Abstract
One feature of hypertension is a microbial imbalance with increased intestinal permeability. In this study, we examined whether an alteration in the microbiota affects blood pressure and intestinal permeability in spontaneously hypertensive rats (SHRs). We performed a 16S metagenome analysis of feces from 10- to 15-week-old SHRs using a synthetic long-read sequencing approach, and found a candidate for the microbiome treatment, Ligilactobacillus murinus (L. murinus), that was robustly decreased. Oral administration of L. murinus to SHRs for 2 weeks significantly inhibited blood pressure elevation and improved endothelium-dependent vasodilation but did not attenuate enhanced vascular contraction in SHR mesenteric arteries. The proximal colon of SHRs exhibited increased intestinal permeability with decreased levels of the tight junction protein claudin 4, morphological changes such as decreased intestinal crypts and elevated TNF-α levels, which was reversed by treatment with L. murinus. Consistent with these intestinal phenotypes, plasma lipopolysaccharides levels were elevated in SHR but decreased following L. murinus administration. We concluded that oral administration of L. murinus to SHRs exerts protective effects on intestinal permeability via restoration of claudin 4 expression and reversal of morphologic disorder, which may improve low-grade endotoxemia and thus reduce development of hypertension via recovery of endothelial vasodilating functions.
Similar content being viewed by others
Introduction
Microbiome research has made significant recent progress and generated worldwide focus and attention. Accumulating evidence indicates that the microbiota plays important roles in physiological and pathological events in the host. For instance, the gut microbiome regulates not only host nutrients but also the immune system to protect against infection1. A significant relationship exists between gut microbial imbalances and gastrointestinal, metabolic, immune, cardiovascular, psychiatric, and developmental diseases2, 3. Additional research is thus required to obtain an in-depth understanding of health and disease in the context of the gut microbiome.
Hypertension is the most common risk factor for cardiovascular disease4, and several recent studies have suggested a link between cardiovascular disease and gut dysbiosis5. For example, transplantation of fecal microbiota from a hypertensive human donor to germ-free mice was shown to cause blood pressure elevation6. Consistent with this observation, angiotensin II-induced hypertension and vascular dysfunction are attenuated in germ-free mice7, suggesting that the gut microbiota can cause or accelerate the development of hypertension.
Additionally, in cases of hypertension with dysbiosis, the intestinal permeability is disrupted8. Increased intestinal permeability allows allergens and pathogens to penetrate the intestinal barrier and stimulate the immune system9. Symptoms associated with increased intestinal permeability are observed in diverse diseases, from inflammatory bowel disorder to infection, cancer, and metabolic disease10,11,12. Accumulating evidence has demonstrated that hypertension, cardiac infarction, and atherosclerosis are also associated with a breakdown in intestinal barrier function13,14,15. Thus, normalization of an imbalance in the gut microbiota and restoration of intestinal permeability are novel research topics in the context of non-gastrointestinal diseases, and such research could lead to the identification of a new class of therapeutic targets for treating cardiovascular disease.
In the present study, we examined whether treatment of spontaneous hypertensive rats (SHRs) with gut microbiota organisms has an effect on blood pressure and intestinal permeability. We found that oral administration of Ligilactobacillus murinus (L. murinus) to SHRs for 2 weeks rescued defective vascular endothelial function and lowered blood pressure in the rats and also decreased plasma lipopolysaccharide (LPS) levels. We also found that L. murinus administration strengthened the intestinal barrier system in the proximal colon by upregulating tight junction proteins.
Results
Ratio of L. murinus was decreased in feces of SHRs
Feces from 10- to 15-week-old SHRs and WKY rats were examined by 16S metagenome analysis using a synthetic long-read sequencing LoopSeq approach. The analysis revealed that the rations of two different species of the microbiome, L. murinus and Akkermansia muciniphilla, were decreased in SHRs compared with WKY rats. The analysis also showed that Bacteroides caecimuris and Bacteroides thetaiotaomicron were increased in SHRs. We confirmed that one of the characteristic phenotypes, Firmicutes/Bacteroidetes ratio was significantly increased in SHR compared with WKY. These data are shown in Supplementary Fig. 1 online.
Treatment with L. murinus lowered blood pressure and improved vascular endothelial function in SHRs
Because L. murinus was relatively easily handled, we determined whether restoration of L. murinus affected blood pressure in SHR. We first attempted to isolate L. murinus from feces of 10- to 15-week-old WKY rats. Nine strains of 48 candidates were identified as L. murinus by PCR using species-specific primer sets (Supplementary Fig. 2). 16S rRNA sequences of the nine strains showed 99.9% identity to the sequence of L. murinus NBRC 14221 (type strain). These isolated strains were designated Ligilactobacillus murinus WO strains (WO9, WO17, WO22, WO28, WO29, WO32, WO39, WO46 and WO48) and divided into three groups by ERIC-PCR. The band patterns of the strains in ERIC-PCR analyses clearly differed from the band pattern of NBRC 14221 (Supplementary Fig. 3).
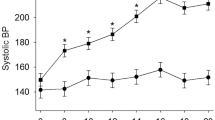
We then administered L. murinus (as an equal mixture of WO strains, approximately 1 × 108 CFU/mL) to 10- to 15-week-old SHRs orally every day for 2 weeks. Preliminary analyses confirmed an increase in systolic blood pressure (Fig. 1A). Although L. murinus orally administered for 2 weeks did not affect the body weight of 10- to 15-week-old SHRs (Supplementary Fig. 4A), the elevation in blood pressure was significantly reversed (Fig. 1B,C and Supplementary Fig. 4B). However, treatment with L. murinus did not affect heart rate or the increase in heart weight of SHRs (Supplementary Fig. 4C–G).
Blood pressure and vascular function in untreated SHRs and SHRs treated with Ligilactobacillus murinus (L. murinus). (A,B) Systolic blood pressure (SBP) measured via tail-cuff plethysmography in 10- to 15-week-old WKY rats and SHRs (A) or SHRs + Control and SHRs + L. murinus (B). (C) SBP was measured for 14 days after initiation of treatment with Control or L. murinus (arrow) in SHRs. (D–I) Isometric tension experiments were performed using 2nd-branch mesenteric artery in WKY rats, SHRs, SHRs + Control and SHRs + L. murinus. Cumulative concentration–response curves for acetylcholine (ACh, 1 nM–30 μM) in mesenteric arteries from WKY rats and SHRs (n = 8 per group) (D) and SHRs + Control and SHRs + L. murinus (n = 6 per group) (E). Cumulative concentration–response curves for sodium nitroprusside (SNP, 0.1 nM–3 μM) in mesenteric arteries from WKY and SHR (n = 8 per group) (F) and SHR + Control and SHR + L. murinus (n = 6 per group) (G). Cumulative concentration–response curves for 5-HT (10 nM–30 μM) in mesenteric arteries from WKY rats and SHRs (n = 8 per group) (H) and SHRs + Control and SHRs + L. murinus (n = 6 per group) (I). All data are mean ± SEM. *P < 0.05 vs. WKY rats or day 0, #P < 0.05 vs. SHRs + Control.
We next examined vascular functions in SHRs before and after administration of L. murinus. We observed that ACh-induced endothelium-dependent relaxation was impaired in mesenteric arteries of SHRs, and this was significantly reversed by L. murinus treatment (Fig. 1D and E). There was no difference in sodium-nitroprusside-induced, endothelium-independent relaxation in any of the groups (Fig. 1F and G). In contrast, vascular contraction in response to 5-HT was increased in SHRs, and this was not affected by L. murinus (Fig. 1H and I).
Increased intestinal permeability in SHR proximal colon was improved by L. murinus
Next, we examined whether L. murinus affects the integrity of the gut epithelial barrier in SHRs. Adult SHRs (10–15 weeks old) showed altered intestinal permeability in the proximal colon compared with age-matched WKY rats, but no change in permeability of the ileum was observed (Fig. 2A–H). Treatment with L. murinus for 2 weeks lowered the permeability of the proximal colon, suggesting that L. murinus exerts a protective effect on the intestinal epithelium. We then determined the expression levels of tight junction proteins in SHRs. The expression levels of claudin 4, occludin, cingulin, and ZO-1 were decreased in the proximal colon of SHRs compared with the proximal colon of WKY rats (Fig. 3A and B and Supplementary Figs. 5 and 6). There were no changes in the expression levels of tight junction proteins in the ileum of 10-to 15-week-old SHRs (Supplementary Figs. 7 and 8). Administration of L. murinus significantly increased claudin 4 expression but not that of other tight junction proteins. Immunostaining data showed a decrease in claudin 4 expression in the proximal colon intestinal epithelium of SHRs, which was reversed by L. murinus (Fig. 3C).
Intestinal permeability in untreated SHRs and SHRs treated with L. murinus. (A–D) Apparent permeability of the ileum of 10- to 15-week-old WKY rats and SHRs (A,C) (n = 4 per group) or SHRs + Control and SHRs + L. murinus (B,D) (n = 5 per group) was measured using the non-everted gut sac exam with 4-kDa (A,B) or 70-kDa FITC (C,D). (E–H) Apparent permeability of the proximal colon of 10- to 15-week-old WKY rats and SHRs (E,G) (n = 4 per group) or SHRs + Control and SHRs + L. murinus (F,H) (n = 5 per group) was measured using the non-everted gut sac exam with 4-kDa (E,F) or 70-kDa FITC (G,H). All data are mean ± SEM. *P < 0.05 vs. WKY rats, #P < 0.05 vs. SHRs + Control.
Tight junction proteins in untreated SHRs and SHRs treated with L. murinus. (A,B) Western blotting analysis of indicated proteins (representative of 8–10 experiments) in the proximal colon of 10- to 15-week-old WKY rats and SHRs (n = 8 per group) or SHRs + Control and SHRs + L. murinus (n = 10 per group). Representative (A) and quantified (B) Western blots for claudin 4, occludin, cingulin, ZO-1, and ZO-2. (C) Immunostaining analysis of claudin 4 (representative of 4–5). All data are mean ± SEM. *P < 0.05 vs. WKY rats, #P < 0.05 vs. SHRs + Control. Scale bar: 50 μm.
L. murinus ameliorated changes in the intestinal morphology of SHRs
We examined the effect of L. murinus on intestinal morphology in SHRs. Adult SHRs exhibited a decrease in intestinal crypts in the proximal colon (Fig. 4A and B), but there were no pronounced changes in the duodenum, jejunum, or ileum (Supplementary Fig. 9). The number of goblet cells in the proximal colon was slightly decreased in SHRs compared with WKY rats, but the difference was not significant (Supplementary Fig. 10). Treatment with L. murinus restored the intestinal crypts compared with the control group (Fig. 4A–C). Real-time PCR analysis revealed significant decreases in mRNA levels of mucin 2, mucin 1, and leucine-rich repeat containing G protein-coupled receptor (LGR)5 (Fig. 4D–I). In addition, a decreasing trend in telomerase reverse transcriptase (Tert) expression was observed in SHR proximal colon (Supplementary Fig. 11A and B). No change in mucin 4 expression was observed in SHRs (Supplementary Fig. 11C and D). The expression of these genes was not altered by treatment with L. murinus.
Changes in morphology of the proximal colon of SHRs and SHRs treated with L. murinus. (A) The proximal colon was sectioned and stained with hematoxylin and eosin or PAS to examine intestinal crypts. (B,C) Intestinal crypts in proximal colon of 10- to 15-week-old WKY rats and SHRs (B) (n = 5 per group) or SHRs + Control and SHRs + L. murinus (C) (n = 4–5 per group) were measured. Quantitative PCR analysis of mucin 2 (D,E), mucin 1 (F,G), and leucine-rich repeat containing G protein-coupled receptor 5 (Lgr5) (H,I) in proximal colon of 10- to 15-week-old WKY rats and SHRs (n = 8 per group) or SHRs + Control and SHRs + L. murinus (n = 8 per group). All data are mean ± SEM. *P < 0.05 vs. WKY rats, #P < 0.05 vs. SHRs + Control. White scale: 100 μm, black scale: 25 μm.
Gut inflammation in SHRs was attenuated by L. murinus
We next investigated the effect of L. murinus administration on immunologic properties in SHRs. The mRNA level of TNF-α was significantly increased in proximal colon in 10- to 15-week-old SHRs (Fig. 5A). Treatment with L. murinus decreased the expression levels of TNF-α (Fig. 5B). In contrast, no differences in the expression of the toll-like receptor 2 (TLR2), TLR4, transforming growth factor β (TGF-β), CD3, and CD68 genes were observed between the WKY and SHR groups (Fig. 5C–L).
Inflammatory cytokines, toll-like receptors (TLRs), and inflammatory cells in the proximal colon of WKY rats, SHRs, and SHRs treated with L. murinus. Quantitative PCR analysis of tumor necrosis factor (TNF)-α (A,B), transforming growth factor (TGF)-β (C,D),TLR2 (E,F), TLR4 (G,H), CD3 (I,J), and CD68 (K,L) in the proximal colon of 10- to 15-week-old WKY rats and SHRs (n = 8 per group) or SHRs + Control and SHRs + L. murinus (n = 8 per group). All data are mean ± SEM. *P < 0.05 vs. WKY rats, #P < 0.05 vs. SHRs.
T helper 17 cells (Th17) and type 1 helper cells (Th1) are associated with the development of hypertension and cardiovascular target-organ damage, but regulatory T cells (Tregs) exert anti-inflammatory effects16. We therefore examined whether these immune cells are involved in gut inflammation in 10- to 15-week-old SHRs using flow cytometry analysis with a specific gating strategy (Supplementary Fig. 12). No changes in total T lymphocytes (CD4+CD45+), Tregs (CD4+FoxP3+), Th1 cells (CD4+INFγ+), or Th17 cells (CD4+IL17+) were observed in SHR lymph nodes (Supplementary Fig. 13A–E) and spleen (Supplementary Fig. 13F–I) compared with age-matched WKY rats.
Plasma endotoxin levels were decreased by L. murinus
LPS exposure induces endothelial dysfunction and vascular inflammation, and human studies have shown that plasma levels of LPS are positively correlated with hypertension17. We therefore examined whether L. murinus affects LPS levels in SHRs. Plasma levels of LPS were increased in SHRs, and administration of L. murinus reversed this increase (Fig. 6).
Plasma levels of endotoxin in untreated SHRs and SHRs treated with L. murinus. Plasma levels of lipopolysaccharide (LPS) in WKY rats and SHRs (A) (n = 6 per group) or SHRs + Control and SHRs + L. murinus (B) (n = 6 per group). All data are mean ± SEM. *P < 0.05 vs. WKY rats, #P < 0.05 vs. SHRs + Control.
Discussion
Accumulating evidence indicates that dysbiosis is strongly associated with the development of cardiovascular diseases, including hypertension. However, the pathophysiologic mechanism by which an imbalance in the gut microbiota causes hypertension remains unclear. In this study, we focused on determining whether treatment to reverse a decrease in specific microbiota affects the gut environment and cardiovascular system in hypertensive rats. The main findings of our study are as follows: (1) two different species of microbiota were markedly decreased in 10- to 15-week-old SHRs; (2) treatment with L. murinus for 2 weeks ameliorated the disruption of intestinal barrier function in the proximal colon via increased claudin 4 expression; (3) morphological changes with TNF-α expression in the proximal colon were improved in SHRs treated with L. murinus; and (4) vascular dysfunction and blood pressure elevation were reversed with decreasing in plasma levels of endotoxin by L. murinus administration. These results support the hypothesis that an imbalance in the gut microbiota is related to the development of hypertension.
Increased intestinal permeability with dysbiosis is observed in several diseases and conditions, including obesity, aging, infection, and cancer18. In addition, several reports indicated that hypertensive model exhibited increased intestinal permeability and morphological changes8, 19, 20. In this study, we observed an increase in intestinal permeability in the proximal colon with decreased expression of tight-junction proteins (claudin 4, occludin, cingulin, and ZO-1) in hypertensive model rats. It is notable that the increase in intestinal permeability was reversed with increased claudin 4 expression by administration of L. murinus. Claudin 4 regulates the paracellular sodium barrier and is expressed in various organs, including the intestine (colon), kidney, and lung21. Deletion of claudin 4 reportedly increases susceptibility to lung injury22. It is notable that short-chain fatty acids such as acetate reportedly increase claudin 4 expression in intestinal epithelial cells23. These findings suggest that metabolites of L. murinus increase the expression of claudin 4 in the proximal colon, resulting in improved intestinal barrier function.
Consistent with the change in gut permeability, morphological changes were also observed in hypertensive model rats. The most notable and reproducible phenotype of SHRs was decreased intestinal crypts, which consist of the intestinal epithelium and villi. Crypt-villus tissue, which continuously proliferates, enables the intestine to act as a barrier and also serves as the primary site of nutrient uptake24. However, chronic NF-κB activation by TNF-α was shown to reduce intestinal crypts via apoptosis in inflammatory bowel disease25. In our study, the proximal colon in SHRs exhibited decreased expression of stem cell markers (LGR5 and Tert) and mucus markers (MUC1, 2, 4). In addition, TNF-α expression was increased in hypertensive model rats, and this was reversed by treatment with L. murinus. Pronounced morphological changes were observed in the proximal colon but not the duodenum, jejunum, or ileum of 10- to 15-week-old SHRs.
Host immune cells in the gut interact with the microbiome to regulate systemic immune responses. Numerous studies have shown that cells of the innate and adaptive immune systems play important roles in the development of hypertension16. In particular, activation of Th17 and Th1 cells is strongly associated with the development of hypertension26, 27, whereas Tregs exert an anti-inflammatory effect on the cardiovascular system via production of IL-1028. Unexpectedly, the present study found no significant differences in these immune cells in intestinal lymph nodes and spleen between 10- to 15-week-old SHRs and the relatively young adult age-matched WKY rats. These results suggest that the immune response might play a more important role in the middle to late stages of the development of hypertension in SHRs.
Some studies have proposed that gut-derived, low-grade endotoxemia is a risk factor for cardiovascular events29. In gut dysbiosis, LPS, a component of gram-negative bacteria in the gut, enters the circulation due to dysfunction in the intestinal barrier scaffolding, leading to low-grade inflammation in several cell types, including endothelial cells and leukocytes. Activation of TLR4 signaling due to LPS causes systemic inflammation, including vascular endothelial dysfunction, by increasing the production of reactive oxidative stress and activating NF-κB signaling. Consistent with current hypotheses, a hypertensive model showed elevated plasma endotoxin levels with increased intestinal permeability20. In addition, TLR4 inhibition was shown to alleviate hypertension and vascular dysfunction in animal models30, 31. In our study, 10- to 15-week-old SHRs exhibited increased plasma levels of LPS along with increased intestinal permeability and vascular endothelial dysfunction. Importantly, treatment with L. murinus significantly reduced the LPS level in SHRs, suggesting that administration of probiotics improves the intestinal environment and therefore could be a candidate therapeutic approach for treating hypertension.
Mice with high salt intake reportedly exhibit a decrease in the abundance of L. murinus in feces. Treatment with L. murinus was shown to prevent salt-induced hypertension by modulating Th17 cells32. Additionally, high-salt challenge was shown to decrease Lactobacillus spp. in the feces of healthy individuals, although Lactobacillus is not a dominant microorganism in human feces. In the present study, we found a marked reduction in the abundance of L. murinus in 10- to 15-week-old SHRs compared with WKY rats. Treatment with L. murinus reversed the increase in blood pressure and vascular dysfunction and lowered plasma LPS levels.
As a preliminary study, we examined the gut microbiome profile in Japanese hypertensive patients. Analysis of 16S amplicons revealed that “Lactobacillus Low” was seen more in subjects with hypertension than “Lactobacillus High” (41.7% vs. 25.0%, Supplementary Fig. 14). Although this study was a preliminary data and there was no significance (p = 0.642, Fisher’s Exact Test with two-tailed), the results support a hypothesis that hypertension might be associated with decrease in members of the former Lactobacillus group species, including Ligilactobacillus spp. Because the etiology of hypertension is complex, the role of Lactobacillus group species in human clinical subjects warrants further investigation.
This study focused on determining whether the treatment to reverse a decrease in specific microbiota affects the gut and cardiovascular system using male hypertensive rats. We recognize that several evidences suggest that blood pressure response in females are different from males in hypertensive rats33, 34. Similarly, in addition to the effects of diet and age, it also has been shown sex differences in gut microbiota especially in animals35. Thus, future studies should be directed to the gender difference of cardiovascular response and gut microbiota in hypertension.
Several recent animal model studies5 and human clinical studies6 have revealed a link between gut dysbiosis and cardiovascular diseases, including hypertension. One feature of hypertension-related dysbiosis is an accompanying increase in intestinal permeability8. However, the pathophysiologic mechanism by which an imbalance in the gut microbiota causes hypertension remains unclear. In the present study, we demonstrated that treatment with L. murinus reverses the increase in blood pressure and vascular endothelial dysfunction in SHRs. In addition, treatment with L. murinus reversed the disruption in intestinal barrier function by up-regulating claudin 4 and down-regulating TNF-α expression, resulting in reduced plasma levels of LPS. Although we still did not observe any significant differences in members of the former Lactobacillus group, including Ligilactobacillus spp., in human subjects with hypertension compared with normotensive controls, our findings were consistent with the hypothesis that gut dysbiosis–mediated low-grade endotoxemia is an important risk factor for cardiovascular events29. These findings enhance our understanding of the potential role(s) of gut dysbiosis in the pathogenesis of hypertension and highlight the possibilities of a new class of therapeutic agents for treating hypertension.
Methods
Animals
Ten male Wistar Kyoto (WKY) rats (10–15 weeks old) and thirty male SHRs (10–15 weeks old) were used in this study, and SHRs were divided into three groups of ten rats each (no treatment, control and L. murinus treatment). In some analysis, the difference in the numbers of experiments was attributable to the amounts of samples available for the analysis. We have analyzed all the data obtained from appropriately collecting samples and conducting experiments to the extent possible. Care of these animals was in accordance with standards set forth by the National Institutes of Health guidelines for the care and use of experimental animals. All procedures were approved by the Animal Care and Use Committee of the Okayama University of Science (2021-086) and performed in accordance with ARRIVE guidelines.
All animals were acclimatized for at least 4 weeks at our animal facility. Animals were fed standard laboratory chow (CE-2) (CLEA Japan, Tokyo, Japan), water ad libitum and bred with standard laboratory bedding (CL-4163) (CLEA Japan, Tokyo, Japan). In some experiments, 10- to 13-week-old SHRs were randomized to receive 1 mL of 10% glycerol alone or 10% glycerol with L. murinus (as an equal mixture of WO strains described in the Results section, approximately 1 × 108 CFU/mL per day) by oral gavage every day for 2 weeks. Animals were sacrificed with isoflurane overdose and exsanguination.
All animals were anesthetized with isoflurane (5%, MSD Animal Health, Readington Township, NJ) and euthanized by exsanguination at the end of the studies.
16S rDNA data analysis
Rats were acclimatized in the animal facility for 4–6 weeks, then fresh feces from WKY and SHR were collected. Fecal DNA was extracted by using commercial kit (NucleoBond HMW DNA, Takara, Japan) and DNA integrity was assessed using the 2200 TapeStation systems (Agilent Technologies, Santa Clara, CA, United States). Each sample corresponded to feces derived from one rat for the sequencing. These samples were prepared with LoopSeq 16S microbiome SSC 24plex kit (Loop Genomics, San Jose, CA, United States), sequenced on the illumine NextSeq and analyzed at Bioengineering Lab. Co, Ltd (Kanagawa, Japan). The datasets generated during the current study are available in the DDBJ Sequence Read Archive (DRA) repository (Accession number: DRA016499).
Isolation and cultivation of L. murinus
Rats were acclimatized in the animal facility for 4–6 weeks, and then fresh feces were collected from WKY rats. Fecal samples were suspended in 0.9% NaCl and serially diluted tenfold to obtain 10−3, 10−4, 10−5 and 10−6 dilutions. Aliquots (100 μL) of the diluted solutions were spread on Rogosa agar plates (Merck, Rahway, NJ, USA) with or without 20 µg/mL vancomycin. The spread plates were incubated anaerobically at 37 °C for 48 h, after which single colonies were randomly picked and inoculated individually into MRS medium (Solabia Biokar Diagnostics, Ile-de-France, France). After incubation at 37 °C, each culture was collected to prepare glycerol stocks (final glycerol concentration adjusted to 25%). The glycerol stocks were stored at − 80 °C prior to use.
PCR using species-specific primer sets (57-76F and 202-182R) was performed to detect L. murinus36. Each 20-µL reaction mixture contained 1× GoTaq Green Master Mix (Promega), 0.5 µM each primer (57-76F and 202-182R), and 2 µL of the respective template DNA. PCRs were performed using the following temperature profiles: one cycle at 95 °C for 2 min, followed by 30 cycles at 95 °C for 30 s, 55 °C for 30 s, 72 °C for 45 s, and one cycle at 72 °C for 5 min. The resulting PCR amplicons were electrophoresed on 2% (w/v) agarose gel at a constant voltage of 100 V for 30 min at room temperature. The gel was then stained with ethidium bromide (0.5 µg/mL) and visualized under UV light at 312 nm.
Partial 16S rDNA sequences of the isolates in this study were amplified by PCR using the bacterial consensus primers Eu8f (Escherichia coli positions 8 to 27) and Eu1492r (E. coli positions 1510 to 1492)37. The sequences were determined and used for identification from the EZBioCloud database38. The 16S rDNA sequences of L. murinus isolates were registered in the DDBJ/ENA/GenBank under accession no. LC741556-LC741564.
Enterobacterial Repetitive Intergenic Consensus Polymerase Chain Reaction (ERIC-PCR) was conducted according to a method described previously, with a slight modification39. The 25-µL reaction mixture contained 1× DreamTaq Buffer including 3 mM MgCl2 (Thermo Scientific), 200 µM dNTP mix (Thermo Scientific), 1 µM each primer (ERIC1R and ERIC2), 0.625 U of DreamTaq DNA Polymerase (Thermo Scientific) and 25 ng of the respective template DNA. PCRs were performed using the following temperature profiles: one cycle at 95 °C for 3 min, followed by 35 cycles at 95 °C for 30 s, 48 °C for 1 min, 72 °C for 5 min, and one cycle at 72 °C for 7 min. The resulting PCR amplicons were electrophoresed on a 1.5% (w/v) agarose gel at a constant voltage of 70 V for 2 h 30 min at 4 °C. The gel was then stained with ethidium bromide (0.5 µg/mL) and visualized under UV light at 312 nm.
Bacterial strains used in this study were isolated from fresh feces of WKY rats (especially strains belonging to L. murinus), and L. murinus NBRC 14221 was used as the type strain. Isolates of L. murinus (WO strains described in the Results section) were incubated overnight at 37 °C in MRS medium. After harvesting, each culture of WO strains was equally mixed and washed with 0.9% NaCl. After centrifugation, the cell pellet was resuspended in 10% glycerol and used for oral administration of L. murinus to rats. The 10% glycerol solution containing L. murinus was divided into small portions and stored at − 80 °C prior to use.
Genomic DNA for PCR assays to detect L. murinus and 16S rDNA gene sequencing was extracted from fresh cells cultured in MRS medium by using PrepMan Ultra Sample Preparation Reagent (Applied Biosystems, Foster City, CA, USA). High-purity DNA was extracted for ERIC-PCR using the Wizard Genomic DNA Purification kit (Promega) following the manufacturer's protocol.
Blood pressure measurement using a tail-cuff method
Systolic blood pressure was measured in Wistar-Kyoto rats (WKY) and spontaneously hypertensive rats (SHR) using a tail-cuff method (Softron, Tokyo, Japan) as previously described40. Rats were trained to reduce stress before measurement, and then blood pressure was measured at room temperature without a heater.
Vascular function
Mesenteric arterial functions were assessed using a wire myograph preparation as previously described41. The secondary branches of mesenteric arteries were dissected and cut into small pieces. The preparations were suspended in an organ bath containing Kreb’s buffer (mmol/l: 118.3 NaCl, 4.7 KCl, 1.2 MgSO4, 1.2 KH2PO4, 25 NaHCO3, 2.5 CaCl2, and 11 glucose) maintained at 37 °C and 95% O2/5% CO2. Mesenteric arteries were then equilibrated for 45 min under a resting tension of 0.03–0.05 g, and contraction was recorded in response to KCl (10–100 mmol/L). Concentration-dependent response curves to acetylcholine (ACh, 0.3 nmol/L–30 μmol/L) or sodium nitroprusside (SNP, 0.1 nmol/L–10 μmol/L) were performed after an initial submaximal precontraction (50–70%) with U46619 (1–10 μmol/L). In addition, concentration-dependent response curves to serotonin (10 nmol/L–30 μmol/L) was performed.
Measurement of intestinal permeability
Intestinal permeability in the ileum and proximal colon was assessed using the non-everted gut sac method, as previously described42, 43. Rats were euthanized after fasting for 12–14 h, and then the ileum or proximal colon was carefully dissected and cut into 3- to 5-cm pieces. FITC-Dextran, molecular weight 4 K or 70 K, was placed into the intestinal pieces and tied with cotton thread. The preparations were placed in an organ bath containing Tyrode’s solution without calcium (mmol/L: 136.9 NaCl, 2.68 KCl, 1.05 MgCl2, 0.41 NaH2PO4, 11.9 NaHCO3 and 5.55 glucose) and maintained at 37 °C and 95% O2/5% CO2. Medium was collected at 0, 30, 60, 90, and 120 min time points and analyzed for FITC on a fluorescent plate reader (Tecan, Männedorf, Switzerland). The apparent permeability of each individual intestinal sac was then calculated.
Western blotting
Proximal colon and ileum were cleaned of fat and snap-frozen in liquid nitrogen. Frozen samples were homogenized in lysis buffer containing 50 mmol/l Tris·Cl buffer, 0.1 mmol/l EDTA (pH 7.5), 1% (wt/vol) Na deoxycholic acid, 1% (vol/vol) Nonidet P-40, and 0.1% (vol/vol) SDS with protease inhibitor and phosphatase inhibitors (Nacalai Tesque, Kyoto, Japan). Samples were rotated for 1 h at 4 °C and centrifuged (20,000g) for 10 min at 4 °C and then supernatants were collected. The protein concentration in the lysis buffer was determined by a Lowry assay (Nacalai Tesque). Equal amounts of proteins (50 μg) were separated by SDS-PAGE (8–12%) and transferred to a PVDF membrane (Millipore, Burlington, MA, USA). Membranes were blocked with 5% skim milk and incubated with primary antibodies at 4 °C overnight and then visualized using horseradish peroxidase-conjugated secondary antibodies (1:10,000 dilution, 1 h). Antibodies against claudin 4, occluding, cingulin, ZO-2 (Proteintech, Rosemont, IL, USA), and ZO-1 (Cell Signaling Technology, Danvers, MA, USA) were used for these experiments. GAPDH was used as a loading control (Santa Cruz, Dallas, TX, USA). Some membranes were cut prior to incubation with primary antibodies.
Histology
Proximal colon was fixed with 10% neutral buffered formalin and subjected to paraffin sectioning. Sections were antigen retrieval in Tris–EDTA buffer (pH 9.0) and against claudin 4 (1:400 dilution, Proteintech, Rosemont, IL, USA). Intestinal morphology was determined by hematoxylin and eosin staining. Intestinal crypt and goblet cell were visualized by PAS staining. The area of the intestinal crypts stained with PAS and the number of goblet cells on intestinal mucosa were measured using ImageJ software (National Institutes of Health). When comparing between samples, adjustments to microscope settings (NIS-Elements, Nikon, Tokyo, Japan) were kept constant throughout image collection. The entire intestinal mucosa was captured and analyzed.
Quantitative real-time RT-PCR (qPCR)
RNA was extracted from proximal colon, and quantitative real-time RT-PCR (qPCR) was performed as previously described44. Briefly, using a commercial kit (ReverTra Ace qPCR RT Master Mix, Toyobo, Osaka, Japan), cDNA was synthesized from 200–400 ng of total RNA extracted from the tissues using RNeasy spin columns (RNeasy Mini Kit, QIAGEN, Hilden, Germany). Each Q-PCR reaction was performed in duplicate. 2–5 ng of cDNA was subjected to gene expression assays using PrimeTime Gene Expression Master Mix (IDT) and the targeted probes. The following IDT probes were used on the Applied Biosystems QuantStudio System to evaluate gene expression levels: GAPDH (Rn.PT.39a.11180736.g), tumor necrosis factor α (TNF-α) (Rn.PT.58.36305979), IL-6 (Rn.PT.58.13840513), TGF-β (Rn.PT.58.6690138), LGR5 (Rn.PT.58.8656422), tert (Rn.PT.58.13068002), MUC2 (Rn.PT.58.45157067), MUC1 (Rn.PT.58.45226306), MUC4 (Rn.PT.58.44816706), TLR2 (Rn.PT.58.11978329), TLR4 (Rn.PT.58.11700071), CD3 (Rn.PT.58.13215743) and CD68 (Rn.PT.58.37733352). ΔΔCT was calculated using GAPDH as a reference gene to determine relative mRNA expression levels.
Flow cytometry
Mesenteric lymph nodes and spleen were collected from rats. The tissues were mashed with slides in RPMI1640 medium and the solutions were filtered through a 100 μm cell strainer. After centrifugation, cells were resuspended with RPMI1640 medium containing 10% fetal bovine serum (FBS) and were adjusted to a concentration of 2 × 106 cells/mL. A total of 1 mL of cells were seeded to each well on 24-well plate and incubated with 1 ug brefeldin A, 1 μg of ionomycin, and 50 ng of phorbol 12-myristate 13-acetate. After 4.5 h of incubation at 37 °C in 5% CO2, cells in each well were harvested, washed once with PBS, and blocked with anti-CD32 (BD biosciences, clone CD34-485, San Jose, CA, USA) for 10 min at 4 °C to avoid non-specific antibody binding to Fc-gamma receptors. After that, the cell surface staining was performed with mAbs anti-CD4 (Biolegend, clone W3/25), anti-CD45 (Biolegend, clone OX-1), and viability dye (LIVE/DIED® Fixable Aqua Dead cell Stain Kit, ThermoFisher, Waltham, MA, USA) for 20 min at 4 °C. Then, cells were fixed with 4% paraformaldehyde at 4 °C for 20 min, washed once, and permeabilized by PBS containing 0.5% saponin (Nakalai tesque) and 0.5% bovine serum albumin (Fujifilm Wako, Richmond, VA, USA) at 4 °C for 30 min. After washing the fixed and permeabilized cells, intracellular staining was conducted with mAbs anti-IL17A (Biolegend, clone TC11-18H10.1), and anti-FoxP3 (eBiosciences, clone FJK-16s, San Diego, CA, USA), and anti-IFNγ (Biolegend, DB-1). Then, the cells were washed once, resuspended with PBS containing 2% FBS, and transferred to a 5 mL polystyrene tube through a 100 μm mesh. All samples were analyzed using a flow cytometer BD LSRFortessa (BD Biosciences) with FACSDIVA software.
Plasma concentration of endotoxin
Plasma was collected from WKY rats and SHRs. The endotoxin level was measured using a commercial kit (Lonza, Basel, Switzerland).
Human study
This study is approved by the Institutional Review Board of Ehime University Graduate School of Medicine (Reference no.1912011) and Institutional Review Board of the Okayama University of Science (Reference no. 3-2) and all methods in this study were performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from all subjects by opt-out methods45. Briefly, Control (not taking anti-hypertensive medication) and Hypertensive (currently under hypertensive treatment or not taking anti-hypertensive medication) subjects were identified during their routine of health checkup at JA Ehime Kouseiren Checkup Center (Ehime, Japan). Major exclusion criteria for this study were as follows: (1) currently or previous antibiotic treatment within the last 2 months of study enrollment or (2) currently taking probiotics. Each subject was 50 years old or above of age. Upon registration with opt-out consent, an office ambient BP measurement was recorded for each individual and stool sample collection kits containing sample collection and return instructions were provided. Stool samples were collected using disposable test kit of bowel cancer by the patients, placed in a stool collection tube and fecal DNA was isolated. These samples were sent to Bioengineering Lab. Co, Ltd (Kanagawa, Japan), sequenced on the illumine MiSeq and analyzed by Qiime2. Data analysis was based on office BP measurements. Cutoff value for “Low” result of Lactobacillus was less than 0.047. Cutoff value was determined by receiver operating characteristic curve [ROC] analysis. χ2-tests were performed to find the significant differences between two groups. The datasets generated during the current study are available in the DDBJ Sequence Read Archive (DRA) repository (Accession number: DRA016495).
Chemicals
ACh, SNP, 40 K and 70 K FITC-dextran and phorbol 12-myristate 13-acetate were purchased from Sigma (St. Louis, MO). KCl, serotonin, U46619 and ionomycin were obtained from Fujifilm Wako (Richmond, VA, USA).
Statistical analysis
Experiments were performed in similar numbers between genotypes and control and treatment groups. Results are expressed as mean ± SEM. The data were statistically evaluated using GraphPad Prism software (San Diego, CA, USA). Where appropriate, the unpaired Student’s t-test was used to compare differences between two groups. In other experiments, two-way ANOVA (repeated measures when appropriate) with post hoc Tukey’s tests was used to compare data. Differences were considered significant at P < 0.05. Normality was assessed using a Kolmogorov–Smirnov test.
Data availability
The data from this study are available from the corresponding author on reasonable request. The datasets of 16S rDNA data generated during the current study are available in the DDBJ Sequence Read Archive (DRA) repository (Accession number: DRA016499 and DRA016495).
References
Jandhyala, S. M. et al. Role of the normal gut microbiota. World J. Gastroenterol. 21, 8787–8803. https://doi.org/10.3748/wjg.v21.i29.8787 (2015).
Kelly, J. R. et al. Breaking down the barriers: The gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front. Cell Neurosci. 9, 392. https://doi.org/10.3389/fncel.2015.00392 (2015).
Shreiner, A. B., Kao, J. Y. & Young, V. B. The gut microbiome in health and in disease. Curr. Opin. Gastroenterol. 31, 69–75. https://doi.org/10.1097/MOG.0000000000000139 (2015).
Collaborators, G. B. D. R. F. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1659–1724. https://doi.org/10.1016/S0140-6736(16)31679-8 (2016).
Yang, T. et al. Gut dysbiosis is linked to hypertension. Hypertension 65, 1331–1340. https://doi.org/10.1161/HYPERTENSIONAHA.115.05315 (2015).
Li, J. et al. Gut microbiota dysbiosis contributes to the development of hypertension. Microbiome 5, 14. https://doi.org/10.1186/s40168-016-0222-x (2017).
Karbach, S. H. et al. Gut microbiota promote angiotensin II-induced arterial hypertension and vascular dysfunction. J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.116.003698 (2016).
Santisteban, M. M. et al. Hypertension-linked pathophysiological alterations in the gut. Circ. Res. 120, 312–323. https://doi.org/10.1161/CIRCRESAHA.116.309006 (2017).
Niewiem, M. & Grzybowska-Chlebowczyk, U. Intestinal barrier permeability in allergic diseases. Nutrients https://doi.org/10.3390/nu14091893 (2022).
Bischoff, S. C. et al. Intestinal permeability—A new target for disease prevention and therapy. BMC Gastroenterol. 14, 189. https://doi.org/10.1186/s12876-014-0189-7 (2014).
Damms-Machado, A. et al. Gut permeability is related to body weight, fatty liver disease, and insulin resistance in obese individuals undergoing weight reduction. Am. J. Clin. Nutr. 105, 127–135. https://doi.org/10.3945/ajcn.116.131110 (2017).
Duan, Y. et al. Bone marrow-derived cells restore functional integrity of the gut epithelial and vascular barriers in a model of diabetes and ACE2 deficiency. Circ. Res. 125, 969–988. https://doi.org/10.1161/CIRCRESAHA.119.315743 (2019).
Lewis, C. V. & Taylor, W. R. Intestinal barrier dysfunction as a therapeutic target for cardiovascular disease. Am. J. Physiol. Heart Circ. Physiol. 319, H1227–H1233. https://doi.org/10.1152/ajpheart.00612.2020 (2020).
Troseid, M., Andersen, G. O., Broch, K. & Hov, J. R. The gut microbiome in coronary artery disease and heart failure: Current knowledge and future directions. EBioMedicine 52, 102649. https://doi.org/10.1016/j.ebiom.2020.102649 (2020).
Kazemian, N., Mahmoudi, M., Halperin, F., Wu, J. C. & Pakpour, S. Gut microbiota and cardiovascular disease: Opportunities and challenges. Microbiome 8, 36. https://doi.org/10.1186/s40168-020-00821-0 (2020).
Avery, E. G. et al. The gut microbiome in hypertension: Recent advances and future perspectives. Circ. Res. 128, 934–950. https://doi.org/10.1161/CIRCRESAHA.121.318065 (2021).
Grylls, A., Seidler, K. & Neil, J. Link between microbiota and hypertension: Focus on LPS/TLR4 pathway in endothelial dysfunction and vascular inflammation, and therapeutic implication of probiotics. Biomed. Pharmacother. 137, 111334. https://doi.org/10.1016/j.biopha.2021.111334 (2021).
Camilleri, M. Leaky gut: Mechanisms, measurement and clinical implications in humans. Gut 68, 1516–1526. https://doi.org/10.1136/gutjnl-2019-318427 (2019).
Yang, T. et al. Transcriptomic signature of gut microbiome-contacting cells in colon of spontaneously hypertensive rats. Physiol. Genomics 52, 121–132. https://doi.org/10.1152/physiolgenomics.00087.2019 (2020).
Toral, M. et al. Critical role of the interaction gut microbiota—Sympathetic nervous system in the regulation of blood pressure. Front. Physiol. 10, 231. https://doi.org/10.3389/fphys.2019.00231 (2019).
Van Itallie, C., Rahner, C. & Anderson, J. M. Regulated expression of claudin-4 decreases paracellular conductance through a selective decrease in sodium permeability. J. Clin. Investig. 107, 1319–1327. https://doi.org/10.1172/JCI12464 (2001).
Kage, H. et al. Claudin 4 knockout mice: Normal physiological phenotype with increased susceptibility to lung injury. Am. J. Physiol. Lung Cell Mol. Physiol. 307, L524-536. https://doi.org/10.1152/ajplung.00077.2014 (2014).
Saleri, R. et al. Effects of different short-chain fatty acids (SCFA) on gene expression of proteins involved in barrier function in IPEC-J2. Porcine Health Manag. 8, 21. https://doi.org/10.1186/s40813-022-00264-z (2022).
Gehart, H. & Clevers, H. Tales from the crypt: New insights into intestinal stem cells. Nat. Rev. Gastroenterol. Hepatol. 16, 19–34. https://doi.org/10.1038/s41575-018-0081-y (2019).
Wong, J. et al. RIPK1 mediates TNF-induced intestinal crypt apoptosis during chronic NF-kappaB activation. Cell Mol. Gastroenterol. Hepatol. 9, 295–312. https://doi.org/10.1016/j.jcmgh.2019.10.002 (2020).
Madhur, M. S. et al. Interleukin 17 promotes angiotensin II-induced hypertension and vascular dysfunction. Hypertension 55, 500–507. https://doi.org/10.1161/HYPERTENSIONAHA.109.145094 (2010).
Marko, L. et al. Interferon-gamma signaling inhibition ameliorates angiotensin II-induced cardiac damage. Hypertension 60, 1430–1436. https://doi.org/10.1161/HYPERTENSIONAHA.112.199265 (2012).
Didion, S. P., Kinzenbaw, D. A., Schrader, L. I., Chu, Y. & Faraci, F. M. Endogenous interleukin-10 inhibits angiotensin II-induced vascular dysfunction. Hypertension 54, 619–624. https://doi.org/10.1161/HYPERTENSIONAHA.109.137158 (2009).
Violi, F. et al. Gut-derived low-grade endotoxaemia, atherothrombosis and cardiovascular disease. Nat. Rev. Cardiol. https://doi.org/10.1038/s41569-022-00737-2 (2022).
Bomfim, G. F. et al. Toll-like receptor 4 inhibition reduces vascular inflammation in spontaneously hypertensive rats. Life Sci. 122, 1–7. https://doi.org/10.1016/j.lfs.2014.12.001 (2015).
Dange, R. B., Agarwal, D., Teruyama, R. & Francis, J. Toll-like receptor 4 inhibition within the paraventricular nucleus attenuates blood pressure and inflammatory response in a genetic model of hypertension. J. Neuroinflamm. 12, 31. https://doi.org/10.1186/s12974-015-0242-7 (2015).
Wilck, N. et al. Salt-responsive gut commensal modulates TH17 axis and disease. Nature 551, 585–589. https://doi.org/10.1038/nature24628 (2017).
Elmarakby, A. A. & Sullivan, J. C. Sex differences in hypertension: Lessons from spontaneously hypertensive rats (SHR). Clin. Sci. 135, 1791–1804. https://doi.org/10.1042/CS20201017 (2021).
Sosnowski, D. K. et al. Cardiomyocyte-specific disruption of soluble epoxide hydrolase limits inflammation to preserve cardiac function. Am. J. Physiol. Heart Circ. Physiol. 323, H670–H687. https://doi.org/10.1152/ajpheart.00217.2022 (2022).
Kim, Y. S., Unno, T., Kim, B. Y. & Park, M. S. Sex differences in gut microbiota. World J. Mens Health 38, 48–60. https://doi.org/10.5534/wjmh.190009 (2020).
Gomes-Neto, J. C. et al. A real-time PCR assay for accurate quantification of the individual members of the Altered Schaedler Flora microbiota in gnotobiotic mice. J. Microbiol. Methods 135, 52–62. https://doi.org/10.1016/j.mimet.2017.02.003 (2017).
Weisburg, W. G., Barns, S. M., Pelletier, D. A. & Lane, D. J. 16S ribosomal DNA amplification for phylogenetic study. J. Bacteriol. 173, 697–703. https://doi.org/10.1128/jb.173.2.697-703.1991 (1991).
Yoon, S. H. et al. Introducing EzBioCloud: A taxonomically united database of 16S rRNA gene sequences and whole-genome assemblies. Int. J. Syst. Evol. Microbiol 67, 1613–1617. https://doi.org/10.1099/ijsem.0.001755 (2017).
Ventura, M. & Zink, R. Specific identification and molecular typing analysis of Lactobacillus johnsonii by using PCR-based methods and pulsed-field gel electrophoresis. FEMS Microbiol. Lett. 217, 141–154. https://doi.org/10.1111/j.1574-6968.2002.tb11468.x (2002).
Mukohda, M., Mizuno, R. & Ozaki, H. Increased blood pressure causes lymphatic endothelial dysfunction via oxidative stress in spontaneously hypertensive rats. Hypertension 76, 598–606. https://doi.org/10.1161/HYPERTENSIONAHA.119.14636 (2020).
Mukohda, M. et al. RhoBTB1 protects against hypertension and arterial stiffness by restraining phosphodiesterase 5 activity. J. Clin. Investig. 129, 2318–2332. https://doi.org/10.1172/JCI123462 (2019).
Liu, W. et al. Developments in methods for measuring the intestinal absorption of nanoparticle-bound drugs. Int. J. Mol. Sci. https://doi.org/10.3390/ijms17071171 (2016).
Mateer, S. W. et al. Ex vivo intestinal sacs to assess mucosal permeability in models of gastrointestinal disease. J. Vis. Exp. https://doi.org/10.3791/53250 (2016).
Mukohda, M., Mizuno, R., Saito, F., Matsui, T. & Ozaki, H. Hypertension is linked to enhanced lymphatic contractile response via RGS16/RhoA/ROCK pathway. Am. J. Physiol. Heart Circ. Physiol. 323, H1118–H1129. https://doi.org/10.1152/ajpheart.00496.2022 (2022).
Vellinga, A., Cormican, M., Hanahoe, B., Bennett, K. & Murphy, A. W. Opt-out as an acceptable method of obtaining consent in medical research: A short report. BMC Med. Res. Methodol. 11, 40. https://doi.org/10.1186/1471-2288-11-40 (2011).
Acknowledgements
We thank Dr. Satoshi Matsumoto at Yakult Central Institute and Drs. Fumiyo Saito, Koji Hayakawa, and Shuichi Tawara at Okayama University of Science for helpful suggestions. The authors also thank Mr. Ryo Miyase and Ms. Saori Misaki of JA Ehime Kouseiren Checkup Center (Ehime, Japan) for assistance for correcting human samples. The authors would like to acknowledge assistance from the Experimental Animal Facility at Okayama University of Science.
Funding
Funding was provided by Japan Society for the Promotion of Science (Grant numbers: 22H02527, 22K08369), Promotion of Okayama University of Science (OUS) Research Project (Grant number: OUS-RP-21-1) and The Sanyo Broadcasting Foundation.
Author information
Authors and Affiliations
Contributions
M.M. and H.O. conceived and designed the research; M.M., T.Y., T.M., S.N., J.M. and K.T. performed experiments; M.M., T.Y., T.M., J.M. and K.T. analyzed data; M.M., T.Y., T.M., S.N., J.M., K.T., R.M., R.M. and H.O. interpreted the experimental results; M.M. prepared the figures and drafted the manuscript; H.O. provided extensive editing and revision of the manuscript; T.Y., J.M., T.M., K.T., R.M. and R.M. edited and revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mukohda, M., Yano, T., Matsui, T. et al. Treatment with Ligilactobacillus murinus lowers blood pressure and intestinal permeability in spontaneously hypertensive rats. Sci Rep 13, 15197 (2023). https://doi.org/10.1038/s41598-023-42377-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42377-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.