Abstract
Mycobacterium tuberculosis complex has an impact on public health and is responsible for over one million deaths per year. Substantial numbers of people infected with M. tuberculosis can develop tuberculosis lymphadenitis; however, there is a limited study in Adama, Ethiopia. The aim of this study was to determine the magnitude of Tuberculosis lymphadenitis, its predictors, and rifampicin-resistance gene-positive M. tuberculosis. A total of 291 patients with enlarged lymph nodes were recruited from May 2022 to August 30 at Adama Comprehensive Specialized Hospital Medical College (ACSHMC). GeneXpert, Ziehl–Neelsen staining, and cytology were used for the diagnosis of TB lymphadenitis from the Fine Needle Aspirate (FNA) specimen. Rifampicin-resistant gene was detected using GeneXpert. For data entry and analysis, Epi Data version 3.0 and SPSS version 25 were used respectively. A binary logistic regression model was used to identify predictors of TB lymphadenitis. A p < 0.05 with a 95% confidence interval (CI) was taken as a cut point to determine the significant association between dependent and independent variables. The prevalence of TB lymphadenitis using GeneXpert, Ziehl–Neelsen staining, and cytology were 138 (47.4%) (95% CI 41.70–53.10), 100 (34.4%) (95% CI 28.94–39.85), and 123 (42.3%) (95% CI 36.63–47.00) respectively. Nine (3.1%) participants were infected with rifampicin-resistant gene-positive M. tuberculosis. Out of the total M. tuberculosis detected by GeneXpert (n = 138), 9 (6.5%) were positive for rifampicin resistance-gene. Participants with a chronic cough had 2 times odds of developing TB lymphadenitis (AOR: 2.001, 95% CI 1.142–3.508). Close to half of patients with enlarged lymph nodes were positive for M. tuberculosis by the GeneXpert method in the study area. Chronic cough was significantly associated with TB lymphadenitis. Rifampicin-resistant gene-positive M. tuberculosis was relatively prevalent among patients with enlarged lymph node in the study area.
Similar content being viewed by others
Introduction
Tuberculosis is one of the leading causes of death, killing 2 million people each year1. TB lymphadenitis is the most common type of extrapulmonary tuberculosis that occurs outside of the lungs2. According to Stop TB Partnership, Ethiopia is among 30 countries suffering from high tuberculosis burden. In Ethiopia, about one-third of cases of tuberculosis are attributed to TB lymphadenitis3.
Lymphadenitis refers to lymph nodes that are abnormal in size, number, or consistency and can have etiologic agents ranging from infectious processes to malignant disease. The cause of lymphadenitis is difficult to diagnose based on history and physical examination alone. Fine needle aspiration cytology (FNAC) is a widely accepted, cost-effective, and safe method for the diagnosis of TB lymphadenitis and other lymph node abnormalities4.
TB lymphadenitis is a chronic specific granulomatous inflammation of the lymph node with caseous necrosis caused by infection with Mycobacterium tuberculosis or related bacteria. T cell lymphocytes and fibroblasts granulomatous tuberculosis eventually lead to the development of central caseous necrosis and a tendency to merge with the replacement of lymphoid tissue5. TB lymphadenitis (cervical) can be caused by the spread of M. tuberculosis from a lung infection6.
Currently, lymphadenitis is a common pathological problem in the world. Many studies have been conducted to determine the magnitude and etiology of lymphadenitis. The pattern of the disease varies across different ethnic backgrounds and countries. Information regarding the magnitude and etiology of lymphadenitis in a specific geographic area is essential for a better diagnosis, treatment, and control of the disease7.
According to a study conducted in Ethiopia, 196 M. tuberculosis isolated from enlarged lymph nodes belongs to different lineages8. In a review and meta-analysis conducted in Africa, a total of 6746 TB lymphadenitis cases were identified. The majority of the cases (70.6%) were from Ethiopia. Over 77% and 88% of identified TB lymphadenitis involved the cervical region and did not receive anti-TB drugs9.
In addition to TB lymphadenitis, there are various causes of pathologies of lymph nodes; the most common are malignant tumor, reactive hyperplasia, Hodgkin lymphoma, non-Hodgkin lymphoma, purulent abscess, and other chronic inflammation. Lymph nodes have a characteristic presentation depending on the etiology and can present as acute painful swelling due to infection or chronic painless swelling7,10,11.
Even though Ethiopia is among high TB burden countries, there is limited data of TB lymphadenitis from Adama, East Shoa zone, Oromia Regional State. In this study, we aimed to determine the magnitude of TB lymphadenitis among patients with enlarged lymph nodes at ACSHMC using GeneXpert, Ziehl–Neelsen (ZN) staining, and cytology.
Materials and methods
Study design and area
An institutional-based prospective cross-sectional study was conducted from May, 2022, to August, 2022. The study was conducted in the East Shoa zone, Oromia Regional State, Ethiopia, ACSHMC, Adama, Ethiopia. Adama city is located in the East-South direction about 100 km from the capital city of Ethiopia. Based on the 2021/2022 TB data, Adama Comprehensive Specialized Hospital Medical College (ACSHMC) has suspected a total of 1458 all forms of TB cases, from this 456 were confirmed TB Lymphadenitis in cytological diagnosis methods only. Gene X pert and AFB are not in use in the study site for the diagnosis of the disease.
Study population
All patients with enlarged lymph nodes who visited ACSHMC, the pathology department for FNAC examination during the study period were considered for the study. The required sample size was determined using a single population proportion formula by considering prevalence reported from Bahirdar, Ethiopia (22.1%)12 and 95% confidence level. After considering 10% for the non-response rate, the total sample size was 291. We have used convenient sampling technique to recruit study participants.
Eligibility criteria
Inclusion criteria
All patients who had enlarged lymph nodes and visited the pathology department at ACSHMC were included.
Exclusion criteria
The patient who had enlarged lymph node but the FNA sample is not sufficient for the laboratory test and patents not voluntary for this study were excluded.
Study variables
Dependent variable: TB Lymphadenitis diagnosed by GeneXpert.
Independent variables: Socio-demographic and clinical characteristics.
Data collection
For the collection of demographic and clinical characteristics, we used an interviewer-based structured questionnaire prepared after reviewing similar studies12,13,14. About 1.5–3 ml Fine Needle Aspirate (FNA) specimens were collected from enlarged lymph nodes to be diagnosed using GeneXpert16, ZN staining17, and Cytology18.
Data quality control
The questionnaire was pre-tested on a population representing 5% of the sample size to check its consistency before the actual data collection. Each day, after data collection, collected data were checked and evaluated for completeness, accuracy, and clarity. The sample processing control contains non-infectious spores in the form of a dry spore cake that is included in each cartridge to verify adequate processing of TB. To control bias that could arise from laboratory investigation, smear microscopy were read by three professionals before the final issuance of the result.
Statistical analysis
Data were entered into the computer using Epi Data version 3.1 and exported to SPSS version 25 (Statistical Package for Social Science) software for analysis. Bivariable and multivariable binary logistic regression were used to determine the association between dependent and independent variables. Initially, data were analysed using bivariable logistic regression; variables with p < 0.25 were further analyzed by multivariable logistic retrogression. The statistical significance was considered at a p < 0.05.
Ethical consideration
Ethical clearance was obtained from the nationally registered ethical institutional review board of Hawassa University medical college (Ref No. IRB\148\14). All participants were informed of the purpose, risk, and benefit of the study and their participation was voluntary. Written informed consent was obtained from all participants. For minors, consent from the parents or legal guardians and assent from minors were obtained. The identifier of study participants were removed from all formats. All methods were carried out in accordance with relevant guidelines and regulation as mentioned by Declaration of Helsinki.
Results
Socio demographic characteristics
A total of 291 study participants with enlarged lymph nodes were included in this study, of which 121 (41.8%) were males. The mean age of study participants was 28 (SD ± 14.8). Most of the patients did not have history of treatment for TB (Table 1).
Clinical characteristics
The common clinical presentations were fever (55%), weight loss (50.9%), night sweating (54.6%), and fatigue (52.6%). The most involved body sites (lymph nodes) were cervical (54.6%), axillary (11.3%) supraclavicular (10.3%), and submandibular (15.5%). The least affected lymph node were the auricular and inguinal lymph node with (1.4%), and (6.9%) respectively (Table 2).
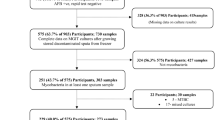
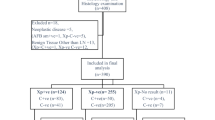
Prevalence of TB lymphadenitis
From 291 participants with enlarged lymph nodes, 138 (47.4%) (95% CI 41.70–53.10) were MTB positive by the GeneXpert method. Whereas 100 (34.4%) (95% CI 28.94–39.85) and 123 (42.3%) (95% CI 36.63–47.00) were positive by ZN staining and cytology respectively. 85 (29.2%) were positive in all three methods; 102 (35%) positive by AFB and GeneXpert; 116 (39.9%) were positive by GeneXpert and cytology. Non-acid fast bacilli Bacteria were detected among 33 (11.3%) participants using Gram staining technique, out of which 32/33 (97%) were Gram—positive cocci and 1/33 (3%) were Gram—negative rods. Moreover, cytological diagnosis revealed 89 (30.6%) reactive lymphadenitis, 27 (9.3%) lymphoma, 16 (5.5%) chronic abscess, 6 (2.1%) malignancy and 8 (2.7%) carcinoma, 8 (2.7%) pyogenic, 5 (1.7%) benign, 3 (1.0%) hematoma 3 (1.0%) granuloma and 3 (1.0%) abscess.
Rifampicin drug resistance gene
Out of 291 participants, 9 (3.1%) were infected with rifampicin-resistant genes positive M. tuberculosis while 3 (1.0%) of them were infected with M. tuberculosis which was rifampicin-intermediate. Overall, 9 out of 138 M. tuberculosis (6.5%) were positive for the rifampin-resistant gene.
Factors associated with TB lymphadenitis
Variables such as place of residence, marital status, educational level, consumption of raw milk, and chronic cough showed a p < 0.25 in bivariable analysis and were selected for multivariable analysis. In multivariable analysis, TB lymphadenitis was significantly associated with chronic cough (Table 3).
Discussion
According to cytological studies, TB lymphadenitis is reported to be the common problem in Ethiopia12,13,18. However, these studies are mostly of retrospective type in nature and used cytology for the diagnosis of TB lymphadenitis12,13,17. The prevalence of TB lymphadenitis may vary depending on the method used for the diagnosis and the clinical background of the patients.
Many studies including our study revealed high prevalence of TB lymphadenitis among patients with enlarged lymph nodes as compared to other clinical conditions. In the current study, the overall prevalence of TB lymphadenitis using GeneXpert was 47.4%. Our finding is in line with the prevalence of TB lymphadenitis reported from Hawassa, Ethiopia (48.8%)7 and Addis Ababa, Ethiopia (49.3%)15. However, higher prevalence TB lymphadenitis was reported from Gondar, Ethiopia (65.7%)13, Jimma, Ethiopia (58.0%)14, Butajira, Ethiopia (72.8%)19 and Tanzania (69.5%)20. In contrast to our study, low prevalence of TB lymphadenitis was reported from Nigeria (24.45%)21 and Pakistan (44%)22. The variation might be due to socio-demographic factors and the laboratory method used. Some of the studies used cytological methods whereas others used molecular method which might be responsible for the differences observed.
The prevalence of TB lymphadenitis using ZN staining method was 34.4%. This finding is high compared to study conducted in Addis Ababa, Ethiopia (14.5%) which used a similar laboratory methods—ZN staining method16. A study conducted in a Sudan also reported low AFB positivity (9%) of lymphadenitis23.
According to the cytological examination (FNAC) of the present study, the prevalence of TB lymphadenitis was 42.3%. Reactive lymphadenitis was the second most frequent cause of enlarged lymph nodes. Lymphoma and the chronic abscess was the third and fourth frequent cause of enlarged lymph nodes respectively. The prevalence of TB lymphadenitis identified by cytological methods correlates with a study conducted in different parts of Ethiopia7,12. Another study from South Ethiopia showed a higher prevalence of TB lymphadenitis (68.7%) using cytological diagnosis15.
Overall, the performance of GeneXpert in diagnosing TB lymphadenitis was superior (47.4%) compared to the cytological method (42.3%) and ZN staining (34.4%). From the total study participants (N = 291), 29.2%, 35%, and 39.9% were positive for MTB by all three methods, AFB and GeneXpert, GeneXpert, and cytology respectively. Bacteria other than MTB were detected from 11.3% of participants with enlarged lymph nodes; the predominant bacteria were Gram-positive cocci. This indicates the role of other bacteria in lymphadenitis or it can be a super infection and need further study.
In contrast to a study conducted in Gondar13, in the current study male participants were more affected by lymphadenitis (48.8%) than their female counterparts (46.5%). This could be due to differences in lifestyle among males and females in different localities.
The majority of participants with enlarged lymph nodes were adults. 46% of participants within the age group of 25–34 years had enlarged lymph nodes whereas those within 15–24 years old accounted for 25%. This finding is inconsistent with other studies done in Ethiopia; where 25–34 years old are the commonest age group affected14,15. Review and Meta-analysis conducted in Africa indicated a high frequency of enlarged lymph nodes among individuals within the 20–40 years age group24.
Chronic cough was the only independent variable significantly associated with TB lymphadenitis. Patients who had a history of chronic cough had 2 times odds of developing TB lymphadenitis as compared to those who had no history of cough. This finding is in line with the finding reported from Jimma, Ethiopia14; however, it is not comparable to a study conducted in Gondar, Ethiopia13.
In this study, the cervical lymph node was found to be the most commonly affected site (54.6%). Similar finding was reported from northern parts of Ethiopia (57.1%)12. Hawassa, Ethiopia (57.1%)7, and Gondar, Ethiopia (47.5%)13. In addition, a report from India indicated a high prevalence of lymphadenitis involving cervical lymph nodes4.
The history of drinking raw milk among TB lymphadenitis cases was (21.0%). However, the history of drinking uncooked milk was not significantly associated with the occurrence of TB lymphadenitis. This finding is in line with the studies conducted in Addis Ababa, Ethiopia15.
In this study, 3.1% of participants were infected with rifampicin-resistant gene positive M. tuberculosis which is in line with the study conducted in Gondar, Ethiopia 3.9%24, India (2.9%)25, and Kenya (3.7%)26. A study conducted in Hawassa, Ethiopia among patients suspected of pulmonary TB revealed a prevalence of rifampicin resistance of 1.24% which is lower than the current study27. Out of 138 M. tuberculosis detected in this study, 9 were positive for the rifampin-resistant gene giving a proportion of 6.5%. Additionally, several studies reported a high prevalence of rifampicin resistance gene positive M. tuberculosis such as study from Nigeria (14.7%)28, India (5.4%)4, Addis Ababa, Ethiopia (9.9%)29, and Adigrat, Ethiopia (9.1%)30.
Limitation of the study
As this study is a cross-sectional study, it will not establish the cause and effect. The participants might forget some variables which asks about their previous experience and might have led to recall bias. Use of convenient sampling technique might have introduced selection bias.
Conclusions
Close to 50% of patients with enlarged lymph node were positive for TB lymphadenitis by GeneXpert in the study area. GeneXpert detected high number of TB lymphadenitis as compared to cytology and ZN staining technique. Chronic cough was significantly associated with TB lymphadenitis. The prevalence of rifampicin-resistant gene positive M. tuberculosis was relatively prevalent among patients with enlarged lymph node in the study area.
Data availability
All relevant data are available within the paper.
References
Smith, I. Mycobacterium tuberculosis pathogenesis and molecular determinants of virulence. Clin. Microbiol. Rev. 16(3), 463–496 (2003).
Tadesse, M. et al. Concentration of lymph node aspirate improves the sensitivity of acid fast smear microscopy for the diagnosis of tuberculous lymphadenitis in Jimma, southwest Ethiopia. PLoS ONE 9(9), e106726 (2014).
World Health Organization. Global tuberculosis control (2014).
Singh, S. K. & Tiwari, K. K. Tuberculous lymphadenopathy: Experience from the referral center of Northern India. Niger. Med. J. 57(2), 134 (2016).
Moule, M. G. & Cirillo, J. D. Mycobacterium tuberculosis dissemination plays a critical role in pathogenesis. Front. Cell. Infect. Microbiol. 10, 65 (2020).
Francis, D. O. et al. Voice-related patient-reported outcome measures: A systematic review of instrument development and validation. J. Speech Lang. Hear. Res. 60(1), 62–88 (2017).
Buli, G. & Lukas, F. Cytologic patterns of lymph node diseases in Hawassa University referral hospital, southern Ethiopia. J. Coast. Life Med. 3(5), 395–397 (2015).
Biadglegne, F., Merker, M., Sack, U., Rodloff, A. C. & Niemann, S. Tuberculous lymphadenitis in Ethiopia predominantly caused by strains belonging to the Delhi/CAS lineage and newly identified Ethiopian clades of the Mycobacterium tuberculosis complex. PLoS ONE 10(9), e0137865 (2015).
Mekonnen, D. et al. Epidemiology of tuberculous lymphadenitis in Africa: A systematic review and meta-analysis. PLoS ONE 14(4), e0215647 (2019).
Aggarwal, R., Nautiyal, A., Mathur, P. & Joshi, Y. A review on tuberculosis [TB], its control and management. Int. J. Sci. Dev. Res. 7(3), 2455–2631 (2022).
Adkins, M. S., Raccuia, J. S. & Acinapura, A. J. Esophageal perforation in a patient with acquired immunodeficiency syndrome. Ann. Thorac. Surg. 50(2), 299–300 (1990).
Biadglegne, F., Tesfaye, W., Sack, U. & Rodloff, A. C. Tuberculous lymphadenitis in northern Ethiopia: In a public health and microbiological perspectives. PLoS ONE 8(12), e81918 (2013).
Muluye, D., Biadgo, B., Woldegerima, E. & Ambachew, A. Prevalence of tuberculous lymphadenitis in Gondar University Hospital, Northwest Ethiopia. BMC Public Health 13, 1–5 (2013).
Abebe, G. et al. Tuberculosis lymphadenitis in Southwest Ethiopia: A community based cross-sectional study. BMC Public Health 12(1), 1–7 (2012).
Fantahun, M. et al. Diagnostic accuracy of Xpert MTB/RIF assay and non-molecular methods for the diagnosis of tuberculosis lymphadenitis. PLoS ONE 14(9), e0222402 (2019).
Siala, M. et al. First-time detection and identification of the Mycobacterium tuberculosis complex members in extrapulmonary tuberculosis clinical samples in south Tunisia by a single tube tetraplex real-time PCR assay. PLoS Negl. Trop. Dis. 11(5), e0005572 (2017).
Bruckner, M. Z. Gram staining. Microbial Life Educational Resources (2016).
Yassin, M. A. et al. Diagnosis of tuberculous lymphadenitis in Butajira, rural Ethiopia. Scand. J. Infect. Dis. 35(4), 240–3 (2003).
Perenboom, R. M. et al. Diagnosis of tuberculous lymphadenitis in an area of HIV infection and limited diagnostic facilities. Trop. Geogr. Med. 46(5), 288–292 (1994).
Mandal, N., Anand, P. K., Gautam, S., Das, S. & Hussain, T. Diagnosis and treatment of paediatric tuberculosis: An insight review. Crit. Rev. Microbiol. 43(4), 466–480 (2017).
Majeed, M. M. & Bukhari, M. H. Evaluation for granulomatous inflammation on fine needle aspiration cytology using special stains. Pathol. Res. Int. 2011, 851524 (2011).
Kaur, A., Bunger, R., Jad, B., Singh, V. A. & Mahajan, N. C. Extrapulmonary tuberculosis in MMIMSR, Muallana Ambala: A microbiological & histopathological study. JK Sci. 14(3), 139 (2012).
Reddy, D. L., Venter, W. D. & Pather, S. Patterns of lymph node pathology; fine needle aspiration biopsy as an evaluation tool for lymphadenopathy: A retrospective descriptive study conducted at the largest hospital in Africa. PLoS ONE 10(6), e0130148 (2015).
Jaleta, K. N. et al. Rifampicin-resistant Mycobacterium tuberculosis among tuberculosis-presumptive cases at University of Gondar Hospital, northwest Ethiopia. Infect. Drug Resist. 10, 185 (2017).
Raja, R., Sreeramulu, P. N., Dave, P. & Srinivasan, D. GeneXpert assay—A cutting-edge tool for rapid tissue diagnosis of tuberculous lymphadenitis. J. Clin. Tuberc. Other Mycobact. Dis. 21, 100204 (2020).
Likhovole, C. et al. Mycobacterium tuberculosis resistance to isoniazid and rifampicin in a HIV-1 endemic population in Western Kenya in 2014. BMJ Glob. Health 2(Suppl 2), A1–A67 (2017).
Andarge, D. B., Anticho, T. L., Jara, G. M. & Ali, M. M. Prevalence of Mycobacterium tuberculosis infection and rifampicin resistance among presumptive tuberculosis cases visiting tuberculosis clinic of Adare General Hospital, Southern Ethiopia. SAGE Open Med. 9, 20503121211045540 (2021).
Cadmus, S. I., Oluwasola, A. O., Okolo, C. A. & Bethrand, A. F. Pattern of tuberculous lymphadenitis diagnosed by fine needle aspiration cytology at the University College Hospital, Ibadan, Nigeria. Afr. J. Med. Med. Sci. 39(3), 193–197 (2010).
Arega, B., Menbere, F. & Getachew, Y. Prevalence of rifampicin resistant Mycobacterium tuberculosis among presumptive tuberculosis patients in selected governmental hospitals in Addis Ababa, Ethiopia. BMC Infect. Dis. 19(1), 1–5 (2019).
Abay, G. K. & Abraha, B. H. Trends of Mycobacterium tuberculosis and rifampicin resistance in Adigrat General Hospital, eastern zone of Tigrai, North Ethiopia. Trop. Dis. Travel Med. Vaccines 6(1), 1–9 (2020).
Funding
No specific funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
H.K.: Protocol development, data collection, and data analysis, D.Y.R.: Supervision, Protocol development. M.S.: Data analysis, laboratory protocol development, data collection A.T.: Data analysis, laboratory protocol development M.D.O.: Supervision and validation of method MMA Protocol development, supervision during data collection, manuscript preparation. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kumbi, H., Reda, D.Y., Solomon, M. et al. Magnitude of tuberculosis lymphadenitis, risk factors, and rifampicin resistance at Adama city, Ethiopia: a cross-sectional study. Sci Rep 13, 15955 (2023). https://doi.org/10.1038/s41598-023-43206-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43206-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.