Abstract
No studies have evaluated the effect of fibular strut augmentation on the stability of locking plate fixation for osteoporotic proximal humeral fractures with lateral wall comminution. The purpose of this study was to evaluate the stability of locking plate fixation with a fibular strut graft compared with locking plate alone in an osteoporotic two-part surgical neck fracture model with lateral cortex comminution. Ten paired fresh-frozen cadaveric humeri were randomly allocated into two groups, either the locking plate alone (LP group) or locking plate with fibular strut graft augmentation (LPFSG group), with an equal number of right and left osteoporotic surgical neck fractures with lateral wall comminution of the greater tuberosity. Varus, internal/external torsion, and axial compression stiffness as well as single load to failure were measured in plate-bone constructs, and the LPFSG group showed significantly greater values in all metrics. In conclusion, this biomechanical study shows that fibular strut augmentation significantly enhances varus stiffness, internal torsion stiffness, external torsion stiffness, and maximum failure load of a construct compared to locking plate fixation alone in proximal humeral fractures with lateral wall comminution.
Similar content being viewed by others
Introduction
Proximal humeral fractures are one of the most common fractures in the elderly, and the incidence of proximal humeral fractures has increased with longer life expectancy1,2,3. Approximately 70% of all proximal humeral fractures occur in patients aged 60 and older4. Most cases can be treated conservatively; however, surgical treatment is favored over conservative treatment if the fracture is unstable and displaced5.
Stable fixation followed by adequate rehabilitation has shown satisfactory outcomes in proximal humeral fractures, and among the many fixation methods, locking plate techniques have shown good results in patients with compromised bone quality6,7. In addition, calcar screws and strut bone grafts have been associated with enhanced mechanical stability against varus collapse and satisfactory surgical outcomes in proximal humeral fractures with medial metaphyseal comminution or poor bone quality related to osteoporosis8,9.
Typically, solid fixation can be achieved through the use of plate and screw fixation of the near and far cortex10. However, in the proximal humerus fracture, fixation is dependent on the cancellous bone within the humeral head and the cortical bone of the lateral wall of the greater tuberosity, which are frequently involved in proximal humerus fracture. The involvement of the greater tuberosity (GT) is known to be common with its incidence up to 20% among all types of proximal humerus fractures11. Furthermore, the fixation plate is commonly placed lateral wall of the GT12,13. Considering that proximal humeral fractures occur in the elderly, stability of fixation may be significantly compromised by lack of lateral wall integrity of the greater tuberosity, especially in cases of low bone mass in the humeral head4. Although it is well known that fibular strut grafts have enhanced the results of locking plate fixation in unstable osteoporotic proximal humerus fractures with medial wall comminution8,14, no studies have evaluated the effect of fibular strut augmentation on the stability of locking plate fixation for osteoporotic proximal humeral fractures with lateral wall comminution.
In this study, we aim to evaluate the stability of locking plate fixation with a fibular strut graft compared with locking plate alone in an osteoporotic two-part surgical neck fracture model with lateral cortex comminution. We hypothesized that augmentation with a fibular strut graft will enhance the biomechanical stability of locking plate fixation in proximal humeral fractures with lateral wall comminution.
Methods
Specimen preparation
Ten pairs of fresh-frozen cadaveric humeri without any gross deformities or a history of injury or operation were used in this study. All specimens were stored frozen at − 20 °C and thawed at room temperature 24 h before use. All soft tissue of the humerus were thoroughly removed before use.
Quantitative computed tomography was used to measure bone mineral density (BMD) of each humeral head. BMD was evaluated at the greatest transverse diameter of the humeral head along three parallel sections separated by 1.5-mm distance15. The square region of interest (ROI) was positioned over the bone slice so that every edge of the square could reach the subcortical shell of the humeral head. The mean BMD of the three slices was used15. (Fig. 1).
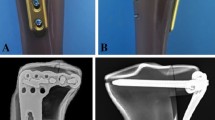
A two-part surgical neck fracture with a comminuted lateral wall of the greater tuberosity model was created by performing osteotomy at the following points using a microsagittal saw (Fig. 2): (1) a 5-mm wedge shaped gap one centimeter distal to the most inferior portion of the articular cartilage on the humeral head perpendicular to the humeral shaft16,17,18,19 and (2) a 5-mm-thick segment posterior to the bicipital groove corresponding to zones 2, 3, and 4 of the applied Proximal Humerus Internal Locking System (PHILOS) plate (Fig. 3), leaving two millimeters of the tip of the greater tuberosity intact to serve as a reference for locking plate application13,20,21.
(A) A PHILOS humerus plate with 9 proximal screw holes in Sections A-E for locking screws, 10 proximal suture holes to help maintain fracture reduction, and 3 distal screw holes. (B) Screws were categorized into several zones based on position20.
Block randomization was used to allocate the paired specimens (left and right side) into two groups: (1) locking plate alone (LP group) and (2) locking plate with fibular strut graft augmentation (LPFSG group). Each group was assigned an equal number of right and left humeri. All specimens were fixed with the same locking plate (PHILOS; Synthes, Paoli, Pennsylvania) using 12 screw holes (three distal and nine proximal) and the standard technique (Fig. 3). Plates were fixed on the lateral wall of the proximal humerus using six locking screws on the most proximal screw holes (Sections A, B, and C) and three screws on the shaft (Sections F, G, and H). Two additional screws were inserted on Section E (Fig. 3) for medial calcar support. Specimens in the locking plate with fibular strut graft augmentation group were fixed with an additional intramedullary fibular strut graft. An 80 mm segment from the ipsilateral fibular diaphysis of the cadaver was inserted into the medullary cavity of the diaphysis and humeral head. Then, 5 cm of the graft was impacted into the diaphysis and stabilized with three locking screws.
The humeral shaft was cut transversely at 16.5 cm from the upper margin of the wedge resection that is perpendicular to the anatomical axis of the humeral shaft and secured in a 7-cm-long tube with unsaturated polyester resin (EC‐304, Aekyung Chemical Co.)22,23. The humeral head was placed in unsaturated polyester resin up until 2 cm from the proximal wedge-shaped cut at the surgical neck and mounted to a customized jig.
Biomechanical testing
Measurement variables for biomechanical testing included axial compression, varus bending, torsional stiffness, and one single load to failure of varus bending, which commonly used in mechanical testing24. Biomechanical axial compression and varus bending and single load to failure tests were conducted using an electrohydraulic materials test system (model 3366; Instron, Norwood, Massachusetts), and rotational stiffness was measured using a torsional stiffness tester (DPTST; DYPHI).
First of all, quasi-static internal and external torsional tests were performed, with rotating the humeral head at 0.2Nm torque per second + 3.5 Nm and − 3.5 Nm for internal and external torsional stiffness, respectively (Fig. 4A). Secondly, axial compression test was performed with an axial force up to 200N at a rate of 0.1 mm per second (Fig. 4B). The four-point varus bending stiffness test was performed using an electrohydraulic materials test system setup (Fig. 4C), with a supporting span of 21 cm, and a loading span of 13 cm, with 3.5Nm at 0.1 mm per second. The stiffness was determined by calculating the slope of the linear region in the force/displacement graph at the fifth cycle (Fig. 5A–D). Finally, the single load to failure test was measured in the four-point varus test setup, until a sudden change occurred due to loss of fixation in the force/displacement curve25 (Fig. 5E).
(A) Test for rotational stiffness using a torsional stiffness tester (DPTST; DYPHI). (B) Test for axial compression using an electrohydraulic materials test system (model 3366; Instron, Norwood, Massachusetts). (C) Test for four-point bending using an electrohydraulic materials test system (model 3366; Instron, Norwood, Massachusetts).
Statistical analysis
Sample size calculation for comparison between two groups requires estimates of treatment effect26,27; however, because there were no previous studies in the literature, we performed a pilot study using three paired humeri (six specimens). Sample size was calculated using the varus stiffness values, and the mean ± standard deviation values for the LP group and LPFSG group were 338.69 ± 158.54 N/mm and 493.44 ± 171.91 N/mm, respectively. Accordingly, 10 specimens were required to achieve a power of 80% at an α level of 0.05.
Due to the small sample size, we used the non-parametric Wilcoxon signed-rank test to compare the differences in mechanical testing values between the paired samples. Statistical significance was set at p < 0.05, and statistical analyses were performed using IBM SPSS Statistics for Windows (version 25.0; IBM Corp.).
Ethics statement
This study was approved by the Institutional Review Board of Yonsei University Health System, Severance Hospital (4-2022-0989). All experiments were performed in accordance with relevant guidelines and regulations. The informed consent was obtained from the donors or their legal guardians.
Results
The mean BMD for the LP group was 32.10 mg/cm3 and 33.69 mg/cm3 for the LPFSG group. The two groups did not show a significant difference in BMD (p = 0.139). The mean varus stiffness, mean internal torsion stiffness, mean external torsion stiffness, mean axial compression stiffness, and single load to failure values were 265.32 N/mm, 2.34 N/deg, 1.72 N/deg, 320.92 N/mm, and 199.50 N in the LP group, respectively, and 417.65 N/mm, 0.72 N/deg, 0.68 N/deg, 384.55 N/mm, and 455.45 N in the LPFSG group. The LPFSG group showed significantly greater values in all biomechanical metrics excluding axial compression stiffness (Table 1).
Discussion
In the osteoporotic proximal humeral fracture with lateral wall comminution model of this study, we compared the stability of locking plate alone versus locking plate fixation with fibular strut graft augmentation. As we hypothesized, augmentation with a fibular strut graft significantly enhanced the biomechanical stability of locking plate fixation in proximal humeral fractures with lateral wall comminution in terms of varus stiffness, internal and external torsion stiffness compared with that of lateral wall comminution alone.
Due to comminution and a low bone mass within the humeral head in elderly patients, fixation failure is frequent despite the developments in fixation materials and techniques, including a locking plate and screw system. Particularly in surgical neck fractures with medial cortex comminution, the importance of medial calcar support screw fixation has been emphasized in many biomechanical and clinical studies28,29. On the contrary, although many proximal humerus fractures involve the lateral wall of the GT where the plate is applied, it has not been highlighted. Supposedly, this is because non-displaced lateral wall fractures of the GT with comminution are only identified on computed tomography (CT) and can be easily missed on plain x-ray.
Once the lateral wall is involved, application of the locking screw and plate system on the fractured lateral wall seems to be difficult to provide stable fixation, especially when the quality of humeral head bone is poor due to osteoporosis. Naturally, postoperative rehabilitation including ROM exercise is very limited due to concern about fixation failure and morbidities in elderly patients resulting from subsequent re-operation.
The endosteal fibular allogenous strut bone graft technique was introduced to improve fixation stability in cases of proximal humerus fracture with medial cortex comminution with low bone mass30. However, we thought that it would be helpful in cases of concomitant lateral wall fracture with osteoporosis; therefore, an unstable medial column model with osteoporosis was created with elderly cadaver specimens as in a previous study29, and unstable lateral column components were added. If loss of lateral wall integrity and low bone mass within the humeral head are present, the stability of the proximal fragment will not be sufficient, even with the medial calcar screw. Recently, Jang et al. published a study comparing locking plate with medial support screw and locking plate with intramedullary fibular graft fixation in varus collapsed proximal humerus fracture models31. Despite several studies reporting the advantages of the medial support screw, the fibular strut graft showed significantly better biomechanical stability than the medial support screw.
As we hypothesized, the use of fibular strut bone graft significantly improved fixation stability compared to the LP group in the osteoporotic proximal humerus fracture model with lateral wall comminution. Thus, the presence of lateral wall comminution of the greater tuberosity should be identified in preoperative planning, and strut bone augmentation should be considered for sold fixation in osteoporotic proximal humerus fractures.
To the best of our knowledge, this is the first biomechanical study comparing the stability of locking plate alone versus locking plate fixation with fibular strut graft augmentation in a proximal humeral fracture model with lateral wall comminution. However, our study has several limitations. First, as in most other cadaver studies, this was time-zero research. In studies using cadavers, additional bracing typically yields better fixation stability. However, it is well known that the strut bone blocking the medullary canal will become an obstacle in conversion to arthroplasty. Therefore, the use of strut bone augmentation should be carefully determined in preoperative planning and surgical field assessment on a case-by-case basis. Second, lateral wall comminution in an osteoporotic proximal humerus fracture model had no conventional reference. Although we tried our best to simulate the most similar model based on the clinical data experienced in our institute, we would not have the same specimens represented in the actual lateral wall comminution models. The degree of osteotomy was determined by referring to the existing surgical neck comminuted fracture model.
In conclusion, this biomechanical study shows that fibular strut augmentation significantly enhances the varus stiffness, internal torsion stiffness, external torsion stiffness, and maximum failure load of a construct compared to locking plate fixation alone in proximal humeral fracture models with lateral wall comminution.
Data availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
Change history
29 March 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41598-023-32259-3
References
Barrett, J. A. et al. Fracture risk in the U.S. Medicare population. J. Clin. Epidemiol. 52(3), 243–9 (1999).
Court-Brown, C. M. & Caesar, B. Epidemiology of adult fractures: A review. Injury 37(8), 691–697 (2006).
Palvanen, M. et al. Update in the epidemiology of proximal humeral fractures. Clin. Orthop. Relat. Res. 442, 87–92 (2006).
Court-Brown, C. M., Garg, A. & McQueen, M. M. The epidemiology of proximal humeral fractures. Acta Orthop. Scand. 72(4), 365–371 (2001).
Jo, M. J. & Gardner, M. J. Proximal humerus fractures. Curr. Rev. Musculoskelet. Med. 5(3), 192–198 (2012).
Lekic, N. et al. Treatment of two-part proximal humerus fractures: Intramedullary nail compared to locked plating. HSS J. 8(2), 86–91 (2012).
Südkamp, N. et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J. Bone Joint Surg. Am. 91(6), 1320–8 (2009).
Tuerxun, M. et al. Locking plate combined with endosteal fibular allograft augmentation for medial column comminuted proximal humeral fracture. Orthopedics 43(6), 367–372 (2020).
Zeng, L. Q. et al. Influence of medial support screws on the maintenance of fracture reduction after locked plating of proximal humerus fractures. Chin. Med. J. (Engl.) 131(15), 1827–1833 (2018).
Hak, D. J. et al. The influence of fracture fixation biomechanics on fracture healing. Orthopedics 33(10), 752–755 (2010).
Gruson, K. I., Ruchelsman, D. E. & Tejwani, N. C. Isolated tuberosity fractures of the proximal humeral: Current concepts. Injury 39(3), 284–298 (2008).
Castro-Franco, A. D. et al. Trends in the characterization of the proximal humerus in biomechanical studies: A review. Appl. Sci. 10(18), 6514 (2020).
Hasan, A. P. et al. Fracture line morphology of complex proximal humeral fractures. J. Shoulder Elbow Surg. 26(10), e300–e308 (2017).
Chun, Y.-M. & Lee, W. Operative treatment with intramedullary fibular strut allograft for osteoporotic proximal humerus fracture. Clin. Shoulder Elbow 20(2), 95–99 (2017).
Röderer, G. et al. Biomechanical in vitro assessment of fixed angle plating using a new concept of locking for the treatment of osteoporotic proximal humerus fractures. Int. Orthop. 35(4), 535–541 (2011).
Edwards, S. L. et al. Two-part surgical neck fractures of the proximal part of the humerus. A biomechanical evaluation of two fixation techniques. J. Bone Joint Surg. Am. 88(10), 2258–64 (2006).
Foruria, A. M. et al. Proximal humerus fracture rotational stability after fixation using a locking plate or a fixed-angle locked nail: The role of implant stiffness. Clin. Biomech. (Bristol, Avon) 25(4), 307–311 (2010).
Ponce, B. A. et al. The role of medial comminution and calcar restoration in varus collapse of proximal humeral fractures treated with locking plates. J. Bone Joint Surg. Am. 95(16), e113 (2013).
Williams, G. R. Jr. et al. The influence of intramedullary fixation on figure-of-eight wiring for surgical neck fractures of the proximal humerus: A biomechanical comparison. J. Shoulder Elbow Surg. 6(5), 423–428 (1997).
Jabran, A. et al. Biomechanical comparison of screw-based zoning of PHILOS and Fx proximal humerus plates. BMC Musculoskelet. Disord. 19(1), 253 (2018).
Majed, A. et al. Cortical thickness analysis of the proximal humerus. Shoulder Elbow 11(2), 87–93 (2019).
Burke, N. G. et al. Locking plate fixation with and without inferomedial screws for proximal humeral fractures: A Biomechanical study. J. Orthop. Surg. 22(2), 190–194 (2014).
Huff, L. R. et al. Proximal humeral fracture fixation: A biomechanical comparison of two constructs. J. Shoulder Elbow Surg. 22(1), 129–136 (2013).
Jabran, A., Peach, C. & Ren, L. Biomechanical analysis of plate systems for proximal humerus fractures: A systematic literature review. Biomed. Eng. Online 17(1), 47 (2018).
Hast, M. W. et al. Mechanical effects of bone substitute and far-cortical locking techniques in 2-part proximal humerus fracture reconstruction: A cadaveric study. J. Orthop. Trauma 34(4), 199–205 (2020).
Charan, J. & Biswas, T. How to calculate sample size for different study designs in medical research?. Indian J. Psychol. Med. 35(2), 121–126 (2013).
Olson, S. A. et al. Designing a biomechanics investigation: Choosing the right model. J. Orthop. Trauma 26(12), 672–677 (2012).
Laux, C. J. et al. Current concepts in locking plate fixation of proximal humerus fractures. J. Orthop. Surg. Res. 12(1), 137 (2017).
Mehta, S. et al. Calcar screw position in proximal humerus fracture fixation: Don’t miss high!. Injury 49(3), 624–629 (2018).
Cheng, H. et al. Treatment of 2-part proximal humeral fractures in osteoporotic patients with medial calcar instability using a PHILOS plate plus an allogeneic fibula inserted obliquely—A retrospective study. Geriatr. Orthop. Surg. Rehabil. 12, 21514593211050156 (2021).
Jang, Y. & Kim, D. Biomechanical study of Proximal humeral fracture fixation: Locking plate with medial support screw vs. locking plate with intramedullary fibular graft. Clin. Biomech. (Bristol, Avon) 90, 105510 (2021).
Acknowledgements
We thank JH Kim, JH Bang, and T-J Ha from the Surgical Anatomy Education Center at the Yonsei University College of Medicine, Seoul, for technical support.
Author information
Authors and Affiliations
Contributions
H.-H.C. contributed in carrying out the experiment including data collection and analysis, writing, reviewing and editing of the manuscript. J.-R.L., T.-H.Y. helped with the data collection and analysis. K.-H.L. and An HMS contributed in reviewing the manuscript. Y.-M.C. conceptualized and guided the experiments, including reviewing and editing of the manuscript. All authors have reviewed and approved the final submitted manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article omitted an affiliation for all authors. Additionally, the Acknowledgments section was omitted. Full information regarding the correction made can be found in the correction for this Article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chang, HH., Lim, JR., Lee, KH. et al. The biomechanical effect of fibular strut grafts on humeral surgical neck fractures with lateral wall comminution. Sci Rep 13, 3744 (2023). https://doi.org/10.1038/s41598-023-30935-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-30935-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.