Abstract
The aims of this study were to determine the prevalence and predictors of nocturnal polyuria (NP) in Japanese patients. This multicentral, observational study enrolled patients with the chief complaint of nocturia at 17 Japanese institutions between January 2018 and December 2022. The frequency of daily voiding and volume of urination were evaluated using bladder diaries. NP was diagnosed in patients with an NP index of > 33%. The primary endpoint was NP prevalence in patients with nocturia. The secondary endpoints were the prevalence of NP according to sex and age and the identification of factors predicting NP. This study analyzed 875 eligible patients. NP was present in 590 (67.4%) patients, with prevalence rates of 66.6% and 70.0% in men and women, respectively. Age ≥ 78 years, body mass index (BMI) < 23.0 kg/m2, and patients with ischemic heart or cerebrovascular disease were significant predictors of NP (P < 0.001, P < 0.001, P = 0.014, P = 0.016, respectively). This is the first large multicenter study to investigate the prevalence of NP in Japanese patients with nocturia. NP has a prevalence of 67.4%. Significant predictors of NP include age, BMI, and cardiovascular disease.
Similar content being viewed by others
Introduction
Nocturia is defined as the number of times during the main sleep period that the patient must be awake for the desire to urinate1. In addition, the patient must be asleep or willing to go to sleep each time the patient urinates after the first time of awakening to urinate1. It is one of the most common lower urinary tract symptoms (LUTS), and its prevalence does not vary by sex but increases with age2, 3. Nocturia has been reported to be a risk factor for sexual dysfunction, depression, and metabolic syndrome4,5,6. In addition, frequent nocturia causing multiple awakenings has been reported to cause sleep deprivation and poor sleep quality, resulting in a significant reduction in the patients’ quality of life (QoL) and interference with daily life7. In older adult patients, nocturia has been shown to be a risk factor for falls and fractures, leading to decreased patient QoL and worse prognoses8.
In Japan, the population of people aged over 65 years accounted for 28.4% of the total population in 2019. By 2030, the number of Japanese people aged over 75 years is expected to reach 22 million, a phenomenon that no other country in the world has ever experienced9. Therefore, nocturia appears to be a critical problem for Japan, as it is facing a super-aging society.
Nocturia can be classified according to its four main causes: (1) 24-h polyuria (excessive urination during the daytime and nighttime); (2) bladder storage disorders, such as overactive bladder (OAB) or benign prostatic hyperplasia (BPH); (3) nocturnal polyuria (NP); (4) various related factors, including OAB and NP10.
NP is considered one of the main causes of nocturia and is associated with the decreased secretion of the antidiuretic hormone, arginine vasopressin (AVP)11, 12. The treatment for NP has dramatically changed with randomized controlled trials that have shown that desmopressin acetate, a synthetic AVP analog, is an effective and well-tolerated treatment for NP regardless of sex11, 13, 14. Accordingly, an accurate diagnosis of the etiology of NP is important for appropriate treatment, necessitating the investigation of the prevalence of NP in patients with nocturia.
Using bladder diaries, the prevalence of NP has been reported to range from 76 to 88% in Europe, the United States, and Canada11; however, few studies have clarified the prevalence of NP in Japanese patients with nocturia4, 8. Therefore, we conducted a multicenter retrospective study to investigate the prevalence of NP in patients with nocturia and investigated the predictive factors of NP.
Materials and methods
Patients
Medical Research Ethics Committee of Gifu University, University of Yamanashi, and Fukushima Medical University approved this study (approval number: 2021-053, 2481, and 2021-154, respectively). Informed consent was not required because of the retrospective nature of the study. Moreover, in accordance with the Japanese Ethics Committee and its ethical guidelines, written informed consent was not obtained because retrospective and observational studies using existing materials and other data have already been published. Instead, we used an opt-out approach and provided patients with the opportunity to decline participation. More information on this study, which is available only in Japanese, can be found at https://www.med.gifu-u.ac.jp/visitors/disclosure/docs/2021-053.pdf (accessed May 31, 2021). All methods were carried out in accordance with relevant guidelines and regulations and in accordance with the World Medical Association Declaration of Helsinki.
In this multicenter, retrospective, observational study, patients with the chief complaint of nocturia, who visited 17 institutions in Japan between January 2018 and December 2022, were enrolled. Patients with bladder stone disease, urinary tract infections, urogenital malignancies, or those using desmopressin were excluded from the study. The following clinical data were collected in this study: age, sex, body mass index (BMI), Eastern Cooperative Oncology Group performance status (ECOG-PS)15, post-void residual, estimated glomerular filtration rate (eGFR), medical history, and concomitant medications. Prostate volume and prostate-specific antigen levels were measured in male patients. Urinary frequency and voided volume were evaluated using a bladder diary, and patients were requested to maintain the bladder diary for at least 2 days2. The time and volume of each voiding session, bedtime (intention to sleep), and awakening time were recorded in a diary. After the patients returned their diaries, the mean value of the data was calculated. Clinical variables, such as the number of voiding episodes during the daytime, nighttime, and 24-h periods, as well as the volume of urine during the daytime and nighttime, were obtained from the bladder diaries. Data from the first urination after awakening was recorded as daytime urinary frequency and nighttime urine volume.
Definition of NP
The NP index (NPi) was used to evaluate NP. NPi was calculated by dividing the nocturnal urine volume by the 24-h urine volume. Patients with an NPi > 33% were diagnosed with NP2.
Statistical analysis
The primary endpoint was the prevalence of NP in patients with nocturia. The secondary endpoints were the prevalence of NP according to sex and age. In addition, logistic regression analysis was used to evaluate the predictors of NP. Data analysis was performed using JMP 14 software (SAS Institute Inc., Cary, NC, USA). The cutoff values for clinical parameters were determined using receiver operating characteristic curve analysis16. Statistical significance was defined as a two-sided P-value of < 0.05.
Results
Patient characteristics
A total of 909 patients with nocturia were enrolled. After applying the exclusion criteria, 875 patients were eligible for analysis. The patient characteristics are listed in Table 1. Thirty-four patients (3.9%) had an ECOG-PS ≥ 2. The most common medical history was hypertension, with 47.3% of the patients receiving antihypertensive medication.
Bladder diary
The median number of daytime and nighttime urinations was 7.6 (interquartile range [IQR]: 6–9) and 3.0 (IQR: 2–4), respectively. Median 24-h, daytime, and nighttime voided volume were 1650 mL (IQR: 1270–2150), 980 mL (IQR: 700–1323), and 630 mL (IQR: 430–860), respectively. The median NPi was 38.0% (IQR: 29.0–49.0).
The prevalence of NP in patients with nocturia
Approximately 70% of the enrolled patients had NP (Fig. 1), and a similar trend was observed when the data was examined according to sex (Fig. 2). When examined by age, the prevalence of NP tended to increase with advancing age (Fig. 3).
The prevalence of nocturnal polyuria (NP) according to age in patients with nocturia. When patients were divided according to age, the prevalence of NP in patients < 50 years, 50–59 years, 60–69 years, 70–79 years, and 80 ≤ years were 38.1%, 55.3%, 56.7%, 66.5%, and 79.3%, respectively. When examined by age, the prevalence of NP tended to increase with advancing age.
Predictive factors of NP
The associations between NP and its clinical covariates are presented in Table 2. In the univariate analysis, age, BMI, eGFR, and the presence of hypertension, diabetes, ischemic heart disease, insomnia, and cerebrovascular disease were significant predictors of NP. Conversely, age, BMI, and the presence of ischemic heart and cerebrovascular diseases were significant predictors of NP in the multivariate analysis. Additionally, we evaluated the relationship between BMI and NP in Fig. 4. The prevalence of NP decreased significantly with increasing BMI (Fig. 4).
Discussion
Several studies have evaluated the prevalence of NP in patients with nocturia11, 13, 14, 17,18,19. Weiss et al.11 investigated the prevalence of NP using data from two double-blind, randomized, placebo-controlled phase III trials13, 14, 17. The NOCTUPUS trial, which investigated the safety and efficacy of desmopressin for nocturia was conducted primarily in Europe, while another trial that evaluated the effect of desmopressin on nocturia was conducted in North America. In the NOCTUPUS study, the overall prevalence of NP in patients with evaluable frequency-volume chart (FVC) records was 76%, of which 79% of men and 72% of women had NP13, 14. In the North American phase III study, the overall prevalence of NP based on FVC was 88%, of which 90% of men and 85% of women had NP17. A previous study that analyzed 200 consecutive records of patients complaining of nocturia found that the etiology of nocturia was BPH in 23% of men, urinary incontinence in 4%, stress urinary incontinence in 13%, and detrusor instability in 27%18. Overall, only 7% of the cases were due to NP alone, 57% were due to OAB, and 36% were due to both NP and OAB18. In contrast, in a study conducted by Chang et al. that investigated the causes of nocturia in 41 male patients, NP was found in 82.9% of the patients and was a significant factor influencing nocturia19. In the present study, NP was found in 67.4% of all cases, with a prevalence of 66.6% in male patients and 70.0% in female patients, although the prevalence of NP tended to be slightly lower than that reported in previous studies12, 18, 19, NP was found in more than two-thirds of cases regardless of sex, suggesting that NP is one of the most common causes of nocturia in Japanese patients. Despite the essential need for an accurate diagnosis that is dependent on etiology to treat nocturia, the condition is still considered as a storage symptom associated with OAB or BPH and thus has not been adequately treated19. Therefore, it is important to use bladder diaries as simple and effective tools to identify patients with NP as the primary cause of nocturia.
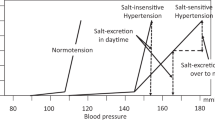
In this current study, the prevalence of NP increased with advancing age; a significant predictor of NP was age ≥ 78 years. Various reasons have been postulated for the increase in nocturnal urine volume with age13, 20,21,22. Robertson et al.20 reported that the proportion of nocturnal urine volume increased to 34% ± 15% in older individuals compared to approximately 14% ± 4% of the total daily urine volume in those aged 21–35 years. The increase in nocturnal urine volume with age may be due to age-related physiological changes in renal function and circadian rhythm changes in water and electrolyte regulatory hormones21. Indeed, decreased renal concentrating capacity and sodium conservation have been observed in the older adult population21. Asplund et al.13 found that nocturnal serum antidiuretic hormone concentrations were higher in younger adult subjects and lower in older adult subjects13. Therefore, changes in water/electrolyte-regulating hormones are thought to contribute to increased nocturnal urine volume13. Atrial natriuretic peptide (ANP) is also thought to contribute to increased nocturnal urinary output22, 23. Although some reports have found no difference in ANP levels between patients with and without NP22, 23, it has been shown that nocturnal ANP levels are increased in patients with NP and that urinary ANP levels are higher in older adult patients with nocturia and NP22, 23. These results suggest that physiological changes in the kidneys and related hormonal changes may be associated with the increased prevalence of NP with age.
Interestingly, a BMI < 23.0 kg/m2 was a significant predictive factor for NP in this study. Although few studies have examined the association between NP and BMI, several have examined the association between LUTS, nocturia and BMI24,25,26. While some reports have indicated that a high BMI is a risk factor for LUTS and nocturia24, 25, both high and low BMI (< 18.5 kg/m2) in women are associated with nocturia26. In recent years, frailty has received increased attention in the older adult population because of its associated increased risk of falls, disability, hospitalization, and death27. The phenotypic definition of frailty comprises five physical characteristics including unintentional weight loss27. In fact, a significant correlation between nocturia (four or more episodes), frailty, and polypharmacy has been reported (P < 0.05)28. Because nocturia is fairly common and is associated with insomnia, frailty, polypharmacy, incontinence, falls, slow walking, and functionality in older adult women, it has been suggested that nocturia is crucial to geriatric practice and that two or more episodes of nocturia could be an indicator of poor health in older adult women28. In this study, we examined the relationship between BMI and NP because BMI < 23.0 kg/m2 was a significant predictor of NP according to multivariate analysis. Based on the results, we found that the prevalence of NP decreased with increasing BMI. Although the clear reasons for these results remain uncertain, the relationship, including that with frailty, will need to be reconsidered in future prospective studies.
In this study, ischemic heart and cerebrovascular diseases was an independent predictor of NP. In a previous report, nocturia was independently associated with cardiovascular disease after adjusting for other known confounders29. Although nocturia was also associated with a lower odds ratio for the presence of heart failure, a history of coronary artery disease was not associated with nocturia29. The association between nocturia and cardiovascular morbidities raises several interesting questions. Nocturia adversely affects the cardiovascular system by disrupting sleep and causing sleep deprivation29. It has been suggested that poor or inadequate sleep may lead to adverse cardiovascular morbidity; however, according to this previous report, nocturia was not associated with cardiovascular disease, including time awake after sleep onset29. The report concluded that the relationship between natriuretic peptides, nocturia, and cardiovascular outcomes is complex and requires further study, although nocturia decreases the circulating blood volume and may reduce cardiac preload in patients29. NPs also have multifactorial etiologies as well as urologic diseases. Namely, untreated diabetes, insomnia, cardiovascular disease, chronic kidney disease (CKD), and primary polydipsia have been identified30, 31. The present study also investigated various factors such as diabetes, hypertension, insomnia, and CKD; however, these factors were not detected as significant risk factors for NP. However, diabetes and hypertension are known risk factors for ischemic heart disease and cerebrovascular disease32,33,34. In addition, obstructive sleep apnea is known to be a risk factor for cerebrovascular disease35. The results of this study suggested that ischemic heart disease and cerebrovascular disease might be associated with a higher risk of developing vascular disease compared to diabetes and hypertension, and might also contribute to the occurrence of NP.
Several limitations remain to be addressed in this study. First, this was a retrospective, multicenter study; thus, the potential for inherent bias could not be eliminated. Second, nocturia and NP were examined using bladder diaries recorded by patients, suggesting that the criteria for these assessments may not be consistent. Additionally, some patients may not have accurately recorded urine volume and the frequency of voiding in their bladder diaries. Third, there was a need to examine the validity of the cutoff value of NPi for the diagnosis of NP, which was adopted in this study. The definition of NPi as > 33% was commonly used for patients over 65 years of age, while a definition of 20% was accepted for younger patients2, 36. However, a clear definition of NP based on specific age categories has not yet been established. In this study, we adopted NPi > 33% as the definition of NP because the majority of the enrolled patients were ≥ 65 years of age, suggesting that a clear definition of NP based on age categories may be necessary in the future. Fourth, the high proportion of male patients in this study may require cautious interpretation of the results obtained in this study even though nocturia is generally considered to occur regardless of gender2, 3. Fifth, the health status of the enrolled patients was not objectively assessed using a screening tool for older adults; therefore, the true impact of aging is unclear. Finally, we were unable to investigate the etiology of NP because we did not perform hematological tests for nocturia or NP.
Conclusions
To the best of our knowledge, this is the first large, multicenter study to investigate the prevalence of NP in Japanese patients with nocturia. The prevalence of NP in Japanese patients with nocturia is 67.4%. Independent predictors of NP include age ≥ 78 years, BMI < 23.0 kg/m2, and the presence of ischemic heart disease and cerebrovascular disease. Whether these factors truly influence NP would need to be examined in future prospective studies with a large number of patients.
Data availability
The data that support the findings of this study are available in this manuscript.
References
Hashim, H. et al. International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol. Urodyn. 38, 499–508. https://doi.org/10.1002/nau.23917 (2019).
van Kerrebroeck, P. et al. The standardisation of terminology in nocturia: Report from the Standardisation Sub-committee of the International Continence Society. Neurourol. Urodyn. 21, 179–183. https://doi.org/10.1002/nau.10053 (2002).
Bing, M. H. et al. Prevalence and bother of nocturia, and causes of sleep interruption in a Danish population of men and women aged 60–80 years. BJU Int. 98, 599–604. https://doi.org/10.1111/j.1464-410X.2006.06390.x (2006).
Obayashi, K., Saeki, K., Negoro, H. & Kurumatani, N. Nocturia increases the incidence of depressive symptoms: A longitudinal study of the HEIJO-KYO cohort. BJU Int. 120, 280–285. https://doi.org/10.1111/bju.13791 (2017).
Brookes, S. T., Link, C. L., Donovan, J. L. & McKinlay, J. B. Relationship between lower urinary tract symptoms and erectile dysfunction: Results from the Boston Area Community Health Survey. J. Urol. 179, 250–255. https://doi.org/10.1016/j.juro.2007.08.167 (2008).
Kupelian, V. et al. Association of lower urinary tract symptoms and the metabolic syndrome: Results from the Boston Area Community Health Survey. J. Urol. 182, 616–624. https://doi.org/10.1016/j.juro.2009.04.025 (2009).
Andersson, F. et al. Assessing the impact of nocturia on health-related quality-of-life and utility: Results of an observational survey in adults. J. Med. Econ. 19, 1200–1206. https://doi.org/10.1080/13696998.2016.1211136 (2016).
Nakagawa, H. et al. Impact of nocturia on bone fracture and mortality in older individuals: A Japanese longitudinal cohort study. J. Urol. 184, 1413–1418. https://doi.org/10.1016/j.juro.2010.05.093 (2010).
Iijima, K. et al. Toward the development of a vibrant, super-aged society: The future of medicine and society in Japan. Geriatr. Gerontol. Int. 21, 601–613. https://doi.org/10.1111/ggi.14201 (2021).
Weiss, J. P., Weinberg, A. C. & Blaivas, J. G. New aspects of the classification of nocturia. Curr. Urol. Rep. 9, 362–367. https://doi.org/10.1007/s11934-008-0063-7 (2008).
Weiss, J. P., van Kerrebroeck, P. E., Klein, B. M. & Nørgaard, J. P. Excessive nocturnal urine production is a major contributing factor to the etiology of nocturia. J. Urol. 186, 1358–1363. https://doi.org/10.1016/j.juro.2011.05.083 (2011).
Asplund, R. & Aberg, H. Diurnal variation in the levels of antidiuretic hormone in the elderly. J. Intern. Med. 229, 131–134. https://doi.org/10.1111/j.1365-2796.1991.tb00320.x (1991).
Mattiasson, A., Abrams, P., Van Kerrebroeck, P., Walter, S. & Weiss, J. Efficacy of desmopressin in the treatment of nocturia: A double-blind placebo-controlled study in men. BJU Int. 89, 855–862. https://doi.org/10.1046/j.1464-410x.2002.02791.x (2002).
Lose, G., Lalos, O., Freeman, R. M., van Kerrebroeck, P., Nocturia Study Group. Efficacy of desmopressin (Minirin) in the treatment of nocturia: A double-blind placebo-controlled study in women. Am. J. Obstet. Gynecol. 189, 1106–1113. https://doi.org/10.1067/s0002-9378(03)00593-3 (2003).
Oken, M. M. et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 5, 649–655 (1982).
Perkins, N. J. & Schisterman, E. F. The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am. J. Epidemiol. 163, 670–675. https://doi.org/10.1093/aje/kwj063 (2006).
Weiss, J. P., Zinner, N. R., Klein, B. M. & Nørgaard, J. P. Desmopressin orally disintegrating tablet effectively reduces nocturia: Results of a randomized, double-blind, placebo-controlled trial. Neurourol. Urodyn. 31, 441–447. https://doi.org/10.1002/nau.2224 (2012).
Weiss, J. P., Blaivas, J. G., Stember, D. S. & Brooks, M. M. Nocturia in adults: Etiology and classification. Neurourol. Urodyn. 17, 467–472. https://doi.org/10.1002/(sici)1520-6777(1998)17:5%3c467::aid-nau2%3e3.0.co;2-b (1998).
Chang, S. C., Lin, A. T., Chen, K. K. & Chang, L. S. Multifactorial nature of male nocturia. Urology 67, 541–544. https://doi.org/10.1016/j.urology.2005.09.037 (2006).
Robertson, G. Nocturnal polyuria. BJU Int. 84, 17–19. https://doi.org/10.1046/j.1464-410x.1999.00066.x (1999).
Miller, M. Nocturnal polyuria in older people: Pathophysiology and clinical implications. J. Am. Geriatr. Soc. 48, 1321–1329. https://doi.org/10.1111/j.1532-5415.2000.tb02608.x (2000).
Carter, P. G., Cannon, A., McConnell, A. A. & Abrams, P. Role of atrial natriuretic peptide in nocturnal polyuria in elderly males. Eur. Urol. 36, 213–220. https://doi.org/10.1159/000068000 (1999).
Khosla, L. et al. Impact of aging on urinary natriuretic peptides in nocturia and nocturnal polyuria. Int. Neurourol. J. 26, 135–143. https://doi.org/10.5213/inj.2142330.165 (2022).
Wang, Y. et al. Prevalence, risk factors, and symptom bother of nocturia: A population-based survey in China. World J. Urol. 33, 677–683. https://doi.org/10.1007/s00345-014-1411-5 (2015).
Madhu, C. et al. Nocturia: Risk factors and associated comorbidities; Findings from the EpiLUTS study. Int. J. Clin. Pract. https://doi.org/10.1111/ijcp.12727.1508-16 (2015).
Ito, H. et al. Low and high body mass index values are associated with female nocturia. Neurourol. Urodyn. 38, 2250–2254. https://doi.org/10.1002/nau.24126 (2019).
Fried, L. P. et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 56, 146–156. https://doi.org/10.1093/gerona/56.3.m146 (2001).
Dutoglu, E. et al. Nocturia and its clinical implications in older women. Arch. Gerontol. Geriatr. https://doi.org/10.1016/j.archger.2019.103917 (2019).
Parthasarathy, S. et al. Nocturia, sleep-disordered breathing, and cardiovascular morbidity in a community-based cohort. PLoS One https://doi.org/10.1371/journal.pone.0030969 (2012).
Ohishi, M. et al. Hypertension, cardiovascular disease, and nocturia: A systematic review of the pathophysiological mechanisms. Hypertens. Res. https://doi.org/10.1038/s41440-021-00634-0 (2021).
Athanasopoulos, A. Nocturia due to nocturnal polyuria (NP). A common disorder. Arch. Ital. Urol. Androl. https://doi.org/10.4081/aiua.2022.3.366 (2022).
Sarwar, N. et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet https://doi.org/10.1016/S0140-6736(10)60484-9 (2010).
Yusuf, S. et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet https://doi.org/10.1016/S0140-6736(19)32008-2 (2020).
Fujiyoshi, A. et al. Blood pressure categories and long-term risk of cardiovascular disease according to age group in Japanese men and women. Hypertens. Res. https://doi.org/10.1038/hr.2012.87 (2012).
Loke, Y. K. et al. Association of obstructive sleep apnea with risk of serious cardiovascular events: A systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes https://doi.org/10.1161/CIRCOUTCOMES.111.964783 (2012).
Everaert, K. et al. International Continence Society consensus on the diagnosis and treatment of nocturia. Neurourol. Urodyn. https://doi.org/10.1002/nau.23939 (2019).
Author information
Authors and Affiliations
Contributions
Study concept and design: K.I., Y.N., Y.K., T.M., and T.K.; acquisition and curation of data: K.I., Y.N., K.M., T.I., S.M., R.T., Y.H., K.I., M.T., S.Y., H.H., K.Y., T.Y., Y.K., K.M., M.K.; statistical analysis: K.I.; drafting of the manuscript: K.I. and T.K. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Iinuma, K., Nishino, Y., Matsuoka, K. et al. The prevalence and predictive factors of nocturnal polyuria in Japanese patients with nocturia: a multicentral retrospective cohort study. Sci Rep 13, 18128 (2023). https://doi.org/10.1038/s41598-023-45311-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45311-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.