Abstract
Ankle arthrodesis is commonly performed to treat end-stage ankle osteoarthritis. The aim of this study was to determine whether the use of fibular autograft might increase the fusion rate and decrease the complication rate in ankle arthrodesis (AA) fixed using cannulated screws. To perform this PRISMA-compliant proportional meta-analysis, multiple databases were searched for studies in which patients undergone AA (using exclusively cannulated screws and augmented with fibular bone graft) were followed. The characteristics of the cohort, the study design, surgical details, the nonunion and complication rate at the longest follow-up were extracted and recorded. The modified Coleman Methodology Score (mCMS) was applied to appraise the quality of studies. Two groups were built: arthrodeses fixed with screws combined with cancellous autograft (G1) and arthrodeses fixed with screws combined with cancellous autograft and augmented with a lateral fibular onlay (G2). A third group (arthrodeses fixed with screws and no graft, G3) was extracted from previous literature for a further comparison. Overall, we included 306 ankles (296 patients) from ten series (ten studies). In G1 and G2 there were 118 ankles (111 patients) and 188 ankles (185 patients), respectively. In patients where cancellous autograft was used, a further augmentation with a fibular lateral strut autograft did not change significantly the nonunion (4% [95% CI 1–9] in G1 vs. 2% [95% CI 0–5) in G2, p = 0.99) nor the complication rate (18% [95% CI 0–36] in G1 vs. 13% [95% CI 6–21) in G2, p = 0.71). Upon comparison with 667 ankles (659 patients, G3) in which arthrodeses had been performed without grafting, the nonunion and complication rates did not differ significantly either (pooled estimates: 3% [95% CI 1–3) in G1 + G2 vs. 3% [95% CI 2–4] in G3, p = 0.73 for nonunion; 15% [8–23] in G1 + G2 vs. 13% [95% CI 9–17] in G3, p = 0.93 for complications). In ankle arthrodesis fixed with cannulated screws combined with cancellous autograft at the fusion site, a construct augmentation with a distal fibular onlay strut graft positioned laterally at the ankle joint does not reduce the risk of nonunion or complication. In general, the use of bone graft does not influence significantly the nonunion nor the complication rate as compared to non-grafted screw-fixed ankle arthrodeses.Kindly check and confirm the corresponding author mail id is correctly identified.It's all correct
Similar content being viewed by others
Introduction
Severe ankle osteoarthritis resistant to non-surgical treatments represents a common indication for ankle arthrodesis (AA) or Ankle Arthroplasty1,2,3,4. Multiple studies have been undertaken over the last years comparing these two techniques, often concluding that both procedures could lead to a satisfactory outcome in this setting. There is good consensus about the fact that for ankles presenting after an infection, or with marked joint deformity or with bony defects AA represent the gold standard. From a technical point of view, AA can be performed using a number of fixation methods (such as cannulated screws, one or more plates, a nail or an external fixator) and following various strategies (arthroscopically-assisted procedures, use or not of bone or synthetic graft, one or two-stage procedures) depending on the specific case3, 5,6,7,8,9,10. Surgeons usually rely on their experience and on the patient’s conditions in order to choose a fixation method to achieve the fusion of the ankle joint, since no technique has been proven more effective than another11, 12.
Some recent literature has been produced focusing on AA performed using cannulated screws8, 13,14,15, overall suggesting that using different number of screws or combining various thread designs or positioning metalwork in different configurations does not clearly affect the success rate of the procedure. At times, surgeons may decide to place some cancellous bone at the fusion site or to use an onlay fibular strut autograft placed laterally as a bridge between the tibia and the talus, with the aim to add both a biological and mechanical augmentation to the fixation16. A systematic review (without a formal meta-analysis) performed by Heifner et al. has included studies dealing with open ankle arthrodeses fixated using screws published until October 2019. The authors have concluded that using bone graft did not have a significant effect on union rates16. However, to the best of our knowledge, a consensus about the value of fibular bone grafting both for open or arthroscopically-assisted procedures is still lacking.
In this setting, we performed a proportional meta-analysis to determine whether the use of a distal fibular autograft (as cancellous bone interposed at the fusion site or as lateral strut) in AA fixed using cannulated screws might influence the union and complication rate. We hypothesized that, in ankle arthrodesis fixed with cannulated screws combined with cancellous autograft at the fusion site, augmenting the fixation with a distal fibular onlay strut graft positioned laterally at the ankle joint might reduce the risk of nonunion or complication. A second hypothesis was that the use of bone graft at the fusion site might increase the union rate and reduce the number of complications as compared to non-grafted constructs.
Results
Study population
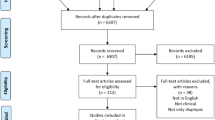
Overall, we included 306 ankles (296 patients) from ten series (ten studies) (Fig. 1)17,18,19,20,21,22,23,24,25,26.
In G1 and G2 there were 118 ankles (111 patients) and 188 ankles (185 patients), respectively (Table 1). Raw data of a third group (G3, 15 studies) composed of 667 ankles (659 patients, G3) in which arthrodeses had been performed without grafting, was extracted from the study by Izzo et al.13 (Fig. 1) (Table 1).
In the three groups, the sample size (p = 0.52), mean age of patients (p = 0.33), sex distribution (p = 0.67) and follow-up (p = 0.27) were comparable (Table 2). The mean mCMS (48.8 ± 9, range, 35–66) revealed only an overall moderate quality of studies, with a risk of bias which was comparable in the three groups (46.2 in G1, 45.6 in G2 and 50.8 in G3; p = 0.43).
Cancellous bone versus cancellous bone + fibular onlay graft
In patients where cancellous autograft was used, a further augmentation with a fibular lateral strut autograft did not change significantly the nonunion (4% [95% CI 1–9] in G1 vs. 2% [95% CI 0–5) in G2, p = 0.99) (Fig. 2) nor the complication rate (18% [95% CI 0–36] in G1 vs. 13% [95% CI 6–21) in G2, p = 0.71) (Fig. 3). For the nonunion rate, intra-group heterogeneity was significant in G1 (p = 0.01) but not in G2 (p = 0.29), while inter-group heterogeneity was nonsignificant (p = 0.548), supporting the pooling of data into one pooled measure (3%, [95% CI 1–5]) (Fig. 2). For the complication rate, intra-group heterogeneity was significant both in G1 and G2 (p < 0.001 and p = 0.01, respectively), but intergroup heterogeneity was nonsignificant (p = 0.629) with a pooled measure at 15% [95% CI 8–23] (Fig. 3).
In the manuscript we found that reference [8,17,25,28] is a duplicate of [16,18,31,33] and hence the repeated version has been deleted. Please check.Apologies for the mistake, thank you.
Autograft versus no autograft
Upon comparison between AA performed with autograft and without graft, the nonunion and complication rates did not differ significantly either (pooled estimates: 3% [95% CI 1–3) in G1 + G2 vs. 3% [95% CI 2–4] in G3, p = 0.73 for nonunions (Fig. 4); 15% [8–23] in G1 + G2 vs. 13% [95% CI 9–17] in G3, p = 0.93 for complications (Fig. 5)). For what concerns the nonunion rate, intragroup heterogeneity was nonsignificant in G1 + G2 (p = 0.05) and significant in G3 (p < 0.001). However, the intergroup heterogeneity was nonsignificant (p = 0.750) with a pooled estimate at 3% [95% CI 2–4) (Fig. 4). Regarding the complication rate, the intragroup heterogeneity was significant both in G1 + G2 and in G3 (p < 0.001 for both), while there was no significant intergroup heterogeneity (p = 0.648) with a pooled estimate at 14% [95% CI 10–17) (Fig. 5).
Meta-analysis of the proportion of nonunions in patients undergone Ankle Arthrodesis fixed with cannulated screws and augmented with a fibular autograft (including both only cancellous graft and cancellous graft augmented with a lateral fibular strut graft) versus Arthrodesis performed without autograft. Output generated by the Stata procedure metaprop.
Meta-analysis of the proportion of complications in patients undergone Ankle Arthrodesis fixed with cannulated screws and augmented with a fibular autograft (including both only cancellous graft and cancellous graft augmented with a lateral fibular strut graft) versus Arthrodesis performed without autograft. Output generated by the Stata procedure metaprop.
Discussion
The main finding of this study is that in ankle arthrodeses fixed using cannulated screws the use of fibular bone graft, whether as standalone cancellous bone interposed at the tibiotalar fusion site or as cancellous bone augmented with an onlay lateral distal fibular graft, does not significantly influence the union or the complication rate. In fact, the risk of nonunion did not differ between grafted constructs and only-screws fixation methods.
With regard to the fibular bone graft, our findings support the idea that it may be not necessary in the majority of AAs, which corroborates some previous literature. In a recent systematic review, Heifner et al. reported a similar fusion rate in AA both with and without bone graft and fibular onlay (94.7% and 95.3%, respectively), concluding that the graft was not needed routinary in AA and should be dedicated to patients at high-risk of failure16. Interestingly, in their analysis the authors used the CMS to assess the quality of studies included which scored at 60, being not far from our 48.8 and confirming the only moderate quality of literature produced in this field16. On the other side, it should be emphasized that, as compared to our study, Heifner et al. adopted slightly different inclusion criteria since they excluded studies reporting arthroscopic arthrodeses (which is nowadays commonly performed in association with screw fixation) and including studies with a follow-up shorter than 12 months (which limits the strength of their conclusion in terms of complication rate). In another study by Duan et al. the use of two cannulated screws in arthroscopic AA led to a fusion rate of 100% with no use of bone graft27. Regardless of the use of fibular graft, in our study the pooled fusion rate was at least 96% (with a pooled nonunion rate ranging from 2 to 4%), which could be retained as indicative value for arthrodeses fixed using cannulated screws. It should be noted, however, that we included both open and arthroscopic AAs in the same group.
From a technical standpoint, the use of a fibular onlay autograft inevitably requires an open procedure which should inherently carry a higher risk of complications as compared to arthroscopic arthrodeses28. Also, preparing the distal fibula before using it as a graft (which includes harvesting it, shaping and/or morselising it) may require additional surgical time in those settings where a limited number of scrubbed assistants are available during surgery. While the complication rate in the studies selected in our analysis varied quite largely, ranging from 0 to 30%18, 19, 21,22,23,24, 26, 29, 30, the pooled estimate for complications in arthrodeses where fibular graft was used was 15%, being slightly higher but not statistically different from the complication rate of only-screws constructs (13%). Considering the greater number of screws used to stabilise a lateral fibular strut, we would have expected a higher complication rate related to irritation from metalwork in this group, which was not the case. Also, it should be emphasized that unfortunately data coming from a number of high-quality studies, such as the longitudinal cohort study recently published by Abuhantash et al. in which 351 AAs were followed up at 5 years, could not be used in this meta-analysis due to the heterogeneity of fixation methods (i.e., cross-screws, retrograde nailing, or plate fixation) reported in their study28. Anyway, along with the findings related to nonunion, we believe that the numbers related to the risk of complication might be extremely valuable in the clinical setting to correctly inform the patient during the pre-surgical counselling for these procedures.Please confirm the section headings are correctly identified.They are correct
This study is not without limitations. First, the Level of Evidence provided in this meta-analysis is IV since most studies included are of Level III and IV studies, which weakens the strength of our conclusions. Second, no clinical data has been reported in our analysis. Although this would have undoubtedly been useful, in primary studies we did not find sufficient clinical raw data to run any meaningful statistical analysis on this. Third, the comparison with only-screw constructs was performed using historical data taken from another study by Izzo et al., which inherently increases the risk of bias for our findings. However, since data extracted from that study were almost identical to the current work, we reckon that the results of the comparison performed in this meta-analysis might be still reliable and meaningful for clinicians. Fourth, intragroup heterogeneity was significant for most of the groups analyzed in this study. Although this may not be strictly interpreted as lack of consistency between studies in the same group, it should be taken into account when analysing our findings. In our opinion this statistical heterogeneity likely corresponds to differences in study design and surgical technique of primary studies. Even if AA generally represents the gold standard to treat ankle osteoarthritis while fibula autograft is usually considered in severe bone loss or deformity, the procedure can be carried out in multiple ways according to various habits for surgeons around the world. On the other side, intergroup assessments always revealed a good consistency among studies, which represents a further strength of our study. Finally, we acknowledge that other factors that have a known influence on bone healing and postoperative complications in AA (such as diabetes, body mass index and smoking) have not been evaluated in this study.
In conclusion, this proportional meta-analysis suggests that in ankle arthrodesis fixed with cannulated screws combined with cancellous autograft at the fusion site, a construct augmentation with a distal fibular onlay strut graft positioned laterally at the ankle joint does not reduce the risk of nonunion or complication. In general, the use of bone graft does not influence significantly the nonunion nor the complication rate as compared to non-grafted screw-fixed ankle arthrodeses. The quality of evidence provided in literature so far is only moderate, therefore high-level comparative and prospective studies around the use of graft in ankle arthrodesis are warranted.
Methods
Protocol and registration
This systematic review was designed according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA). It was prospectively registered as a part of larger project on AA in the PROSPERO database (CRD42022322784).
Eligibility criteria
The inclusion criteria were as follows: studies reporting data after AA (open or arthroscopically-assisted) stabilized using only screws in patients aged between 15 and 85 years; clear description of the surgical technique with one or more statements about the number of screws used and a systematic use of two or more screws and 1) a distal fibula autograft used as cancellous bone interposed between the tibia and the talus or 2) a distal fibula autograft used as cancellous bone at the fusion site augmented with a structural lateral construct or) in the whole cohort; studies including a sample size larger than 10 ankles; assessment of radiographic results through pre- and post-operative weightbearing standardized radiographs; reporting the fusion rate and complications after AA; minimum follow-up of 12 months; clinical studies; published in any language; full text availability either online either after direct contact with the authors.
Exclusion criteria were: studies reporting results after AA stabilized using other methods (nail, external fixator, plate, hybrid constructs); studies in which screws were used as unique way of fixation but without clear definition about the use of bone graft; data on skeletally-immature patients; case reports, biomechanical studies, cadaveric studies, expert opinions, letters to the editor, studies on animals and instructional courses. Narrative or systematic reviews were also excluded from this study but references were double checked in order to identify potential eligible studies.
Information sources and search
A systematic search was conducted on Pubmed, Embase, Cochrane Library and Scopus, from the earliest entries through April 30, 2023 with the following key words and Boolean operators: ((ankle) AND (arthrodes*)) OR ((ankle) AND (fusion)). Additional studies were identified in the bibliographies of articles. Two reviewers (AI and MD) independently screened the results of the research, then the full text of eligible studies was analyzed. Disputes were resolved by the senior author (AB). Unpublished studies and gray literature were not considered.
Data charting and items
Data were charted independently by two investigators (AI and MD) using an Excel sheet. Data were harvested regarding the cohort, the study design, the surgical technique the nonunion and the complication rate at the longest follow-up. Two groups were built: arthrodeses fixed with screws combined with cancellous autograft (G1) and arthrodeses fixed with screws combined with cancellous autograft and augmented with a lateral fibular onlay (G2). A convenience sample of arthrodeses fixed with cannulated screws and no graft (G3) (with all the relevant raw data) was extracted from a previous study for a further comparison13.
Risk of bias
The modified Coleman Methodology Score (mCMS) was used to assess the quality of studies included, as in previous foot and ankle literature31, ranging from 0 to 100. Two investigators performed the mCMS assessment twice (AI and MD), with an interval of 10 days, then discussed the scores when more than a two-point difference was present, until consensus was reached. A score higher than 85 was considered excellent, good from 70 to 84, moderate from 50 to 69 and poor when less than 50.
Synthesis of results
Baseline data (reported as average value, standard deviation (SD) and range values in the three groups) were tested for normality using a Shapiro–Wilk test and were then compared using the ANOVA (for normally distributed variables) or the Kruskal–Wallis rank sum test (for nonnormally distributed variables). A proportional meta-analysis was run to pool data regarding the nonunion and the complication rate. The ‘metaprop’ command was used to compute 95% confidence intervals using the score statistic and the exact binomial method and incorporate the Freeman-Tukey double arcsine transformation of proportions. Heterogeneity among studies was assessed through the Higgins’ I2 statistic and a random-effect model was applied in all cases. A meta regression (metareg module) was used to compare pooled proportions as follows: (1) G1 versus G2; (2) pooled G1 + G2 versus G3. The significance level for the overall estimates of effect was set at p < 0.05. All analyses were performed using STATA statistical software package (Version 16.0, StataCorp, 2019).
Data availability
Some or all data, models, or code generated or used during the study are available from the corresponding author upon request.
References
Yang, T. C., Tzeng, Y. H., Wang, C. S., Chang, M. C. & Chiang, C. C. Arthroscopic ankle arthrodesis provides similarly satisfactory surgical outcomes in ankles with severe deformity compared with mild deformity in elderly patients. Arthroscopy 36, 2738–2747 (2020).
Quayle, J. et al. Arthroscopic versus open ankle arthrodesis. Foot Ankle Surg. 24, 137–142 (2018).
Mehdi, N., Bernasconi, A., Laborde, J. & Lintz, F. Comparison of 25 ankle arthrodeses and 25 replacements at 67 months’ follow-up. Orthop. Traumatol. Surg. Res. 105, 139–144 (2019).
Anigian, K. et al. Comparison of short-term outcomes after total ankle replacement and ankle arthrodesis: An ACS-NSQIP database study. Foot Ankle Spec. https://doi.org/10.1177/19386400211043363 (2021).
Ogut, T., Glisson, R. R., Chuckpaiwong, B., Le, I. L. D. & Easley, M. E. External ring fixation versus screw fixation for ankle arthrodesis: A biomechanical comparison. Foot Ankle Int. 30, 353–360 (2009).
Betz, M. M. et al. Primary stability and stiffness in ankle arthrodes-crossed screws versus anterior plating. Foot Ankle Surg. 19, 168–172 (2013).
Clifford, C., Berg, S., McCann, K. & Hutchinson, B. A biomechanical comparison of internal fixation techniques for ankle arthrodesis. J. Foot Ankle Surg. 54, 188–191 (2015).
van den Heuvel, S. B. M., Penning, D. & Schepers, T. Open ankle arthrodesis: A retrospective analysis comparing different fixation methods. J. Foot Ankle Surg. 61, 233–238 (2022).
van den Heuvel, S. B. M., Doorgakant, A., Birnie, M. F. N., Blundell, C. M. & Schepers, T. Open ankle arthrodesis: A systematic review of approaches and fixation methods. Foot Ankle Surg. 27, 339–347 (2021).
Mendicino, R., Catanzariti, A. R. & Reeves, C. L. Posterior calcaneal displacement osteotomy: A new percutaneous technique. J. Foot Ankle Surg. 43, 332–335 (2004).
Xie, Q. et al. Comparisons of ankle arthrodesis with different internal fixation methods in the treatment of post-traumatic osteoarthritis. J. Orthop. Sci. https://doi.org/10.1016/J.JOS.2023.02.009 (2023).
Wang, R., Wu, J., Akhtyamov, I., Ziatdinov, B. & Cai, J. A network meta-analysis of the efficacy of arthrodesis with various fixation methods in the treatment of advanced ankle osteoarthritis. Injury https://doi.org/10.1016/J.INJURY.2023.05.025 (2023).
Izzo, A. et al. Does the number of screws influence the union rate in ankle arthrodesis? A meta-analysis and systematic review. Foot Ankle Spec. https://doi.org/10.1177/19386400231171508 (2023).
Yokoo, S. et al. Larger sagittal inter-screw distance/tibial width ratio reduces delayed union or non-union after arthroscopic ankle arthrodesis. Eur. J. Orthop. Surg. Traumatol. https://doi.org/10.1007/S00590-022-03307-X (2022).
Valiyev, N. et al. The effects of different screw combinations on the initial stability of ankle arthrodesis. J. Am. Podiatr. Med. Assoc. 111, (2021).
Heifner, J. J., Monir, J. G. & Reb, C. W. Impact of bone graft on fusion rates in primary open ankle arthrodesis fixated with cannulated screws: A systematic review. J. Foot Ankle Surg. 60, 802–806 (2021).
Chen, Y. J., Huang, T. J., Shih, H. N., Hsu, K. Y. & Hsu, R. W. W. Ankle arthrodesis with cross screw fixation. Good results in 36/40 cases followed 3–7 years. Acta Orthop. Scand. 67, 473–478 (1996).
Monroe, M. T., Beals, T. C. & Manoli, A. Clinical outcome of arthrodesis of the ankle using rigid internal fixation with cancellous screws. Foot Ankle Int. 20, 227–231 (1999).
Kennedy, J. G., Hodgkins, C. W., Brodsky, A. & Bohne, W. H. Outcomes after standardized screw fixation technique of ankle arthrodesis. Clin. Orthop. Relat. Res. 447, 112–118 (2006).
Colman, A. B. & Pomeroy, G. C. Transfibular ankle arthrodesis with rigid internal fixation: An assessment of outcome. Foot Ankle Int. 28, 303–307 (2007).
Nielsen, K. K., Linde, F. & Jensen, N. C. The outcome of arthroscopic and open surgery ankle arthrodesis: A comparative retrospective study on 107 patients. Foot Ankle Surg. 14, 153–157 (2008).
Akra, G. A., Middleton, A., Adedapo, A. O., Port, A. & Finn, P. Outcome of ankle arthrodesis using a transfibular approach. J. Foot Ankle Surg. 49, 508–512 (2010).
Smith, J. T., Chiodo, C. P., Singh, S. K. & Wilson, M. G. Open ankle arthrodesis with a fibular-sparing technique. Foot Ankle Int. 34, 557–562 (2013).
Napiontek, M. & Jaszczak, T. Ankle arthrodesis from lateral transfibular approach: Analysis of treatment results of 23 feet treated by the modified Mann’s technique. Eur. J. Orthop. Surg. Traumatol. 25, 1195–1199 (2015).
Lee, D. Y. et al. A modified transfibular technique of ankle arthrodesis using partial fibular resection and onlay bone graft. PLoS One 15, e0241141 (2020).
Kim, J. B., Lee, B. J., Jung, D., Jeong, U. & An, C. Comparing outcomes of the ankle arthrodesis by using two different materials via a transfibular approach. Acta Ortop. Bras. 28, 55–59 (2020).
Duan, X., Yang, L. & Yin, L. Arthroscopic arthrodesis for ankle arthritis without bone graft. J. Orthop. Surg. Res. 11, 1–8 (2016).
Abuhantash, M. et al. Arthroscopic versus open ankle arthrodesis: A 5-year follow up. J. Bone Jt. Surg. Am. 104, 1197–1203 (2022).
Lee, H. J., Min, W. K., Kim, J. S., Yoon, S. D. & Kim, D. H. Transfibular ankle arthrodesis using burring, curettage, multiple drilling, and fixation with two retrograde screws through a single lateral incision. J. Orthop. Surg. (Hong Kong) 24, 101–105 (2016).
Suo, H. et al. End-stage ankle arthritis treated by ankle arthrodesis with screw fixation through the transfibular approach: A retrospective analysis. Orthop. Surg. 12, 1108–1119 (2020).
Bernasconi, A. et al. Tendoscopy of achilles, peroneal and tibialis posterior tendons: An evidence-based update. Foot Ankle Surg. 24, 374–382 (2018).
Author information
Authors and Affiliations
Contributions
A.B.: Study design, selection of studies, statistical analysis, interpretation of results, writing of the manuscript, revision of the manuscript. A.I.: Selection of studies, interpretation of results, writing of the manuscript, revision of the manuscript. M.D.: Study design, interpretation of results, writing of the manuscript, revision of the manuscript. M.M.: Study design, interpretation of results, writing of the manuscript, revision of the manuscript. A.C.: Study design, interpretation of results, writing of the manuscript, revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bernasconi, A., Izzo, A., D’Agostino, M. et al. Role of fibular autograft in ankle arthrodesis fixed using cannulated screws: a proportional meta-analysis and systematic review. Sci Rep 13, 18614 (2023). https://doi.org/10.1038/s41598-023-46034-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46034-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.