Abstract
The incidence of colorectal cancer (CRC) is increasing in low- and middle-income countries. This study aimed to estimate the burden of CRC attributable to nutritional risk in the Middle East and North Africa (MENA) region. The GBD 2019 methods were used to estimate age-standardized mortality rates (ASMRs) and disability-adjusted life-years (DALYs) in 2019 and over the past three decades. We evaluated the 30-year trend in DALYs and mortality rates from nutrition-related risks of CRC, from 1990 to 2019 by sex and age groups in 21 countries in the MENA region. The rate of DALYs/100,000 due to diet-related risks for CRC in 2019 was 79.71 (95% UI: 56.79, 98.44) and 65.16 (95% UI: 45.86, 80.95) in men and women, respectively. The percent changes of DALYs/100,000 in men and women were 8.15% and 2.50%, respectively, between 1990 and 2019. The percent changes in ASMRs in men and women were 8.32% and 3.44%, respectively. The highest DALYs and ASMRs were observed in both sexes in the age group 75–79 years and above. The highest percent changes in DALYs/100,000 and ASMRs were observed between 1990 and 2019 in Afghanistan, Egypt, Iran, Iraq, Lebanon, Libya, Morocco, Palestine, Qatar, Saudi Arabia, Sudan and Yemen. DALYs and ASMRs attributed to dietary risk for CRC increased in 21 countries in the MENA region from 1990 to 2019. A modified diet with more fiber, dairy products and less red meat intake is a highly recommended strategy for prevention CRC.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) ranks third in incidence and second in mortality rate in worldwide1. The incidence of CRC was estimated at 1.8 million new cases and 881,000 deaths in 2018, and is projected to increase by about 60% by 20302. In low- and middle-income countries, CRC has shown an increasing trend2. Age-standardized incidence, mortality rates and disability-adjusted life-years (DALYs) for CRC in the Middle East and North Africa (MENA) are 13.9, 9.8 and 218.7 per 100,000, respectively3.
While the exact cause of CRC is still unknown. However, evidence suggests that the incidence of CRC is influenced by genetic, environmental, obesity, behavioral habits (smoking and inactivity) and metabolic risks4, 5. The modifiable environmental and behavioral risk factors such as diet and nutritional habits are potentially preventable6, 7. Epidemiological studies have demonstrated an association between dietary intake and the risk of CRC. In 2017, a low- fiber diet contributed to 25,561 CRC deaths, with population attributable fractions (PAFs) of 13.7% in China8. A study by Mint et al. has shown an association between meat consumption and CRC risk in the MENA region9. The association between dairy consumption and risk of CRC in the MENA region in a systematic review indicates conflicting results10. In general, diets high in fiber, whole grains, milk and calcium can reduce the risk of CRC8, 11, 12, whereas red and processed meats, animal fats, and high-cholesterol foods increase the risk11. The results of a meta-analysis (2016) show that "healthy" dietary pattern may reduce the risk of CRC, while "western-style" and "alcohol-consumption" patterns may increase the risk of CRC13. A study by Yujiao Deng et al. (2021) showed that CRC deaths and DALYs due to nutritional risks increased by 50.88% and 47.63% respectively, over the past 30 years6.
According to the Global Burden of Disease (GBD) study (2015), the attributable burden due to nutritional risks is estimated to be 12.2% and 9% of total DALYs for men and women worldwide in 2015, respectively, making dietary risk a greater burden than smoking or alcohol consumption14. This highlights the importance of improving nutrition at the global, regional, and national levels. In fact, diet is one of the modifiable risk factors that can reduce the burden of CRC. Identifying CRC risk factors helps policy makers to design prevention programs. This study aimed to estimate the mortality and burden of CRC attributable to nutritional risks in the MENA region from 1990 to 2019.
Methods
Data source, case definition and exposure
This study was conducted using the Global Burden of Disease-2019 (GBD-2019) study, which can be found on the Institute for Health Metrics and Evaluation (IHME) website. Data are presented by country, age, and sex from 1990 to 2019 (https://vizhub.healthdata.org/gbd-compare/). The study population includes the MENA region, which includes 21 countries. Therefore, we extracted data for 21 countries, including Afghanistan, Algeria, Bahrain, Egypt, Iraq, Iran, Morocco, Oman, Palestine, Jordan, Kuwait, Lebanon, Libya Qatar, Saudi Arabia, Sudan, Syria, Tunisia, Turkey, the United Arab Emirates, and Yemen.
The CRC is defined as colon and rectal cancer. International Classification of Diseases-10 (ICD-10) codes were used to represent CRC (C18–C21, D01.0–D01.2, and D12–D12.8)15.
Diet-related risks were considered as risk factors. According to GBD study, six dietary risk factors have been evaluated, including diets high in red meat, low in fiber, low in calcium, low in milk, and low in whole grains6. Diets low in whole grains consist of consumption of less than 140 to 160 gram/day of whole grains (germ, endosperm and bran in normal proportions) from pancakes, cookies, bread, breakfast cereals, biscuits, tortillas, rice, pasta and others source. Low-milk diets are the average daily consumption of less than 360 to 500 gram/day of milk (high-fat, low-fat and fat-free), excluding soy milk and other plant derivatives. Diets high in red meat include consumption of red meat (gram/day), such as lamb, pork, beef, and goat, but exclude eggs, fish, poultry, and all processed meats. Diets high in processed meat represent any consumption of meat (gr/day) that is preserved by cooking, smoking, salting, or adding chemical preservatives. Diets low in fiber indicate an average intake of less than 21 to 22 gr/day of fiber per day from all sources, especially grains, fruits, legumes, vegetables, and legumes. Low-calcium diets are defined based on an average intake of less than 1.06–1.1 gram/day of calcium from all sources, including cheese, milk, and yogurt6.
Statistical analysis
DALY was computed as follows: DALY = Years lost due to disability (YLD) + years of life lost (YLL). DALYs and age-standardized mortality rates (ASMRs) attributable to dietary risks were presented by country and sex. The age composition of the population in MENA region is different and it is necessary to adjust the effect of age. Therefore, age-standardized estimates are reported. We report age-standardized estimates and 95% confidence intervals (CIs) for rates or numbers of DALYs, deaths, and 10-year percent change from 1990 to 2019 in the MENA region and 21 countries. All rates were per 100,000 persons. Percent change was calculated at three time points by sex and country. All analyses were performed using R software version 4.0.2 (2020.06.22).
Ethics approval and consent to participate
The study was approved by the ethics committee of Kermanshah University of Medical Sciences (KUMS.REC.1402.056). All methods were carried out by relevant guidelines and regulations.
Results
The rate of DALYs/100,000 attributed to dietary risk for CRC and the percent change from 1990 to 2019 in MENA countries are shown in Table 1. The rate of DALYs/100,000 attributed to dietary risk for CRC in 1990, 2000, 2010 and 2019 were 70.77 (95% UI 51.69, 92.56), 65.37 (95% UI 48.41, 78.76), 73.70 (95% UI 53.21, 88.64) and 79.71 (95% UI 56.79, 98.44), respectively, among men in the MENA region. The rate of DALYs/100,000 attributed to dietary risk for CRC in 1990, 2000, 2010, and 2019 was 63.59 (95% UI 46.04, 81.94), 59.16 (95% UI 43.98, 70.80), 63.57 (95% UI 44.88, 76.26), and 65.16 (95% UI 45.86, 80.95), respectively, among women in the MENA region.
The rate of DALYs/100,000 attributed to dietary risk for CRC increased among men and women in Afghanistan, Egypt, Iran, Iraq, Lebanon, Libya, Morocco, Palestine, Qatar, Saudi Arabia, Sudan and Yemen from 1990 to 2019. The highest percentage changes in the rate of DALYs/100,000 attributed to dietary risk for CRC between 2010 and 2019 were observed in Egypt, Iran, Iraq, Morocco, and Palestine. In Kuwait, Bahrain, Oman, Qatar, and the United Arab Emirates, the percentage change was negative between 1990 and 2019. In all countries in the MENA region, the rate of DALYs/100,000 attributable to diet-related risk for CRC is higher in men than in women, except in Afghanistan and Qatar.
The ASMRs attributed to diet-related risk for CRC in MENA countries from 1990 to 2019 is shown in Table 2. ASMR attributed to diet-related risk for CRC increased in men and women in Afghanistan, Egypt, Iran, Iraq, Morocco, Palestine, and Sudan from 1990 to 2019. ASMRs attributed to dietary risk for CRC increased by 8.32% in men and 3.44% in women between 2010 and 2019 in MENA countries. ASMRs attributed to diet-related risk for CRC is higher among men than women in MENA countries.
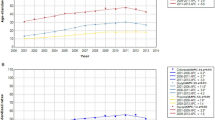
Mortality and burden of diet-related risk for CRC in MENA countries for both sexes are shown in Fig. 1. It shows the trend of ASMRs and DALYs attributable to diet-related risks for CRC in MENA countries for both sexes in 1990, 2000, 2010, and 2019. The trend of DALYs/100,000 attributable to nutritional risk increased in Saudi Arabia, Morocco, Jordan, Libya, and Afghanistan for men from 1990 to 2019. The trend of ASMRs attributable to nutritional risk increased in women in Palestine and Tunisia and in men in Yemen, Syrian Arab Republic, Palestine, and Tunisia from 1990 to 2019.
Figure 2 DALYs/100,000 and mortality rate attributable to diet-related risks were higher in Palestine, the United Arab Emirates, Jordan, Lebanon, Turkey and Bahrain than in other countries. DALYs/100,000 and mortality rates were higher in the age group 75–79 years and older.
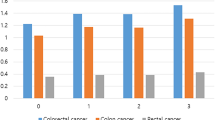
DALYs/100,000 and ASMRs of attributable to diets high in red meat, low in calcium, low in milk, low in fiber and low in whole grains were higher in men in Palestine, the United Arab Emirates, Jordan, Lebanon, Turkey, and Bahrain than in other countries. DALYs/100,000 and ASMRs attributed to a diet high in red meat, low in calcium, low in milk, low in fiber, and low in whole grains for CRC were higher in Palestine, the United Arab Emirates, Jordan, Lebanon, Qatar, Libya, Afghanistan, Turkey, and Bahrain among women than in other countries. A diet low in fiber, milk, and whole grains was associated with a higher risk of CRC than a diet high in red meat and low in calcium in men and women in MENA countries (Fig. 3).
Figures 4 and 5 show that the age-standardized DALYs and mortality rates of CRC due to dietary risk with socio-demographic index (SDI) are not significantly different from each other in MENA countries.
Discussion
DALYs and ASMRs attributed to nutritional risk for CRC increased in MENA regions from 1990 to 2019. The percent changes related to ASMRs in men and women were 8.32% and 3.44%, respectively. The percent changes related to DALYs/100,000 in men and women were 8.15% and 2.50%, respectively. The highest DALYs and ASMRs were observed in both sexes in the age group 75–79 years and above. The highest percent changes in DALYs/100,000 and ASMRs were observed between 1990 and 2019 in Afghanistan, Egypt, Iran, Iraq, Lebanon, Libya, Morocco, Palestine, Qatar, Saudi Arabia, Sudan and Yemen.
The study by Deng et al. (2019) reported that 32% of deaths and 34% of DALYs worldwide due to CRC were attributable to diet-related factors, and the age-standardized rate (ASR was higher in men than in women6. According to the results of a systematic analysis (2022), age standardized incidence and mortality rates were higher in men than in women3. The incidence of colorectal cancer has increased in younger age groups (20–49 years) in high-income countries3, 16. The increasing trend of diet-related CRC may be attributed to improved screening programs, increased consumption of fast food (high in salt and fat), and increased prices of healthy foods (fruits, vegetables, and dairy products) in some countries.
Our analysis also showed that the lowest DALYs and ASMR of CRC were attributed to diets rich in milk, fiber, whole grains and calcium, and low in red meat in MENA countries. However, the risk of a diet low in fiber, milk, and whole grains was much higher than that of a diet rich in red meat and low in calcium. In general, the role of these four dietary factors (milk, fiber, whole grains, red meat and calcium) was identified as the most important nutritional factors for the incidence of CRC8, 12, 17,18,19. One study showed that a diet low in milk, calcium, and whole grains was responsible for 81.64% of DALYs and 81.61% of deaths for CRC6. The results of a systematic review showed that the three most important risk factors for DALYs attributable to CRC in 195 countries, were a low calcium diet (20.5%), alcohol consumption (15.2%), and a low milk diet (14.3%) were for both sexes20. A study comparing disease risk factors using GBD data showed that diet-related risk factors increased the global burden more than smoking or alcohol14. The results of the study by Vulcan et al. showed that the association between meat consumption and CRC varied by meat type, sex, and tumor location in the intestine21. The effects of diet on inflammation and carcinogenesis were examined. In a study by Chou et al., it was reported that a pro-inflammatory diet—characterized by a low intake of fruits and vegetables and a high intake of grains—was strongly associated with an increased risk of CRC. However, the association between pro-inflammatory diet and the risk of CRC may vary depending on the genetic variant of IL-17F, anatomical location and other risk factors22. The anti-cancer effect of food has always been an interesting topic for researchers and scientists. Some research has shown that consumption of milk has a protective effect against colon cancer23, 24. In addition, vitamin D, calcium, conjugated linoleic acid, butyric acid, and lactose in milk also have certain antitumor effects23, and whole grains have anti-cancer properties of fiber, antioxidants, and phytochemicals25. This finding highlights the need to improve diet in different ethnicities, regions, and countries. Therefore, diet modification is one of the most important strategies to prevent CRC and can reduce the burden of this disease in worldwide.
Dietary factors increase the risk of CRC through two possible mechanisms, including increasing weight and causing inflammation. Thus, a balanced diet helps to maintain a balanced weight and prevents obesity and its consequences26,27,28,29. According to scientific evidence, obesity is an important risk factor for CRC30,31,32. Obesity causes inflammation in the body and especially in the intestine. Therefore, inflammation due to obesity is one of the possible factors that increase the risk of various cancers, especially CRC in people, which may lead to CRC due to pro-inflammatory effects and oxidative stress33, 34. Therefore, a balanced diet with maintaining a balanced weight and reducing hormones and inflammatory markers such as leptin, adiponectin IL-6, and TNF-α may be a preventive strategy against CRC. Leptin is a risk factor for CRC35, 36, and circulating leptin levels are high in obese individuals who have leptin resistance37. Epidemiological studies have shown that decreased plasma adiponectin levels are inversely associated with colorectal cancer risk38, 39. TNF-α and IL-6 are also secreted from adipose tissue, which is an important inflammatory factor in the acute inflammatory reaction, and is involved in the pathogenesis of CRC40, 41.
DALYs/100,000 and ASMRs of attributable to diets high in red meat, low in calcium, low in milk, low in fiber, and low in whole grains were higher in Palestine, the United Arab Emirates, Jordan, Lebanon, Turkey and Bahrain than in other countries. The percentage of DALYs due to CRC attributable to a low calcium and low milk diet in the MENA region was similar to the global percentage (20.6% vs. 20.5%), lower than in African regions (Western, Eastern, Central and Southern Sub-Saharan Africa), and higher than Western Europe, Australasia, Central Europe, Eastern Europe and Central Asia20.
Some limitations in this study were unavoidable. Part of the limitation is related to countries’ screening programs and the changes that have occurred in screening programs over the past 30 years. Some countries with poor health systems may not have a proper cancer registration system. The study of a large region of 21 countries is one of the strengths of this study. The results of this study provide data from 21 countries and allow comparability among countries in the region.
Conclusion
DALYs and ASMRs attributed to diet-related risk for CRC increased in 21 countries in the MENA region from 1990 to 2019, and this increase was greater in men than in women. The highest DALYs and ASMR were observed in the age group 75–79. Afghanistan, Egypt, Iran, Iraq, Lebanon, Libya, Morocco, Palestine, Qatar, Saudi Arabia, Sudan and Yemen had the highest percent changes in DALYs/100,000 and ASMRs between 1990 and 2019. A diets high in milk, fiber, whole grains, and calcium and low in red meat is associated with a lower risk of CRC in MENA countries. Therefore, dietary modification with an increase in fiber and dairy products intake and a decrease in red meat intake is highly recommended strategy for prevention CRC.
Data availability
The data sets generated during this study are available from the correspondence author on reasonable request via email.
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424 (2018).
Arnold, M. et al. Global patterns and trends in colorectal cancer incidence and mortality. Gut 66, 683–691 (2017).
Sharma, R. et al. Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol. Hepatol. 7, 627–647 (2022).
Al-Zalabani, A. Preventability of colorectal cancer in Saudi Arabia: Fraction of cases attributable to modifiable risk factors in 2015–2040. Int. J. Environ. Res. Public Health 17, 320 (2020).
Al-Zalabani, A. H. Cancer incidence attributable to tobacco smoking in GCC countries in 2018. Tobacco Induced Dis. 18, 118722 (2020).
Deng, Y. et al. Dietary risk related colorectal cancer burden: Estimates from 1990 to 2019. Front. Nutr. 8, 568 (2021).
Yang, J. et al. Development of a colorectal cancer diagnostic model and dietary risk assessment through gut microbiome analysis. Exp. Mol. Med. 51, 1–15 (2019).
Wang, Z.-Q. et al. Burden and trend of ischemic heart disease and colorectal cancer attributable to a diet low in fiber in China, 1990–2017: findings from the Global Burden of Disease Study 2017. Eur. J. Nutr. 60, 3819–3827 (2021).
Mint Sidi Deoula, M., El Kinany, K., Hatime, Z., Boudouaya, H. A. & El Rhazi, K. Meat and colorectal cancer in Middle Eastern and North African countries: Update of literature review. Public Health Rev. 41, 1–13 (2020).
El Kinany, K., Deoula, M., Hatime, Z., Bennani, B. & El Rhazi, K. Dairy products and colorectal cancer in middle eastern and north African countries: A systematic review. BMC Cancer 18, 1–8 (2018).
Song, M., Chan, A. T. & Sun, J. Influence of the gut microbiome, diet, and environment on risk of colorectal cancer. Gastroenterology 158, 322–340 (2020).
Wang, Z. et al. Burden of colorectal cancer attributable to diet low in milk in China, 1990–2017: Findings from the global burden of disease study 2017. J. Hum. Nutr. Dietetics 34, 233–242 (2021).
Feng, Y.-L. et al. Dietary patterns and colorectal cancer risk: A meta-analysis. Eur. J. Cancer Prev. 26, 201–211 (2017).
Forouzanfar, M. H. et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1659–1724 (2016).
Annual report of national cancer registration: cancer incidence in 2005 and survival for 1993–2005. http://www.iarc.fr/. Accessed 10 Sep 2008.
Cavestro, G. M. et al. Early onset sporadic colorectal cancer: Worrisome trends and oncogenic features. Dig. Liver Dis. 50, 521–532 (2018).
Haslam, A., Wagner Robb, S., Hébert, J. R., Huang, H. & Ebell, M. H. Association between dietary pattern scores and the prevalence of colorectal adenoma considering population subgroups. Nutr. Dietetics 75, 167–175 (2018).
Lee, J., Shin, A., Choi, J.-Y., Kang, D. & Lee, J.-K. Adherence to the recommended intake of calcium and colorectal cancer risk in the HEXA study. Cancer Res. Treatm. 53, 140 (2021).
Sasso, A. & Latella, G. Dietary components that counteract the increased risk of colorectal cancer related to red meat consumption. Int. J. Food Sci. Nutr. 69, 536–548 (2018).
Safiri, S. et al. The global, regional, and national burden of colorectal cancer and its attributable risk factors in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 4, 913–933 (2019).
Vulcan, A., Manjer, J., Ericson, U. & Ohlsson, B. Intake of different types of red meat, poultry, and fish and incident colorectal cancer in women and men: Results from the Malmö Diet and Cancer Study. Food Nutr. Res. 61, 13419810 (2017).
Cho, Y. et al. Inflammatory dietary pattern, IL-17F genetic variant, and the risk of colorectal cancer. Nutrients 10, 724 (2018).
Barrubés, L., Babio, N., Becerra-Tomás, N., Rosique-Esteban, N. & Salas-Salvadó, J. Association between dairy product consumption and colorectal cancer risk in adults: A systematic review and meta-analysis of epidemiologic studies. Adv. Nutr. 10, S190–S211 (2019).
Larsson, S. C. et al. Genetically proxied milk consumption and risk of colorectal, bladder, breast, and prostate cancer: A two-sample Mendelian randomization study. BMC Med. 18, 1–7 (2020).
Aune, D. et al. Dietary fibre, whole grains, and risk of colorectal cancer: Systematic review and dose-response meta-analysis of prospective studies. BMJ 343, 6617 (2011).
Darbandi, M., Najafi, F., Pasdar, Y., Mostafaei, S. & Rezaeian, S. Factors associated with overweight and obesity in adults using structural equation model: mediation effect of physical activity and dietary pattern. Eat. Weight Disord. Stud. Anorexia Bulimia Obes. 25, 1561–1571 (2020).
Hsu, K.-J., Liao, C.-D., Tsai, M.-W. & Chen, C.-N. Effects of exercise and nutritional intervention on body composition, metabolic health, and physical performance in adults with sarcopenic obesity: A meta-analysis. Nutrients 11, 2163 (2019).
Jessri, M., Wolfinger, R. D., Lou, W. Y. & L’Abbé, M. R. Identification of dietary patterns associated with obesity in a nationally representative survey of Canadian adults: Application of a priori, hybrid, and simplified dietary pattern techniques. Am. J. Clin. Nutr. 105, 669–684 (2017).
Sun, J., Buys, N. J. & Hills, A. P. Dietary pattern and its association with the prevalence of obesity, hypertension and other cardiovascular risk factors among Chinese older adults. Int. J. Environ. Res. Public Health 11, 3956–3971 (2014).
Dong, Y. et al. Abdominal obesity and colorectal cancer risk: Systematic review and meta-analysis of prospective studies. Biosci. Rep. 37, 45 (2017).
Elangovan, A. et al. Colorectal cancer, age, and obesity-related comorbidities: A large database study. Dig. Dis. Sci. 66, 3156–3163 (2021).
Liu, P.-H. et al. Association of obesity with risk of early-onset colorectal cancer among women. JAMA Oncol. 5, 37–44 (2019).
Bilski, J. et al. Role of obesity, mesenteric adipose tissue, and adipokines in inflammatory bowel diseases. Biomolecules 9, 780 (2019).
Nani, A., Murtaza, B., Sayed Khan, A., Khan, N. A. & Hichami, A. Antioxidant and anti-inflammatory potential of polyphenols contained in Mediterranean diet in obesity: Molecular mechanisms. Molecules 26, 985 (2021).
Endo, H. et al. Leptin acts as a growth factor for colorectal tumours at stages subsequent to tumour initiation in murine colon carcinogenesis. Gut 60, 1363–1371 (2011).
Modzelewska, P., Chludzińska, S., Lewko, J. & Reszeć, J. The influence of leptin on the process of carcinogenesis. Contemp. Oncol. 23, 63 (2019).
Engin, A. Diet-induced obesity and the mechanism of leptin resistance. Obes. Lipotoxicity 1, 381–397 (2017).
Kelesidis, I., Kelesidis, T. & Mantzoros, C. Adiponectin and cancer: A systematic review. Br. J. Cancer 94, 1221–1225 (2006).
Wei, E. K., Giovannucci, E., Fuchs, C. S., Willett, W. C. & Mantzoros, C. S. Low plasma adiponectin levels and risk of colorectal cancer in men: A prospective study. J. Natl. Cancer Inst. 97, 1688–1694 (2005).
Ellulu, M. S., Patimah, I., Khaza’ai, H., Rahmat, A. & Abed, Y. Obesity and inflammation: the linking mechanism and the complications. Arch. Med. Sci. AMS 13, 851 (2017).
Wei, X. et al. TNF-α activates Wnt signaling pathway to promote the invasion of human colon cancer stem cells. Chin. J. Cell. Mol. Immunol. 34, 982–988 (2018).
Acknowledgements
The authors thank the Kermanshah University of Medical Sciences.
Funding
This research was supported by Kermanshah University of Medical Sciences (Grant Number: 4020191).
Author information
Authors and Affiliations
Contributions
Protocol/project development: M.D., Y.P. Data collection or management: M.D., B.H., F.K.S., M.G.H. Data analysis: F.K.S., M.D. Manuscript writing/editing: M.D., D.S., Y.P., H.L.F., B.M.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pasdar, Y., Shadmani, F.K., Fateh, H.L. et al. The burden of colorectal cancer attributable to dietary risk in Middle East and North African from 1990 to 2019. Sci Rep 13, 20244 (2023). https://doi.org/10.1038/s41598-023-47647-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-47647-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.