Abstract
The COVID-19 infection is assumed to induce cognitive failure. Identifying the relationship between COVID-19, the effect of vaccination and medication, and accommodating non-COVID-19 factors to cognitive failure is essential. This study was conducted in Indonesia from September 2021 to January 2023. Demographic information, clinical data, comorbidities, vaccination, and medication during COVID-19 were obtained, as well as a 6-month cognitive assessment with Cognitive Failures Questionnaire/CFQ, Fatigue Severity Score, and Generalized Anxiety Disorder (GAD-7). A Structural Equation Model explains the relationship between potential predictors and cognitive failure. The average score of CFQ after 6 months was 45.6 ± 23.1 out of 100. The severity of the disease, which was associated with vaccination status, age, previous infection, and unit of treatment (p < 0.05), was not related to cognitive failure (p = 0.519), although there is a significant direct impact of worst vaccination status to cognitive failure(p < 0.001). However, age, fatigue, and current anxiety were associated with higher cognitive failure (p < 0.001), although comorbidities and recent headaches were not significant in other models (p > 0.05). This study concludes that cognitive failure after COVID-19 is a multifactorial event and does not solely depend on COVID-19 severity. It is crucial to re-address the factors related to the long-term efficacy of vaccination and medication and focus on non-health factors affecting cognitive failure.
Trial Registration: NCT05060562.
Similar content being viewed by others
Introduction
The Coronavirus Disease 2019 (COVID-19) caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) has become a global burden with a large number of people infected and rapid virus mutation. With 668 million patients with 6.73 million fatalities (as of January 2023)1, a concern regarding the long-term post-COVID-19 impact on a larger population should be addressed to prevent plummeted productivity and altered quality of life2. One of the main issues is cognitive failure after COVID-19.
COVID-19 and cognitive failure
Limited evidence explains the debilitating effect of COVID-19 on the central nervous system. A proposed model in mice mimicking mild COVID-19 infection showed a neuroinflammatory condition due to microglial activation linked to the alteration of oligodendrocytes. Furthermore, the demyelination process and neurogenesis inhibition occur, particularly in the hippocampus, which could explain the disturbance of memory formation3. A systematic review revealed a substantial cognitive decline after COVID-19, specifically the working memory4. Furthermore, a 9-month follow-up of COVID-19 survivors reported that up to 26% presented with mild cognitive impairment, and 1% had a moderate alteration in cognitive function5.
Vaccination and treatment on cognitive failure after COVID-19
Since the plausible mechanism of SARS-CoV-2 infection and neurodegenerative impact has been identified, there are some questions about whether vaccination and specific treatment have pivotal roles in alleviating cognitive failure through their mechanism of preventing viral replication, interaction with cell hosts and enhancing the neutralization effect. Even in the presence of the latest variant, vaccination with boosters reduces the severity6. In the previous study, two-dose vaccination effectively lowered selected post-COVID-19 symptoms7. However, the long-term effect of vaccination, booster doses, and heterologous regimens on cognitive failure in people with COVID-19 remains unanswered. It is also essential to re-evaluate the efficacy of the antiviral drug in preventing central nervous system (CNS) disorder of COVID-19 survivors, notably the best administration time.
Individual comorbidities and socioeconomic factors on cognitive failure
Cognitive failure is a part of ageing that is affected by many factors. A study in Taiwan raised the importance of recognizing socioeconomic status in achieving good cognitive function8, which during the pandemic, was abruptly affected. Furthermore, chronic diseases, particularly hypertension and diabetes mellitus, are also connected to cognitive deterioration9. A sedentary lifestyle, obesity, and smoking also shorten the cognitive-impairment-free life expectancy10. It is imperative to address these factors as competing variables to explain the precise impact of COVID-19 on cognitive failure.
As the large population-based study of cognitive failure after COVID-19 is limited, this study would prove or address the possible mechanism of cognitive failure after COVID-19 by accommodating other confounders using a robust statistical model from an Indonesian cohort as the highlight and novelty of this study.
Methodology
Study design and setting
This longitudinal study utilized a cohort of Indonesian post-COVID-19 patients recruited since September 2021 and extracted in January 2023. Participants with a history of COVID-19 were followed up for residual symptoms. We assessed cognitive function 6 months after diagnosis and their first symptoms through an online submission system, and this platform was disseminated to the entire country through social media, health care providers, and survivor groups.
Participants
Subjects with previous COVID-19 infection (at least thirty days from the onset or diagnosis) were diagnosed using either Indonesian Food and Drug Administration-approved antigen test for the anterior nasal sample (sensitivity over 80%)11 or real-time polymerase chain reaction (RT-PCR) of the nasopharyngeal, nasal, or pooled samples12. These procedures were performed by trained staff, as the self-administered antigen test was not recognized during the study period. This study covered all types of patients, from asymptomatic to hospitalized. After the provision of consent given by the participants, a follow-up cognitive assessment was made, and those without responses of expected outcomes were omitted. Aside from having self-reported mental illness and stroke, there is no other exclusion or limit for those with specific morbidities, age, and digital literacy. Moreover, the snowball sampling approach recruited more individuals to this cohort.
Variables and measurement tools
Demographic characteristics, health behaviour, chronic diseases, and other comorbidities were the baseline information covered in the questionnaire. Additionally, this study recorded the latest COVID-19 episode, including date and diagnostic methods, duration of symptoms, type of medication, vaccination status, type of vaccine, and time between doses. Investigators also identified the date from vaccination to infection and the type of care received (home isolation, hospitalization, or both). These variables may interact with each other and affect the relationship between COVID-19 and cognitive failure.
This study cited the definition of cognitive failure as a cognitive mistake made while performing a task that a person would typically complete successfully in daily life. Problems with memory, perception, and focus are signs of cognitive failure13.
This study measured the cognitive failure 6 months after the COVID-19 infection. Investigators implemented the assessment using a questionnaire that is in proximity to clinical cognitive assessment, the Cognitive Failures Questionnaire (CFQ)(14), consisting of 25 5-Likert scale questions. The responses range from 0 to 4, where a higher number indicates frequent cognitive failure events. The Indonesian version of this questionnaire was derived from a study with a Cronbach alpha value of 0.94214. Furthermore, one study disclosed three domains in the questionnaire which are forgetfulness (related to something known or planned), distractibility (alteration of attention and focus), and false triggering15.
Investigators assessed other residual COVID-19 symptoms and neuropsychiatry conditions to identify the possible contribution of these symptoms to cognitive failure. Investigators evaluated any presence of residual symptoms after the first onset or diagnosis using a set of measurement tools such as the Fatigue Severity Scale (FSS)16 over the past 6 months, Generalised-Anxiety Disorder (GAD-7) to screen for recent anxiety and a 10-Likert scale question to identify its incidence over the past two weeks.
Bias
Investigators admit that the quality of baseline data was heavily affected by recall bias. Therefore, participants were required to provide the answers based on the observation chart, written source (such as medical records summary), and through the PeduliLindungi application (for data related to testing, vaccinations, and individual information).
Participants might experience reinfection. Hence, only the last episode of COVID-19 should be provided as the response. By applying this approach, the investigators could not examine in detail the previous infection and, possibly, its latent impact on cognitive function.
Investigators knew that robust cognitive assessments such as Cambridge Neuropsychological Test Automated Battery (CANTAB) could provide objective cognitive results. However, the investigators considered the survey exhaustion and other factors affecting the response, such as internet connection and adaptation to the measurement tools. The questionnaire was deemed sufficient to represent the domains tested by these standardized clinical tests.
Study size
There is limited information on long-term cognitive situations after COVID-19. However, a study of CFQ application to neurosarcoidosis (a subset of sarcoidosis, a multi-inflammatory systemic disorder) shows a mean score of 45.6 ± 20.713. Therefore, investigators assumed that the variance of cognitive failure values of COVID-19 survivors is approximately 20.7. Using the equivalence formula from the assumed score, with 5% type 1 error, 90% power of the study, the absolute mean difference between the assumpted mean and sample means of 1, a 5% equivalence limit, and 10% listwise deletion of incomplete response, a total of 5653 participants should be drawn from the cohort.
Quantification and discretization
Several data were presented as discrete variables, including the duration of symptoms and administration of drugs. Moreover, to assume the possible variant, the investigators matched the date of diagnosis with the variant surveillance reports issued by the Ministry of Health according to surveillance week and region. Other continuous data were kept at their original values. Each type of vaccine possesses different efficacy17. Hence an ordinal level of this variable was made, where a higher ordinal level of vaccination means worse vaccination status (unvaccinated) (Supplementary Data 1).
Statistical method
The analysis involved participants with complete responses; hence no imputation and other missing data analysis were undertaken. Descriptive statistics and bivariate analysis of variables were conducted before the final analysis. We performed the structural equation model. First, the whole model was built (Fig. 1) and simplified by the trimming approach. The structure of the model consists of exogenous variables, latent variables, and CFQ score as endogenous factors. The assumption was that vaccination, medication, virus variant, and comorbidity might affect the severity of COVID-19 and, eventually, cognitive failure. Aside from COVID-19, demography, chronic fatigue over the past 6 months, recent headaches, and anxiety may affect the cognitive situation. The investigators constructed latent variables with confirmatory factor analysis. The selection of the explanatory factors was based on bivariate analysis and model fitting assessed using the Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Standardized Root Mean Square Residual (SRMR), and Root Square Mean Error of Approximation (RMSEA). The Lavaan library in R performed the analysis and produced the final plot.
Proposed Model of Cognitive Failure post-COVID-19. This model comprises four exogenous latent variables (circle variables), and one variable acts as both an exogenous and endogenous latent variable (severity). The final endogenous factor is cognitive failure. Factor loadings of the latent variable are presented with diverging arrows from the latent variable (Recent Headache with six elements. Demography with three factors. Vaccination with two factors. Severity with three factors, and comorbidities with four factors). Converging arrows indicate the impact of the exogenous variable on the endogenous factor.
Ethical approval
This study was authorized by the Hasanuddin University Research Ethics Review Committee for Research Involving Human Research Participants (full-board review number 758/UN4.6.4.5.31/PP36/2021). We confirm that all procedures, particularly the clinical data collection, were performed following relevant guidelines and regulations. Informed consent was obtained from all participants when they provided information to the cohort. We appropriately de-identified, stored, and used the data while respecting confidentiality. Any circumstances that needed immediate action were directed to a professional. This research is a subset of a clinical trial with the identifier NCT05060562 on clinicaltrials.gov.
Results
A total of 5680 participants were involved in this study. The average age was 28.36 ± 8.96 years (18–65 years old). This cohort was dominated by participants aged less than 30 years old (69.9%), followed by 30–40 years old (18.7%), 40–50 years old (8.3%), and above 50 years old for 3.1%. The distribution of sex assigned at birth was almost equal (49.9% male). As 30.2% of participants were undergraduates and graduates, and 5.3% of the participants were medical staff currently working at healthcare facilities. The distribution of cases follows the population density of each island, where participants from Java dominated the cohort (34.5%), followed by Sumatera (25.5%), Kalimantan (12.8%), Sulawesi (12.5%), Maluku and Papua (8.1%), and last with Bali and Nusa Tenggara (6.6%). Real-time PCR detected 41.1% of cases, followed by antigen test (40.5%) and RT-PCR + Antigen test (18.4%). Figure 2 depicts the selection of participants from the primary cohort.
The mean CFQ score in this cohort was 45.6 ± 23.1. Table 1 describes the distribution of variables according to the mean CFQ score. The selection of these potential predictors was based on the plausible mechanism of these factors to cognitive failure.
From Table 1, study participants with higher cognitive failure were significantly younger and graduated from junior high school or lower, compared to higher education levels (p < 0.05). Medical workers were less likely to have higher cognitive failure. There were no significant differences in exercise, smoking, and prescription of any antiviral agent, but there was an insignificant risk of uncontrolled hypertension, diabetes, and higher cognitive failure (p > 0.05). Those with a history of reinfection, particularly with newer variants and the latest infection caused by earlier variants, were more likely to have a higher cognitive failure (p < 0.05). Regarding vaccination, unvaccinated people were prone to severe cognitive outcomes (p < 0.05). Interestingly, a proportion of higher cognitive failure was seen in people who underwent self-isolation (p < 0.05). People with a higher level of fatigue within 6 months and higher anxiety over the past two weeks tended to have a higher cognitive failure (p < 0.05).
However, by treating the CFQ as a raw score (assuming that mean CFQ score discriminant ability is unknown), smoking was associated with a higher score of CFQ (p = 0.024). Moreover, antiviral prescription time was also associated with CFQ score (p = 0.002) as well as the occurrence of the infection, but not with the unit of treatment (p = 0.056). Nevertheless, the investigators included all variables in the initial SEM model and the trimming approach was applied.
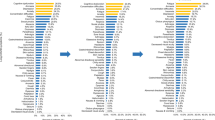
Figure 3 depicts the CFQ score of some variables with a p-value below < 0.01. Those people who remain unvaccinated and infected, those with a history of omicron infection, or those infected with wild-type variants had a higher CFQ score. Despite having a significant p-value, the median CFQ score between four different antivirus prescription times shows a similar trend.
Comparison of CFQ Score in each variable. Six separate figures illustrate the comparison of CFQ score in the subset of selected variables, including the type of vaccination received before infection, time of antivirus prescription (but not time of initial ingestion), days of last dose injection to infection, the occurrence of infection according to last vaccination doses, previous infection, and latest period of infection.
The investigators proposed a model using linear structural relation (LISREL), as shown in Fig. 1. A cutoff of a p-value of more than 0.2 and plausibility was applied for variable selection; hence, re-specification of the model was performed. There are four latent exogenous variables in the model. The first latent variable is recent headache, which consists of five different types of headache and one associated symptom, namely tension, cluster, migraine, vertigo, and ice pick headache followed by vomit and nausea (Fitness index CFI 0.966, TLI 0.944, SRMR 0.025) Second is comorbidities, which consists of exercise, smoking, diabetes mellitus and hypertension (CFI 0.992, TLI 0.976, SRMR 0.018). This paper wants to address the effect of vaccination. Hence, the type of vaccination, days to infection, and occurrence of infection were merged into two variables (dose-day and dose-type) and created vaccination as a latent exogenous factor. The direction of the vaccination variable was the longer duration between doses and the lower number of doses received was defined as worse vaccination status. Specific symptoms (Shortness of breath, loss of smell, and headache) construct the severity, a latent exogenous factor (CFI 1.0, TLI 1.0, SRMR < 0.001). Since two demographic factors were significantly associated with CFQ, these two variables represent a latent demography variable. Cognitive failure is assumed to be affected by severity, demography, fatigue condition, anxiety level, and recent headache, while severity is predicted by age, previous infection, latest variant, and treatment unit.
There are three proposed models with good fitness indices. However, one model possessed an acceptable fitness index (CFI 0.958, TLI 0.940, SRMR 0.044, and RMSEA score of 0.056, although χ2/df = 18.8). Figure 4 depicts the LISREL of the model.
The Linear Structural Relation Of The Final Model. Variables in the circle are the latent variables constructed by other variables (as written in the figure). The line shows the p-value of the relationship where the interrupted line indicates a non-significant relationship and the intact lines were significant. The number represents the standardized estimate of the parameters (β), except for the circular bi-directional arrows, which represent the variance of latent variables. Bidirectional arrows present the covariance between demography and vaccination.
Table 2 elaborates on the estimates of each variable of the final model. Regarding the severity of the disease, represented by the duration of shortness of breath and headache during the latest COVID-19 episode, unvaccinated people were at risk of having severe disease compared to those receiving more doses and a heterologous regimen. Furthermore, there was a link between severe illness and hospitalization, older age, and absence of previous infection or previous infection with earlier variants.
There were four significant predictors of cognitive failure. It is interesting to see that younger age was associated with higher CFQ score (p < 0.001). Cognitive failure was linear to higher chronic fatigue and anxiety levels but not associated with demographic features (p = 0.677). Further covariance analysis showed that people with lower education and unemployed tended to have worse vaccination status (as represented by covariance analysis p < 0.05). In the previous model, higher comorbidities were independent of severity and cognitive failure (Supplementary Table S1). Recent headaches, which could represent any CNS disorder, were also not associated with cognitive failure in the full model (Supplementary Table S1), which was then omitted from the final model. A significant relationship was also seen between the latest variant and severity (p = 0.046 Supplementary Table S2) on the non-fit model, where the newest variant was associated with a shorter duration of each symptom (Supplementary Table S3), which shows possible collinearity. To produce a better model, the variable latest variant was omitted from the final model as its p-value is the highest among other predictors of severity (Supplementary Table S4).
Finally, in the Structural Equation Model, there are several factors linked to cognitive failure in the post-COVID-19 period. The severity of the disease as the latent variable was not associated with the CFQ score 6 months after infection (p = 0.519) as well as education and working position (p = 0.677). However, worse vaccination status as a latent variable was associated with higher CFQ scores (standardized estimate β = 0.149 p < 0.001). External factors such as age (standardized estimate β = − 0.060 p < 0.001), anxiety (GAD score, standardized estimate β = 0.264 p < 0.001) and fatigue (FSS score, standardized estimate β = 0.101 p < 0.001) also affect the CFQ score). Among the four factors, according to the standardized estimate β, generalized anxiety is the most influential factor of cognitive dysfunction. However, these five factors only explain 14.7% of the variance of the CFQ score. Further analysis according to each domain of CFQ score revealed similar significant factors including forgetfulness (Supplementary Table S3), distraction (Supplementary Table S4), and false trigger (Supplementary Table S5). However, fatigue score was not associated with distraction (p = 0.051).
Discussion
The average score and median score of CFQ was 45 out of 100, which explains that cognitive failure after 6 months should not be underestimated. This cohort was dominated by younger age (< 30 years) as this group is more vulnerable and transmitting infection18 due to higher mobility and is among the non-priority groups for booster vaccination. This study revealed that younger people were prone to cognitive failure. Younger ages are sensitive to changes in cognitive function as they are heavily affected by stress, anxiety, and depression when responding to their surroundings19. This could be an underlying issue that CFQ consists of questions related to daily activities that most elder people would not do, and if they do, it would not be as complex as what the younger are engaged in. Hence younger people will be more sensitive to smaller changes of limitation in doing the reported activities in CFQ and thus, show a higher fluctuation of CFQ score.
The consideration to select the three symptoms (loss of smell, shortness of breath, and headache) to build a latent variable representing COVID severity was based on the plausibility of SARS-CoV-2 infection to central nervous system (CNS) perturbation, the possible ascending transmission through olfactory nerve20 which represent by loss of smell, shortness of breath, which could lead to hypoxia, and the possible CNS inflammatory condition, roughly marked by headache21. In the final model, loss of smell was omitted due to insignificance in predicting CFQ class (p > 0.05), provided in Supplementary Table S6. In theory, specific variants are linked to severe disease, and a significant relationship was seen between the latest variant and severity (Supplementary Table S6) where people infected during the delta period had a bigger proportion of having a longer duration of symptoms, compared to other variants. However, including the newest variant variable in the structural model did not produce a fit model as the goodness of fit indices is below the recommended value (Supplementary Table S2) and improvement was seen when omitting the latest variant (Supplementary Table S7). A better model without loss of smell and the latest variant is shown in Supplementary Table S8, showing a more acceptable cognitive failure model.
Severity was assumed to be the mediator of other variables to cognitive failure—the absence of previous infection or previous infection with newer variants negatively correlated with severity. A study revealed frequent reinfection with the latest variant, although the severity remains lower than the first infection22. This study also identified the benefit of vaccination in reducing the severity, particularly for those who received booster doses with a heterologous regimen and had a shorter duration from vaccination to infection, which is in line with a meta-analysis23. It is important to note that the association between severity and hospitalization should be interpreted cautiously, as severe diseases are likely to be admitted. In bivariate analysis, the prescription and administration of antiviral agents were maximized in hospitalized individuals (p < 0.05) (Supplementary Table S9). In practice, vaccinated people with mild symptoms are less likely to receive antiviral agents than those with moderate and severe diseases. Table 1 indicates that mild cases who underwent self-isolation experienced higher cognitive failure, which ignites the role of antiviral agent prescription to limit viral ascending to CNS and preventing cognitive impairment. Nevertheless, there was no significant association between disease severity and cognitive failure. Receiving vaccination or antiviral agent is not enough as it should be done and administered in an appropriate time.
Early and rigorous viral clearance is essential to reduce the severity and subsequent CNS injury, affecting cognitive function through rapid viral neutralization with antibodies and suppression of viral replication with antiviral agents. A study in Japan demonstrated the reduction of median neutralizing antibody (NAb) titer antibody up to 44.3%, 12 months after wild-type infection and undetected at 35.5 months24. Furthermore, the number of Nab against ancestral and delta variants in vaccinated individuals was 7.8 and 4.0 higher than in unvaccinated individuals. This study also revealed a faster time to reach peak concentration among those vaccinated participants (two weeks versus three weeks). However, the number of NAb titers was not associated with the duration of viral clearance (p < 0.267). It should be noted that the participants were vaccinated with inactivated virus vaccine and protein subunit vaccine25. With the mRNA vaccine, inhibition against live omicron-type viruses was the lowest among other variants and remained moderate using the serum of patients who received a third dose and took it after three weeks26. A heterologous regimen (inactivated + booster mRNA) demonstrated better protection against omicron by enhancing the memory B cell and specific T cell response compared to the homologous inactivated vaccine27. The finding concludes an insignificant indirect vaccination effect on cognitive failure by reducing disease severity (p-value 0.521 in Table 2). However, when considering a direct effect on CFQ, worse vaccination status as a latent variable was associated with higher CFQ scores (standardized estimate β = 0.149 p < 0.001) In short, only relying on neutralizing antibodies attained by vaccination is insufficient against the virus and severity prevention, but not in cognitive dysfunction prevention.
It is crucial to address how fast the dissemination of the virus to multiple organs versus the viral clearance is. The heatmap of SARS-CoV-2 RNA showed that the distribution of subgenomic RNA copies during the first four days of illness was higher in the dura mater and cerebral cortex. Furthermore, from 5 to day 13, at least 0.05- < 0.1 copies per nanogram of RNA SARS-CoV-2 input was found in the basal ganglia and even higher in the cerebral cortex28. Considering the slower duration to reach the peak level of neutralizing activity of antibodies achieved by vaccination, relying on the vaccination-attained antibody, particularly in high-risk individuals, is insufficient. It is relevant to consider the early initiation of antiviral agents to boost viral clearance. However, a systematic review of molnupiravir versus placebos showed no significant difference in mean viral load and duration of viral clearance (14–15 days) in unvaccinated individuals and people with mild-moderate non-hospitalized cases29. Another systematic review of favipiravir exhibited faster viral clearance for up to 7 days after initiation30, although a study on mild COVID-19 did not show a better duration of viral clearance31. In this cohort, various antiviral agent was prescribed, but the time from diagnosis to prescription and ingestion was unidentifiable. A study emphasized that a golden period of treatment from onset to hospitalization is within four days32 to reduce the severity, which could explain the detrimental efficacy of antiviral agents. Moreover, this study revealed a significant connection between increasing age and the severity as older age was linked to higher viral load33 and severe inflammatory conditions34. Thus, considering these factors, it is cogitable why the indirect effect of the unit of treatment on cognitive failure via severity of disease was not significant (p-value 0.521 in Table 2).
This study also identified other factors that were connected to cognitive failure. Fatigue over the past 6 months was related to cognitive failure. The FSS questionnaire also assessed the fatigue impact on the duties and responsibilities linked to cognitive function. Fatigue was one of the most common post-COVID-19 symptoms, and several theories postulated the origin of fatigue and cognitive dysfunction through indirect mechanisms, mainly the inflammatory condition and altered metabolism of neuron cells35. Furthermore, fatigue is hypothetically affected by conditional and physiological aspects related to mental capacity, task complexity, and surrounding conditions36. Following the theory mentioned above, the GAD, which reflects state anxiety and possibly trait anxiety, could be a competing factor that affects cognitive function, particularly overstimulating alerting and orientation or alteration in the executive control network37, and it is proven to affect cognitive failure in this study. It is pivotal to assess people's psychosocial condition during the pandemic comprehensively.
This study constructed a latent demography variable as mental capacity and decision-making are linked to education level and organizational factors. A review shows that highly educated people seem to have better cognitive functions38 but are mostly affiliated with higher-pressure occupations. Long working hours were associated with negative cognitive performance, particularly in middle age39. A study comparing the psychological distress about COVID-19 between health workers and the general population showed an alarming rate of stress and anxiety in health workers40. However, the final model showed a non-significant relationship between demography and cognitive failure (p = 0.677), which could imply variety in working conditions and individual coping mechanisms.
There is a question of whether a recent headache is sequelae of COVID-19. This study identified the headache that occurred before the cognitive assessment to eliminate possible CNS disorder that affects cognitive function. A study pointed out that at least 20% of COVID-19 patients will develop chronic headaches for up to 9 months41. Full vaccination status could reduce chronic headaches after 90 Days from COVID-19 first onset7, which could illustrate the effect of vaccination on cognitive failure via the prevention of chronic headaches. However, the additional model shows an insignificant indirect impact of vaccination on cognitive failure via prevention of recent headaches (p-value 0.217 in Supplementary Table S7). To summarize, cognitive failure after COVID-19 is not solely a subsequent effect of disease severity but is highly affected by other external factors.
Some limitations should be addressed despite the study covering longer periods of observation, more representative participants, and various vaccination statuses. It is vital to compare cognitive failure among people who never get infected. Due to the higher number of participants and limited resources, this study could not conduct such a test. Although this study excluded people with self-reported mental illness and CNS disturbances such as stroke, there is still a possibility of undetected CNS disorders in participants that should be clinically ruled out. Even with the additional questions to identify the headache that might be related to CNS disease, this procedure was less appropriate to justify the actual clinical situation. Furthermore, to see the true effectiveness of antiviral agents in reducing the severity and cognitive failure, the duration of symptoms should be measured starting from the time of receiving medication, not recording the entire duration of symptoms.
There is a question of whether this questionnaire is suitable for measuring cognitive failure in COVID-19. A study implemented cognitive assessment using Perceived Memory and Attentional Failures Questionnaires (PerMAFaq) during the COVID-19 period but focused on the mental health of healthy people42. Moreover, one study evaluating the effect of COVID-19 on cognitive failure at work applied three measurement tools43 which are not linear with this study's objectives and settings. This study is one of the initial studies that utilized the CFQ to assess post-COVID-19 symptoms. Although using proxy tools for a more reliable clinical assessment of cognitive function, there is a lack of clinical correlation between CFQ and CANTAB44. To justify the use of CFQ, the authors explored the connection between the changes in brain anatomy and physiology that are common after COVID-19 and the cognitive failure measured by CFQ. Disturbance in the Gamma-Aminobutyric Acid (GABA)ergic system occurs in COVID-19, marked a depletion of GABA and dysregulation of the GABAergic system45. Moreover, increased grey matter volume was common among people with previous COVID-19 infection46. A study to explore GABA and grey matter volume (GMV) in connection to cognitive failure using CFQ showed that there wass a negative correlation between GABA and CFQ, as well as positive correlation of GMV and CFQ47. Thus CFQ is appropriate in measuring the cognitive failure after COVID-19.
Conclusion
This study demonstrates the structural relationship of factors associated with cognitive failure among COVID-19 survivors and this study indicates that cognitive failure after COVID-19 is not solely because of COVID-19, but rather a combination of external, psychological factors and 85.3% of unexplored factors. Vaccination remains essential to reduce the severity, although doses, type, and timing of administration should be maximized to enhance the long-term benefit of cognitive dysfunction prevention. It is also recommended to assess the non-health circumstances that influence the mental health of individuals (including fatigue and anxiety), as during the COVID-19 pandemic, people encounter financial hardship and are exposed to psychosocial stressors. To address some unexplored variance (85.3%), further suggestions should be considered, including measuring the anatomical changes of the brain that is prevalent among COVID-19 survivors, (this include the assessment of cognitive-related area and GABA function), applying repeated measures of external factors, including job stress and quality of life and conducting objective measurement of chronic disease status and progression, including complication and medication which may affect the cognitive failure.
Data availability
The data is available at the following repository: https://figshare.com/s/a54eaaa299610353a2a3.
Change history
18 December 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41598-023-48244-9
References
Organization, W. H. WHO Coronavirus (COVID-19) Dashboard, Situation By Region, Country, Territory, and Area. https://covid19.who.int/table. Accessed 31 Jan 2023.
Tarazona, V., Kirouchena, D., Clerc, P., Pinsard-Laventure, F. & Bourrion, B. Quality of life in COVID-19 outpatients: A long-term follow-up study. J. Clin. Med. 11(21), 6478 (2022).
Venkataramani, V. & Winkler, F. Cognitive deficits in long Covid-19. N. Engl. J. Med. 387(19), 1813–1815. https://doi.org/10.1056/NEJMcibr2210069 (2022).
Tavares-Júnior, J. W. L. et al. COVID-19 associated cognitive impairment: A systematic review. Cortex 152, 77–97. https://doi.org/10.1016/j.cortex.2022.04.006 (2022).
Hartung, T. J. et al. Fatigue and cognitive impairment after COVID-19: A prospective multicentre study. eClinicalMedicine https://doi.org/10.1016/j.eclinm.2022.101651 (2022).
Li, H. et al. The effects of vaccination on the disease severity and factors for viral clearance and hospitalization in Omicron-infected patients: A retrospective observational cohort study from recent regional outbreaks in China. Front Cell. Infect. Microbiol. https://doi.org/10.3389/fcimb.2022.988694 (2022).
Herman, B., Wong, M.C.-S. & Viwattanakulvanid, P. Vaccination status, favipiravir, and micronutrient supplementation roles in post-COVID symptoms: A longitudinal study. PLOS ONE 17(7), e0271385. https://doi.org/10.1371/journal.pone.0271385 (2022).
Hsu, H.-C. & Bai, C.-H. Individual and environmental factors associated with cognitive function in older people: A longitudinal multilevel analysis. BMC Geriatr. 22(1), 243. https://doi.org/10.1186/s12877-022-02940-9 (2022).
Kim, J., Park, E. & An, M. The cognitive impact of chronic diseases on functional capacity in community-dwelling adults. J. Nurs. Res. 27(1), 1–8. https://doi.org/10.1097/jnr.0000000000000272 (2019).
Anstey, K. J. et al. The influence of smoking, sedentary lifestyle and obesity on cognitive impairment-free life expectancy. Int. J. Epidemiol. 43(6), 1874–1883. https://doi.org/10.1093/ije/dyu170 (2014).
Organization, W. H. Antigen-detection in the diagnosis of SARS-CoV-2 infection. 6 October 2021 2021. [Online]. Available: https://apps.who.int/iris/rest/bitstreams/1376869/retrieve
Organization, W. H. Diagnostic Testing for SARS-CoV-2 (World Health Organization, 2020).
Voortman, M. et al. Everyday cognitive failure in patients suffering from neurosarcoidosis. Sarcoidosis Vasc. Diffus. Lung Dis. 36(1), 2–10. https://doi.org/10.36141/svdld.v36i1.7412 (2019).
Indrawan, F., Wahyuning, C. S., & Liansari, G. P. EVALUASI PERFORMANSI KOGNITIF KRU DARAT PT KERETA API INDONESIA DAOP II BANDUNG DENGAN MENGGUNAKAN COGNITIVE FAILURE QUESTIONNAIRE DAN DIRECTRT (2014).
Rast, P., Zimprich, D., van Boxtel, M. P. J. & Jolles, J. Factor structure and measurement invariance of the cognitive failures questionnaire across the adult life span. Assessment 16, 145–158 (2009).
Jason, L. A. et al., Fatigue scales and chronic fatigue syndrome: Issues of sensitivity and specificity. Disabil. Stud. Q. 31 (1), (2011).
Feikin, D. R. et al. Duration of effectiveness of vaccines against SARS-CoV-2 infection and COVID-19 disease: Results of a systematic review and meta-regression. The Lancet 399(10328), 924–944. https://doi.org/10.1016/S0140-6736(22)00152-0 (2022).
Alessandretti, L. What human mobility data tell us about COVID-19 spread. Nat. Rev. Phys. 4(1), 12–13. https://doi.org/10.1038/s42254-021-00407-1 (2022).
Varma, P., Junge, M., Meaklim, H. & Jackson, M. L. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog. Neuropsychopharmacol. Biol. Psychiatry 109, 110236. https://doi.org/10.1016/j.pnpbp.2020.110236 (2021).
Brann, D. H. et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Sci. Adv. 6(31), eabc5801. https://doi.org/10.1126/sciadv.abc5801 (2020).
Dono, F. et al. New daily persistent headache after SARS-CoV-2 infection: A report of two cases. Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol. 42(10), 3965–3968. https://doi.org/10.1007/s10072-021-05444-3 (2021).
Flacco, M. E. et al. Risk of reinfection and disease after SARS-CoV-2 primary infection: Meta-analysis. Eur. J. Clin. Investig. 52(10), e13845. https://doi.org/10.1111/eci.13845 (2022).
Deng, J. et al. Comparison of the effectiveness and safety of heterologous booster doses with homologous booster doses for SARS-CoV-2 vaccines: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 19(17), 10752. https://doi.org/10.3390/ijerph191710752 (2022).
Ishizaki, A. et al. Neutralizing-antibody response to SARS-CoV-2 for 12 months after the COVID-19 workplace outbreaks in Japan. PLOS ONE 17(8), e0273712. https://doi.org/10.1371/journal.pone.0273712 (2022).
Zhu, L. et al. Impact of vaccination on kinetics of neutralizing antibodies against SARS-CoV-2 by serum live neutralization test based on a prospective cohort. Emerg. Microbes Infect. 12(1), 2146535. https://doi.org/10.1080/22221751.2022.2146535 (2023).
Wang, L. et al. Differential neutralization and inhibition of SARS-CoV-2 variants by antibodies elicited by COVID-19 mRNA vaccines. Nat. Commun. 13(1), 4350. https://doi.org/10.1038/s41467-022-31929-6 (2022).
Zuo, F. et al. Heterologous immunization with inactivated vaccine followed by mRNA-booster elicits strong immunity against SARS-CoV-2 Omicron variant. Nat. Commun. 13(1), 2670. https://doi.org/10.1038/s41467-022-30340-5 (2022).
Stein, S. R. et al. SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nature 612(7941), 758–763. https://doi.org/10.1038/s41586-022-05542-y (2022).
Mali, K. R. et al. Efficacy and safety of Molnupiravir in COVID-19 patients: A systematic review. Irish J. Med. Sci. (1971-) https://doi.org/10.1007/s11845-022-03139-y (2022).
Manabe, T., Kambayashi, D., Akatsu, H. & Kudo, K. Favipiravir for the treatment of patients with COVID-19: A systematic review and meta-analysis. BMC Infect. Dis. 21(1), 489. https://doi.org/10.1186/s12879-021-06164-x (2021).
Bosaeed, M. et al. Efficacy of favipiravir in adults with mild COVID-19: A randomized, double-blind, multicentre, placebo-controlled clinical trial. Clin. Microbiol. Infect. 28(4), 602–608. https://doi.org/10.1016/j.cmi.2021.12.026 (2022).
Ogawa, F. et al. Severity predictors of COVID-19 in SARS-CoV-2 variant, delta and omicron period; single center study. PLOS ONE 17(10), e0273134. https://doi.org/10.1371/journal.pone.0273134 (2022).
Dadras, O. et al. The relationship between COVID-19 viral load and disease severity: A systematic review. Immun. Inflamm. Dis. 10(3), e580. https://doi.org/10.1002/iid3.580 (2022).
Gao, C. et al. Proinflammatory cytokines are associated with prolonged viral RNA shedding in COVID-19 patients. Clin. Immunol. 221, 108611. https://doi.org/10.1016/j.clim.2020.108611 (2020).
Ceban, F. et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: A systematic review and meta-analysis. Brain Behav. Immun. 101, 93–135. https://doi.org/10.1016/j.bbi.2021.12.020 (2022).
Rudroff, T., Fietsam, A. C., Deters, J. R., Bryant, A. D. & Kamholz, J. Post-COVID-19 fatigue: Potential contributing factors. Brain Sci. 10(12), 1012. https://doi.org/10.3390/brainsci10121012 (2020).
Pacheco-Unguetti, A. P., Acosta, A., Callejas, A. & Lupiáñez, J. Attention and anxiety: Different attentional functioning under state and trait anxiety. Psychol. Sci. 21(2), 298–304. https://doi.org/10.1177/0956797609359624 (2010).
Lövdén, M., Fratiglioni, L., Glymour, M. M., Lindenberger, U. & Tucker-Drob, E. M. Education and cognitive functioning across the life span. Psychol. Sci. Public Interest 21(1), 6–41. https://doi.org/10.1177/1529100620920576 (2020).
Virtanen, M. et al. Long working hours and cognitive function: The whitehall II study. Am. J. Epidemiol. 169(5), 596–605. https://doi.org/10.1093/aje/kwn382 (2009).
Simione, L. & Gnagnarella, C. Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. Front. Psychol. Orig. Res. 11, 2166. https://doi.org/10.3389/fpsyg.2020.02166 (2020).
Garcia-Azorin, D. et al. Post-COVID-19 persistent headache: A multicentric 9-months follow-up study of 905 patients. Cephalalgia 42(8), 804–809. https://doi.org/10.1177/03331024211068074 (2022).
Santangelo, G. et al. Subjective cognitive failures and their psychological correlates in a large Italian sample during quarantine/self-isolation for COVID-19. Neurol. Sci. 42(7), 2625–2635. https://doi.org/10.1007/s10072-021-05268-1 (2021).
Beck, J. W. & Flow, A. The effects of contracting Covid-19 on cognitive failures at work: Implications for task performance and turnover intentions. Sci. Rep. 12(1), 8826. https://doi.org/10.1038/s41598-022-13051-1 (2022).
Brück, E. et al. Lack of clinically relevant correlation between subjective and objective cognitive function in ICU survivors: A prospective 12-month follow-up study. Crit. Care 23(1), 253. https://doi.org/10.1186/s13054-019-2527-1 (2019).
Sfera, A. et al. Neuronal and non-neuronal GABA in COVID-19: Relevance for psychiatry. Reports 5(2), 22 (2022).
Besteher, B. et al. Larger gray matter volumes in neuropsychiatric long-COVID syndrome. Psychiatry Res. 317, 114836. https://doi.org/10.1016/j.psychres.2022.114836 (2022).
Sandberg, K. et al. Occipital GABA correlates with cognitive failures in daily life. Neuroimage 87, 55–60. https://doi.org/10.1016/j.neuroimage.2013.10.059 (2014).
Acknowledgements
All authors thank all participants and the Faculty of Medicine at Hasanuddin University Indonesia for their contribution.
Funding
This study in Indonesia is funded by the Second Century Fund (C2F) of Chulalongkorn University Thailand. The funder has no role in the study design, data collection, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
B.H. and P.V. contributed to the conceptualization, methodology, project administration, formal analysis, and funding acquisition and wrote the original draft. F.F.H. and B.H. contributed to project administration, investigation, and supervision at the local level, and revised the intellectual content of the initial draft. M.C.W. and .P.C contributed to the methodology, and supervision, and finalized the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in the spelling of the author Pramon Viwattanakulvanid which was incorrectly given as Pramon Viwattankulvanid.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Herman, B., Wong, M.C.S., Chantharit, P. et al. Longitudinal study of disease severity and external factors in cognitive failure after COVID-19 among Indonesian population. Sci Rep 13, 19405 (2023). https://doi.org/10.1038/s41598-023-46334-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46334-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.