Abstract
Schistosomiasis japonicum can cause different degrees of organ damage and complex human immune pathological reactions, which often invade the intestine and liver. The purpose of this study was to explore the pathological types and pathological changes of Schistosomiasis and their correlation with some digestive system tumors. Hematoxylin eosin staining was performed on the diseased tissues of 1111 Schistosomiasis cases. We counted the deposition sites of Schistosoma eggs, analyzed the pathological characteristics, and compared the clinicopathological characteristics of Schistosomiasis associated digestive system tumors and non-Schistosomiasis digestive system tumors. We found that Schistosoma japonicum can cause multi organ and multi system damage, with 469 cases of inflammation, 47 cases of adenoma, and 519 cases of adenocarcinoma. Other types include cysts, stromal tumors, malignant lymphomas, and neuroendocrine tumors. Schistosomiasis associated tumors, including gastric cancer, liver cancer, colon cancer and rectal cancer, were compared with non-Schistosomiasis tumors. There were significant differences in age, gender and tumor differentiation between the two groups. Our study shows Schistosomiasis is a systemic disease, causing multiple organ and system damage in the human body. Its clinicopathological types are diverse, and there may be a pathological change process of “Inflammation-adenoma-carcinoma”. Schistosomiasis associated digestive system tumors differ from non-Schistosomiasis tumors in some clinicopathological features.
Similar content being viewed by others
Introduction
Schistosomiasis is a zoonotic parasitic disease. In China, Schistosoma japonicum is mainly prevalent in the Yangtze River basin1. By the end of 2021, there were 12 Schistosomiasis endemic provinces (municipalities and autonomous regions) and 450 Schistosomiasis endemic counties (cities and districts). There are approximately 72,937 cases of Schistosomiasis and 29,037 cases of advanced Schistosomiasis in China. In the life cycle of Schistosoma japonicum, the tail spider, the adult worm and the egg can all lead to varying degrees of damage and complex immunopathological reactions to the human body2. Schistosomiasis is a chronic immune disease caused by egg granuloma. Pathological examination is one of the important methods for the diagnosis of Schistosomiasis3. Its pathological basis is the stimulation of a large number of mature eggs deposited in the intestinal and liver tissues, the pathological immune response of the host to the soluble antigen secreted by live cercariae, and the formation of egg granuloma and secondary fibrosis4. Rarely known by people, the eggs can also cause different types of pathological changes in other parts of the body. However, only a few case reports and small sample size studies can not reflect the correlation between Schistosomiasis and the pathological changes in other body parts.
With the development of society and the changes of people’s lifestyle, the incidence and mortality of cancer are rising rapidly5, among which digestive tract-related malignant cancer have become the main cause of human death. In recent years, the relationship between Schistosomiasis and tumor attracts much attention. According to the International Agency for Research on Cancer (IARC), Schistosoma haematobium has a clear carcinogenic effect on humans. Schistosoma haematobium can cause bladder cancer. Its pathogenic process is that the adults lay eggs in the bladder venous plexus, and the eggs spread along the blood vessels to the bladder, ureter and genital tract. The eggs stimulate the tissue to produce continuous inflammatory response, leading to Urogenital Schistosomiasis (UGS)6, 7. Bladder cancer is one of the common complications of UGS. Although the carcinogenic effects of Schistosoma japonicum and Schistosoma mansoni are not clear, they are often found parasitic in mesenteric veins and oviposit. The eggs spread with the blood. Eggs deposited in liver and intestinal tissues recruit a variety of inflammatory factors leading to granuloma formation. Some of these inflammatory cells can release a large amount of reactive oxygen species and NO, leading to oxidative stress-induced DNA damage, thereby causing malignant transformation of tissue cells8,9,10,11. In China, where Schistosomiasis japonica is endemic, gastric cancer, liver cancer and colorectal cancer are common malignant tumors of the digestive system. In this study, 1111 cases of Schistosoma japonicum were pathologically confirmed to observe the deposition site and pathological types of Schistosoma eggs, and to compare the pathological features of Schistosomiasis associated tumors and non-Schistosomiasis tumors.
Materials and methods
Patient data collection
The clinicopathological data of 1111 patients with chronic Schistosomiasis in the First Affiliated Hospital of Wannan Medical College and Chizhou people’s Hospital from January 2015 to December 2021 were collected and retrospectively in this study. (These two hospitals are the main hospitals for treating Schistosomiasis patients, and a total of 2500 beds are opened to treat patients in Schistosomiasis endemic areas). The patients included in the study were all from the Schistosomiasis endemic area in southern Anhui Province. The included patients showed Schistosoma eggs by histopathological examination of lesions, and patients with other parasitic infections and overseas tourism history were excluded. Pathological specimens were obtained by surgical resection, endoscopic biopsy, and needle biopsy. All pathological specimens were diagnosed by two pathologists.
A total of 498 patients with gastric cancer, liver cancer, colon cancer and rectal cancer were selected from this study and included in Schistosomiasis associated tumor group. The Schistosoma eggs and tumor cells could be seen in the pathological examination of the included patients, and the tumor and metastatic tumor caused by other factors (such as bacterial infection, viral infection, poison contact, genetic and other factors) were excluded. We collected almost the same number of patients with non-Schistosomiasis tumors each year. A total of 569 patients with gastric cancer, liver cancer, colon cancer and rectal cancer without Schistosomiasis in the same region during the same period were collected as non-Schistosomiasis tumor group. These patients were definitely diagnosed by clinicopathology. Metastatic tumors and tumors caused by other factors were excluded from the enrolled patients. All tumor patients were confirmed by clinicopathology. The clinicopathological data of the two groups were collected.
This study was approved by the ethics committee of the First Affiliated Hospital of Wannan Medical College [Research Proposal Notification IRB Review Decision (2022) (No.33)]. Informed consent was obtained from all patients which were involved in this study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the Declaration of Helsinki.
Hematoxylin–eosin staining
1218 pathological specimens from 1111 patients with Schistosomiasis were roasted in an oven at 60 °C for 30 min, and after taking out the specimen, put it into xylene I and II for dewaxing for 5 min each. The specimens were put into gradient alcohol 100%, 95%, 85% and 75% for 1 min respectively for hydration. Then all specimens were rinsed with distilled water for 1 min, stained with hematoxylin for 4 min, differentiated with hydrochloric acid and ethanol for 15 s after rinsing, and then rinsed with pure water and then added with 0.5% eosin staining solution for 1 min. The specimens were rinsed with distilled water and dried, then put into gradient alcohol 95% I, 95% II, 100% I, 100% II for 5 min each, finally put into xylene I and II for 5 min each, mount.
Statistical method
SPSS 20.0 statistical software was used to analyze the data. Data are presented as frequency (n), percentage (%), mean ± standard deviation (SD), and quartiles, respectively. The clinicopathological data of Schistosomiasis associated tumor group and non-Schistosomiasis tumor group were analyzed (Variables such as age, sex, and pathological characteristics of tumors were analyzed). Student t test and Mann Whitney U test were used. Categorical variables were analyzed using chi square test. P < 0.05 was statistically significant.
Result
Distribution characteristics of Schistosomiasis patients
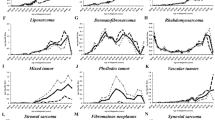
A total of 1111 cases of Schistosomiasis were collected from January 2015 to December 2021, including 747 males and 364 females, and aged from 18 to 93 years. There are 36 cases (4.05%) from 10 to 39 years old, 72 cases (6.481%) from 40 to 49 years old, 173 cases (15.572%) from 50 to 59 years old, 465 cases (41.855%) from 60 to 69 years old, 304 cases (27.363%) from 70 to 79 years old and 61 cases (5.491%) from 80 to 99 years old. The incidence of Schistosomiasis is mainly concentrated in the middle-aged and elderly people aged 60–69 years. (Fig. 1).
Deposition of Schistosoma eggs
Analysis of 1218 Schistosoma eggs deposition organs from 1111 patients revealed that Schistosoma eggs were mainly distributed in the digestive system, accounting for up to 84.56%. The main deposition organs of Schistosoma eggs are colon, rectum, appendix and stomach, and a few eggs are found in rare deposition organs such as esophagus, duodenum, ileum, cecum, gallbladder and pancreas. The egg deposition rate of Schistosoma japonicum in the lymphatic system was 13.55%, second only to the digestive system. In addition, Schistosoma eggs were also deposited in the reproductive system (1.07%), respiratory system (0.58%), nervous system (0.25%), etc. (Table 1; Figs. 2, 3).
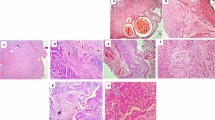
Schistosoma eggs deposition in the organs of the digestive system. (A) Schistosoma eggs are deposited in esophageal tissue; (B) Schistosoma eggs are deposited in the stomach tissue; (C) Schistosoma eggs are deposited in duodenal tissue; (D) Schistosoma eggs are deposited in colon tissue; (E) Schistosoma eggs are deposited in appendix tissue; (F) Schistosoma eggs are deposited in rectal tissue; (G) Schistosoma eggs are deposited in liver tissue; (H) Schistosoma eggs are deposited in pancreatic tissue; (I) Schistosoma eggs are deposited in gallbladder tissue. Magnification, × 100 or × 400.
Pathological features
In addition to the lymph nodes with Schistosoma egg deposits (165 cases), the pathological types of 1053 organ lesions with Schistosoma egg deposits are mainly inflammation, adenoma and adenocarcinoma, and only a few are other pathological types, such as cysts, stromal tumors, malignant lymphomas and neuroendocrine tumors. 469 organ lesions were inflammatory, including stomach, duodenum, small intestine (ileum, cecum), colon, appendix, rectum, liver, gallbladder, brain, ovary, fallopian tube, lung, and the appendix was the most prone to inflammation. 47 organ lesions were adenomas, including stomach, duodenum, colon, appendix, rectum, gallbladder, ovary, and colon was prone to adenomas. 519 organ lesions were adenocarcinoma, including esophagus, stomach, duodenum, ileum, cecum, colon, rectum, liver, pancreas, gallbladder, ovary, lung, and colon, rectum, stomach were prone to adenocarcinoma. Inflammation, adenoma, and adenocarcinoma can occur simultaneously in the stomach, duodenum, colon, rectum, gallbladder, and ovary. (Table 2).
The ages of 1035 cases with inflammation, adenoma and adenocarcinoma were (61.555 ± 13.025) years, (63.936 ± 9.628) years and (66.730 ± 9.156) years, respectively. There was no significant difference in age between the inflammation group and the adenoma group (P = 0.087), but there was a significant difference in age between the inflammation group and the adenocarcinoma group (P < 0.001), and there was a significant difference in age between the adenoma group and the adenocarcinoma group (P = 0.026). There were 664 males and 371 females, and the difference was statistically significant (P = 0.047). (Table 3).
Clinicopathological analysis of Schistosomiasis associated tumor group and non-Schistosomiasis tumor group
Based on this group of data, we selected the tumors with the top four proportions of Schistosomiasis combined with adenocarcinoma, gastric cancer, liver cancer, colon and rectal cancer. Schistosomiasis associated tumors were compared with non-Schistosomiasis tumors in the same period.
Comparison of clinicopathological data of gastric cancer:
In the gastric cancer group, the average ages of Schistosomiasis associate gastric cancer group (n = 156) and non-Schistosomiasis gastric cancer group (n = 179) were (67.449 ± 7.959) years and (62.14 ± 10.832) years, respectively, and the ages of the former were significantly higher than those of the latter (P < 0.001). There were more males than females in both groups, but the male to female ratio in the Schistosomiasis associated gastric cancer group was significantly higher than that in the non-Schistosomiasis gastric cancer group (P = 0.006). In terms of pathological characteristics of tumors in the two groups, Schistosomiasis associated gastric cancer mainly occurred in the body of the stomach, while non-Schistosomiasis gastric cancer mainly occurred in the pylorus, and the difference was statistically significant (P = 0.001). The differentiation degree of tumors in the two groups was different (P = 0.003), tumor appearance was different in 214 cases (P = 0.745), tumor blood vessels were different in 215 cases (P = 0.116), and regional lymph node metastasis was different in 214 cases (P = 0.904). (Table 4).
Comparison of clinicopathological data of hepatocellular carcinoma
In patients with liver cancer, the average ages of Schistosomiasis associated liver cancer group (n = 44) and non-Schistosomiasis liver cancer group (n = 64) were (65.886 ± 6.738) years and (64.438 ± 9.179) years, respectively, and there was no significant difference in age between the two groups (P = 0.43). There were more males than females in the two groups, but there was no statistical difference in the proportion of males and females in the two groups (P = 0.58). The proportion of poorly differentiated tumors in the Schistosomiasis associated liver cancer group was significantly higher than that in the non-Schistosomiasis liver cancer group (P = 0.019), but there was no statistical difference in the source of tumor cells (P = 0.135), the number of tumors (P = 0.159), the presence of tumor thrombus (P = 0.4) and the integrity of tumor envelope (P = 0.077). (Table 5).
Comparison of clinicopathological data of colon cancer
Among colon cancer patients, the average ages of Schistosomiasis associated colon cancer group (n = 158) and non-Schistosomiasis colon cancer group (n = 159) were (67.331 ± 10.082) years and (61.194 ± 11.675) years, respectively, with statistical differences (P < 0.001). There were more males than females in the two groups, and the male to female ratio in the Schistosomiasis associated colon cancer group was significantly higher than that in the non-Schistosomiasis colon cancer group (P = 0.005). In terms of tumor pathological characteristics, there was a statistically significant difference in the degree of differentiation between the two groups (P = 0.013), but there was no difference in the tumor prone site (0.177), tumor phenotype (0.195), presence or absence of tumor thrombus (0.069), and presence or absence of lymph node metastasis (0.076). (Table 6).
Comparison of clinicopathological data of rectal cancer
In patients with rectal cancer, the average ages of Schistosomiasis associated rectal cancer group (n = 140) and non-Schistosomiasis rectal cancer group (n = 167) were (65.706 ± 9.5549) years and (59.517 ± 15.242) years, respectively, with statistically significant differences (P < 0.001). There were more males than females in the two groups, and the male to female ratio of Schistosomiasis associated rectal cancer was higher than that of non-Schistosomiasis rectal cancer group, but the difference was not statistically significant (P = 0.061). In terms of tumor pathological characteristics, there was a statistically significant difference in tumor differentiation between the two groups (P = 0.001), but there was no statistically significant difference in tumor phenotype (P = 0.378), tumor thrombus (P = 0.388), and lymph node metastasis (P = 0.331). (Table 7).
Discussion
Schistosomiasis is the most important parasitic disease that endangers people’s health12, 13. There are mainly six kinds of Schistosomiasis that infect humans: Schistosoma haematobium, Schistosoma mansoni, Schistosoma japonicum, Schistosoma mekongi, Schistosoma interdental and Schistosoma malayi14. China is an endemic area of Schistosomiasis japonica. Schistosomiasis is prevalent in the Yangtze River Basin and 12 provinces in the south of China. The pathological changes of Schistosomiasis are mainly caused by eggs, which are mainly deposited in the liver and colon wall of the host. Granuloma and fibrosis caused by Schistosomiasis are the main pathological changes of Schistosomiasis15. The formation of egg granuloma is an immune response of the host to pathogenic factors. On the one hand, the eggs are destroyed and removed by granuloma reaction, and the antigens released by eggs can be isolated and removed. Reduce the formation of antigen–antibody complex in blood circulation and damage to the body. On the other hand, granuloma reaction destroys the normal tissue of the host, and the continuous formation of egg granuloma forms interconnected scars, leading to a series of lesions such as trunk cirrhosis and intestinal wall fibrosis16.
Schistosoma japonicum usually lives in the portal vein system, mainly involving the colon and liver17, especially the sigmoid colon and rectum, and small intestinal lesions are rare18. Occasionally, in some cases of severe infection, adult worms and egg granulomas are found outside the portal system, causing ectopic damage, mainly in the lungs and brain19. In long-term research, scholars believe that Schistosoma japonicum and Schistosoma mansoni can lead to liver and intestinal damage, and Schistosoma haematobium mainly leads to urinary and reproductive system damage8, 20, 21. However, there is no report summarizing which human organs are affected by Schistosoma japonicum in addition to its ability to damage the digestive system. This study found that Schistosoma eggs are deposited in more human system organs and cause damage. Schistosoma eggs are mainly deposited in the digestive system (esophagus, stomach, duodenum, ileum, cecum, colon, rectum, gallbladder, pancreas, liver). In addition, a few insect eggs are also deposited in the respiratory system (lung), nervous system (brain), reproductive system (uterus, ovary, fallopian tube), but most of the case samples found that insect eggs are deposited in the lymphatic system, causing damage to the lymphatic system. Therefore, we believe that Schistosomiasis japonica has caused multiple organ and system damage to the human body.
A total of 1111 cases of Schistosomiasis japonica patients diagnosed pathologically were collected in this study, including 747 males and 364 females. Males were significantly more than females. The age of the patients ranged from 18 to 93 years old, and the main age groups were 50–59 years old (15.572%), 60–69 years old (41.855%) and 70–79 years old (27.363%). The age of onset of Schistosomiasis is concentrated in 60–69 years old, which is basically consistent with the age of onset of Schistosomiasis associated colorectal cancer45. The main pathological types of Schistosoma eggs were inflammation in 469 cases, adenoma in 47 cases and adenocarcinoma in 519 cases. The ages of the three pathological types were (61.555 ± 13.025) years, (63.936 ± 9.628) years and (66.730 ± 9.156) years, respectively. Inflammatory reactions play an important role in the occurrence and development of tumors22. In this study, according to the age sequence of the three pathological types, it is not difficult to find that the lesion may have a development trend of “Inflammation-adenoma-carcinoma”. Chronic inflammation of local tissues caused by Schistosomiasis may eventually lead to cancer, which is similar to the occurrence of Schistosoma haematobium and bladder cancer7, Hepatitis B Virus (HBV) infection leading to liver cancer23 and Helicobacter pylori (Hp) infection leading to gastric cancer24. We speculate that there may be a correlation between Schistosomiasis and cancer. At the same time, it was also found that other pathological types could be present in the lesion, including cysts, stromal tumors, malignant lymphomas and neuroendocrine tumors.
Interestingly, when analyzing the deposition sites and pathological types of Schistosoma eggs in this set of data, it was found that appendicitis has a high incidence in Schistosomiasis endemic areas, and some patients with Schistosomiasis appendicitis can also develop adenomas25. However, few literatures have reported whether Schistosomiasis japonica is related to appendicitis. Some chronic appendicitis occurred insidiously, and most of them have no obvious symptoms. When the appendix needs to be removed for reasons such as intestinal tumors, it is found that Schistosoma eggs are deposited in the appendix. It is reported that more than 30% of appendiceal specimens taken from patients in Schistosomiasis endemic areas can be found to be Schistosoma eggs26. The reason for this phenomenon may be that Schistosoma eggs are wrapped in the tissue to form a granuloma, which further fibrosis makes the appendix wall and appendix cavity narrow, prone to fecal retention and obstruction of appendix cavity.
The relationship between Schistosoma japonicum infection and intestinal malignancy has been controversial since the 1980s. Since then, epidemiological studies have found that people infected with Schistosoma japonicum have an increased risk of colorectal cancer27,28,29. But so far, no carcinogen has been isolated from adult worms or eggs of Schistosoma japonicum. Research has found some evidence to prove their correlation. Many literatures have reported the relationship between Schistosomiasis japonica and colorectal tumors, but few have reported the relationship between other tumors such as gastric cancer and small intestinal tumors and Schistosomiasis japonica30,31,32. In fact, in addition to causing more extensive and serious intestinal damage, Schistosoma japonicum infection may also have an impact on the digestive system, one of the most serious consequences is the occurrence of malignant tumors. Among many malignant tumors of digestive system, the top ten tumors with morbidity and mortality include liver cancer, gastric cancer and colorectal cancer5. The risk factors of gastric cancer include age, sex, race, Helicobacter pylori infection, smoking, diet, genetics and other factors33. At present, only a few studies believe that there may be a correlation between Schistosomiasis and gastric cancer, but there is no clear mechanism to confirm the relationship34,35,36. The risk factors for liver cancer include viral infection, metabolic related fatty liver disease, long-term exposure to toxicants, and parasitic infection. However, Clonorchis sinensis is a well-known parasite associated with liver cancer. Schistosoma eggs are often deposited in the hepatic portal vein, causing liver injury and causing liver and spleen Schistosomiasis. It is unclear whether liver and spleen Schistosomiasis can be used as a precancerous lesion of liver cancer37. Among the risk factors for colorectal cancer, those confirmed by research include age, sex, family history, intestinal inflammatory polyps, excessive alcohol consumption, smoking, obesity and long-term use of processed meat38. However, chronic Schistosomiasis as a risk factor for colorectal cancer has been debated for decades39. According to this group of data, the incidence of Schistosomiasis with adenocarcinoma is relatively high, and the most common sites are stomach, liver, colon and rectum.
This study shows that the incidence of gastric cancer in patients with gastric Schistosomiasis is more than 50%, and the clinical manifestations are similar to those of chronic gastritis, peptic ulcer and advanced gastric cancer, which can only be confirmed by postoperative gastroscopic biopsy or pathological examination40. In this study, the age of Schistosomiasis associated gastric cancer group was significantly higher than that of non-Schistosomiasis group (P < 0.001), and the male to female ratio of the former was much higher than that of the latter (P = 0.006). In terms of tumor location, gastric cancer with Schistosomiasis mainly occurred in the cardia, fundus and body of the stomach, which is consistent with the predilection site of gastric cancer proposed in previous reports41. Most non-Schistosomiasis gastric cancers occurred in pylorus. The difference between the two groups was statistically significant (P = 0.001). There were no significant differences in tumor phenotype (P = 0.745), differentiation (P = 0.232), intravascular tumor thrombus formation (P = 0.116) and local lymph node metastasis (P = 0.904) between the two groups.
The patients with non-Schistosomiasis liver cancer served as the control group and were compared with the Schistosomiasis associated liver cancer group. The two groups of liver cancer patients showed statistical differences only in the degree of tumor differentiation (P = 0.019), and the proportion of poorly differentiated liver cancer in the Schistosomiasis associated liver cancer group was higher than that in non-Schistosomiasis liver cancer. There were no statistically significant differences in age, gender, source of tumor cells, number of tumor cells, presence or absence of tumor thrombi in blood vessels, and integrity of tumor capsule. These data cannot clearly explain whether Schistosomiasis affects the occurrence and development of gastric cancer and liver cancer. However, Schistosomiasis associated gastric cancer and Schistosomiasis associated liver cancer differ from non-Schistosomiasis tumors in age, sex, susceptible site and tumor differentiation, which means that Schistosomiasis may change the relevant mechanism of tumorigenesis.
In recent years, some studies have shown that the occurrence of colon cancer is related to the infection of some pathogens, such as bacteria42, 43, parasites38, 44 and other pathogens. In this study, we found statistically significant differences in age and sex between the Schistosomiasis associated colon cancer group and the non-Schistosomiasis group. The average age of patients in the Schistosomiasis associated colon cancer group was (67.331 ± 10.082) years, which was significantly higher than that in the non-Schistosomiasis group (61.194 ± 11.675) years, and the difference was statistically significant (P < 0.001). The male to female ratio of Schistosomiasis associated colon cancer group was higher than that of non-Schistosomiasis group (P = 0.005). There was significant difference in tumor differentiation between the two groups (P = 0.013). There was no difference in tumor location, tumor morphology, tumor thrombus and local lymph node metastasis between the two groups. Our results showed that in addition to rectal cancer, there were chronic inflammation and adenomas in the colonic lesions of Schistosomiasis. It is known that patients with long-term Schistosomiasis associated chronic inflammation and adenomas have an increased risk of colorectal cancer45. These pathological changes are considered to be the pathological basis of the malignant potential of Schistosomiasis associated colorectal cancer.
Among rectal cancer patients, there are statistical differences in age and gender between the Schistosomiasis associated rectal cancer group and the non-Schistosomiasis group. The average age of the former is (65.706 ± 9.5549) years, which is higher than the latter (59.517 ± 15.242) years, and the difference is statistically significant (P < 0.001). There were more males than females in both groups, and the male to female ratio in the former was significantly higher than that in the non-Schistosomiasis group (P = 0.005). There was a significant difference in tumor differentiation between the two groups of patients (P = 0.013). There was no significant difference in tumor morphology, tumor thrombus, and local lymph node metastasis between the two groups. Low differentiated tumors often have poor prognosis, which is consistent with the reported poor prognosis of Schistosomiasis associated rectal cancer compared to non-Schistosomiasis rectal cancer in the literature. Moreover, regardless of the intervention of treatment methods, the prognosis of the former is relatively poor compared to the latter29, 46.
Conclusion
In summary, Schistosoma japonicum can cause damage to multiple systems and organs, and the types of lesions are diverse. Inflammation, adenoma and carcinoma are still common lesion types. According to the average age of the three lesion types, the pathological change process showed a trend of “Inflammation-adenoma-carcinoma”. So, we speculate that Schistosomiasis may be associated with the occurrence of cancer. Some pathological characteristics of patients with Schistosomiasis associated tumors are different from those of non-Schistosomiasis associated tumors. Schistosomiasis may affect the pathogenesis of tumors. Further exploration of the correlation between Schistosomiasis and digestive system tumors and the pathogenesis of Schistosomiasis associated tumors will help to prevent and treat malignant tumors, reduce the incidence of malignant tumors in endemic areas, and improve the survival time of patients with chronic Schistosomiasis.
Data availability
The data were obtained in Department of infectious diseases, the First Affiliated Hospital of Wannan Medical College and Chizhou first people’s Hospital. The datasets used and during the current study are available from the corresponding author on reasonable request.
References
Colley, D. G., Bustinduy, A. L., Secor, W. E. & King, C. H. Human schistosomiasis. Lancet 383(9936), 2253–2264 (2014).
Wang, X. Y., He, J., Yang, K. & Liang, S. Applications of spatial technology in schistosomiasis control programme in The People’s Republic of China. Adv. Parasitol. 92, 143–163 (2016).
Gobbi, F. et al. New insights on acute and chronic schistosomiasis: Do we need a redefinition?. Trends Parasitol. 36(8), 660–667 (2020).
McManus, D. P. et al. Schistosomiasis-from immunopathology to vaccines. Semin. Immunopathol. 42(3), 355–371 (2020).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
von Bülow, V. et al. Does Schistosoma Mansoni facilitate carcinogenesis?. Cells 10(8), 1982 (2021).
Santos, L. L. et al. Urogenital schistosomiasis-history, pathogenesis, and bladder cancer. J. Clin. Med. 10(2), 205 (2021).
Llanwarne, F. & Helmby, H. Granuloma formation and tissue pathology in Schistosoma japonicum versus Schistosoma mansoni infections. Parasite Immunol. 43(2), e12778 (2021).
Masamba, P. & Kappo, A. P. Immunological and biochemical interplay between cytokines, oxidative stress and Schistosomiasis. Int. J. Mol. Sci. 22(13), 7216 (2021).
Vennervald, B. J. & Polman, K. Helminths and malignancy. Parasite Immunol. 31(11), 686–696 (2009).
Klaunig, J. E. Oxidative stress and cancer. Curr Pharm Des. 24(40), 4771–4778 (2018).
Moreira-Filho, J. T. et al. Schistosomiasis drug discovery in the era of automation and artificial intelligence. Front. Immunol. 12, 642383 (2021).
Mawa, P. A., Kincaid-Smith, J., Tukahebwa, E. M., Webster, J. P. & Wilson, S. Schistosomiasis morbidity hotspots: Roles of the human host, the parasite and their interface in the development of severe morbidity. Front. Immunol. 12, 635869 (2021).
Zhao, G. H. et al. Biotechnological advances in the diagnosis, species differentiation and phylogenetic analysis of Schistosoma spp. Biotechnol. Adv. 30(6), 1381–1389 (2012).
Masi, B., Perles-Barbacaru, T. A., Bernard, M. & Viola, A. Clinical and Preclinical Imaging of Hepatosplenic Schistosomiasis. Trends Parasitol. 36(2), 206–226 (2020).
Qin, X. et al. The clinical features of chronic intestinal schistosomiasis-related intestinal lesions. BMC Gastroenterol. 21(1), 12 (2021).
Huang, Y. et al. Effect of miR-182 on hepatic fibrosis induced by Schistosomiasis japonica by targeting FOXO1 through PI3K/AKT signaling pathway. J. Cell Physiol. 233(10), 6693–6704 (2018).
Eder, B. V. A., Bösmüller, H., Schubert, T. & Bissinger, A. L. Sigmoid colon cancer due to Schistosomiasis. Infection 47(6), 1071–1072 (2019).
Houlder, E. L., Costain, A. H., Cook, P. C. & MacDonald, A. S. Schistosomes in the lung: Immunobiology and opportunity. Front Immunol. 12, 635513 (2021).
Hodder, S. L. et al. Predisposition to urinary tract epithelial metaplasia in Schistosoma haematobium infection. Am. J. Trop. Med. Hyg. 63(3–4), 133–138 (2000).
Hotez, P. J., Fenwick, A. & Kjetland, E. F. Africa’s 32 cents solution for HIV/AIDS. PLoS Negl Trop Dis. 3(5), e430 (2009).
Grivennikov, S. I., Greten, F. R. & Karin, M. Immunity, inflammation, and cancer. Cell 140(6), 883–899 (2010).
Zang, M. et al. IL-23 production of liver inflammatory macrophages to damaged hepatocytes promotes hepatocellular carcinoma development after chronic hepatitis B virus infection. Biochim. Biophys. Acta. Mol. Basis Dis. 1864(12), 3759–3770 (2018).
Amieva, M. & Peek, R. M. Jr. Pathobiology of helicobacter pylori-induced gastric cancer. Gastroenterology 150(1), 64–78 (2016).
Jiang, Y. et al. Schistosomiasis may contribute to goblet cell carcinoid of the appendix. J. Parasitol. 98(3), 565–568 (2012).
Lamps, L. W. Infectious causes of appendicitis. Infect. Dis. Clin. North Am. 24(4), 995–1018 (2010).
Katsidzira, L. et al. A case-control study of risk factors for colorectal cancer in an African population. Eur. J. Cancer Prev. 28(3), 145–150 (2019).
Wang, M., Wu, Q., He, W. & Wang, Z. Clinicopathological characteristics and prognosis of schistosomal colorectal cancer. Colorectal. Dis. 18(10), 1005–1009 (2016).
Feng, H. et al. Comparison of non-schistosomal rectosigmoid cancer and schistosomal rectosigmoid cancer. World J. Gastroenterol. 21(23), 7225–7232 (2015).
Probst, A., Schaller, T., Ebigbo, A. & Messmann, H. Colonic schistosomiasis and early rectal cancer: coincidence or causal relationship?. Endoscopy 46(Suppl 1 UCTN), E671 (2014).
Elsaied, N. A., Abbas, A. T., El-Beshbishi, S. N. & Elsheikha, H. M. Increased Helicobacter pylori-associated pathology in outbred mice coinfected with schistosomiasis. Parasitol. Res. 105(2), 297–299 (2009).
Chaves, D. M. et al. Comparative study of portal hypertensive gastropathy in schistosomiasis and hepatic cirrhosis. Endoscopy 34(3), 199–202 (2002).
Joshi, S. S. & Badgwell, B. D. Current treatment and recent progress in gastric cancer. CA Cancer J. Clin. 71(3), 264–279 (2021).
Yan, L. et al. Effect of helicobacter pylori eradication on gastric cancer prevention: Updated report from a randomized controlled trial with 26.5 Years of follow-up. Gastroenterology 163(1), 154-162.e3 (2022).
Bhattacharjee, S. et al. Concomitant Infection of S. mansoni and H. pylori promotes promiscuity of antigen-experienced cells and primes the liver for a lower fibrotic response. Cell Rep. 28(1), 231-244.e5 (2019).
Du, Y. et al. Helicobacter pylori and Schistosoma japonicum co-infection in a Chinese population: helminth infection alters humoral responses to H. pylori and serum pepsinogen I/II ratio. Microbes Infect. 8(1), 52–60 (2006).
Peters, L., Burkert, S. & Grüner, B. Parasites of the liver—epidemiology, diagnosis and clinical management in the European context. J. Hepatol. 75(1), 202–218 (2021).
Hamid, H. K. S. Schistosoma japonicum-associated colorectal cancer: A review. Am. J .Trop. Med. Hyg. 100(3), 501–505 (2019).
Jatzko, G., Kleinert, R. & Denk, H. Die intestinale Schistosomiasis, eine fakultative Präcancerose? Eine Literaturübersicht anlässlich eines Schistosomia japonicum assoziierten Rectumcarcinoms [Intestinal schistosomiasis, a facultative precancerous condition? Review of the literature with reference to Schistosoma japonicum associated rectum carcinoma]. Chirurg 68(7), 727–731 (1997).
Waku, M. et al. Risk of cancer onset in sub-Saharan Africans affected with chronic gastrointestinal parasitic diseases. Int. J. Immunopathol. Pharmacol. 18(3), 503–511 (2005).
Blot, W. J., Devesa, S. S., Kneller, R. W. & Fraumeni, J. F. Jr. Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA 265(10), 1287–1289 (1991).
Okuda, S. et al. Profiling of host genetic alterations and intra-tumor microbiomes in colorectal cancer. Comput. Struct. Biotechnol. J. 19, 3330–3338 (2021).
Chung, Y. et al. A synthetic probiotic engineered for colorectal cancer therapy modulates gut microbiota. Microbiome 9(1), 122 (2021).
Sulżyc-Bielicka, V. et al. Colorectal cancer and Blastocystis sp. infection. Parasit. Vectors 14(1), 200 (2021).
Wang, Z. et al. Comparison of the clinicopathological features and prognoses of patients with schistosomal and nonschistosomal colorectal cancer. Oncol. Lett. 19(3), 2375–2383 (2020).
Wang, Z. et al. Polarization of intestinal tumour-associated macrophages regulates the development of schistosomal colorectal cancer. J. Cancer. 12(4), 1033–1041 (2021).
Author information
Authors and Affiliations
Contributions
Y.Y. and X.-Y.W. wrote manuscripts, and they collected and analyzed data. C.D. and Z.-J.W. completed the experimental section and drew charts. H.-Y.S., X.-L.X., and W.-J.W. corrected the manuscript. J-H.Y. provides research design and article writing ideas. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, Y., Wang, XY., Duan, C. et al. Clinicopathological characteristics and its association with digestive system tumors of 1111 patients with Schistosomiasis japonica. Sci Rep 13, 15115 (2023). https://doi.org/10.1038/s41598-023-42456-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42456-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.