Abstract
The gastrointestinal tract's most commonly occurring primary mesenchymal tumor is the gastrointestinal stromal tumor (GIST). However, few cases worldwide were reported associated with renal cell carcinoma (RCC). Therefore, we aimed to identify the association of genitourinary tumors in patients with GIST in our tertiary care hospital in Saudi Arabia and compare it to the literature. We identified all patients in the pathology department database with the diagnosis of GIST. We excluded duplicate and recurrent cases. We examined patients’ files for the presence of RCC, adrenal tumors, or other genitourinary cancer. A systematic review of the association was conducted. From 2003 to 2020, 170 patients had a histopathologic diagnosis of primary GIST, 100 men and 70 women, median age of 57 (range 9–91) years at the time of diagnosis. The site of primary GIST was gastric 103, small bowel 43, mesenteric 5, omentum/peritoneum 7, abdomen 4, isolated adrenal 1, and other 7. Six patients had associated primary genitourinary cancer. Three patients had RCC (two clear cell RCC and one radiologic diagnosis only), and three had adrenal tumors (one adrenal carcinoma, one an isolated adrenal GIST, and one pheochromocytoma). In addition, two patients had a tumor invading the urinary bladder. Although the cohort included 63 men aged 60 or above (median 71 ± 8.7 years, range 60–94), none demonstrated clinical prostatic carcinoma. Data was compared to 69 systematic review articles. We report the rare association between GIST tumors and primary genitourinary cancer, mainly RCC and adrenal tumors. Also, we identified a secondary invasion of the urinary bladder. Unlike the reported series, none of the older male patients had clinical prostate cancer.
Similar content being viewed by others
Introduction
The most commonly occurring primary mesenchymal tumor in the gastrointestinal tract is a gastrointestinal stromal tumor (GIST). Since the tumor has been molecularly characterized only recently, it is not easy to determine its actual frequency; however, population-based studies suggest that the annual incidence per million population is between 11 and 151. Most GISTs seemingly occur sporadically, but nearly 5% of all GISTs are linked with inheritable mutations or syndromes.
Several studies reported the association between GIST and second primary malignancies. Next to other gastrointestinal tumors, genitourinary (GU) cancer is associated with GIST2,3,4,5,6. In addition, the association is often related to KIT mutations7,8.
The most reported associated primary GU tumors are prostatic adenocarcinoma, renal cell carcinoma (RCC), urothelial cancer, seminoma, and adrenal tumors. Therefore, we set out to identify the prevalence of genitourinary tumors in our hospital patients with histopathological diagnosis of GIST.
Material and methods
This retrospective study included all patients diagnosed with GIST in the pathology department database. The association with RCC and other genitourinary tumors was identified. We defined genitourinary cancer as any cancer involving the kidney, adrenals, urinary bladder, prostate, testis, or penis. We cross-examined the RCC database for the association of GIST. Inclusion criteria included any patient with a histopathologic diagnosis of primary GIST. We excluded duplicate pathology reports of the same patient and cases with GIST recurrences. We excluded tumors of the ovaries and the female genital tract. Descriptive statistics were used. A systematic review literature search was made in Medline/PubMed. The search syntax was generated to combine MeSH terms of “GIST” OR “Gastrointestinal Stromal Tumors” AND MeSH terms of “Neoplasms, Second Primary” OR “Neoplasms, Multiple Primary” OR a text word indicating genitourinary cancer (renal, adrenal, urothelial, bladder, prostatic, OR testicular cancer) OR a genitourinary organ (kidney, adrenal, prostate, urinary bladder, ureter, OR testis). A filter was added restricting the search to the English language and humans.
Ethical approval
This retrospective chart review study involving human participants was following the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments. The Human Investigation Committee (IRB) and Research Ethics Committee of King Faisal Specialist Hospital and Research Center approved this study.
Consent for publication
The Human Investigation Committee (IRB) and Research Ethics Committee of King Faisal Specialist Hospital and Research Center waived the consent because of the study's retrospective nature, and all the procedures being performed were part of the routine care.
Results
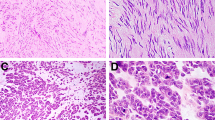
Our patients: From 2003 to 2020, 170 patients had a histopathologic diagnosis of primary GIST, 100 men and 70 women, median age of 57 (range 9–91) years at the time of diagnosis. There were 144 patients with GIST-only tumors (84.7%), 26 with other primary cancer, including six patients with primary genitourinary cancer and two with GIST direct invasion of the urinary bladder (Table 1). Primary GIST was most commonly gastric, spindle cell type, had a low mitotic rate and CD117, DOG1, or both immunostainings. Few cases underwent genetic mutation analysis, and none had genetic counseling. Only one-third of patients were treated with imatinib. Patients with another primary cancer had significantly lower TNM stage and less epithelioid histopathology than GIST-only patients. No significant differences were observed amongst patients with GU vs. no GU cancer.
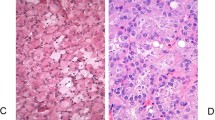
All GIST – GU tumors in our cohort were synchronously discovered during the investigation and treatment of the GU cancer. Two patients had associated clear cell RCC. One tumor was a renal mass with radiological characteristics suggesting papillary RCC (Fig. 1). The tumor was 8 mm in diameter. As there was no indication for surgery, it was followed up by observation with no histological diagnosis. Follow-up CT after two years was consistent with RCC (Fig. 2). Cross-examination of the RCC database retrieved the two histologically proven RCCs. Three cases had adrenal tumors (one adrenal carcinoma, one an isolated adrenal GIST, and one pheochromocytoma). One tumor presented as a urinary bladder mass and was evaluated by transurethral resection. The bladder tumor on histopathology was GIST due to direct invasion from the colon that was not clear on the preoperative radiological diagnosis. Another patient had a urinary bladder invasion by GIST arising from the mesentery.
Radiological diagnosis of RCC in a GIST patient. MRI showing a coronal section of the abdomen with renal lesion (arrows). (a) T1 FS image showing a mild low signal intensity of a right posterior 8 mm renal mass. (b) T2 FS image showing increased intensity of the renal lesion. (c) T1 FS image showing hyperenhancement of the lesion after contrast injection. d. ADC MAP showing diffuse restriction of the lesion.
CT scan of the abdomen at follow up of the same patient after 2 years showing Hounsfield density measurement of the renal tumor consistent with right RCC (arrows). (a) CT without contrast, lesion density 33 ± 13. (b) Arterial phase, the density increased to 138 ± 12. (c) Venous phase the density decreased to 118 ± 13. (d) Delayed phase the density decreased to 94 ± 16.
Of note is that the GIST cohort included 63 male patients who were 60 years or older (median 71 ± 8.7 years, range 60–94). None of them, however, had prostate cancer.
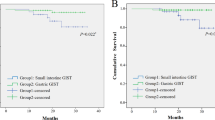
Systematic review: A total of 429 articles were identified, and abstracts were reviewed. Further selection was based on information indicating the presence of GIST in association with genitourinary cancer or organ. Duplicate publications were removed. We found 59 articles meeting the selection criteria and added ten more from references in these articles. A total of 69 articles were reviewed. Seventeen articles reported the prevalence of genitourinary cancer associated with GIST ranging 2.1–15.6% (Table 2)7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23. Prostatic adenocarcinoma was the most common primary genitourinary cancer (2.1–14%), followed by RCC (0.6–11.4%). Rarely seminoma8,11,16,21 and a single case of adrenal neuroblastoma were reported19. Additional 52 articles included case reports of the association (Table 3)2,3,5,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55, or a primary genitourinary organ GIST (Table 4)56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72.
There were 35 case reports of an association between GIST and genitourinary cancer. The most common associations were prostatic cancer (12), adrenal pheochromocytoma (11), and RCC (10). Case reports of primary extra gastrointestinal stromal tumor (EGIST) affecting the genitourinary tract were 17. The most common genitourinary EGIST was affecting the prostate (n = 15). The radiological and pathological evidence suggested that the GIST was not an extension from the adjacent bowel. Two cases were reported from the adrenal; one was from our institution56,57.
Discussion
The number of our patients ranks 9th among the 17 studies reporting the prevalence of GU cancer in GIST patients (Table 2). In contrast, we report a 3.5% association ranking our study among the four least reported associations. The lower rate in our patients is probably related to the absence of prostate cancer compared to others. Series that reported prostate adenocarcinoma had a mean and median age between 65 and 777,9,13,15,16. In our study, 61.3% of men were 60 years or older (Table 5). Those men had a median age of 71 and ranged from 60 to 94. At this age range, we expected to identify some cases of prostate cancer, but we did not find any73. The discrepancy is probably related to the high incidence and prevalence of prostate cancer in USA cancer registries compared to the Saudi and worldwide population (Table 6)74. There is a marked discrepancy in the cancer prevalence of the genitourinary tract74. The prevalence rate per 100,000 population of cancers in the USA is threefold higher than the reported worldwide rate and seven times the Saudi Arabian rate (Table 6). Several factors, like geographical differences in genetic makeup, risk factors, early detection, reporting period, and reporting system, may explain these differences. Of note is that the reported prevalence of prostatic cancer is much higher in patient populations than in the community. For example, in the USA, the prevalence of prostate cancer in the community for men 60 years and above is 1.96%, whereas the corresponding prevalence in the Surveillance, Epidemiology and End Results (SEER) database is 4.8–16.7%73,74. As our report is in a patient cohort rather than a community-based study, we believe that the lack of prostate cancer detection is an actual difference compared to other western countries. These findings may indicate that the association between prostate cancer and GIST is not due to a common risk factor but rather a geographical difference for prostate cancer. Another discrepancy is the absence of primary urothelial cancer in our cohort. Others reported 0.9–2.9% prevalence associated with urothelial cancer8,13,15,16,17,20. This feature is also surprising as urothelial cancer is highly prevalent in Saudi Arabia, comparable to renal cancer (Table 6).
On the other hand, the prevalence of 1.8% of renal cancer is comparable to most studies (0.6–2.2%), except two reporting 4.35% and 11.4%8,12. Out of the three cases, two were CRCC, and the radiological features of the third were suggestive of papillary RCC. This is not surprising as papillary RCC prevalence in GIST patients is much proportionally higher14,23. The GISTs in our GU cancer patients were incidental during planned nephrectomy or adrenalectomy. The incidental GIST was small but otherwise pathologically comparable to GIST with no associated GU cancer (Table 1). No genetic analysis was available to link the two pathologies. Clinically, however, none of our patients had VHL or NF-1 disease.
Other unique features of this study involve a rarely reported association with adrenal tumors. Of interest is the primary GIST of the adrenal gland. There is only one reported adrenal EGIST other than the one reported from our institution (Table 4)56,57. There is no radiological evidence that the adrenal GIST was a direct or distant spread of another primary GIST lesion. We also report two adrenal tumors, one carcinoma, and the other pheochromocytoma, none reported in the reviewed prevalence series (Table 2). However, sporadic cases of 11 pheochromocytomas were reported and most associated with NF1, unlike our patient (Table 3). There is only one adrenal carcinoma case report in addition to the one in our series (Table 3)35. Rarely was urothelial cancer reported in association with GIST (Table 2). Although one case presented as a bladder tumor, unlike the other reports, the two bladder tumors we report were secondary to direct invasion of a primary intestinal GIST. In addition, unlike the reports, we did not find associated testicular tumors. The strong point of this study is that it includes a large cohort of patients with histopathology-proven GIST comparable to large international series. In addition, it highlights prevalence differences unique to our geographical location. The study's weakness is that it did not include molecular and genetic profiling of the tumors and its retrospective design.
Conclusion
We report the rare association between GIST tumors and primary genitourinary cancer, mainly RCC and adrenal tumors. Also, we identified a secondary invasion of the urinary bladder. Unlike the reported series, none of the older male patients had clinical prostate cancer.
Data availability
Data generated or analyzed during this study are included in the supplementary file.
References
Nilsson, B. et al. Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era–a population-based study in western Sweden. Cancer 103, 821–829 (2005).
Jiang, Q. et al. A novel germline mutation in SDHA identified in a rare case of gastrointestinal stromal tumor complicated with renal cell carcinoma. Int. J. Clin. Exp. Pathol. 8, 12188–12197 (2015).
Gill, A. J. et al. Germline SDHC mutation presenting as recurrent SDH deficient GIST and renal carcinoma. Pathology (Phila.) 45, 689–691 (2013).
Torous, V. F., Su, A., Lu, D. Y. & Dry, S. M. Adult patient with synchronous gastrointestinal stromal tumor and Xp11 translocation-associated renal cell carcinoma: a unique case presentation with discussion and review of literature. Case Rep. Urol. 2015, 814809 (2015).
Dasanu, C. A., Jethava, A., Ali, S. & Codreanu, I. Gastrointestinal stromal tumor of small intestine and synchronous bilateral papillary renal cell carcinoma. Conn. Med. 77, 405–407 (2013).
Karlidag, I. et al. A rare case of renal gastrointestinal stromal tumor. Urol. Case Rep. 24, 100881 (2019).
Hechtman, J. F. et al. Additional primary malignancies in patients with gastrointestinal stromal tumor (GIST): a clinicopathologic study of 260 patients with molecular analysis and review of the literature. Ann. Surg. Oncol. 22, 2633–2639 (2015).
Mayr, P. et al. Malignancies associated with GIST: a retrospective study with molecular analysis of KIT and PDGFRA. Langenbecks Arch. Surg. 404, 605–613 (2019).
Szczepaniak, K. & Nasierowska-Guttmejer, A. The occurrence of gastrointestinal stromal tumors with second malignancies—Case series of a single institution experience. Pathol. Res. Pract. 228, 153662 (2021).
Shen, C. et al. Long-term survival among patients with gastrointestinal stromal tumors diagnosed after another malignancy: A SEER population-based study. World J. Surg. Oncol. 18, 88 (2020).
Comandini, D. et al. Gastrointestinal stromal tumors and second primary malignancies: a retrospective monocentric analysis. Neoplasma 67, 1416–1423 (2020).
Petrelli, F. et al. Risk of second primary tumors in GIST survivors: A systematic review and meta-analysis. Surg. Oncol. 29, 64–70 (2019).
Fernández, J. A. et al. Additional malignancies in patients with gastrointestinal stromal tumors (GIST): incidence, pathology and prognosis according to a time of occurrence-based classification. Clin. Transl. Oncol. Off. Publ. Fed. Span. Oncol. Soc. Natl. Cancer. Inst. Mex. 21, 646–655 (2019).
Mendonca, S. J. et al. The association of renal cell carcinoma with gastrointestinal stromal tumors. J. Surg. Oncol. 117, 1716–1720 (2018).
Aghdassi, A. et al. Gastrointestinal stromal tumors: Clinical symptoms, location, metastasis formation, and associated malignancies in a single center retrospective study. Dig. Dis. Basel Switz. 36, 337–345 (2018).
Kramer, K. et al. Frequence, spectrum and prognostic impact of additional malignancies in patients with gastrointestinal stromal tumors. Neoplasia N. Y. N 17, 134–140 (2015).
Murphy, J. D. et al. Increased risk of additional cancers among patients with gastrointestinal stromal tumors: A population-based study. Cancer 121, 2960–2967 (2015).
Vassos, N., Agaimy, A., Hohenberger, W. & Croner, R. S. Coexistence of gastrointestinal stromal tumours (GIST) and malignant neoplasms of different origin: prognostic implications. Int. J. Surg. Lond. Engl. 12, 371–377 (2014).
Gonçalves, R. et al. Occurrence of other tumors in patients with GIST. Surg. Oncol. 19, e140-143 (2010).
Pandurengan, R. K. et al. Survival of patients with multiple primary malignancies: a study of 783 patients with gastrointestinal stromal tumor. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 21, 2107–2111 (2010).
Agaimy, A., Wünsch, P. H., Sobin, L. H., Lasota, J. & Miettinen, M. Occurrence of other malignancies in patients with gastrointestinal stromal tumors. Semin. Diagn. Pathol. 23, 120–129 (2006).
Agaimy, A. & Wuensch, P. H. Gastrointestinal stromal tumours in patients with other-type cancer: a mere coincidence or an etiological association? A study of 97 GIST cases. Z. Gastroenterol. 43, 1025–1030 (2005).
Au, W. Y., Ho, K. M. & Shek, T. W. Papillary renal cell carcinoma and gastrointestinal stromal tumor: a unique association. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 15, 843–844 (2004).
Arif, A. A. et al. Pancreatic gastrinoma, gastrointestinal stromal tumor (GIST), pheochromocytoma, and hürthle cell neoplasm in a patient with neurofibromatosis Type 1: A case report and literature review. Am. J. Case Rep. 22, e927761 (2021).
Vongsumran, N., Kongkarnka, S., Watanawittawas, P. & Manosroi, W. Pheochromocytoma and gastrointestinal stromal tumours in an adult neurofibromatosis type 1 patient: A rare co-occurrence. BMJ Case Rep. 13, e235129 (2020).
Gorgel, A. et al. Coexistence of gastrointestinal stromal tumors (GISTs) and pheochromocytoma in three cases of neurofibromatosis type 1 (NF1) with a review of the literature. Intern. Med. Tokyo Jpn. 53, 1783–1789 (2014).
Vlenterie, M. et al. Pheochromocytoma and gastrointestinal stromal tumors in patients with neurofibromatosis type I. Am. J. Med. 126, 174–180 (2013).
Carşote, M. et al. The immunohistochemistry aspects in two cases of neurofibromatosis-associated abdominal tumors. Romanian J. Morphol. Embryol. Rev. Roum. Morphol. Embryol. 53, 401–405 (2012).
Boguszewski, C. L. et al. Genetic studies in a coexistence of acromegaly, pheochromocytoma, gastrointestinal stromal tumor (GIST) and thyroid follicular adenoma. Arq. Bras. Endocrinol. Metabol. 56, 507–512 (2012).
Hataya, Y. et al. A case of neurofibromatosis type 1 coinciding with bilateral pheochromocytomas, multiple gastrointestinal stromal tumors, and malignant peripheral nerve sheath tumor. Intern. Med. Tokyo Jpn. 51, 1531–1536 (2012).
Kramer, K., Hasel, C., Aschoff, A. J., Henne-Bruns, D. & Wuerl, P. Multiple gastrointestinal stromal tumors and bilateral pheochromocytoma in neurofibromatosis. World J. Gastroenterol. 13, 3384–3387 (2007).
Teramoto, S. et al. Two von Recklinghausen’s disease cases with pheochromocytomas and gastrointestinal stromal tumors (GIST) in combination. Int. J. Urol. Off. J. Jpn. Urol. Assoc. 14, 73–74 (2007).
Nemoto, H. et al. Novel NF1 gene mutation in a Japanese patient with neurofibromatosis type 1 and a gastrointestinal stromal tumor. J. Gastroenterol. 41, 378–382 (2006).
Bümming, P., Nilsson, B., Sörensen, J., Nilsson, O. & Ahlman, H. Use of 2-tracer PET to diagnose gastrointestinal stromal tumour and pheochromocytoma in patients with Carney triad and neurofibromatosis type 1. Scand. J. Gastroenterol. 41, 626–630 (2006).
Kovecsi, A. et al. First case report of a sporadic adrenocortical carcinoma with gastric metastasis and a synchronous gastrointestinal stromal tumor of the stomach. Medicine (Baltimore) 94, e1549 (2015).
Tansir, G. et al. Carney’s triad in an adult male from a tertiary care center in India: a case report. J. Med. Case Rep. 15, 559 (2021).
Huang, Y.-C., Wang, J.-Y., Lin, P.-Y., Chin, C.-C. & Chen, C.-S. Synchronous prostate stromal sarcoma and gastrointestinal stromal tumor of rectum: Case report and review of the literature. Urology 68(672), e11-13 (2006).
Wei, S.-C., Li, W.-H., Xu, L. & Li, W.-W. Malignant jejunal gastrointestinal stromal tumor with history of prostate cancer: A case report. Medicine (Baltimore) 98, e15332 (2019).
Watanabe, R., Ozawa, A., Iseda, T. & Hatano, H. A case report of synchronous prostate cancer and rectal gastrointestinal stromal tumor and its management. Urol. J. 16, 322–325 (2019).
Przybylik-Mazurek, E. et al. Coexistence of neurofibromatosis type 1 with multiple malignant neoplasia. Neuro Endocrinol. Lett. 39, 149–155 (2018).
Laurens, S. T., Witjes, F., Janssen, M., Flucke, U. & Gottardt, M. 68Ga-prostate-specific membrane antigen uptake in gastrointestinal stromal tumor. Clin. Nucl. Med. 43, 60–61 (2018).
Rebegea, L. F., Pătraşcu, A., Miron, D., Dumitru, M. E. & Firescu, D. Metachronous gastrointestinal stromal tumor associated with other neoplasia - case presentation. Romanian J. Morphol. Embryol. Rev. Roum. Morphol. Embryol. 57, 1429–1435 (2016).
Healy, C. F., Ferguson, D., Mohammed, M. F., Waterhouse, J. & Harris, A. C. An unusual ‘collision tumour’ of the prostate gland and rectum. Can. J. Gastroenterol. Hepatol. 2016, 7486473 (2016).
Waisbren, J., Uthe, R., Siziopikou, K. & Kaklamani, V. BRCA 1/2 gene mutation and gastrointestinal stromal tumours: a potential association. BMJ Case Rep. 2015, (2015).
Macías-García, L. et al. Collision tumour involving a rectal gastrointestinal stromal tumour with invasion of the prostate and a prostatic adenocarcinoma. Diagn. Pathol. 7, 150 (2012).
Engin, H. & Ustündağ, Y. Coexistence of prostate cancer and colorectal cancer in a patient with gastrointestinal stromal tumor. Turk. J. Gastroenterol. Off. J. Turk. Soc. Gastroenterol. 20, 231–232 (2009).
Yaman, E. et al. Coexistence of gastrointestinal stromal tumor (GIST) of the rectum and adenocarcinoma of the prostate in a patient with familial GIST. Onkologie 31, 697–699 (2008).
Kalender, M. E. et al. Gastric and prostate adenocarcinoma in a patient with metastatic gastrointestinal stromal tumor. Onkologie 30, 568–570 (2007).
Miettinen, M. et al. Mapping of succinate dehydrogenase losses in 2258 epithelial neoplasms. Appl. Immunohistochem. Mol. Morphol. AIMM 22, 31–36 (2014).
Omeroglu, S., Gulmez, S. & Bozkurt, E. The first case: acute abdomen due to gastric gastrointestinal stromal tumor perforation with synchronous renal cell carcinoma. Ann. Ital. Chir. 11, S2239253X22038117 (2022).
Juric, I. & Basic-Jukic, N. Multiple primary malignancies: The first case of a combination of a gastrointestinal stromal tumor and renal cell carcinoma in a kidney transplant recipient. Transplant. Proc. 51, 3070–3071 (2019).
Reşorlu, B., Baltaci, S., Reşorlu, M., Kankaya, D. & Savaş, B. Coexistence of papillary renal cell carcinoma and gastrointestinal stromal tumor in a case. Turk. J. Gastroenterol. Off. J. Turk. Soc. Gastroenterol. 18, 47–49 (2007).
Lim, J. C. & Wojcik, E. M. Fine-needle aspiration cytology of papillary renal cell carcinoma: the association with concomitant secondary malignancies. Diagn. Cytopathol. 34, 797–800 (2006).
Jawiarczyk-Przybyłowska, A. et al. Acromegaly associated with GIST, non-small cell lung carcinoma, clear cell renal carcinoma, multiple myeloma, medulla oblongata tumour, adrenal adenoma, and follicular thyroid nodules. Endokrynol. Pol. 70, 213–217 (2019).
Tao, J. et al. The coexistence of clear cell renal cell carcinoma and gastrointestinal stromal tumor with portal vein metastasis, and its favorable response to sunitinib. Expert Rev. Anticancer Ther. 13, 131–136 (2013).
Abou Al-Shaar, H., Solimanie, S., Azzam, A., Amin, T. & Abu-Zaid, A. Gastrointestinal stromal tumor of the adrenal gland:a case report and review of the literature. Endocr. Pathol. 26, 27–32 (2015).
Sereg, M. et al. Gastrointestinal stromal tumor presenting as a hormonally inactive adrenal mass. Endocrine 39, 1–5 (2011).
Li, L. et al. Current knowledge of primary prostatic extra-gastrointestinal stromal tumor: a case report and review of the literature. J. Int. Med. Res. 49, 3000605211013172 (2021).
Shen, H. et al. Primary prostatic extra-gastrointestinal stromal tumor treated with imatinib mesylate as neoadjuvant and adjuvant therapy: A case report and literature review. OncoTargets Ther. 12, 11549–11553 (2019).
Alabed, Y. Z. Gastrointestinal stromal tumor of the prostate: Staging and evaluation of response to therapy with 18F-FDG PET/CT. Clin. Nucl. Med. 43, 52–54 (2018).
You, Y.-H. & Zhang, Y. Primary prostatic extragastrointestinal stromal tumor: a case report and literature review. J. Int. Med. Res. 46, 4343–4349 (2018).
Etit, D., Kar, H., Ekinci, N., Yenipazar, A. E. & Çakalağaoğlu, F. Extra-gastrointestinal stromal tumor of prostate. Balk. Med. J. 34, 168–171 (2017).
Liu, Y. & Xu, B. Primary prostatic extragastrointestinal stromal tumor on 18F-FDG PET/CT. Clin. Nucl. Med. 41, 224–226 (2016).
Huh, J.-S., Park, K. K., Kim, Y. J. & Kim, S. D. Diagnosis of a gastrointestinal stromal tumor presenting as a prostatic mass: A case report. World J. Mens Health 32, 184–188 (2014).
Liu, S. et al. Primary gastrointestinal stromal tumor of the prostate: A case report and literature review. Oncol. Lett. 7, 1925–1929 (2014).
Zhou, J. & Teng, X. Primary extragastrointestinal stromal tumor of the prostate: a case report. Anal. Quant. Cytopathol. Histopathol. 36, 55–60 (2014).
Zhang, Z.-H. et al. A young man with primary prostatic extra-gastrointestinal stromal tumor: a rare case report and review of the literature. Int. J. Clin. Exp. Pathol. 7, 1764–1770 (2014).
Ou, Z., Cao, Z., He, Y. & Tang, D. Diagnosis and multimodal therapy for extragastrointestinal stromal tumor of the prostate: A case report. Exp. Ther. Med. 6, 378–380 (2013).
Loeb, S., Lotan, T. L., Thornton, K., Gearhart, S. L. & Schoenberg, M. P. A case of gastrointestinal stromal tumor diagnosed on prostate biopsy. Nat. Clin. Pract. Urol. 6, 54–57 (2009).
Yinghao, S., Bo, Y. & Xiaofeng, G. Extragastrointestinal stromal tumor possibly originating from the prostate. Int. J. Urol. Off. J. Jpn. Urol. Assoc. 14, 869–871 (2007).
Lee, C.-H., Lin, Y.-H., Lin, H.-Y., Lee, C.-M. & Chu, J.-S. Gastrointestinal stromal tumor of the prostate: a case report and literature review. Hum. Pathol. 37, 1361–1365 (2006).
Van der Aa, F. et al. Gastrointestinal stromal tumor of the prostate. Urology 65, 388 (2005).
Noone, A. M. et al. (eds). SEER Cancer Statistics Review, 1975–2015, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2015/, based on November 2017 SEER data submission, posted to the SEER web site (2018).
Ferlay, J., et al. (2020). Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. https://gco.iarc.fr/today, accessed (28 April 2022).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. The first draft of the manuscript was written by R.S., and all authors commented on previous versions. All authors read and approved the final manuscript. R.S., T.M.A., and W.A. did the study conception and design. K.A.C., A.A., A.A., O.A., A.G.S., M.A., R.A.A., A.Al-G., and T.Al-H. performed the acquisition of data. R.S., T.Al-H., T.M.A., and W.A. analyzed and interpreted the data. R.S. and W.A. drafted the manuscript and performed its critical revision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seyam, R., Chaer, K.A., Abouelkhair, A. et al. The association of genitourinary cancer among Saudi patients with gastrointestinal stromal tumors and a systematic literature review. Sci Rep 13, 4325 (2023). https://doi.org/10.1038/s41598-023-28060-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-28060-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.