Abstract
Late-life balance disorders remain a severe problem with fatal consequences. Perturbation-based balance training (PBT), a form of rehabilitation that intentionally introduces small, unpredictable disruptions to an individual's gait cycle, can improve balance. The Tethered Pelvic Assist Device (TPAD) is a cable-driven robotic trainer that applies perturbations to the user's pelvis during treadmill walking. Earlier work showcased improved gait stability and the first evidence of increased cognition acutely. The mobile Tethered Pelvic Assist Device (mTPAD), a portable version of the TPAD, applies perturbations to a pelvic belt via a posterior walker during overground gait, as opposed to treadmill walking. Forty healthy older adults were randomly assigned to a control group (CG, n = 20) without mTPAD PBT or an experimental group (EG, n = 20) with mTPAD PBT for a two-day study. Day 1 consisted of baseline anthropometrics, vitals, and functional and cognitive measurements. Day 2 consisted of training with the mTPAD and post-interventional cognitive and functional measurements. Results revealed that the EG significantly outperformed the CG in several cognitive (SDMT-C and TMT-B) and functional (BBS and 4-Stage Balance: one-foot stand) measurements while showcasing increased confidence in mobility based on FES-I. To our knowledge, our study is the first randomized, large group (n = 40) clinical study exploring new mobile perturbation-based robotic gait training technology.
Similar content being viewed by others
Introduction
Late-life balance disorders remain a severe problem with fatal consequences1,2. Balance disorders can lead to impaired walking ability and the inability to adapt to the environment3. Abnormal walking ability and the inability to efficiently respond to instability increase the risk of falls. In the United States, falls account for the leading cause of fatal injuries among the older adults4 and consume billions of dollars in medical costs annually5. Not only that, but also falls cause anxiety, reduced mobility, and frequent clinic visits for patients6. Consequently, resolving balance disorders while preventing falls has become a foremost priority for public health7 among an increasingly aging US population8.
Perturbation-based balance training (PBT) can improve balance and reduce falls among older adults6,9,10,11. PBT is a form of rehabilitation that intentionally introduces minor, unpredictable disruptions to an individual’s gait cycle, allowing them to react and build motor skills safely. Through PBT, individuals can become more physically adept at recovering from real-life disruptive situations where they must control abrupt shifts in body weight or unexpected trips on external barriers6,12.
The methods of PBT implementation vary and include standing on a surface, like a thick foam, balance board, or slip board, or experiencing external forces applied by a physical therapist (PT), occupational therapist (OT), or a robotic platform13,14,15. One benefit of robotic platform PBT is the application of precise, measurable forces for specific time intervals. Utilizing robotic platforms in training enables PTs and OTs to progress and track training dosage and performance metrics systematically16.
There are numerous robotic platforms that provide PBT, and they can be distinguished by the location where the PBTs are applied, according to Shirota et al.17. Some devices apply perturbations at the foot level through an automated platform that changes position or orientation18,19,20) or even underfoot stiffness21. Soft exosuits can also apply perturbations to specific joints, like the hip joint with the SR-Hex22. Other platforms provide force pulses to the pelvis to study and train complete lower body reactions to these external forces. Rigid structures can apply these external forces, like that of the BAR-TM, which applies lateral perturbations23, or the exoskeletal LOPES III, which uses anterior perturbations24. While these allow large forces to be applied, they add inertia to the individual, which may alter human dynamics. A robot adding more than 6 kg of mass to the user’s pelvis can significantly alter their gait25. Cable-driven robotic gait trainers (CDRGTs) modulate the length or tension in cables to apply forces to the pelvis, like the TPAD26 or the CaLT27. These systems are typically lightweight and require multiple cables to apply forces in different directions.
The Robotics and Rehabilitation (RoaR) lab has developed the Tethered Pelvic Assist Device (TPAD, Fig. 1), a cable-driven robotic platform designed to apply customized forces to the pelvis for treadmill gait training, making it well suited for PBT28. A pilot study by Martelli et al.10 involved the TPAD and revealed promising results. The study investigated the effectiveness of a single session of PBT and established evidence of improved gait stability with the TPAD. Participants in the experiment group, i.e., those repeatedly subjected to multidirectional perturbations during training, were better adapted to counteract timed diagonal waist-pull perturbations. The study was also the first evidence of acute benefits to cognitive performance after PBT. They proposed that the likely mechanism behind this close relationship is the cerebral cortex, the outermost area of the brain, responsible for higher cognitive functions (e.g., complex decision-making or goal-setting), short-term memory, and social behavior29,30,31. The cerebral cortex also controls compensatory responses by priming the central nervous system to perturbations32. As such, cognitive performance relates to sensing perturbations and evoking a rapid balance reaction in the individual6.
The TPAD’s lightweight pelvic belt adds minimal inertia and lower limb restrictions to the user, minimally altering participants’ posture as they walk on a treadmill. However, treadmill gait differs from overground gait (walking over a natural surface, such as a sidewalk, floor, or trail) when differences in kinematic, kinetic, and electromyographic parameters are not considered33,34. Furthermore, variance in muscle activation has been noted between the two walking modalities35. Individuals on a treadmill exhibit differences, particularly in the tibialis anterior throughout the stance phase of the gait cycle, and in the vastus medialis, hamstrings, and adductor longus during swing. In addition, discernible differences are observable in joint movement. Those on the treadmill demonstrate less range of motion (ROM) in dorsiflexion, and knee extension, while greater ROM in hip extension35. Another study showed shear forces from the movement of the treadmill belt impact the center of pressure in the initial stance phase. Additionally, there is decreased propulsive force during late stance during treadmill walking due to minimal acceleration acted on an individual's center of mass36. Given the differences between treadmill and overground gait, treadmill constraint removal is essential. To improve accessibility and allow gait training during overground walking, our lab has also developed the mobile Tethered Pelvic Assist Device (mTPAD, Fig. 1), an overground extension of the TPAD37. The mTPAD, which uses a posterior rollator as the frame, does not require a treadmill and is a fully contained, portable device that may be better adaptable to various locations and with the potential for offsite training, expanding accessibility. Furthermore, the mTPAD is a low-cost system that could operate in low-resource settings.
Based on the promising results of the TPAD’s PBT and the ability of the mTPAD to provide similar perturbations during overground gait, the mTPAD allows the study of how overground PBT can impact older individuals’ balance and cognition. Our pilot study investigates overground PBT’s feasibility, safety, and effectiveness with the mTPAD in healthy adults 50 and older, the age when fall risk increases38. Our novel study is the first randomized, large group (n = 40) clinical study investigating the potential of overground PBT using mTPAD, a CDRGT. This technical advancement would translate to a new paradigm in functional rehabilitation that could assist patients in gaining or regaining their balance.
Methods
A functional and cognitive measures dataset was collected from a group of neurotypical older adults to evaluate the mTPAD’s potential for overground PBT. We hypothesize that a single session of PBT with the mTPAD can effectively produce acute improvements in cognitive performance and balance. Acute changes in balance were measured using (1) various functional task assessments, (2) a validated questionnaire, and (3) performance markers collected from an instrument gait mat. Additionally, vitals and anthropometric measurements further characterized functional performance. Three different screening tools and tests evaluated individuals’ cognitive function at baseline to track acute, subtle changes in cognitive function. By investigating these measures during multiple overground walking conditions, we can validate the mTPAD as a PBT tool and determine the mTPAD’s PBT effects on balance and cognition.
Participants
Forty healthy older adults, age 50 and older and who live independently, were randomly assigned to either the control group (CG, n = 20) or the experimental group (EG, n = 20). Assignment to the EG and CG was random using computer-generated numbers. A breakdown of each group’s characteristics is detailed in the results section. The exclusion criteria included: (1) the presence of acute, severe, or unstable medical illness; (2) reporting any significant neural, muscular, or skeletal disease; and (3) inability to safely walk overground without mobility aids, e.g., cane, walker, crutches. The Columbia University Medical Center Institutional Review Board approved this study (IRB Number: AAAT7862; Expiration Date: 07/04/2023). Before beginning, study personnel informed participants of the study procedure, risks, and benefits. Participants had the opportunity to ask questions, and once the research staff answered questions, all participants signed an informed consent form. Procedures were carried out adhering to all applicable guidelines and regulations throughout.
Procedure
Table 1 and Fig. 2 summarize the procedure for the two days participants were asked to come in.
Day 1 consisted of an intake interview and collection of baseline anthropometrics, functional measurements, and cognitive measurements. Functional measures included the 4-Stage Balance test, Falls Efficacy Scale—International (FES-I), Berg Balance Scale (BBS), and Short Physical Performance Battery (SPPB). For 4-Stage Balance test, the following parameters were measured: (1) Feet Side-by-Side, (2) Semi-tandem Stand, (3) Tandem Stand, and (4) One-foot stand.
Cognitive measurements included the Montreal Cognitive Assessment (MOCA) and Trail Making Test Parts A and B (TMT-A, TMT-B). In addition, participants were assessed by the Symbol Digit Modalities Test (SDMT) with the following parameters measured: SDMT-60s (SDMT-60), SDMT-90s (SDMT-90), and SDMT time to complete (SDMT-C). Baseline vitals were also obtained, including systolic and diastolic blood pressure and heart rate.
Day 2 consisted of training with the mTPAD, a mobile robotic platform that applies timed forces to the pelvis37,39, and post-intervention cognitive and functional measurements. The research team secured mTPAD’s pelvic belt snugly at the level of the iliac crests, and the mTPAD height was self-selected between 36–41 inches.
The mTPAD experimental protocol consisted of 5 trials: Gait Baseline, Test Pre, Training, Test Post, and Gait Post. Participants walked on the Zeno Walkway at their preferred pace throughout all 5 trials. The Zeno Walkway, created by Protokinetics, is a durable pressure-sensitive walkway mat equipped with multiple sensors to analyze gait and balance during walking (https://www.protokinetics.com/zeno-walkway/). All participants had the opportunity to practice walking before the start of the trials. All trials involved 5 min of walking except for Training, which consisted of 10 min of walking. The mTPAD applied perturbations at a force equal to ~ 10% of the participant’s body weight (BW). Participants in both the EG and CG were exposed to the same conditions for Gait Baseline, Test Pre, Test Post, and Gait Post. The Training served as the intervention and differentiated the EG and CG. During Gait Baseline, participants walked without cables and without perturbations to establish the participant’s baseline walking. The research team attached cables before the start of Test Pre. Participants experienced lateral perturbations randomized by direction (left or right) and timing during the trial while walking. Next, Training was conducted with cables still attached. For Training, the mTPAD applied either no perturbations (CG) or randomized perturbations (EG). The EG experienced diagonal perturbations comprised of a combination of a lateral force (left or right) and a vertical force (up or down). Perturbations were randomized by direction and timing throughout the trial. Test Post followed the training session. As with Test Pre, the EG and CG participants experienced randomized lateral perturbations (left or right). Finally, the research team removed the cables from the pelvic brace, and participants walked unperturbed for Gait Post. Participants could take a 5-min break after each condition. No falls, injuries, or adverse events occurred throughout the experimentation. Day 2 continued with a collection of vitals (blood pressure and heart rate). Participants completed a series of cognitive and functional tests similar to those performed on Day 1.
This study changed the perturbation forces based on the protocol condition, including lateral, superior/inferior, and diagonal in the frontal plane. These directions were selected to challenge lateral stability during overground gait. A square wave pulse was used for the perturbations for these three force conditions. The square wave had a low value of 0 Newtons, with a high value being the magnitude of the goal force applied during the experiment. The pulse width was 100 ms, and the timing between pulses was random to mitigate learning effects.
Measures
Cognitive measurements
We employed several widely used screening tools and tests to assess individuals’ baseline cognitive levels and to measure subtle, acute changes in cognitive functioning. To screen for cognitive impairment and evaluate the baseline cognitive function of individuals, we used the MOCA40. To detect subtle, acute changes in cognitive function before and after the mTPAD, we used the TMT and SDMT. The TMT assesses cognitive function by measuring a person’s combined visual attention, mental flexibility, and psychomotor speed41. The SDMT Symbol Digit Modalities measure processing and motor speed42.
Functional measurements
Our study consisted of various functional assessments, including the 4-Stage Balance test, FES-I, BBS, and SPPB. The 4-Stage Balance test assessed static postural balance43. The Falls Efficacy Scale-International (FES-I) is a self-report measure used to assess an individual’s confidence in their ability to perform activities without falling44. The BBS and SPPB are tools used to measure functional fitness and mobility in older adults. For each, scores are calculated based on the individual’s performance on each test, with higher scores indicating better functional fitness and mobility45,46.
Quantitative measurements
As part of the non-clinical data analysis, several key performance measurement variables were collected from the Zeno Walkway and are defined in this section. These temporal, spatial, and pressure-related variables were used for the gait analysis and calculated using the ProtoKinetic software PKMAS47. Stride length is the distance between two successive ipsilateral heel strikes in centimeters48. Stride velocity is the average velocity for each stride. The single support time is the time in seconds when only one foot is in contact with the ground. The integrated pressure measurement quantitatively characterizes the contact between the ground and the foot during locomotion49 and is calculated as the area under each footfall’s pressure curve.
In addition to these parameters, the center of pressure (COP) cyclogram is investigated50. The COP cyclogram is the locus of the COP during a gait cycle51. The COP cyclogram is a butterfly-shaped pattern used in gait analysis that illustrates COP trajectories over time during different phases of the gait cycle. This gait analysis tool spatially illustrates the trajectory of the COP by plotting the COP’s mediolateral displacement with respect to the forward progression on the x-axis against the anteroposterior displacement on the y-axis. By superimposing the two feet next to each other, the COP cyclogram visualizes the cyclic COP trajectory with respect to the individual’s feet and can quantify gait symmetries for those with asymmetric gait like stroke survivors52.
When the individual is in single stance, the COP moves forward along the stance foot, or the foot in contact with the ground. When the foot swinging through the air first contacts the ground again at the heel, and the individual is now on both feet, the COP shifts away from the original stance foot as the individuals shifts their weight from that foot to the other. By studying the cyclic pattern of the COP during gait, gait symmetries and efficiencies can be evaluated especially by investigating where the COP trajectory overlaps, or the COP Cyclogram Intersection Point (CISP). The CISP is studied for both the EG and CG. The CISP change is monitored in the anterior–posterior (AP) and medial–lateral (ML) directions and measures the COP trajectory symmetry. The efficiency of the COP path can also be evaluated, especially during single stance. The single stance COP efficiency is calculated by dividing the magnitude of the horizontal COP vector from the beginning to the end of each foot’s single stance COP trajectory by the actual distance the COP travels. If these distances are the same, or the COP exactly follows the vector from the beginning to the end of the single stance, the COP is 100% efficient. The larger the deviations from this vector, the less efficient and more unstable the gait. These gait measures will illustrate how the gait and stability of the individuals are affected during the different trials.
Anthropometric, socio-demographic, and vitals
Anthropometric measurements included participants’ height, body weight, and hip width and depth. We also assessed the following socio-demographic factors: fall risk, education level, subjective health (5 = excellent; 4 = very good; 3 = good; 2 = fair; 1 = poor), employment status, and housing status. The vitals we obtained included systolic blood pressure, diastolic blood pressure, and heart rate. To assess fall risk, individuals who responded “yes” or affirmatively to any of the following questions were considered “at-risk”13:
-
(1)
Have you fallen in the past 5 years?
-
(2)
Have you lost your balance or almost fallen in recent memory?
-
(3)
Have you reduced your activities or changed your lifestyle because you were concerned that you might fall?
-
(4)
Do you ever feel unsteady when: getting in or out of a chair, changing direction when you are standing or walking, reaching for something above your head, or walking and talking to someone at the same time?
-
(5)
Has anyone, such as a friend or family member, expressed concern that you may have problems with your balance or are at risk of falling?
Statistical analysis
All statistical analyses were performed with Stata 15 (StataCorpLP, College Station, TX, USA), Python version 3.10.8 (Python Software Foundation, Delaware, United States), or Microsoft Excel Office 365 (Microsoft Corporation, Washington, United States). Two-sided p-values of less than 0.05 were considered statistically significant for all tests and were defined as *p < 0.05, **p < 0.01, ***p < 0.001.
Table 2 is a descriptive analysis comparing all of the collected Day 1 baseline data (e.g., cognitive, functional, anthropometrics) between the EG and CG. Table 2 reports all continuous variables (e.g., weight, height, age) as mean ± standard deviation (SD). In contrast, the table presents categorical variables (e.g., sex, education, employment status) with the number and percentage of the total. To obtain p-values and assess differences in Day 1 baseline data between the EG and CG, a Pearson’s Chi-squared test was performed for categorical variables, while a paired t-test was performed for continuous variables.
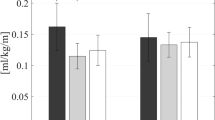
Figure 3 shows the results of a two-factor mixed analysis of variance (mANOVA) comparing vitals, functional measurements, and cognitive measurements obtained on Day 1 and Day 2 for both the EG and CG. Group (EG, CG) and session (Day 1, Day 2) served as between and within-subject factors, respectively.
Plot of Day 1 vs. Day 2 for Vitals (A), Cognitive Measurements (B), and Functional Measurements (C) by group (EG and CG). Means and 95% confidence intervals are plotted per group per day. Statistically significant values were defined with stars as *p < 0.05, **p < 0.01, ***p < 0.001. Main effects of trials are illustrated by black bars and stars underneath each graph’s title, while interaction effect significance is denoted by “IE:” with stars in the lower left-hand corner of graphs where p < 0.05. Interaction effects indicated statistically significant main effects of the session (Day 1, Day 2) × group (EG, CG) interaction term, respectively.
For the gait data, two types of analyses were used. For the comparisons between the Gait Baseline and Gait Post for the EG and CG, an mANOVA was used. An mANOVA was also used for the Test Pre and Test Post comparisons between the EG and CG. All data were checked for normality, sphericity, and homoscedasticity before applying the mANOVA. If the sphericity and homoscedasticity requirements were met, but the data were not normal, then a natural log transform was used. When comparing the training data for the EG and CG, an independent t-test was used if the data satisfied the normality and homoscedasticity conditions. If significantly not normal, a Mann–Whitney U test was used to compare the means. These tests were run for each variable’s mean and standard deviation. By investigating the changes in the standard deviation per person, we can explore the differences in variability induced by perturbation training.
Results
Demographics and baseline
The demographics were analyzed to determine differences between the EG and CG, and shown in Table 2. The average age of participants for both groups was 71 (± 8) years old (p = 0.906). No significant difference was observed between the EG and CG in the collected Day 1 baseline data. Of note, there was no significant difference in Day 1 cognitive performance between the EG and CG, including the MOCA (p = 0.224), TMT A (p = 0.762), TMT B (p = 0.971), SDMT-C (p = 0.842), SDMT-90 (p = 0.946), and SDMT-60 (p = 0.589). In addition, no differences were observed in any Day 1 functional measurement between the EG and CG, including the FES-I (p = 0.780), BBS (p = 0.854), SPPB (p = 0.304), and all 4-Stage Balance tests: (feet side-by-side (p = 1.000); semi-tandem stand (p = 0.560); tandem stand (p = 0.681); one-foot stand (p = 0.740).
Clinical data
Results comparing the clinical data (vitals, cognitive measurements, and functional measurements) of both days by the group are depicted in Fig. 3.
When comparing the vitals of Day 2 to those of Day 1, we observed that all individuals showed significantly elevated systolic blood pressure (F(1,1) = 9.93, p = 0.002), diastolic blood pressure (F(1,1) = 5.81, p = 0.018), and heart rate (F(1,1) = 7.64, p = 0.007) on Day 2. However, no significant interaction effects for the group-x-session were found for any of the vitals: systolic blood pressure (p = 0.411), diastolic blood pressure (p = 0.987), and heart rate (p = 0.802). This indicates that group placement did not significantly alter the vitals.
When comparing Day 2 cognitive measurements to those of Day 1, all test participants showed significantly shorter times for the TMT-B (F(1,1) = 15.15, p < 0.001), SDMT-C (F(1,1) = 18.19, p < 0.001), SDMT-90 (F(1,1) = 78.76, p < 0.001), and SDMT-60 (F(1,1) = 115.46, p < 0.001) on Day 2. No significant interaction effects for the group-x-session were found for the SDMT-90 (p = 0.726) and SDMT-60 (p = 0.148), indicating that group placement did not alter the test improvements. However, a significant interaction of group-x-session was seen for the TMT-B (p < 0.001) and SDMT-C (p = 0.021), highlighting that group placement did alter the rate of improvement between Day 1 to Day 2 and that the EG outperformed the CG in those cognitive tests. TMT-A had no significant main or interaction effect of the group-x-session, indicating that neither group placement nor session significantly impacted performance.
Regarding functional measurements, and when comparing Day 2 to those of Day 1, all individual participants showed significantly lower scores for the FES-I (F(1,1) = 27.81, p < 0.001) on Day 2. At the same time, both groups had significantly higher BBS (F(1,1) = 64.64, p < 0.001) and 4-Stage Balance: one-foot stand (F(1,1) = 20.21, p < 0.001) on Day 2. Further analysis revealed a significant interaction of group-x-session for the FES-I (p = 0.010), BBS (p < 0.001), and 4-Stage Balance: one-foot stand (p = 0.014), highlighting that group placement did alter the rate of improvement between Day 1 to Day 2 and that the EG outperformed the CG on those functional measurements. There were no significant main or interaction effects of group-x-session for SPPB (p = 0.698), 4-Stage Balance: feet side-by-side (p = 1.000), 4-Stage Balance: semi-tandem (p = 0.634), 4-Stage Balance: tandem (p = 0.609), and thus indicates that neither group placement nor session significantly affected performance.
Gait analysis
The mANOVA was repeated for two different trial combinations. The primary objective of this analysis was to determine the variance of gait-related functional parameters during and after the training. This mANOVA was conducted initially between the Gait Baseline and Gait Post trials and secondly between the Test-Pre and Test-Post trials. These trial combinations will be called the Gait and Test trials, respectively. Additionally, an unpaired t-test was conducted for the Training trials to identify any statistically significant differences between the EG and CG.
Gait trials (gait baseline vs. gait post)
To determine if the entire training altered the unperturbed walking between the EG and CG groups, the means and standard deviations of the Gait Baseline and Gait Posts were compared for each group (Fig. 4). Significant main effect of trials were found for the stride length (F(1,36) = 12.6, p = 0.0011), transformed stride velocity (F(1,36) = 15.0, p < 0.001), transformed integrated pressure (F(1,36) = 11.4, p = 0.002), and CISP AP % (F(1,36) = 5.8, p = 0.021). No main effects of trials were found for the CISP ML %, SS COP Path Efficiency, or Single Support Time (p > 0.05). No significant interaction effects were found for the unperturbed trials and groups. Therefore, all participants took longer, faster strides with a more anterior CISP AP % and a lower integrated pressure during the Gait Post trial, regardless of group placement.
Plot of gait baseline vs. gait post for the control and experimental groups for gait characteristics. Means and 95% confidence intervals are plotted per group per trial. Statistically significant values were defined with stars as *p < 0.05, **p < 0.01, ***p < 0.001. Main effects of trials are illustrated by black bars and stars underneath each graph’s title, while interaction effect significance is denoted by “IE:” with stars in the lower left-hand corner of graphs where p < 0.05.
For the variability, each participant’s standard deviations were evaluated. Significant main effect of trials were found for the transformed stride length variability (F(1,36) = 4.1, p = 0.0498), transformed CISP ML % variability (F(1,36) = 4.2, p = 0.047), and the SS COP Path efficiency variability (F(1,36) = 11.6, p = 0.0016) with no interaction effect. No significant main effects of trials were found for the CISP AP % variability, single support time variability, integrated pressure variability, or stride velocity variability (p > 0.05). Therefore, all participants had less variable stride length, SS COP efficiency, and CISP ML % during the Gait Post trial regardless of group placement.
Test trials (test pre vs. test post)
To determine if the perturbation training altered the response to the testing perturbations between the EG and CG groups, the means and standard deviations of the Test Pre and Test Posts were compared for each group (Fig. 5). Significant main effect of trials were found for the stride length (F(1,36) = 18.6, p < 0.001) and stride velocity (F(1,36) = 13.0, p < 0.001), and CISP AP % (F(1,36) = 25.6, p < 0.001). No significant main effects of trials were found for the integrated pressure, CISP ML %, SS COP path efficiency, or single support time (p > 0.05). No significant interaction effects were found for Test trials and Perturbation groups. Therefore, all participants took longer, faster strides with a more anterior CISP AP % during the Test Post trial regardless of group placement.
Plot of test pre vs. test post for the control and experimental groups for gait characteristics. Means and 95% confidence intervals are plotted per group per trial. Statistically significant values were defined with stars as *p < 0.05, **p < 0.01, ***p < 0.001. Main effects of trials are illustrated by black bars and stars underneath each graph’s title, while interaction effect significance is denoted by “IE:” with stars in the lower left-hand corner of graphs where p < 0.05. Interaction effects indicate statistically significant effects of the session (Pre, Post) × group (EG, CG) interaction term.
For the variability, each participant’s standard deviations were evaluated. Significant main effect of trials were found for the time in single support variability (F(1,36) = 7.2, p = 0.011) and transformed CISP AP % variability (F(1,36) = 4.2, p = 0.49) with no interaction effect. Significant interaction effect was seen in the transformed CISP ML % variability (F(1,36) = 4.3, p = 0.045) with no significant main effect of trial. No significant main effects of trials were found for the stride length variability, SS COP path efficiency variability, CISP ML % variability, integrated pressure variability, or stride velocity variability (p > 0.05). Therefore, all participants had less variable single support times and CISP AP % during the Test Post trial regardless of group placement. However, the group placement did significantly affect how the CISP ML % variability changed between the Test Pre and Test Post trials.
Training trials
The differences in each participant’s mean and standard deviation are investigated by comparing the EG’s training to the CG’s and shown in Fig. 6. When comparing the two groups means, the SS COP Efficiency was significantly lower in the EG compared to the CG (EG: 98.7 ± 0.7%, CG: 99.2 ± 0.6%, U = 278, p = 0.0046). The SS COP Efficiency variability was also significantly higher in the EG (EG: 1.15 ± 0.7%, CG: 0.74 ± 0.3%, t = − 2.26, p = 0.030). However, the Stride Length variability was significantly higher in the CG than the EG (EG: 5.14 ± 1.5 cm, CG: 7.31 ± 3.2 cm, U = 265, p = 0.014). No significant differences were found for the integrated pressure, stride length, stride velocity, CISP ML %, CISP AP %, single support time (p > 0.05). No significant differences were found in the variabilities of the CISP ML %, CISP AP %, single support time, integrated pressure, or stride velocity (p > 0.05). Therefore, individuals that experienced the perturbation training had less efficient SS COP trajectories with higher variability, and also walked with less variable stride lengths.
Discussion
Our study investigated the acute effects of PBT with a single session of mTPAD in healthy, neurotypical adults 50 and older. Our study demonstrated several novel findings: a single session of PBT delivered by the mTPAD led to (1) significantly increased cognitive performance in the EG, in addition, we observed (2) significantly increased functional performance by the EG. This is the first randomized, large group (n = 40) clinical study exploring overground perturbation-based CDRGT. As such, future robotic gait trainers that support patients in gaining or regaining their balance may be developed with the help of the research from our study.
The study provides further evidence of acute cognitive improvements after a single session of PBT and aligns with some of the results in Martelli et al.10. Specifically, our results revealed that the EG completed the SDMT-C in significantly less time than the CG (Fig. 3B). We agree with the explanation Martelli et al.10 provided that describes the reasons for the observation. In response to perturbations delivered while walking, the base of support changes rapidly, requiring spatial navigation, coordination, and physical affordances53. To maintain balance, sensorimotor and cognitive processing are necessary for specific domains depending on the task’s type and complexity. We also hypothesize that exposure to perturbations is related to increased activation of cognitive control processes, particularly domains dedicated to the integration of motion and processing speed2,54,55,56,57. Thus, this mode of cognitive activation in the EG may have continued even without stimulation, allowing for increased speed in the SDMT. Extending from Martelli et al.10, we also observed that the EG solved the TMT-B faster than the CG after training, while no significant difference was observed in Martelli et al.10. One possible explanation for this difference is that our study benefited from a larger sample size (n = 40 vs. n = 28) and thus increased statistical power to detect acute, subtle changes. In addition, the inclusion of the MOCA provides a means to screen for underlying cognitive impairments that were not performed priorly. All participants scored within the normal range for the MOCA, with no significant difference between the two groups (Table 2). Furthermore, new evidence points to the validity of the TMT or variants to assess motor-cognitive performance in individuals58,59. Also included in our study was the collection of vitals. Obtained vitals provides evidence that perturbations experienced by the EG did not significantly increase participants’ symptomatic response and arousal than the CG, and thus likely would not be a major contributing factor to observed differences in the EG and CG60. We noted that vitals for both the EG and CG, while significantly elevated upon the mTPAD, were not significantly different between the EG and CG (Fig. 3A).
Our results demonstrated that following the delivery of PBT with the mTPAD, the EG was more adapted to functional tasks, and participants in the EG displayed higher mobility confidence (Fig. 3C). This was evident by participants in the EG standing longer on the 4-Stage Balance Test (one-foot stand) and achieving a higher score on the BBS, which assesses balance through a series of functional tasks. In addition, the EG displayed decreased self-reported concerns about falling after their session as measured by the FES-I.
While there is significant visible variation within the Day 1 and Day 2 clinical test results, the differences in gait characteristics had fewer interaction effects between the group placement and conditions. When walking without force, all study participants took longer, faster strides in the Gait Post session compared to the Gait Baseline. All participant’s CISP AP values were significantly more anterior. This suggests that after undergoing the entire protocol, all participants’ single stance COP trajectory progressed further along the foot, bringing the CISP AP forward. This, along with the significant decrease in integrated pressure, could be tied to increased stride length and velocity, as the lengthening of the stride could have forced the COP further forward along the foot while in a single stance. The variabilities of the stride length, CISP ML, and SS COP path efficiency decreased in Gait Post, indicating that these measures were more repeatable at the end of the protocol. No interaction effects were found for any variable, illustrating that the Experimental condition did not alter any gait characteristics during unloaded walking.
Similar effects were found when comparing the Test Pre and Test Post conditions. All participants took longer, faster strides with a less posterior CISP AP during the second round of lateral perturbations. These changes mirror the changes made from Gait Baseline to Gait Post, which may indicate that participants were more comfortable walking in the mTPAD as the protocol went on. This increase in stride velocity could be a benefit to the individuals as a result of the entire protocol, as slower dual-task walking in older adults has been associated with higher risks of falls61,62. In the second half of the protocol, all participants walked faster, elongating their strides. All participants also had less variable single support time and CISP AP values, supporting that their gait became more regular as they walked. However, the CISP ML variability had a significant interaction effect. While the control group’s ML CISP variability increased slightly from Test Pre to Test Post, the experimental group’s ML CISP variability decreased in Test Post. This decrease in variability for the experimental group highlights that after undergoing the training perturbations, their ML stability increased for the second round of testing perturbations. This improvement of ML stability from Test Pre to Test Post was not seen in the control group, who walked unperturbed for 10 min during the training session. It is possible that the control group, after walking without perturbations for 10 min, were more affected by the lateral perturbations. Therefore, the ML CISP was less variable for those who experienced other perturbations during the training session, highlighting an increased ML stability. While the relative decrease of the EG’s group CISP ML variability may not be clinically relevant, this result highlights the mTPAD perturbations’ ability to train individuals to withstand variability in the ML CISP caused by lateral perturbations.
While the training perturbations caused a decrease in the ML CISP variability during the lateral perturbations, there were also some differences in the training session between the control group and the experimental group. During the training session, the experimental group had significantly less efficient SS COP paths with higher variability and less variable stride lengths than the control group. Having a less efficient COP path with higher variability illustrates that the random perturbations could introduce variability and alter the COP progression of the individuals in the experimental group, which was one goal of this experiment. This significant decrease in efficiency and increase in variability also highlight the efficacy of the mTPAD as an overground perturbation platform. This increase in COP path deviation may be related to the clinical improvements seen by the experimental group, as this is the critical difference between individuals in the EG and CG.
Although the mTPAD is a fully contained, portable, low-cost robotic trainer, it has limitations. The mTPAD’s compact nature limited perturbations to ~ 10% BW. A more rigid frame and powerful motors could increase ground reaction force. Further studies should assess whether acute aftereffects of PBT via the mTPAD produce long-term changes in gait stability and cognitive performance and can be explored by implementing multiple-session training and follow-up. Such a study would benefit from an even larger sample size and a broader range of older adults. Furthermore, although we observed significant changes in the SDMT-C and TMT-B, which assess cognitive performance, and the 4-Stage Balance test, BBS, and FES-I, which serve as functional measurements, several cognitive or functional measurements were not significantly different (Fig. 3A–C). We observed no significant difference in both the main and interaction effect of the following (1) cognitive measurements (SDMT-60, SDMT-90, and TMT-A) and (2) functional measurements (SPPB, 4-Stage Balance: Feet Side-by-Side, 4-Stage Balance: Semi-tandem Stand, 4-Stage Balance: Tandem Stand). Explanations to these observations are (1) regarding non-significant cognitive measurements, the SDMT-60 and SDMT-90 represent the number of correct responses in 60 s and 90 s, respectively, while the SDMT-C represents the completion time in seconds. The difference in range for the SDMT-60 and SDMT-90 were 41 and 61, respectively, versus 260 for the SDMT-C. The SDMT-60 and SDMT-90 may not necessarily represent when most participants completed the task, making them less sensitive benchmarks for detecting subtle, acute differences. A similar consideration should be made when comparing TMT-A and TMT-B. Participants are scored on the completion time and asked to draw a single line to numbered circles for the TMT-A (e.g., 1-2-3-4-5-6). In contrast, participants must alternate between numbers and letters (e.g., 1-A-2-B-3-C) for the TMT-B, and thus more challenging and sensitive. Given the increased complexity, TMT-B requires more time for completion63 as the TMT-B is viewed as a measurement of higher-level cognitive ability64. (2) Regarding non-significant functional measurements, when comparing the SPPB to the BBS, both assessments of functional tasks, the SPPB has a low diagnostic value in detecting acute, incremental changes to predict negative health-related outcomes balance65. For the 4-Stage Balance test, participants perform four progressively challenging positions starting with a two-feet stand to a one-foot stand. We observed a significant difference in the interaction effect between the EG and CG with the one-foot stand, the most challenging and, thus, the likely most sensitive benchmark. Although no study has comparatively validated each stage individually, single leg stance has often been shown sensitive to detect a significant change in a clinical setting66,67,68. With respect to cognitive and functional tests and among key findings with a significant difference (e.g., SDMT-C, TMT-B, FES-I, BBS, 4-Stage Balance: one-foot stand), the observed difference in the SDMT-C between the two treatment groups on Day 2 was above the minimum detectable change (MCD)69, while the FES-I and BBS were not70,71. To our knowledge, no study has individually evaluated the MCD for the TMT-B and 4-Stage Balance: one-foot stand. Given the difference observed in the FES-I and BBS were below MCD, and unknown for TMT-B and 4-Stage Balance: one-foot stand, we cannot fully rule out the results were due to chance.
While further investigation is needed to fully elucidate the benefits and limitations of mobile perturbation-based robotic gait training technology, current evidence indicates that this technology represents a valuable tool in rehabilitation. The technology’s versatility makes it adaptable to various clinical settings, including inpatient rehabilitation facilities, outpatient clinics, and home environments. Another benefit is that the technology can be employed cheaply and function in low-resource settings. Moreover, a key advantage is its capacity to provide consistent and precise feedback to patients during their training sessions which can be tailored to the individual’s specific needs. In conclusion, mobile perturbation-based robotic gait training technology shows great potential in improving individuals’ mobility, balance, and cognitive affluence.
Data availability
The datasets generated during and/or analyzed during the current study will be uploaded to a central repository and made easily available. A curated version of the data will be available at https://1drv.ms/f/s!AjScxpGKPMIOg7o7pV8q2rr5iNAtTw?e=zSyVvY.
References
Holtzer, R. et al. The relationship between specific cognitive functions and falls in aging. Neuropsychology 21, 540–548 (2007).
Snijders, A. H., van de Warrenburg, B. P., Giladi, N. & Bloem, B. R. Neurological gait disorders in elderly people: Clinical approach and classification. Lancet Neurol. 6, 63–74 (2007).
Balance disorders—NIDCD. National Institute on Deafness and Other Communication Disorders (2017). https://www.nidcd.nih.gov/sites/default/files/Documents/health/balance/BalanceDisorders-508.pdf (Accessed 17 Apr 2023).
Bolton, L. Preventing fall injury. Wounds: A compendium of clinical research and practice (2019). https://pubmed.ncbi.nlm.nih.gov/31730506/ (Accessed 17 Apr 2023).
Florence, C. S. et al. Medical costs of fatal and nonfatal falls in older adults. J. Am. Geriatr. Soc. 66, 693–698 (2018).
Mansfield, A., Wong, J. S., Bryce, J., Knorr, S. & Patterson, K. K. Does perturbation-based Balance Training Prevent Falls? systematic review and meta-analysis of preliminary randomized controlled trials. Phys. Therapy 95, 700–709 (2015).
Sturnieks, D., St George, R. & Lord, S. Balance disorders in the elderly. Neurophysiol. Clin. 38, 467–478 (2008).
Juan, S. M. & Adlard, P. A. Ageing and cognition. Subcell. Biochem. 91, 107–122. https://doi.org/10.1007/978-981-13-3681-2_5 (2019).
Gerards, M. H. G., McCrum, C., Mansfield, A. & Meijer, K. Perturbation-based balance training for falls reduction among older adults: Current evidence and implications for clinical practice. Geriatr. Gerontol. Int. 17, 2294–2303 (2017).
Martelli, D., Kang, J., Aprigliano, F., Staudinger, U. M. & Agrawal, S. K. Acute effects of a perturbation-based balance training on cognitive performance in healthy older adults: A pilot study. Front. Sports Act. Living 3, 688519 (2021).
McCrum, C. et al. Perturbation-based balance training: Principles, mechanisms and implementation in clinical practice. Front. Sports Act. Living 4, 1015394 (2022).
Schmidt, H., Piorko, F., Bernhardt, R., Kruger, J., & Hesse, S. Synthesis of perturbations for gait rehabilitation robots. In 9th International Conference on Rehabilitation Robotics, 2005. ICORR 2005, 74–77 (IEEE, 2005).
Mansfield, A., Peters, A. L., Liu, B. A. & Maki, B. E. A perturbation-based balance training program for older adults: Study protocol for a randomised controlled trial. BMC Geriatr. 7, 12 (2007).
Lurie, J. D. et al. Surface perturbation training to prevent falls in older adults: A highly pragmatic, randomized controlled trial. Phys. Therapy 100(7), 1153–1162 (2020).
Meyer, A. et al. A novel body weight-supported postural perturbation module for gait and balance rehabilitation after stroke: Preliminary evaluation study. JMIR Rehabil. Assist. Technol. 9(1), e31504 (2022).
Turner, D. L., Ramos-Murguialday, A., Birbaumer, N., Hoffmann, U. & Luft, A. Neurophysiology of robot-mediated training and therapy: A perspective for future use in clinical populations. Front. Neurol. 4, 184 (2013).
Shirota, C. et al. Robot-supported assessment of balance in standing and walking. J. NeuroEng. Rehabil. 14, 80 (2017).
Kalron, A., Fonkatz, I., Frid, L., Baransi, H. & Achiron, A. The effect of balance training on postural control in people with multiple sclerosis using the Caren Virtual Reality System: A pilot randomized controlled trial. J. NeuroEng. Rehabil. 13, 13 (2016).
van Asseldonk, E. H. F., Carpenter, M. G., van der Helm, F. C. T. & van der Kooij, H. Use of induced acceleration to quantify the (de)stabilization effect of external and internal forces on postural responses. IEEE Trans. Biomed. Eng. 54, 2284–2295 (2007).
Klamroth, S. et al. Interindividual balance adaptations in response to perturbation treadmill training in persons with Parkinson disease. J. Neurol. Phys. Therapy 43, 224–232 (2019).
Chambers, V. & Artemiadis, P. Repeated robot-assisted unilateral stiffness perturbations result in significant aftereffects relevant to post-stroke gait rehabilitation. In 2022 International Conference on Robotics and Automation (ICRA). https://doi.org/10.1109/icra46639.2022.9812323 (2022).
Baye-Wallace, L., Thalman, C. M. & Lee, H. Entrainment during human locomotion using a lightweight soft robotic hip exosuit (SR-HExo). IEEE Robot. Autom. Lett. 7, 6131–6138 (2022).
Matjačić, Z., Zadravec, M. & Olenšek, A. Feasibility of robot-based perturbed-balance training during treadmill walking in a high-functioning chronic stroke subject: A case–control study. J. NeuroEng. Rehabil. 15, 32 (2018).
Farkhatdinov, I. et al. Assisting human balance in standing with a robotic exoskeleton. IEEE Robot. Autom. Lett. 4, 414–421 (2019).
Meuleman, J., Terpstra, W., van Asseldonk, E. H. & van der Kooij, H. Effect of added inertia on the pelvis on gait. In 2011 IEEE International Conference on Rehabilitation Robotics. https://doi.org/10.1109/icorr.2011.5975493 (2011).
Luna, T. D., Santamaria, V., Ai, X. & Agrawal, S. K. Reactive postural control during sit-to-stand motion. IEEE Robot. Autom. Lett. 7, 7185–7192 (2022).
Lin, J.-T. et al. Varied movement errors drive learning of dynamic balance control during walking in people with incomplete spinal cord injury: A pilot study. Exp. Brain Res. 238, 981–993 (2020).
Vashista, V., Jin, X. & Agrawal, S. K. Active tethered pelvic assist device (A-TPAD) to study force adaptation in human walking. In 2014 IEEE International Conference on Robotics and Automation (ICRA). https://doi.org/10.1109/icra.2014.6906933 (2014).
Molnár, Z. et al. New insights into the development of the human cerebral cortex. J. Anat. 235, 432–451 (2019).
Mesulam, M.-M. Chapter 28 the systems-level organization of cholinergic innervation in the human cerebral cortex and its alterations in Alzheimer's disease. In Cholinergic Mechanisms: From Molecular Biology to Clinical Significance 285–297. https://doi.org/10.1016/s0079-6123(08)62112-3 (1996).
Teffer, K. & Semendeferi, K. Human prefrontal cortex. Evolution of the Primate Brain 191–218. https://doi.org/10.1016/b978-0-444-53860-4.00009-x (2012).
Bolton, D. A. E. The role of the cerebral cortex in postural responses to externally induced perturbations. Neurosci. Biobehav. Rev. 57, 142–155 (2015).
Alton, F., Baldey, L., Caplan, S. & Morrissey, M. C. A kinematic comparison of overground and treadmill walking. Clin. Biomech. 13, 434–440 (1998).
Semaan, M. B. et al. Is treadmill walking biomechanically comparable to overground walking? A systematic review. Gait Posture 92, 249–257 (2022).
Lee, S. J. & Hidler, J. Biomechanics of overground vs. treadmill walking in healthy individuals. J. Appl. Physiol. 104, 747–755 (2008).
Hutchinson, L. A., De Asha, A. R., Rainbow, M. J., Dickinson, A. W. L. & Deluzio, K. J. A comparison of centre of pressure behaviour and ground reaction force magnitudes when individuals walk overground and on an instrumented treadmill. Gait Posture 83, 174–176 (2021).
Stramel, D. M. & Agrawal, S. K. Validation of a forward kinematics based controller for a mobile tethered pelvic assist device to augment pelvic forces during walking. In 2020 IEEE International Conference on Robotics and Automation (ICRA). https://doi.org/10.1109/icra40945.2020.9196585 (2020).
Elliott, S., Painter, J. & Hudson, S. Living alone and fall risk factors in community-dwelling middle age and older adults. J. Community Health 34, 301–310 (2009).
Stramel, D. M., Prado, A., Roy, S. H., Kim, H. & Agrawal, S. K. Effects of timed frontal plane pelvic moments during overground walking with a mobile TPAD system. IEEE Trans. Neural Syst. Rehabil. Eng. 31, 48–57 (2023).
Nasreddine, Z. S. et al. The Montreal Cognitive Assessment, MOCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53, 695–699 (2005).
Bowie, C. R. & Harvey, P. D. Administration and interpretation of the trail making test. Nat. Protoc. 1, 2277–2281 (2006).
Ryan, J. et al. Normative data for the symbol digit modalities test in older white Australians and Americans, African-Americans, and Hispanic/latinos. J. Alzheimer’s Dis. Rep. 4, 313–323 (2020).
Assessment the 4-stage balance test. CDC. https://www.cdc.gov/steadi/pdf/STEADI-Assessment-4Stage-508.pdf (Accessed 17 Apr 2023).
Yardley, L. et al. Development and initial validation of the falls efficacy scale-international (FES-i). Age Ageing 34, 614–619 (2005).
Guralnik, J. M. et al. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 49, M85–M94 (1994).
Miranda-Cantellops, N. & Tiu, T. K. Berg balance testing. Statpearls (2023). https://www.ncbi.nlm.nih.gov/books/NBK574518/ (Accessed 17 Apr 2023).
Lynall, R. C., Zukowski, L. A., Plummer, P. & Mihalik, J. P. Reliability and validity of the protokinetics Movement Analysis Software in measuring center of pressure during walking. Gait Posture 52, 308–311 (2017).
Whittle, M. W. Gait Analysis (Elsevier, 2007).
Giacomozzi, C., Caravaggi, P., Stebbins, J. A. & Leardini, A. Integration of foot pressure and foot kinematics measurements for medical applications. Handbook of Human Motion 1–22. https://doi.org/10.1007/978-3-319-30808-1_186-1 (2016).
Roerdink, M. et al. Gaitography applied to prosthetic walking. Med. Biol. Eng. Comput. 52, 963–969 (2014).
Viteckova, S. et al. Gait symmetry measures: A review of current and prospective methods. Biomed. Signal Process. Control 42, 89–100 (2018).
Stramel, D. M., Winterbottom, L., Stein, J. & Agrawal, S. K. Overground robotic gait trainer mtpad improves gait symmetry and weight bearing in stroke survivors. Bioengineering 10, 698 (2023).
Maki, B. E. & McIlroy, W. E. Cognitive demands and cortical control of human balance-recovery reactions. J. Neural Transm. 114, 1279–1296 (2007).
Sturnieks, D. L. et al. Sensorimotor and neuropsychological correlates of force perturbations that induce stepping in older adults. Gait Posture 36, 356–360 (2012).
Senden, R. et al. The influence of age, muscle strength and speed of information processing on recovery responses to external perturbations in Gait. Gait Posture 39, 513–517 (2014).
Patel, P. J. & Bhatt, T. Attentional demands of perturbation evoked compensatory stepping responses: Examining cognitive-motor interference to large magnitude forward perturbations. J. Motor Behav. 47, 201–210 (2015).
Wittenberg, E., Thompson, J., Nam, C. S. & Franz, J. R. Neuroimaging of human balance control: A systematic review. Front. Hum. Neurosci. 11, 170 (2017).
Mishra, R. K., Park, C., Zhou, H., Najafi, B. & Thrasher, T. A. Evaluation of motor and cognitive performance in people with Parkinson’s disease using instrumented trail-making test. Gerontology 68, 234–240 (2021).
Sakai, H. et al. Pen-point trajectory analysis during trail making test based on A time base generator model. In 2021 43rd Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). https://doi.org/10.1109/embc46164.2021.9629991 (2021).
Lambourne, K. & Tomporowski, P. The effect of exercise-induced arousal on cognitive task performance: A meta-regression analysis. Brain Res. 1341, 12–24 (2010).
Beauchet, O. et al. Recurrent falls and dual task-related decrease in walking speed: Is there a relationship?. J. Am. Geriatr. Soc. 56, 1265–1269 (2008).
Faulkner, K. A. et al. Multitasking: Association between poorer performance and a history of recurrent falls. J. Am. Geriatr. Soc. 55(4), 570–576 (2007).
Arbuthnott, K. & Frank, J. Trail making test, part B as a measure of executive control: Validation using a set-switching paradigm. J. Clin. Exp. Neuropsychol. 22, 518–528 (2000).
Crowe, S. F. The differential contribution of mental tracking, cognitive flexibility, visual search, and motor speed to performance on parts A and B of the trail making test. J. Clin. Psychol. 54, 585–591 (1998).
Kameniar, K., Mackintosh, S., Van Kessel, G. & Kumar, S. The psychometric properties of the short physical performance battery to assess physical performance in older adults: A systematic review. J. Geriatr. Phys. Therapy https://doi.org/10.1519/JPT.0000000000000337 (2022).
Michikawa, T., Nishiwaki, Y., Takebayashi, T. & Toyama, Y. One-leg standing test for elderly populations. J. Orthop. Sci. 14, 675–685 (2009).
Franchignoni, F., Tesio, L., Martino, M. T. & Ricupero, C. Reliability of four simple, quantitative tests of balance and mobility in healthy elderly females. Aging Clin. Exp. Res. 10, 26–31 (1998).
Giorgetti, M. M., Harris, B. A. & Jette, A. Reliability of clinical balance outcome measures in the elderly. Physiotherapy Res. Int. 3, 274–283 (1998).
Webb, K. L. et al. Test-retest reliability and minimal detectable change of four cognitive tests in community-dwelling older adults. J. Alzheimer’s Dis. 87, 1683–1693 (2022).
Donoghue, D. & Stokes, E. K. How much change is true change? The minimum detectable change of the Berg balance scale in elderly people. J. Rehabil. Med. 41, 343–346 (2008).
Hirai, H. et al. Studies in the falls efficacy scale-international for patients with cervical compressive myelopathy: Reliability, validity, and minimum clinically important difference. J. Spinal Cord Med. https://doi.org/10.1080/10790268.2023.2192849 (2023).
Acknowledgements
The authors kindly thank the Columbia University Community Engagement Core Resource (CECR: Grant Number UL1 TR001873) team for outreach and recruitment of participants. We also extend our gratitude to Xincheng Zhao, Songwei Zhao, and Fitsum E. Petros for their role in either data collection, manuscript editing or proofreading.
Funding
S.A. is supported by grants from NY State DOH contract # C37719GG, C38336GG, C35595GG which investigate the use of cable-driven robotic devices for functional assistance and training of patients with spinal cord injury.
Author information
Authors and Affiliations
Contributions
The study was designed by A.A., D.S., and S.A. Data collection and system hardware/software were handled by A.A., D.S., D.R., M.R., A.Y., G.K. Data analysis, cleaning, and initial manuscript draft were prepared by A.A., D.S., D.R., M.R., A.Y., G.K. Figures, tables and statistical analysis were created or performed by A.A., D.S., D.R.; D.S. and S.A. supervised the project. All authors contributed extensively to the work presented in this paper, commented on the manuscript throughout the editorial process, and approved the final submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Adeniyi, A., Stramel, D.M., Rahman, D. et al. Utilizing mobile robotics for pelvic perturbations to improve balance and cognitive performance in older adults: a randomized controlled trial. Sci Rep 13, 19381 (2023). https://doi.org/10.1038/s41598-023-46145-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46145-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.