Abstract
Background/objectives
To investigate changes in corneal endothelial cell density (CECD) after initial Ex-PRESS surgery in Japanese patients with open-angle glaucoma (OAG) followed-up for 36 months.
Subjects/methods
Corneal specular microscopy was used to examine preoperative and postoperative (3, 6, 12, 24 and 36 months) CECD and CECD changes were analysed. Kaplan–Meier survival curve was used to examine CECD maintained at 95% level, and Cox proportional hazards model was used to detect the risk factors for CECD loss. Intraocular pressure (IOP) changes during the course were also examined.
Results
A total of 79 eyes of 79 patients (standalone surgery, 24 cases; combined cataract surgery, 55 cases) were investigated. Preoperative CECD (mean ± SD) was 2521 ± 305 cells/mm² and 2429 ± 366 (P = 0.003, adjusted for Bonferroni correction), 2462 ± 332 (P = 0.002), 2457 ± 317 (P < 0.001), 2433 ± 333 (P < 0.001), and 2387 ± 352 (P < 0.001) at 3, 6, 12, 24 and 36 months, respectively. The decrease rate was calculated as 1.8%/year. Further, 95% maintenance CECD at 36 months was 50.0% (95% confidence interval, 37.1–63.0%). Both univariate and multivariate Cox proportional hazard models showed that a low preoperative CECD was a significant risk factor for CECD loss. Baseline IOP of 19.3 ± 5.8 mmHg decreased at all measurement points (P < 0.001) after surgery.
Conclusion
CECD after initial Ex-PRESS surgery in 36 months might not be clinically problematic. However, longer-term follow-up is necessary, and regular CECD measurement should be performed, especially in patients with low CECD.
Similar content being viewed by others
Introduction
The ultimate goal of glaucoma treatment is not to lower intraocular pressure (IOP) but to maintain visual function; however, the only treatable factor among certain risk factors involved in glaucoma progression is IOP [1, 2]. Some clinical studies have reported that reduction in IOP from 20% to 30% from untreated IOP (i.e., baseline IOP) could lead to the inhibition of glaucoma progression [3, 4]. Among some methods to lower IOP, such as eye drops, lasers and surgeries, filtering surgery is presently the most powerful and effective. For more than a quarter of a century, filtering surgery means trabeculectomy (with antimetabolite), which has been the gold standard for glaucoma surgery as a procedure that can be performed for any type of glaucoma [5].
The Ex-PRESS drainage device implantation surgery (Alcon, Fort Worth, Texas, USA) is another type of filtering surgery, which was approved in Japan in December 2011. It differs from trabeculectomy in that it allows the creation of a filtration bleb without any internal eye manipulation [6]. This device can be inserted through the deep scleral bed into the anterior chamber, allowing the anterior aqueous humour to pass under the subconjunctival. Although it demonstrates almost the same IOP-lowering effect as conventional trabeculectomy, it is less likely to cause postoperative low IOP (hypotony) because it is continuously filtered at a constant rate, resulting in faster visual function recovery than trabeculectomy [7,8,9]. Thus, this procedure is favourably selected in the eye with easy collapses, such as eyes with no vitreous body after vitrectomy surgery.
One of the long-term complications related to trabeculectomy that should be considered in addition to the IOP-lowering effect in corneal endothelial cell density (CECD) damage [8]. In Japan, trabeculectomy is reported to be the third leading cause of bullous keratopathy [10]. Regarding Ex-PRESS, some reports showed a significant decrease in CECD [11, 12]; however, in the comparative study of postoperative CECD damage in trabeculectomy and Ex-PRESS, some reports showed less damage with Ex-PRESS [13, 14], whereas others showed vice versa [15, 16].
The long-term course of CECD regularly examined for more than 24 months after Ex-PRESS has not been reported to date. In light of the current widespread use of Ex-PRESS in glaucoma surgery, this study aimed to examine the changes in CECD in patients with open-angle glaucoma (OAG) who underwent initial Ex-PRESS and were regularly followed-up for 36 months and to elucidate its relating factors.
Materials/subjects and methods
The medical records of Japanese patients with glaucoma who underwent an initial Ex-PRESS at Yotsuya Shirato Eye Clinic (Tokyo, Japan) between March 2014 and June 2016 were evaluated. All protocols and methods adhered to the tenets of the Declaration of Helsinki, and the ethics committee of Riverside Internal Medicine Cardiology Clinic (approval ID: RSC-1811RB01) approved this study. As this was a retrospective study, informed consent was waived by the Research Ethics Board.
The patient selection criteria were as follows: (1) primary OAG, (2) those who underwent Ex-PRESS alone or combined surgery and could be followed-up for 36 months, and (3) eyes with no contact of the Ex-PRESS tip with the corneal endothelium confirmed by gonioscope during the course. The exclusion criteria were as follows: (1) primary angle-closure glaucoma, pseudoexfoliation (PE) glaucoma, and secondary glaucoma caused by uveitis, (2) history of laser iridotomy or intraocular lens implantation, and (3) eyes that underwent another glaucoma surgery after Ex-PRESS surgery. We excluded PE glaucoma because patients with PE have lower CECD [17, 18], and uveitis is reported to be a prognostic factor for decreasing CECD after trabeculectomy [19].
Ophthalmic examinations
Slit-lamp examination using gonioscopy had a four-mirror lens (AU-810-4, Ocular), and fundus examinations were routinely conducted at each visit. A calibrated Goldmann applanation tonometer (Haag-Streit, Germany) was used to measure IOP during office hours after administering topical anaesthesia. A corneal specular microscope (EM-3000, TOMEY CORPORATION) was used to examine preoperative (baseline) and postoperative (3, 6, 12, 24 and 36 months) CECD for both the eyes. CECD of the central cornea was used as the mean number of CECD. An autorefractor keratometer (ARK-900, Nidek) was used to measure refractive error.
Surgical technique
Ex-PRESS surgery (including combined surgery) was performed by two well-trained surgeons (SS and MA). The surgical technique was as follows: after instilling anaesthesia into the sub-Tenon space, a 5- to 6-mm fornix-based conjunctival incision was made along the limbus at the temporal or nasal side. This process was followed by cauterization, formation of a single rectangular scleral flap, soaking with 0.05% mitomycin C (MMC) for 1.5 min, and washout of residual MMC with 100 mL of a balanced salt solution). A 25-gauge needle was inserted from the scleral floor to the anterior chamber at the anatomical ring (grey zone), followed by Ex-PRESS insertion, release, and fixation at the same site. Then, placement of two or three 10-0 nylon scleral flap sutures, adjustment of aqueous humour flow with an occasional additional suture, and placement of a wing conjunctival suture with ophthalmic 10-0 nylon sutures (MANI, Utsunomiya, Japan) were performed. In combined cataract surgery cases, a clear corneal incision was made at the superior quadrant with viscoelastic materials [Viscoat 0.5 Ophthalmic Viscoelastic Substance (Alcon, Tokyo, Japan) and 1% Healon Ophthalmic Viscoelastic Substance (AMO, Tokyo, Japan)] using the soft-shell technique. Postoperative medical treatment consisted of four applications of 0.1% betamethasone and moxifloxacin ophthalmic solution. For the combined surgery, two applications of diclofenac sodium ophthalmic solution were added. If IOP was elevated after the surgery, either laser suture lysis (Blumenthal suture lysis lens, Volk) or bleb needling was performed at the surgeon’s discretion to increase the flow rate of the aqueous humour.
Statistical analysis
The first operated eye was selected if both the eyes met the inclusion criteria. The amount of change in CECD after Ex-PRESS surgery was the main evaluation item. A linear mixed model was chosen because the same examination was repeated in the same patient so CECD measurements correlated with each other [20]. The percentage decrease in CECD was calculated as follows: 3-year reduction rate (%) = [(baseline CECD number − final CECD number)/baseline CECD number] × 100 followed by mean annual reduction rate (%/year) = 3-year decrease rate (%)/3 years. Death was defined as a 5% decrease in the number of CECD from baseline CECD, and CECD survival rate at 36 months was examined by Kaplan–Meier survival curve. A log-rank test was used to compare the differences in the surgical methods between single and combined surgeries. Based on these criteria, univariate and multivariate Cox proportional hazard models were used for risk factor analysis for CECD loss. The covariates were age, surgical technique (single or combined), refraction, baseline IOP, baseline CECD (binarization process was performed to determine whether baseline CECD was larger or smaller than 2000 cells/mm², which was considered to be the lower limit of normal and was used in the Cox model), postoperative mean IOP, postoperative IOP fluctuation (defined as standard deviation), number of needling, and number of laser suture lysis. Factors associated with P values < 0.2 for univariate analysis were subjected to multivariate analysis. Finally, the change in IOP during the course was evaluated by analysis of variance performed using a mixed model.
JMP Pro (version 16.0, SAS Institute, Cary, NC, USA) and IBM SPSS Statistics (version 23.0, IBM Corp., Armonk, NY, USA) software were used for all statistical analyses. P < 0.05 was considered statistically significant unless otherwise specified.
Results
In this study, we included 79 eyes of 79 patients (46 males, 33 females), with a mean age of 63.3 ± 11.0 years. The patient characteristics are presented in Table 1. A total of 24 eyes had undergone standalone Ex-PRESS surgery (single), and the other 55 eyes had undergone Ex-PRESS surgery with combined cataract surgery (combined).
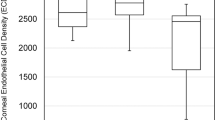
The overall mean CECD ( ± standard deviation: SD) was 2521 ± 305 cells/mm² at baseline (N = 79) and 2429 ± 366 cells/mm² (N = 59) (P = 0.003, adjusted for Bonferroni correction) (95% confidence interval (CI) of the mean difference from the baseline: 13.6–108.4 cells/mm²) at 3 months, 2462 ± 332 cells/mm² (N = 73) (P < 0.001) (95% CI: 14.4–103.9 cells/mm²) at 6 months, 2457 ± 317 cells/mm² (N = 75) (P < 0.001) (95% CI: 33.3–122.1 cells/mm²) at 12 months, 2433 ± 333cells/mm² (N = 72) (P = 0.001) (95% CI: 49.4–139.3 cells/mm²) at 24 months, and 2387 ± 352 cells/mm² (N = 79) (P < 0.001) (95% CI: 89.9–177.2 cells/mm²) at 36 months (Fig. 1). The decrease rate was calculated as 1.8%/year. From baseline to 3 months, a significant decrease was observed in the amount of CECD, but there was no subsequent significant difference in the amount of change of CECD between each measurement (P ≥ 0.155).
The horizontal axis represents the time course (months) and the vertical axis represents the corneal endothelial cell density (CECD: cells/mm²). Error bar represents the 95% confidential interval. A significant decrease was found in CECD at 12, 24 and 36 months compared with baseline. *P = 0.015, **P = 0.001 and ***P < 0.001.
In patients who underwent combined cataract surgery, a significant decrease in CECD was observed after 6 months. No significant decrease was observed in patients who underwent single surgery until 24 months; however, it showed a significant decrease at 36 months (Table 2).
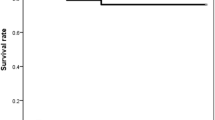
In the cumulative Kaplan–Meier survival analysis, the survival rate of 95% of CECD from baseline was 50.0% (95% CI, 37.1–63.0) at 36 months (Fig. 2a). The survival rate was 48.4% (95% CI, 32.8–62.9) with combined cataract surgery and 54.8% (95% CI, 32.0–77.6) with single surgery (Fig. 2b). No significant difference was found between the surgical methods (P = 0.61, log-rank test). Among single Ex-PRESS surgery (24 eyes), the survival rate for phakic eyes (16 eyes) and pseudophakic eyes (18 eyes) were 50.0% and 25.8%, respectively, with no significant difference between them (P = 0.47, log-rank test).
a Kaplan–Meier survival analysis based on the definition of maintaining 95% CECD in all cases. The horizontal axis represents the time course (months) and the vertical axis represents the survival rate. Error bar represents the 95% confidential interval at each point. b Kaplan–Meier survival analysis based on the definition of maintaining 95% CECD divided by the surgical technique. The horizontal axis represents the time course (months) and the vertical axis represents the survival rate. Green line indicates combined cataract surgery and blue line indicates single surgery, with no difference between them (P = 0.61, log-rank test). Error bar represents the 95% confidential interval at each point.
Low CECD ( < 2000 cells/mm²) at the time of surgery considerably contributed toward the loss in CECD after the surgery (Table 3).
The mean IOP ± SD was 19.3 ± 5.8 mmHg at baseline, whereas it was 11.0 ± 3.8 mmHg (P < 0.001, adjusted for Bonferroni correction), 12.3 ± 3.5 mmHg (P < 0.001), 12.0 ± 3.1 mmHg (P < 0.001), 12.0 ± 3.4 mmHg (P < 0.001), and 13.5 ± 4.9 mmHg (P < 0.001) at 3, 6, 12, 24 and 36 months, respectively.
Discussion
Ex-PRESS surgery is a procedure with a faster postoperative recovery of visual acuity than trabeculectomy [7], and it is widely being indicated for patients with OAG. In this study, we performed Ex-PRESS surgery (including combined cataract surgery) in Japanese patients with OAG and regularly measured CECD for 36 months. There was a significant decrease in CECD at 36 months with a decrease rate of 1.8%/year. When a 5% decrease in CECD from baseline (preoperative) was defined as death in survival analysis, the survival rate of 95% CECD at 36 months was 50%. Low CECD before the surgery was detected as a significant risk factor for CECD loss. The amount of CECD loss in our cases was not thought to be clinically problematic; however, it is mandatory to examine CECD at least once a year. Further, it might be important to mention the possibility of future bullous keratopathy in patients scheduled for Ex-PRESS surgery with considerably reduced CECD.
Ex-PRESS surgery is thought to be a safer procedure than trabeculectomy in postoperative IOP management because a certain amount of aqueous humour is released from the eye into subconjunctival through a metal tube, making postoperative low IOP and eye collapse less likely, but corneal endothelial cell damage is reported as one of the late complications [8], which is discussed in this article. There are reports on postoperative CECD change among several glaucoma procedures, including trabeculectomy, Ex-PRESS, and glaucoma valve tube; however, it is controversial whether which techniques are more likely to decrease CECD [11,12,13,14,15].
First, in a 3-month observational study that examined postoperative CECD among trabeculectomy, Ahmed-valve shunt, and Ex-PRESS, CECD loss was the smallest in Ex-PRESS compared with the former two [13]. This was because there was less anterior chamber collapse in the Ex-PRESS procedure. However, this is only a 3-month report and it requires a longer observation period. Another prospective study comparing the surgical outcomes between trabeculectomy and Ex-PRESS procedure over a 12-month period found no difference in postoperative CECD change in the two procedures [15]. In contrast, a study examined postoperative CECD after trabeculectomy and Ex-PRESS in Japanese patients with glaucoma and found a significant decrease in CECD in Ex-PRESS compared to trabeculectomy at 24 months [11].
There are several reports on treatment with standalone Ex-PRESS surgery. In a study that examined the surgical outcomes of Ex-PRESS in Japanese patients with OAG, there was a significant decrease in CECD at 24 months. However, the actual number of CECD at 24 months was insufficient to cause clinical endothelial damage (i.e., 2428 cells/mm2) [11]. Moreover, a recent report indicated a significant decrease in CECD at 12 months after Ex-PRESS in Japanese patients with normal-tension glaucoma [12]. In contrast, a study reported that CECD did not decrease at 24 months after Ex-PRESS in Japanese patients with glaucoma [14]. The number of patients, number of CECD during the surgery, postoperative management methods, and analysis methods might account for these differences.
The number of CECD is reported to spontaneously decrease in normal eyes, with an annual decrease of approximately 0.6% [21]. The rate of decrease in this study was calculated to be 1.8% per year, which was faster than the rate in the natural course. As the decrease rate of CECD loss after Ex-PRESS varies in the literature (calculated based on the number of CECD in each article; from 0% to 5.4% per year) [11,12,13,14,15,16], postoperative CECD examination is important. Descemet’s membrane endothelial keratoplasty or Descemet’s stripping automated endothelial keratoplasty may be considered in some patients with originally low CECD.
The mechanism of CECD loss after Ex-PRESS surgery remains unclear. The use of intraoperative MMC is thought to be involved in one of the causes of CECD loss after trabeculectomy [22, 23], but there is little knowledge on Ex-PRESS related CECD loss. The damage may have started in the vicinity of the corneal endothelial cells where the Ex-PRESS was inserted, which may be different from the mode of CECD damage after trabeculectomy [16]. Furthermore, the involvement of MMC like trabeculectomy, foreign body reaction, change in aqueous humour flow in the anterior chamber, and mechanical contact between corneal endothelial cells and Ex-PRESS (caused by ocular structural change caused by ocular digital massage) are some of the possibilities.
The aqueous flow rate through Ex-PRESS tube remains constant even after IOP-lowering procedures such as laser suture lysis or bleb needling, suggesting that the anterior chamber might be difficult to collapse and the contact between Ex-PRESS tube and the endothelial cell was unlikely to occur. On the contrary, Ex-PRESS surgery for eyes with preoperative low CECD was found to be a significant negative factor in CECD loss. As the corneal endothelium is a nonregenerative tissue, once the corneal endothelium is damaged in the eyes with low CECD, it may not be able to keep up with the compensation of the surrounding endothelial cells [24], resulting in a faster rate of CECD loss. The presence or absence of concomitant cataract surgery was not associated with CECD loss. In general, there is an association between cataract surgery and corneal endothelial damage [25], but the soft-shell technique protection might minimize this impairment [26]. In addition, there is a report that examined postoperative CECD in the following three groups [27]: trabeculectomy with combined cataract surgery, trabeculectomy alone, and cataract surgery alone. These three groups showed a significant CECD decrease postoperatively, but the difference was not significant among these groups. Although this cannot be directly applied to our cases, these results suggested that current minimum invasive cataract surgery itself is unlikely to have a direct significant effect on CECD loss. Single Ex-PRESS surgery was performed on patients with phakic and pseudophakic eyes, and no difference in survival rate was observed between the two groups (P = 0.27). The effect of standalone Ex-PRESS surgery on CECD loss according to the lens status needs to be further investigated.
This time, we set the successful maintenance rate of CECD as more than 95% at 36 months, but there is no specific definition of this rate. The survival rate was 28% if 97.5% CECD maintenance at 36 months was defined as success, and it was 80% if 90% CECD at 36 months was defined as successful. In normal eyes with a CECD count of 2500 cells/mm² or more, there might be no clinical problem at 36 months postoperatively, but regular CECD examination is essential in patients with low CECD, especially under 2000 cells/mm² at the surgery.
There was a significant reduction of an average of 35% from the baseline IOP, which was a favourable outcome as reported in previous studies [11, 12]. As evidenced by the collaborative normal-tension glaucoma study results [3], it would be quite beneficial in delaying glaucoma progression, if 30% IOP reduction could be achieved. We obtained an IOP reduction rate of 35%, and the relationship with VF progression will be discussed in our next study.
This study has several limitations. First, this was a retrospective study conducted at a single institution, and it is inevitable that there was a selection bias. It is necessary to consider that the accuracy of Ex-PRESS surgery and postoperative results, including IOP management, might correlate to some extent with the years of surgical experience [28]. Therefore, our results may not applicable to all surgeons working with Ex-PRESS. The position of the insertion of Ex-PRESS tube was confirmed using a four-mirror lens; however, it was thought that the positional relationship with the corneal endothelium could also be accurately found using anterior segment optical coherence tomography (AS-OCT). However, this study could not be performed because the facility did not have this machine. Second, the anterior chamber depth was not measured quantitatively during the course. It is easy to imagine that even if the anterior chamber does not become significantly shallow, if the anterior chamber becomes shallow because of over filtration, the possibility of contact of Ex-PRESS with the corneal endothelium increases. It is necessary to consider the relationship between this problem and the corneal endothelium based on quantitative corner opening indices such as angel opening distance 500 by AS-OCT. In long tube surgeries with a plate (such as Ahmed glaucoma drainage device, Baerveldt glaucoma drainage device), it has been reported that the CECD reduction rate is lesser when the tube is placed in the ciliary sulcus than that when it is placed in the anterior chamber [29, 30]. This may be attributed to the fact that there is more physical contact between the corneal endothelium and the tube when it is placed in the anterior chamber. In support of this, when the distance between the tip of the tube and the corneal endothelium was measured by AS-OCT when the Baerveldt glaucoma drainage device was inserted into the anterior chamber, a greater CECD reduction rate was found as the distance between the tip and the corneal endothelium decreased [31]. Based on these results, to examine the physical distance between the tip of the Ex-PRESS and the corneal endothelium are mandatory in future studies. Third, in this study, the number of CECD was substituted in the central cornea. There is a hypothesis that endothelial cells close to Ex-PRESS insertion site are initially damaged [16], then endothelial damage spreads to the central cornea. The measurement site of endothelial cells may help to elucidate the mechanism of endothelial cell damage after Ex-PRESS. This is only a 3-year report and the progress of endothelial cells needs to be monitored from a longer-term perspective. Finally, there are many factors that are difficult to quantify, such as the location and intensity of ocular digital massage, presence or absence of anterior chamber haemorrhage, degree of inflammation, and duration of steroid eye drop use. It is necessary to consider how these confounding factors should be involved in a risk factor analysis.
To summarize, in Japanese patients with OAG undergoing initial Ex-PRESS surgery, a significant CECD decrease was observed at 36 months. Although the decrease rate of 1.8% per year was not clinically problematic, caution should be exercised for patients with low CECD under 2000 cells/mm² at the surgery because the CECD might be significantly reduced. As the Ex-PRESS tube is originally a foreign body that will remain in the anterior chamber for the rest of the patient’s life, further long-term follow-up of CECD is necessary.
Summary
What was known before
-
Although the corneal endothelial cell density (CECD) loss associated with glaucoma surgery is becoming important, the course of CECD after the initial Ex-PRESS surgery has been up to 2 years, and the associated factors have not been investigated.
What this study adds
-
CECD after the initial Ex-PRESS surgery revealed a significant decrease at 3 years but its deterioration rate might not be clinically problematic. That preoperative low CECD (rough estimate < 2000) was revealed a significant risk factor for CECD loss meant that regular CECD measurement should be performed, especially in patients with low CECD at the surgery.
References
Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. Jama. 2014;311:1901–11.
Nakazawa T, Fukuchi T. What is glaucomatous optic neuropathy? Jpn J Ophthalmol. 2020;64:243–9.
Noauthors. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Collaborative Normal-Tension Glaucoma Study Group. Am J Ophthalmol. 1998;126:498–505.
Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120:1268–79.
Arora KS, Robin AL, Corcoran KJ, Corcoran SL, Ramulu PY. Use of various glaucoma surgeries and procedures in medicare beneficiaries from 1994 to 2012. Ophthalmology. 2015;122:1615–24.
Traverso CE, De Feo F, Messas-Kaplan A, Denis P, Levartovsky S, Sellem E, et al. Long term effect on IOP of a stainless steel glaucoma drainage implant (Ex-PRESS) in combined surgery with phacoemulsification. Br J Ophthalmol. 2005;89:425–9.
Netland PA, Sarkisian SR Jr., Moster MR, Ahmed II, Condon G, Salim S, et al. Randomized, prospective, comparative trial of EX-PRESS glaucoma filtration device versus trabeculectomy (XVT study). Am J Ophthalmol. 2014;157:433–40. e433
Shaarawy T, Goldberg I, Fechtner R. EX-PRESS glaucoma filtration device: Review of clinical experience and comparison with trabeculectomy. Surv Ophthalmol. 2015;60:327–45.
Mariotti C, Dahan E, Nicolai M, Levitz L, Bouee S. Long-term outcomes and risk factors for failure with the EX-press glaucoma drainage device. Eye (Lond). 2014;28:1–8.
Shimazaki J, Amano S, Uno T, Maeda N, Yokoi N. National survey on bullous keratopathy in Japan. Cornea. 2007;26:274–8.
Ishida K, Moroto N, Murata K, Yamamoto T. Effect of glaucoma implant surgery on intraocular pressure reduction, flare count, anterior chamber depth, and corneal endothelium in primary open-angle glaucoma. Jpn J Ophthalmol. 2017;61:334–46.
Aihara M, Kuwayama Y, Miyata K, Ohtani S, Ideta R, Hashimoto Y, et al. Twelve-month efficacy and safety of glaucoma filtration device for surgery in patients with normal-tension glaucoma. Jpn J Ophthalmol. 2019;63:402–9.
Casini G, Loiudice P, Pellegrini M, Sframeli AT, Martinelli P, Passani A, et al. Trabeculectomy versus EX-PRESS shunt versus ahmed valve implant: short-term effects on corneal endothelial cells. Am J Ophthalmol. 2015;160:1185–90. e1181
Omatsu S, Hirooka K, Nitta E, Ukegawa K. Changes in corneal endothelial cells after trabeculectomy and EX-PRESS shunt: 2-year follow-up. BMC Ophthalmol. 2018;18:243.
Wagschal LD, Trope GE, Jinapriya D, Jin YP, Buys YM. Prospective randomized study comparing Ex-PRESS to trabeculectomy: 1-year results. J Glaucoma. 2015;24:624–9.
Arimura S, Miyake S, Iwasaki K, Gozawa M, Matsumura T, Takamura Y, et al. Randomised clinical trial for postoperative complications after Ex-PRESS implantation versus trabeculectomy with 2-year follow-up. Sci Rep. 2018;8:16168.
Miyake K, Matsuda M, Inaba M. Corneal endothelial changes in pseudoexfoliation syndrome. Am J Ophthalmol. 1989;108:49–52.
Wang M, Sun W, Ying L, Dong XG. Corneal endothelial cell density and morphology in Chinese patients with pseudoexfoliation syndrome. Int J Ophthalmol. 2012;5:186–9.
Higashide T, Nishino T, Sakaguchi K, Yamada Y, Sugiyama K. Determinants of corneal endothelial cell loss after trabeculectomy with mitomycin C. J Glaucoma. 2019;28:61–67.
Cnaan A, Laird NM, Slasor P. Using the general linear mixed model to analyse unbalanced repeated measures and longitudinal data. Stat Med. 1997;16:2349–80.
Bourne WM, Nelson LR, Hodge DO. Central corneal endothelial cell changes over a ten-year period. Invest Ophthalmol Vis Sci. 1997;38:779–82.
Mietz H, Roters S, Krieglstein GK. Bullous keratopathy as a complication of trabeculectomy with mitomycin C. Graefes Arch Clin Exp Ophthalmol. 2005;243:1284–7.
Mohammadpour M, Jabbarvand M, Javadi MA. Focal corneal decompensation after filtering surgery with mitomycin C. Cornea. 2007;26:1285–7.
Rao GN, Shaw EL, Arthur EJ, Aquavella JV. Endothelial cell morphology and corneal deturgescence. Ann Ophthalmol. 1979;11:885–99.
Rosado-Adames N, Afshari NA. The changing fate of the corneal endothelium in cataract surgery. Curr Opin Ophthalmol. 2012;23:3–6.
Sato M, Sakata C, Yabe M, Oshika T. Soft-shell technique using Viscoat and Healon 5: a prospective, randomized comparison between a dispersive-viscoadaptive and a dispersive-cohesive soft-shell technique. Acta Ophthalmol. 2008;86:65–70.
Demir AG, Olgun A, Guven D, Demir M, Sendul SY, Akarsu Acar OP, et al. The effect of combined phacotrabeculectomy, trabeculectomy and phacoemulsification on the corneal endothelium in the early stage: a preliminary study. Int Ophthalmol. 2019;39:2121–8.
Freidl KB, Moster MR. ExPRESS shunt surgery: preferred glaucoma surgery in residency training? Surv Ophthalmol. 2012;57:372–5.
Hau S, Bunce C, Barton K. Corneal endothelial cell loss after baerveldt glaucoma implant surgery. Ophthalmol Glaucoma. 2021;4:20–31.
Zhang Q, Liu Y, Thanapaisal S, Oatts J, Luo Y, Ying GS, et al. The effect of tube location on corneal endothelial cells in patients with ahmed glaucoma valve. Ophthalmology. 2021;128:218–26.
Tan AN, Webers CA, Berendschot TT, de Brabander J, de Witte PM, Nuijts RM, et al. Corneal endothelial cell loss after Baerveldt glaucoma drainage device implantation in the anterior chamber. Acta Ophthalmol. 2017;95:91–96.
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for the English language review.
Funding
Supported in part by the GRANT 18K16945 from the Ministry of Education, Culture, Sports, Science and Technology of Japan (R.S.). The funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
Study conception and design: MA and SS; Acquisition of data: YA, RS, TF, MH, SS and MA; Analysis of interpretation of data: YA, RS and MA; Drafting of the manuscript: YA, RS and MA; Critical revision: MH, SS and MA.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aoyama, Y., Sakata, R., Fujishiro, T. et al. Changes in corneal endothelial cell density after initial Ex-PRESS drainage device implantation and its relating factors over 3 years. Eye 37, 69–74 (2023). https://doi.org/10.1038/s41433-021-01888-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01888-1
This article is cited by
-
Corneal endothelial cell loss after EX-PRESS surgery depends on site of insertion, cornea or trabecular meshwork
International Ophthalmology (2023)