Abstract
Minimally invasive glaucoma surgery has expanded the surgical treatment options in glaucoma, particularly when combined with cataract surgery. It is clinically relevant to understand the associated postoperative changes in biomechanical properties because they are influential on the measurement of intraocular pressure (IOP) and play an important role in the pathogenesis of open-angle glaucoma (OAG). This retrospective case–control study included OAG patients who underwent cataract surgery combined with microhook ab interno trabeculotomy (µLOT group: 53 eyes of 36 patients) or iStent implantation (iStent group: 59 eyes of 37 patients) and 62 eyes of 42 solo cataract patients without glaucoma as a control group. Changes in ten biomechanical parameters measured with the Ocular Response Analyzer and Corneal Visualization Scheimpflug Technology (Corvis ST) at 3 and 6 months postoperatively relative to baseline were compared among the 3 groups. In all the groups, IOP significantly decreased postoperatively. In the µLOT and control groups, significant changes in Corvis ST-related parameters, including stiffness parameter A1 and stress‒strain index, indicated that the cornea became softer postoperatively. In contrast, these parameters were unchanged in the iStent group. Apart from IOP reduction, the results show variations in corneal biomechanical changes from minimally invasive glaucoma surgery combined with cataract surgery.
Similar content being viewed by others
Introduction
Glaucoma is one of the leading causes of blindness worldwide. Intraocular pressure (IOP) is the only modifiable established factor that halts the progression of glaucoma. The biomechanical properties of an eye are also important in the disease because they affect the measurement of IOP1,2, and moreover, they play an important role in the pathogenesis of glaucoma itself3. Advancements in biometric techniques in recent decades have enabled the direct measurement of biomechanical features of an eye. One of the most representative examples is the Ocular Response Analyzer (ORA; Reichert Inc., Depew, NY). ORA-measured corneal hysteresis (CH) reflects the damping capacity of the cornea4,5,6, which has been reported to be closely associated with the development7, severity8, and progression of glaucoma9,10. In addition, Corneal Visualization Scheimpflug Technology (Corvis ST; Oculus GmbH, Wetzlar, Germany) captures detailed images of the corneal deformation induced by the application of an air jet using an ultrahigh-speed Scheimpflug camera and provides data on various biomechanical parameters. Such Corvis ST parameters are associated with the severity8 and visual field progression11 of glaucoma.
Cataract surgery is often performed in aged patients. The prevalence of glaucoma also increases with increasing age12,13. Many studies have reported that IOP decreases after cataract surgery. However, a recent study indicated that this “IOP reduction” is not associated with the subsequent prevention of the progression of the disease14. We previously speculated that this is probably because of the biomechanical change in the eye following cataract surgery15. Currently, minimally invasive glaucoma surgery (MIGS) has greatly expanded the surgical treatment options in glaucoma, particularly when combined with cataract surgery. Thus, it is clinically relevant to understand the associated postoperative changes in biomechanical properties in relation to the change in IOP. However, there are few reports that shed light on this issue using ORA and Corvis ST.
The microhook ab interno trabeculotomy (µLOT) and iStent trabecular microbypass (Glaukos Corp., San Clemente, CA, USA) implantation procedures are two examples of MIGS, and recently, there has been an increase in the number of cases for both procedures16,17. Both techniques facilitate aqueous outflow, resulting in the reduction of IOP; the microhook incises the trabecular meshwork, whereas iStent is inserted into the trabecular meshwork. In the current study, the changes in IOP and the corneal biomechanical properties measured with ORA and Corvis ST were compared between µLOT combined with cataract surgery and iStent implantation combined with cataract surgery while matching background factors such as age and axial length; solo cataract surgery served as a control.
Methods
This retrospective case‒control study was designed to investigate postoperative changes in biomechanical properties measured with ORA and Corvis ST in open-angle glaucoma (OAG) eyes after µLOT or iStent implantation combined with cataract surgery. Eyes receiving solo cataract surgery in patients without glaucoma were also included as controls. This study was approved by the Research Ethics Committees of the Seirei Hamamatsu General Hospital (#10619). This study was conducted in accordance with the tenets of the Declaration of Helsinki. All participants signed a written informed consent form for their clinical information to be stored in the hospital database and used for research.
Participants
The study included OAG patients who underwent µLOT or iStent implantation combined with cataract surgery (µLOT and iStent group, respectively) and non-OAG eyes that received solo cataract surgery alone as a control group (solo cataract group). Age and axial length were matched among the 3 groups to avoid the possible effects of these variables on the biomechanical properties of the cornea. Inclusion criteria for the µLOT and iStent groups were as follows: (1) typical glaucomatous changes in the optic nerve head (e.g., rim notch with a rim width ≤ 0.1 disc diameter, a vertical cup-to-disc ratio > 0.7, or a retinal nerve fiber layer defect); (2) glaucomatous VF defects compatible with the optic nerve head changes meeting the Anderson–Patella criteria18 on two consecutive examinations; and (3) wide open angle with gonioscopy. The operation method chosen was based on the surgeon’s preference, but µLOT was selected when VF damage threatened the central VF, following the guidelines from the Japanese Ophthalmological Society19.
The solo cataract group included participants with no abnormal eye-related findings except for cataracts on biomicroscopy, gonioscopy, and funduscopy and no history of ocular diseases, such as diabetic retinopathy or age-related macular degeneration.
The exclusion criteria for the 3 groups were as follows: (1) contact lens wearers; (2) any abnormality of the cornea that could affect Corvis ST measurement, such as keratoconus; and (3) experience of any other ocular surgery, including corneal refractive surgery.
Surgical technique
All procedures were performed by a single surgeon (RA) at Seirei Hamamatsu General Hospital between April 2020 and January 2022. All surgeries were performed under topical anesthesia. Phacoemulsification with intraocular lens implantation in the posterior chamber was performed through a clear corneal incision of 2.4 mm in length. After successful lens implantation involving eyes in the µLOT group, the trabecular meshwork was incised through two quadrants using a trabeculotomy microhook. In the case of eyes in the iStent group, the anterior chamber was filled with Opegan (Santen Pharmaceutical Co., Japan), and the iStent was injected under direct visualization into the nasal angle into Schlemm’s canal using a Swan-Jacob gonioprism lens (Ocular Instruments, Bellevue, WA, USA). Postoperatively, patients received both topical anti-inflammatory medication (Bromfenac Sodium Hydrate Ophthalmic Solution 0.1%, two times daily) and topical antibiotic (Moxifloxacin Ophthalmic Solution 1.5%, four times daily) for 6 weeks. All antiglaucoma medications prescribed preoperatively in glaucoma patients (in the µLOT or iStent group) were discontinued after the surgery. These medications were resumed at the discretion of the attending physician in the postoperative follow-up.
Clinical data acquisition
Baseline demographic data regarding parameters such as age, sex, and axial length were collected from the medical charts. Axial length was measured preoperatively using the IOL Master ver. 5.02 (Carl Zeiss Meditec, CA, USA). Corvis ST, ORA, and Goldmann applanation tonometer (GAT)-IOP measurements were obtained preoperatively and at 3 and 6 months postoperatively. Corvis ST and ORA measurements were obtained at 15 min intervals. The order of the measurements was randomly determined.
Corvis ST
The principles underlying Corvis ST measurements have been described in detail elsewhere20. In brief, a high-speed Scheimpflug camera records 140 images in 30 ms of corneal deformation in response to an air pulse emitted from the device. The response of the cornea is characterized by the moment when the cornea is most significantly depressed (highest concavity: HC) and by two moments of applanation, one during inward corneal movement (A1) and one during outward corneal movement (A2). Because the cornea is viscoelastic, it dissipates some of the applied energy, and the corneal shape at the second applanation during the outward motion of the cornea is different from that at the first applanation (Fig. 1). Based on recorded images, the Corvis ST device provides various raw parameters on morphology, such as the flatness of the deformed cornea, stiffness of the cornea, velocity of the corneal apex movement, and the timing of A1, A2, and HC (Table 1). All parameters were calculated using the current version of the Corvis ST software (version 1.6r2223). Corvis ST also provided more intuitive parameters calculated using the raw parameters. For instance, “biomechanical IOP (bIOP)” is the estimated IOP corrected for ocular biomechanical parameters21; “integrated inverse radius” is the integration of curvature during the concave state of the cornea. A higher integrated inverse radius indicates steeper indentation of the cornea, suggesting a softer cornea22. “Stiffness parameter A1” (SP-A1) and “stress‒strain index” (SSI) are also Corvis ST’s parameters related to the stiffness of the cornea. SP-A1 is the ratio of loading on the cornea to its displacement at the first applanation:
where adjAP1 represents the adjusted air pressure on the cornea at the first applanation and A1DeflAmp represents displacement of the corneal apex at the first applanation. A higher SP-A1 value indicates a stiffer cornea as more loading is needed to flatten the cornea23. As the formula suggests, SP-A1 represents a secant elastic modulus at a single state of the cornea, and the nonlinear relationship among IOP, corneal morphology, and the elastic properties of the cornea are not considered in the formula4. As a result, SP-A1 largely depends on IOP and corneal geometry (e.g., CCT). In contrast, the SSI is a measure of the nonlinearity of this stress‒strain relationship of the eye (Fig. 2). More specifically, SSI was developed using finite element methods so that it represents the “stiffness of cornea as material” independent from IOP and corneal geometry24. The SSI is shown on a normalized scale, where the average value of 50-year-old eyes is equal to 1. Higher SSI values indicate stiffer and less deformable corneas. Corvis ST measurements were conducted 3 times, and the average values were used for the analysis. Based on the quality indicator "OK" displayed on the instrument monitor, only reliable Corvis ST measurements were used.
ORA measurement
Details of the ORA measurement have already been summarized elsewhere25. In brief, an air pulse emitted from the instrument deflects the cornea, and the cornea experiences two applanations. After a certain time from the moment of the first corneal applanation, the jet flow decreases. Because the cornea is viscoelastic, some energy is dissipated, and the air jet pressure at the second applanation (P2), where the cornea is moving outward, is lower than the pressure at the first applanation (P1). The difference in pressure at these two applanations (P1-P2) is called CH. CH reflects the energy dissipation of the cornea4,5,6. The ORA measurement was measured in triplicate. Only measurements with a quality index of > 6.5 were used, and the average value was used in the analysis.
Statistical analysis
Mean values of baseline clinical factors, Corvis ST, and ORA parameters were compared among the µLOT, iStent, and solo cataract groups with linear mixed models, where the patient was registered as a random effect because one or two eyes of a patient were included. The postoperative changes in GAT-IOP, Corvis ST and ORA parameters in each group were estimated using linear mixed models. P values were adjusted using the Benjamini‒Hochberg method for multiple comparisons.
All data processing and analyses were performed using the statistical programming language R (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Fifty-three eyes from 36 patients with OAG who had undergone µLOT surgery combined with cataract surgery, 59 eyes from 37 patients with OAG who had undergone iStent surgery combined with cataract surgery, and 62 eyes from 42 patients who had undergone solo cataract surgery were included in the study. In the µLOT group, 51 eyes of 34 patients had primary open-angle glaucoma (POAG), one eye had exfoliation glaucoma (EG), and one eye had steroid-induced glaucoma. In the iStent group, 56 eyes of 35 patients had POAG, and 3 eyes of 2 patients had EG.
Baseline characteristics as well as postoperative eye drop score and GAT-IOP of cases in each group are shown in Table 2. Age, axial length, CCT, and SP-A1 were similar among the 3 groups (all p > 0.05, linear mixed model with adjustment for multiple comparisons using the Benjamini‒Hochberg method). The baseline eye drop score was not significantly different between the µLOT and iStent groups (2.67 and 2.23 on average, respectively, p = 0.18). In contrast, the postoperative medication score was significantly higher in the µLOT group than in the iStent group at 3 (1.15 and 0.64 on average, respectively, p = 0.043) and 6 months (1.43 and 0.80 on average, respectively, p = 0.024). Baseline GAT-IOP was higher in the µLOT group than in the other two groups (p = 0.0018 and 0.023). On the other hand, GAT-IOP at 6 months postoperatively was similar among the 3 groups. Significantly lower CH, longer A1 and A2 time, smaller magnitude of A1 and A2 velocity, lower peak distance and deflection amplitude max were observed in the µLOT group than in the other two groups (all p < 0.05). In addition, the integrated inverse radius was significantly higher in the iStent group than in the solo cataract group (p = 0.016), and the SSI was significantly lower in the iStent group than in the other two groups (p = 0.047 and 0.0060, respectively).
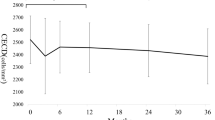
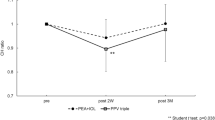
Postoperative changes at 3 and 6 months of GAT-IOP, Corvis ST, and ORA parameters in the µLOT group, iStent group, and solo cataract group are shown in Table 3 (A: µLOT group, B: iStent group and C: solo cataract group), whereas the comparisons of the postoperative changes at 6 months among the 3 groups are shown in Table 4. At 6 months postoperatively, eyes in both the μLOT and iStent groups exhibited significantly lower eye drop scores (− 1.00 and − 1.41, respectively, both p < 0.0001, linear mixed model with the adjustment for multiple comparisons using the Benjamini‒Hochberg method) compared to preoperatively, where there was no significant difference in the reduction of the scores between the two groups (p = 0.22, Table 4). GAT-IOP significantly decreased at 6 months postoperatively (− 3.11, − 1.39, and − 1.42 mmHg in the µLOT, iStent, and solo cataract groups, respectively, p < 0.0001, p = 0.015, and 0.00035, respectively) compared to preoperatively. The magnitude of GAT-IOP reduction at 6 months postoperatively was significantly greater in the µLOT group than in the iStent and solo cataract groups (p = 0.036 and 0.026, respectively, Table 4); however, there was no significant difference between the latter two groups (p = 0.96). bIOP also significantly decreased at 6 months postoperatively in all groups (− 2.12, − 1.15, and − 1.37 mmHg in the µLOT, iStent, and solo cataract groups, respectively, p < 0.0001, p = 0.0016, and p < 0.0001, respectively) compared to preoperatively, where there was no significant difference in the magnitudes of the bIOP reduction among the 3 groups (p = 0.18, 0.61, and 0.11, Table 4). CCT significantly increased at 6 months postoperatively in the µLOT group and iStent group (p = 0.0032 and 0.0016, respectively) but not in the solo cataract group (p = 0.77). CH showed a significant postoperative increase in the µLOT group (0.55 mmHg, p = 0.00026) but not in the iStent and solo cataract groups at 6 months postoperatively (− 0.19 and 0.21 mmHg, p = 0.54 and 0.19, respectively). There were different tendencies observed in the changes in Corvis ST parameters among the 3 groups; no significant changes in biomechanical parameters measured with Corvis ST were observed at 6 months postoperatively in the iStent group compared to preoperatively (Table 3). In contrast, in the µLOT and solo cataract groups, significant increases in A1 and A2 velocity, A2 time, peak distance, deflection amplitude max, and integrated inverse radius were observed at 6 months postoperatively compared to preoperatively; these changes indicated a more deformable cornea postoperatively. Consistent with this, significant decreases in SP-A1 and SSI were also observed in the µLOT (− 6.54 and − 0.20) and solo cataract (− 8.94 and − 0.06) groups at 3 and 6 months postoperatively (p = 0.019, p < 0.0001, p < 0.0001, and p = 0.018, respectively).
All of the patients in the µLOT and iStent groups were prescribed topical prostaglandin analogs with or without other topical anti-glaucomatous drugs preoperatively. At 6 months postoperatively, 45 of 53 eyes (84.9%) in the µLOT group and 26 of 59 eyes (44.1%) in the iStent group were prescribed some kind of antiglaucoma topical medication. In particular, at 6 months postoperatively, 32 of 53 eyes (60.4%) in the µLOT group and 18 of 59 eyes (30.5%) in the iStent group were prescribed topical prostaglandin analogs.
Discussion
In the current study, which included the matching of age and axial length among the three groups, postoperative changes in the corneal biomechanical properties measured with ORA and Corvis ST were examined in 112 OAG eyes that received cataract surgery combined with µLOT or iStent implantation and 62 eyes without OAG that received solo cataract surgery. As a result, a postoperative decrease in IOP was observed in all 3 groups. In addition, corneal stiffness (as suggested by the decrease in SP-A1 and SSI) decreased after µLOT and solo cataract surgery, whereas this was not the case in the iStent group.
Many studies have compared the biomechanical properties measured with Corvis ST between OAG eyes and normal eyes, providing different or partially contradictory results26,27,28,29,30,31,32. Many studies have found a longer A1/HC time, shorter A2 time, smaller magnitude of A1/A2 velocity, and smaller deformation amplitude (nearly equal to the deflection amplitude max plus posterior displacement of the whole eye) in POAG eyes than in normal eyes26,27,31. These reports indicated that corneas caved more slowly (longer A1/HC time and smaller A1 velocity) with smaller concavity (deflection amplitude max) and exhibited fast return to the initial state (shorter A2 time), which suggests stiffer corneas in OAG eyes than in normal controls. It should also be noted that all of these studies included treated OAG eyes. In contrast, it is also true that some case‒control studies have indicated softer corneas in OAG eyes. A softer cornea is represented by faster, greater and steeper indentation of the cornea, which corresponds to such parameters as smaller A1/HC/A2 time, greater peak distance, and larger integrated inverse radius and deflection amplitude ratio, respectively. Pillunat et al. found a smaller HC time and larger deflection amplitude ratio of the cornea at HC in treated normal tension glaucoma than in normal eyes28. Miki et al. reported a smaller A1/A2 time, larger peak distance, integrated inverse radius and deflection amplitude ratio in POAG eyes at the ‘treatment-naïve’ state than in normal eyes29. Another group also reported similar findings in treatment-naïve POAG30. These disagreements could partly be due to differences in the studied populations, such as disease subtype, IOP level, age, axial length, and the effect of antiglaucoma medications, all of which can affect Corvis ST measurements. Recently, Liu et al. conducted a meta-analysis of 15 case‒control studies, including the studies described above, reporting severe heterogeneities between the studies. They found lower A2 time and HC deformation amplitude suggestive of stiffer cornea in high-tension glaucoma (untreated IOP of more than 21 mmHg), whereas lower A1 time, HC time, and higher peak distance, suggestive of softer corneas, were observed in normal tension glaucoma than in normal controls32. In the current population at baseline, eyes in the µLOT group exhibited a significantly longer A1 time, shorter A2 time, smaller magnitude of A1 and A2 velocity, and deflection amplitude max than eyes in the solo cataract group, which are in agreement with the “stiffer cornea” findings in previous studies. This may be because the µLOT group included eyes with relatively high IOP (baseline GAT-IOP was 16.42 mmHg on average, Table 2); in a study on normal eyes, higher IOP was associated with the same direction of changes in A1/A2 time and the magnitude of A1/A2 velocity and deformation amplitude33. In contrast, a significantly higher integrated inverse radius and lower SSI were found in the iStent group than in the solo cataract group. The integrated inverse radius is the integral of the curvature of the cornea when it is concave, and the larger the value, the steeper the concavity of the cornea, suggesting a softer cornea. A lower SSI, a parameter of corneal stiffness independent of IOP24, also indicates softer corneas. These results are consistent with the “softer cornea” findings in normal tension glaucoma compared with normal controls that were previously reported32. Indeed, preoperative IOP was relatively low in the iStent group; this was similar to the solo cataract group while contrasting with the µLOT group.
Cataract surgery induces a reduction in IOP even in nonglaucomatous eyes (by 3.4 to 1.5 mmHg)34,35,36,37. In agreement with this, IOP was reduced by 1.42 and 1.37 mmHg for GAT-IOP and bIOP, respectively, in the solo cataract group (Table 3). The mechanism of the reduction in the IOP value following cataract surgery in nonglaucomatous eyes is yet to be fully understood; however, several mechanisms have been proposed. First, extraction of a thickened crystalline lens and implantation of a thinner intraocular lens changes the anatomic configuration of the anterior segment. Considerable lens volume reduction results in widening of the angle and facilitates aqueous outflow in eyes with relatively narrow angles34. It is also postulated that as the lens thickens, posterior traction on the scleral spur by the anterior lens zonules weakens and decreases outflow facility37,38. Cataract surgery may relieve this condition. Second, trabecular endothelium remodeling or metalloproteinase production may be induced due to stress from ultrasonic vibrations or high IOP during phacoemulsification, resulting in increased outflow facility39,40. In addition to these mechanisms for the “true” IOP reduction, other researchers using the Corvis ST measurements have proposed that the more deformable postoperative cornea was another reason2,22,41. In a prospective randomized trial41 that involved 93 normal eyes that underwent cataract surgery, it was found that bIOP and SP-A1 were decreased, whereas A1 and A2 velocity and deflection amplitude at HC were increased at 3 months postoperatively. In agreement with this, we observed significant increases in A1 and A2 velocity, peak distance, and deflection amplitude max postoperatively in the solo cataract group, suggesting a more deformable cornea in these eyes. Furthermore, two corneal stiffness-related parameters (SP-A1 and SSI) were decreased at 3 and 6 months postoperatively in the solo cataract group. SP-A1 is the ratio of the amount of stress over displacement of the cornea at the first applanation. Although SP-A1 is linearly corrected for bIOP (see the formula in “Methods”), it still depends on IOP because of the nonlinear material property of the cornea. In other words, the elastic modulus of the cornea depends on the external stress (i.e., IOP), which means that a higher IOP makes the cornea even less deformable than predicted by a simple linear stress‒strain relationship. On the other hand, SSI is a parameter of corneal stiffness that arises purely from material status and is independent of IOP24. The nonlinear stress‒strain property of an elastic material is represented as the steepness of the stress‒strain curve (Fig. 2), and the SSI is a parameter of the steepness. This parameter is calculated based on the results of the finite-element model experiment in which biomechanical responses of eyes were analyzed at different IOP levels. As a result, the reduction in SSI in the solo cataract group indicates a more deformable cornea independent of IOP. Thus, the decrease in both SP-A1 and SSI in the solo cataract surgery group suggested that the cornea becomes more deformable, even independent of the decrease in IOP. This is clinically very important when analyzing the effect of cataract surgery on glaucoma because the result is a possible underestimation of IOP after cataract surgery, as discussed above, and there is no settlement on whether postoperative IOP reduction is preventive against glaucoma progression. For instance, some previous reports have suggested that the rate of visual field progression does not change after cataract surgery in OAG eyes despite a decrease in IOP42,43. Furthermore, Kim et al. reported that visual field progression is faster after cataract surgery than preoperatively, which was attributed to postoperative IOP spikes14. These reports raise the question of whether the target IOP of the treatment should be altered after cataract surgery in OAG patients. Indeed, we previously reported that postoperative IOP reduction may not entirely be a true IOP reduction but may be the result of postoperative biomechanical changes, such as corneal softening15. The present study indicates that a similar finding can be observed in post-MIGS (µLOT) eyes; the cornea became more deformable in the µLOT group than in the solo cataract group as suggested by the higher reduction in SSI, deflection amplitude max, and peak distance (Table 4).
In the iStent group, there was a significant reduction in IOP following the surgery (− 1.39 mmHg at 6 months on average, Table 4), similar to the solo cataract group. Of note, SP-A1 and SSI were not significantly changed postoperatively in the iStent group, in contrast to the solo cataract group, which implies that the IOP reduction was not the result of the more deformable cornea. The magnitudes of IOP reduction were similar between the solo cataract and iStent groups (− 1.39 and − 1.42 mmHg, respectively, Table 4); however, this finding was associated with the reduction in medications in the iStent group (2.23 at baseline and 0.80 at 6 months postoperatively). These findings imply that the “reduction of IOP reading” was more due to “true IOP reduction” in the iStent group than in the solo cataract group. Whether this IOP reduction is associated with prevention of VF progression in glaucoma is a matter for further investigation in future studies.
Both iStent and µLOT are glaucoma surgeries targeted at facilitating aqueous outflow by decreasing the resistance of the trabecular meshwork; however, different findings were observed between their postoperative biomechanical properties. First, the magnitude of postoperative IOP reduction was significantly greater with µLOT than with iStent (− 3.11 and − 1.39 mmHg at 6 months postoperatively, Table 3B and C). However, one cannot simply draw a conclusion that µLOT is more effective than iStent in reducing IOP because preoperative IOP was also significantly different between the two groups (16.42 vs. 14.66 mmHg). Moreover, it should be noted that eyes in the μLOT group had a significantly higher postoperative eye drop score than those in the iStent group (1.43 vs. 0.80). Postoperative topical medication usage was sometimes resumed at the discretion of physicians to reach IOP targets. The relative contribution of antiglaucomatous medications to postoperative IOP reduction might be larger in the μLOT group than in the iStent group. In addition, unlike in the iStent group, both SP-A1 and SSI were significantly decreased postoperatively in the µLOT group, which suggests a more deformable cornea. The reason for this difference is not entirely clear; however, a few possible reasons may be applicable. First, the different changes in the Corvis ST parameters between the µLOT and iStent groups may be due to the different MIGS procedures. The resistance to aqueous humor outflow in the trabecular meshwork may be associated with the IOP rise during biomechanical measurements (induced by a sudden external force applied to the cornea). The trabecular meshwork has been reported to be stiffer and more resistant to external stress in eyes with glaucoma44. µLOT removes this resistance in a wider angle compared to iStent, and hence, an eye is likely to be less resistant to IOP increase when an external stress (air-puff) is applied in the former case. Additionally, removing a part of the trabecular meshwork, which may provide mechanical support for the limbal tissue, in the µLOT group could lead to a more deformable cornea postoperatively. The second possible reason is the effect of discontinuation of antiglaucoma medications. Antiglaucoma medications have significant effects on the biomechanical properties of ocular tissue, not only IOP. In particular, topical prostaglandin analogs induce corneal thinning45,46,47 and corneal softening27,48, probably through the activation of matrix metalloproteinase49. Yasukura et al. reported greater corneal compliance after prostaglandin analog use in glaucomatous eyes50. Wu et al. reported higher deflection amplitude measured with Corvis ST in POAG patients using topical prostaglandin analogs than in treatment-naïve POAG patients27. In the current study, all topical antiglaucoma medications, including prostaglandin analogs, were discontinued once postoperatively, and the corneal softening effect of the surgery may have been offset by the effect of discontinuing the use of topical prostaglandin analogs. At 6 months, most patients in the iStent group had not resumed usage of topical prostaglandin analogs at 6 months (18 eyes (30.5%) used topical prostaglandin analogs), whereas this was not the case in the µLOT group (32 eyes (60.4%) used topical prostaglandin analogs). This difference would have led to more pronounced corneal softening in the µLOT group than in the iStent group.
CH is a biomarker for the damping capacity of the cornea and is associated with the development7, severity8, and progression of glaucoma9,10. To our knowledge, changes in CH following the MIGS procedure combined with cataract surgery have yet to be described. In the current study, CH increased postoperatively at 6 months only in the µLOT group. In general, CH is negatively correlated with IOP51. Two groups found increased CH after trabeculectomy, where the magnitude of IOP reduction was 12.9 and 13.6 mmHg, respectively52,53. Another study reported increased CH after selective laser trabeculoplasty, which was discussed as a result of the reduced IOP (by 3.2 mmHg)54. However, another previous study55 reported unchanged CH 6 months after solo cataract surgery in glaucoma patients. In contrast, both in the iStent and solo cataract groups, no significant change in CH was observed at 3 and 6 months postoperatively. The change of CH in microLOT group in the current study can be considered as the result of both cataract surgery (corneal incision and replacement to IOL) and incision of trabecular meshwork. Previous studies indicated a larger postoperative change in CH after cataract surgery performed with a larger incision56,57, suggesting that surgical incision of the cornea affects corneal biomechanical properties. It is also possible that the small amounts of IOP reduction (less than 2 mmHg in GAT-IOP) in the iStent and solo cataract groups were not large enough to induce a detectable CH change in these groups. Another possible reason for this difference would be an effect of discontinuing antiglaucoma medications, particularly prostaglandin analogs. There are conflicting findings on the effect of topical prostaglandin analogs on CH. Tsikripis et al., in a randomized controlled trial, reported an increase in CH following the initiation of treatment with prostaglandin analogs in POAG patients58. In contrast, Meda et al., in a prospective case‒control study, reported a significant increase in CH after cessation of treatment with topical prostaglandin analogs59. In the current study, usage of antiglaucomatous medications was discontinued in many cases in the iStent and µLOT groups. Thus, the bias arising from the discontinuation of antiglaucoma medication usage on the postoperative change in CH could not be completely avoided in these groups.
CCT increased significantly at 6 months postoperatively in the µLOT and iStent groups (by 5.23 and 7.33 µm, respectively). This change is possibly due to corneal edema caused by surgically induced inflammation and the postoperative discontinuation of prostaglandin analogs45,46,47. Possibly, the latter effect may be more influential because the increase of CCT was not observed in the solo cataract group, and no considerable difference would be conceived in the postoperative corneal inflammation between the solo cataract surgery and iStent and µLOT surgeries. It has been reported that the GAT-IOP reading increased by approximately 0.32 mmHg per 10 μm increase in CCT60. In the current population, postoperative GAT-IOP reductions in the µLOT and iStent groups were − 3.11 and − 1.39 mmHg, respectively, which implies that all of them cannot be explained only by the increase in CCT (7.33 and 5.23 μm, respectively). The decrease in bIOP (IOP corrected for CCT21) also supports this speculation that the IOP reduction in both groups is independent of the change in CCT.
The present study has some limitations. The population was relatively small, and further validation of the current result in a larger dataset is needed. The second limitation arises from the nature of retrospective studies. Moreover, a future study should be conducted to assess the differences across different types of MIGS, such as 360-degree suture or Kahook dual-brade trabeculotomy61. µLOT and iStent implantation facilitate aqueous outflow by decreasing the resistance of the trabecular meshwork; however, it is not possible to separate the effect of µLOT and iStent implantation themselves on biomechanical properties from that of biomechanical property changes associated with cataract surgery because these MIGS techniques were performed in combination with cataract surgery; indeed, solo iStent surgery is not allowed in Japan62. Research should be conducted to compare the effect of solo-MIGS surgery in preparing such cases in the future. Additionally, the solo-cataract group, consisting of non-OAG patients without PGA usage, had different baseline characteristics compared to the other two groups, which consisted of OAG patients using PGA, which could affect corneal biomechanical properties. Comparing solo-cataract surgery with MIGS surgery in OAG patients might yield different results.
In conclusion, the current study suggested that corneas becomes more deformable after µLOT combined with cataract surgery in OAG eyes and cataract surgery in non-OAG eyes. These results indicate that "reduced IOP reading" after MIGS is influenced by changes in corneal biomechanics other than true IOP reduction and changes in the use of topical antiglaucoma medications. Such a finding was not observed with iStent combined with cataract surgery in OAG eyes.
Data availability
All data is available if requested to the corresponding author.
References
Kaushik, S., Pandav, S. S., Banger, A., Aggarwal, K. & Gupta, A. Relationship between corneal biomechanical properties, central corneal thickness, and intraocular pressure across the spectrum of glaucoma. Am. J. Ophthalmol. 153, 840-849.e2 (2012).
Liu, J. & Roberts, C. J. Influence of corneal biomechanical properties on intraocular pressure measurement: Quantitative analysis. J. Cataract Refract. Surg. 31, 146–155 (2005).
Burgoyne, C. F., Downs, J. C., Bellezza, A. J., Suh, J. K. & Hart, R. T. The optic nerve head as a biomechanical structure: A new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage. Prog. Retin. Eye Res. 24, 39–73 (2005).
Roberts, C. J. Concepts and misconceptions in corneal biomechanics. J. Cataract Refract. Surg. 40, 862–869 (2014).
Dupps, W. J. Jr. Hysteresis: New mechanospeak for the ophthalmologist. J. Cataract Refract. Surg. 33, 1499–1501 (2007).
Luce, D. A. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J. Cataract Refract. Surg. 31, 156–162 (2005).
Susanna, C. N. et al. A prospective longitudinal study to investigate corneal hysteresis as a risk factor for predicting development of glaucoma. Am. J. Ophthalmol. 187, 148–152 (2018).
Hirasawa, K. et al. Association between corneal biomechanical properties with ocular response analyzer and also corvisST tonometry, and glaucomatous visual field severity. Transl. Vis. Sci. Technol. 6, 18 (2017).
Medeiros, F. A. et al. Corneal hysteresis as a risk factor for glaucoma progression: A prospective longitudinal study. Ophthalmology 120, 1533–1540 (2013).
De Moraes, C. V., Hill, V., Tello, C., Liebmann, J. M. & Ritch, R. Lower corneal hysteresis is associated with more rapid glaucomatous visual field progression. J. Glaucoma 21, 209–213 (2012).
Matsuura, M. et al. The usefulness of CorvisST tonometry and the ocular response analyzer to assess the progression of glaucoma. Sci. Rep. 7, 40798 (2017).
Miglior, S. et al. Predictive factors for open-angle glaucoma among patients with ocular hypertension in the European glaucoma prevention study. Ophthalmology 114, 3–9 (2007).
Gordon, M. O. et al. The ocular hypertension treatment study: Baseline factors that predict the onset of primary open-angle glaucoma. Arch. Ophthalmol. 120, 714–720 (2002).
Kim, J. H. et al. Cataract surgery and rate of visual field progression in primary open-angle glaucoma. Am. J. Ophthalmol. 201, 19–30 (2019).
Aoki, S. et al. Comment on cataract surgery and rate of visual field progression in primary open-angle glaucoma. Am. J. Ophthalmol. 209, 216–217 (2020).
Yang, S. A. et al. Trends and usage patterns of minimally invasive glaucoma surgery in the United States: IRIS® registry analysis 2013–2018. Ophthalmol. Glaucoma 4, 558–568 (2021).
Fujita, A., Hashimoto, Y., Matsui, H., Yasunaga, H. & Aihara, M. Recent trends in glaucoma surgery: A nationwide database study in Japan, 2011–2019. Jpn. J. Ophthalmol. 66, 183–192 (2022).
Anderson, D. R. & Patella, V. M. Automated Static Perimetry 2nd edn. (Mosby, 1999).
Japanese Guidelines. Japanese guidelines for use of iStent(R) trabecular micro bypass in combination with cataract surgery. Nippon Ganka Gakkai Zasshi 120, 494–497 (2016).
Koprowski, R. Automatic method of analysis and measurement of additional parameters of corneal deformation in the Corvis tonometer. Biomed. Eng. 13, 150 (2014).
Joda, A. A., Shervin, M. M., Kook, D. & Elsheikh, A. Development and validation of a correction equation for Corvis tonometry. Comput. Methods Biomech. Biomed. Eng. 19, 943–953 (2016).
Hirasawa, K. et al. Changes in corneal biomechanics and intraocular pressure following cataract surgery. Am. J. Ophthalmol. 195, 26–35 (2018).
Roberts, C. J. et al. Introduction of two novel stiffness parameters and interpretation of air puff-induced biomechanical deformation parameters with a dynamic scheimpflug analyzer. J. Refract. Surg. 2017(33), 266–273 (1995).
Eliasy, A. et al. Determination of corneal biomechanical behavior in-vivo for healthy eyes using CorVis ST tonometry: Stress–strain index. Front. Bioeng. Biotechnol. 7, 105 (2019).
Matsuura, M. et al. The relationship between corvis ST tonometry and ocular response analyzer measurements in eyes with glaucoma. PLoS ONE 11, e0161742 (2016).
Wang, W., Du, S. & Zhang, X. Corneal deformation response in patients with primary open-angle glaucoma and in healthy subjects analyzed by corvis ST. Investig. Ophthalmol. Vis. Sci. 56, 5557–5565 (2015).
Wu, N. et al. Changes in corneal biomechanical properties after long-term topical prostaglandin therapy. PLoS ONE 11, e0155527 (2016).
Pillunat, K. R., Herber, R., Spoerl, E., Erb, C. & Pillunat, L. E. A new biomechanical glaucoma factor to discriminate normal eyes from normal pressure glaucoma eyes. Acta Ophthalmol. 97, e962–e967 (2019).
Miki, A. et al. Dynamic scheimpflug ocular biomechanical parameters in untreated primary open angle glaucoma eyes. Investig. Ophthalmol. Vis. Sci. 61, 19–19 (2020).
Wu, N., Chen, Y. & Sun, X. Association between ocular biomechanics measured with corvis ST and glaucoma severity in patients with untreated primary open angle glaucoma. Transl. Vis. Sci. Technol. 11, 10–10 (2022).
Silva, N. et al. Corneal biomechanics for ocular hypertension, primary open-angle glaucoma, and amyloidotic glaucoma: A comparative study by corvis ST. Clin. Ophthalmol. 16, 71–83 (2022).
Liu, M. X. et al. Corneal Biomechanics in primary open angle glaucoma and ocular hypertension: A systematic review and meta-analysis. J. Glaucoma 32, e24–e35 (2022).
Miki, A. et al. Factors associated with corneal deformation responses measured with a dynamic scheimpflug analyzer. Investig. Ophthalmol. Vis. Sci. 58, 538–544 (2017).
Melancia, D., Abegão Pinto, L. & Marques-Neves, C. Cataract surgery and intraocular pressure. Ophthalm. Res. 53, 141–148 (2015).
Lv, H. et al. Changes of intraocular pressure after cataract surgery in myopic and emmetropic patients. Medicine 97, e12023 (2018).
Slabaugh, M. A. & Chen, P. P. The effect of cataract extraction on intraocular pressure. Curr. Opin. Ophthalmol. 25, 122–126 (2014).
Poley, B. J., Lindstrom, R. L., Samuelson, T. W. & Schulze, R. Jr. Intraocular pressure reduction after phacoemulsification with intraocular lens implantation in glaucomatous and nonglaucomatous eyes: Evaluation of a causal relationship between the natural lens and open-angle glaucoma. J. Cataract Refract. Surg. 35, 1946–1955 (2009).
Johnstone, M. A. The aqueous outflow system as a mechanical pump: Evidence from examination of tissue and aqueous movement in human and non-human primates. J. Glaucoma 13, 421–438 (2004).
Wang, N., Chintala, S. K., Fini, M. E. & Schuman, J. S. Ultrasound activates the TM ELAM-1/IL-1/NF-kappaB response: A potential mechanism for intraocular pressure reduction after phacoemulsification. Investig. Ophthalmol. Vis. Sci. 44, 1977–1981 (2003).
Tumminia, S. J. et al. Mechanical stretch alters the actin cytoskeletal network and signal transduction in human trabecular meshwork cells. Investig. Ophthalmol. Vis. Sci. 39, 1361–1371 (1998).
Wallace, H. B., Misra, S. L., Li, S. S. & McKelvie, J. Biomechanical changes in the cornea following cataract surgery: A prospective assessment with the corneal visualisation Scheimpflug technology. Clin. Exp. Ophthalmol. 47, 461–468 (2019).
Carrillo, M. M., Artes, P. H., Nicolela, M. T., LeBlanc, R. P. & Chauhan, B. C. Effect of cataract extraction on the visual fields of patients with glaucoma. Arch. Ophthalmol. 123, 929–932 (2005).
Su, W. W. et al. Comparison of visual field progression rate before and after cataract surgery in patients with open-angle and angle-closure glaucoma. J. Ophthalmol. 2021, 7655747 (2021).
Last, J. A. et al. Elastic modulus determination of normal and glaucomatous human trabecular meshwork. Investig. Ophthalmol. Vis. Sci. 52, 2147–2152 (2011).
Jang, M., Kang, K. E. & Cho, B. J. Effect of prostaglandin analogues on central corneal thickness: 3-year follow-up results. Korean J. Ophthalmol. 34, 347–352 (2020).
Park, J. H., Yoo, C., Chung, H. W. & Kim, Y. Y. Effect of prostaglandin analogues on anterior scleral thickness and corneal thickness in patients with primary open-angle glaucoma. Sci. Rep. 11, 11098 (2021).
Kadri, R. et al. Effect of prostaglandin analogues on central corneal thickness in patients with glaucoma: A systematic review and meta-analysis with trial sequential analysis. Indian J. Ophthalmol. 70, 1502–1512 (2022).
Jung, Y., Suh, H. & Moon, J. I. Differential impact of prostaglandin analogues on agreement of intraocular pressure measurements obtained by Goldmann applanation, rebound, and noncontact tonometry. BMC Ophthalmol. 21, 436 (2021).
Bergonzi, C. et al. Evaluation of prostaglandin analogue effects on corneal keratocyte density using scanning laser confocal microscopy. J. Glaucoma 19, 617–621 (2010).
Yasukura, Y., Miki, A., Maeda, N., Koh, S. & Nishida, K. Effect of prostaglandin analogues on corneal biomechanical parameters measured with a dynamic scheimpflug analyzer. J. Glaucoma 30, 996–1000 (2021).
Touboul, D. et al. Correlations between corneal hysteresis, intraocular pressure, and corneal central pachymetry. J. Cataract Refract. Surg. 34, 616–622 (2008).
Pakravan, M., Afroozifar, M. & Yazdani, S. Corneal biomechanical changes following trabeculectomy, phaco-trabeculectomy, ahmed glaucoma valve implantation and phacoemulsification. J. Ophthalm. Vis. Res. 9, 7–13 (2014).
Konstantinidis, A. et al. The effect of antiglaucoma procedures (trabeculectomy vs Ex-PRESS glaucoma drainage implant) on the corneal biomechanical properties. J. Clin. Med. 10, 1–10 (2021).
Pillunat, K. R., Spoerl, E., Terai, N. & Pillunat, L. E. Effect of selective laser trabeculoplasty on corneal biomechanics. Acta Ophthalmol. 94, e501–e504 (2016).
Zehavi-Dorin, T. et al. Repeatability of corneal hysteresis measurements in glaucoma patients during routine follow up and after cataract surgery. J. Glaucoma 31, 590–594 (2022).
Zhang, Z. et al. Corneal biomechanical properties changes after coaxial 2.2-mm microincision and standard 3.0-mm phacoemulsification. Int. J. Ophthalmol. 9, 230–234 (2016).
Alió, J. L., Agdeppa, M. C., Rodríguez-Prats, J. L., Amparo, F. & Piñero, D. P. Factors influencing corneal biomechanical changes after microincision cataract surgery and standard coaxial phacoemulsification. J. Cataract Refract. Surg. 36, 890–897 (2010).
Tsikripis, P., Papaconstantinou, D., Koutsandrea, C., Apostolopoulos, M. & Georgalas, I. The effect of prostaglandin analogs on the biomechanical properties and central thickness of the cornea of patients with open-angle glaucoma: A 3-year study on 108 eyes. Drug Des. Dev. Therapy 7, 1149–1156 (2013).
Meda, R., Wang, Q., Paoloni, D., Harasymowycz, P. & Brunette, I. The impact of chronic use of prostaglandin analogues on the biomechanical properties of the cornea in patients with primary open-angle glaucoma. Br. J. Ophthalmol. 101, 120–125 (2017).
Wei, W. et al. Correlation analysis between central corneal thickness and intraocular pressure in juveniles in Northern China: The Jinan city eye study. PLoS ONE 9, e104842 (2014).
Seibold, L. K., Soohoo, J. R., Ammar, D. A. & Kahook, M. Y. Preclinical investigation of ab interno trabeculectomy using a novel dual-blade device. Am. J. Ophthalmol. 155, 524-529.e2 (2013).
Japanese Guidelines. Japanese guidelines for use of iStent trabecular micro bypass in combination with cataract surgery. Nippon Ganka Gakkai Zasshi 120(7), 494–497 (2016).
Acknowledgements
This study was supported by grants (Numbers 19H01114, 18KK0253, 20K09784, and 21K16870) from the Ministry of Education, Culture, Sports, Science and Technology of Japan; the Translational Research Program; the Strategic Promotion for Practical Application of Innovative Medical Technology (TR-SPRINT) from the Japan Agency for Medical Research and Development (AMED); and the Japan Glaucoma Society Research Project Support Program.
Author information
Authors and Affiliations
Contributions
Y.K., R.A., S.N., and H.M. conceptualized and designed the work. Y.F. and R.A. conducted measurement and Y.F. and S.A. analyzed data. S.A. wrote and R.A. revised the main manuscript text and S.A. prepared Figs. 1 and 2. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aoki, S., Asaoka, R., Fujino, Y. et al. Comparing corneal biomechanic changes among solo cataract surgery, microhook ab interno trabeculotomy and iStent implantation. Sci Rep 13, 19148 (2023). https://doi.org/10.1038/s41598-023-46709-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46709-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.