need for early sepsis prognostication is higher among sicker patients with infections in the ED compared with those with mild infections. Thirdly, the time of blood-taking was not standardized, and the CBC data represented values at different times along the trajectory of sepsis progression. Lastly, we did not validate the derived ANN model in a separate cohort of patients. This warrants further large-scale out-of-the-sample validation before clinical application.
In summary, an ANN model that combined presenting hemoglobin, RDW, NLR, PLR, and clinical parameters showed better discriminatory performance than individual CBC parameters in predicting 30-day mortality in adult ED patients with an infection. Further validation studies in larger cohorts are necessary before clinical adoption.
Data availability
The dataset generated during and/or analysed during the current study are not publicly available due to local regulations on patient privacy but de-identified data are available from the corresponding author on reasonable request.
References
Rudd, K. E. et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 395, 200–211 (2020).
Song, J. U., Sin, C. K., Park, H. K., Shim, S. R. & Lee, J. Performance of the quick Sequential (sepsis-related) Organ Failure Assessment score as a prognostic tool in infected patients outside the intensive care unit: A systematic review and meta-analysis. Crit. Care 22, 28 (2018).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 801–810 (2016).
Kilinc-Toker, A., Kose, S. & Turken, M. Comparison of SOFA Score, SIRS, qSOFA, and qSOFA + L Criteria in the diagnosis and prognosis of sepsis. Eurasian J. Med. 53, 40–47 (2021).
Qi, D. & Peng, M. Early hemoglobin status as a predictor of long-term mortality for sepsis patients in intensive care units. Shock 55, 215–223 (2021).
Jung, S. M., Kim, Y. J., Ryoo, S. M. & Kim, W. Y. Relationship between low hemoglobin levels and mortality in patients with septic shock. Acute Crit. Care 34, 141–147 (2019).
Luo, M., Chen, Y., Cheng, Y., Li, N. & Qing, H. Association between hematocrit and the 30-day mortality of patients with sepsis: A retrospective analysis based on the large-scale clinical database MIMIC-IV. PLoS One 17, 3. https://doi.org/10.1371/journal.pone.0265758 (2022).
Zhang, L., Yu, C. H., Guo, K. P., Huang, C. Z. & Mo, L. Y. Prognostic role of red blood cell distribution width in patients with sepsis: A systematic review and meta-analysis. BMC Immunol. 21, 40 (2020).
Al Saleh, K. & AlQahtani, R. M. Platelet count patterns and patient outcomes in sepsis at a tertiary care center: Beyond the APACHE score. Med. Baltim. 100, 18. https://doi.org/10.1097/MD.0000000000025013 (2021).
Huang, Z., Fu, Z., Huang, W. & Huang, K. Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: A meta-analysis. Am. J. Emerg. Med. 38, 641–647 (2020).
Wang, G. et al. Prognostic value of platelet to lymphocyte ratio in sepsis: A systematic review and meta-analysis. Biomed. Res. Int. 2022, 9056363. https://doi.org/10.1155/2022/9056363 (2022).
Djordjevic, D. et al. Neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and mean platelet volume-to-platelet count ratio as biomarkers in critically ill and injured patients: Which ratio to choose to predict outcome and nature of bacteremia?. Mediat. Inflamm. 2018, 3758068. https://doi.org/10.1155/2018/3758068 (2018).
Kim, J. H. et al. A modified simple scoring system using the red blood cell distribution width, delta neutrophil index, and mean platelet volume-to-platelet count to predict 28-day mortality in patients with sepsis. J. Intensive Care Med. 36, 873–878 (2021).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 370, 1453–1457 (2007).
Moons, K. G. et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): Explanation and elaboration. Ann. Intern. Med. 62, W1-73 (2015).
Nah, E. H., Kim, S., Cho, S. & Cho, H. I. Complete blood count reference intervals and patterns of changes across pediatric, adult, and geriatric ages in Korea. Ann. Lab. Med. 38, 503–511 (2018).
Thachil, J. & Bates, I. Approach to the diagnosis and classification of blood cell disorders. Dacie Lewis Pract. Haematol. 497–510, 2017. https://doi.org/10.1016/B978-0-7020-6696-2.00023-0 (2017).
Vincent, J. L. et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 22, 707–710 (1996).
Grissom, C. K. et al. A modified sequential organ failure assessment score for critical care triage. Disaster Med. Public Health Prep. 4, 277–284 (2010).
Farkas, J. D. The complete blood count to diagnose septic shock. J. Thorac. Dis. 12, S16–S21 (2020).
Li, Y. et al. Monocyte/lymphocyte ratio as a predictor of 30-day mortality and adverse events in critically ill patients: Analysis of the MIMIC-III database. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 33, 582–586 (2021).
Herwanto, V. et al. Accuracy of quick sequential organ failure assessment score to predict sepsis mortality in 121 studies including 1,716,017 individuals: A systematic review and meta-Analysis. Crit. Care Explor. 1, e0043 (2019).
Liu, D., Su, L., Han, G., Yan, P. & Xie, L. Prognostic value of procalcitonin in adult patients with sepsis: A systematic review and meta-analysis. PLoS One 10, 6. https://doi.org/10.1371/journal.pone.0129450 (2015).
Viasus, D. et al. Biomarkers for predicting short-term mortality in community-acquired pneumonia: A systematic review and meta-analysis. J. Infect. 72(3), 273–282 (2016).
Acknowledgements
This study was supported by the Heath and Medical Research Fund of the Food and Health Bureau of the Hong Kong Special Administrative Region (Project No. 19201161) and Seed Fund from the University of Hong Kong. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
R.P.K.L., B.P.K.W. and T.H.R. conceived the study and designed the study. R.P.K.L. and T.H.R. obtained research funding. R.P.K.L., T.H.R., T.C.T., M.S.H.T. supervised the conduct of the trial. R.P.K.L., C.Y.T.I., H.C.C., L.Z., M.C.K.L. recruited patients and collected data. R.P.K.L. managed the data, including quality control. R.P.K.L. provided statistical advice on study design and analyzed the data. M.C.K.L prepared figure 3. B.P.K.W. drafted the manuscript, and all authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wong, B.P.K., Lam, R.P.K., Ip, C.Y.T. et al. Applying artificial neural network in predicting sepsis mortality in the emergency department based on clinical features and complete blood count parameters. Sci Rep 13, 21463 (2023). https://doi.org/10.1038/s41598-023-48797-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48797-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.