Abstract
The purpose of this study is to understand psychosocial impacts on cancer survivors using the patient-reported outcomes measurement information system (PROMIS) Psychosocial Illness Impact banks. Cancer survivors (n = 509; age: 59.5 ± 1.4; 51.5% men) completed the PROMIS positive and negative illness impact items consisting of four sub-domains: self-concept (SC), social impact (SI), stress response (SR), and spirituality (Sp). Illness impact was defined as changed scores from items measuring “current” experiences to recalled experiences prior to cancer diagnosis. Descriptive statistics, effect sizes (ES), and coefficient of variation (CV) were calculated at item and sub-domain levels. Analysis of variance was used to identify potentially influential factors on the impacts. Our study found survivors reported stronger positive than negative impacts (overall ES mean: 0.30 vs. 0.23) in general; and more moderate (ES ≧ 0.30) positive than negative impacts at the item level, 54.3% (25 of 46) and 40% (16 of 40) for positive and negative items, respectively. Participants reported more positive impacts on SI and Sp but more negative impacts on SR. The CV results showed more individual differences appeared on positive SC items. Younger survivors reported stronger positive and negative impacts. Women reported higher positive impacts. Survivors with higher education levels tended to have higher positive SI impacts, while those with a lower family income reported higher negative SI and negative SR impacts. We conclude positive and negative psychosocial impacts coexisted—the strength of impacts varied across sub-domains. Age, gender, education, and family income influenced the psychosocial impacts reported by survivors. These findings provide a foundation to develop interventions to strengthen positive and minimize negative impacts and improve cancer survivors’ overall well-being.
Similar content being viewed by others
Introduction
With advances in cancer treatment, many cancers can now be controlled or managed for long periods1. Given the growing number of cancer survivors, understanding the psychosocial impacts of cancer and cancer treatment becomes critical to promoting survivors’ health-related quality of life. Historically, psychosocial research has focused on cancer’s negative consequences, such as mood disturbances, anxiety, cognitive problems, coping challenges, and interference with social relationships2,3,4,5,6,7,8,9,10. However, research also found that cancer experiences may increase personal resilience, which minimizes adverse impacts on illness11, 12. Survivors reported having greater life appreciation, changed priorities, closer relationships with families and friends, and enhanced spirituality after cancer diagnosis and treatment13,14,15,16,17,18,19,20,21,22. Thus, it is crucial to consider both the positive and negative impacts of the cancer experience23 in psychosocial interventions for cancer survivors by minimizing negative impacts yet enhancing positive impacts.
In 2004, the National Institutes of Health initiated a multicenter cooperative group called the Patient-Reported Outcomes Measurement Information System (PROMIS)24. PROMIS investigators developed reliable and valid measures of person-reported physical, mental, and social health, including psychosocial illness impact item banks25. The psychosocial illness impact item banks were developed using patient-centered approaches and items were generated based on interviews with cancer survivors. The initial psychometric evaluation results suggested that positive and negative illness impacts, although coexisting, were two independent constructs from a measurement perspective26. Subsequently, two different measures were recommended. Additional interviews with cancer survivors were conducted to ensure comprehensive content coverage, and the PROMIS Illness Impact Working Group wrote new items according to interview results. Items were classified into four sub-domains: self-concept (SC), social-impact (SI), stress-response (SR), and spirituality (Sp). To better capture the “impacts” of cancer diagnosis and/or treatment, patients provide two responses to each question: one is to consider the time before cancer diagnosis and/or treatment, and the other reflects the present. Field tests on patients with cancer showed that this measure has good reliability and validity26,27,28. The PROMIS psychosocial illness impact item banks are reported using an Item Response Theory (IRT) based T-score scoring matrix. The IRT-based T-scores consider varying degrees of discrimination and difficulty levels of each item on the measurement continuum, enabling a brief yet precise estimation of the construct of interest. Despite the well-known advantages mentioned above, our study showed individual items within the item bank might be more sensitive to individual attributes29. Patients with different types of cancer may have illness impacts in different aspects. For example, breast cancer survivors with a mastectomy and colorectal cancer survivors with an ostomy may have worse body image30, 31. These physical changes can affect cancer survivors not only in appearance but also in intimate relationships. Cancer survivors also face psychological and emotional issues, such as depression, grief, fear of recurrence, survivor guilt, etc32, 33. Understanding psychosocial impacts upon cancer diagnosis and treatment at the item levels and factors associated with those impacts can guide the development of personalized short forms by selecting items sensitive to change based on individual attributes.
This study explored the extent of psychosocial impacts since cancer diagnosis at the item and the sub-domain levels across the disease continuum. We sought to identify items exhibiting the most impacts, differences between negative and positive impacts, and factors associated with the impacts. The results of this study can help pave the way for the development of individualized interventions that strengthen the positive effects of cancer diagnosis and treatment and minimize the negative effects.
Methods
We presented our study design and results following the reporting guideline from the EQUATOR Network34,35,36.
Participants
Participants included 509 cancer survivors recruited from the Duke Cancer Care Research Program in Durham, NC (n = 72), the Duke Tumor Registry (n = 283), and NexCura, a nationwide online registry of more than 500,000 cancer survivors (n = 154). Survivors were eligible if they were 18 years or older, had a cancer diagnosis, and were fluent in English. This study was approved by the Institutional Review Board of Northwestern University, and all participants provided informed consent. All methods performed in this study follow the relevant guidelines and regulations.
Measures
This study was conducted as a cross-sectional study, and participants completed the following measures only once. The PROMIS Psychosocial Illness Impact item banks27 consist of four conceptual sub-domains (see Fig. 1 for the structure of the item banks): Self-Concept (SC), Social-Impact (SI), Stress-Response (SR), and Spirituality (Sp). Across these four sub-domains are 46 items measuring positive psychosocial illness impacts and 40 items measuring negative psychosocial illness impacts, including 11 positive and 9 negative SC items; 12 positive and 11 negative SI items; 11 positive and 10 negative SR items; and 12 positive and 10 negative Sp items (see Tables 1, 2 for item contents). Participants describe the extent to which the concept, as reflected in each item, affected their lives before their cancer diagnosis and/or treatment (How true was this before your illness?) and currently (How true is this now, since your illness?). In the following analyses, “before” referred to “How true was this before your illness?” and “current” referred to responses to “How true is this now, since your illness?” A 5-point rating scale is used: 0 = not at all, 1 = a little bit, 2 = somewhat, 3 = quite a bit, and 4 = very much. “Illness impact” was defined as the changed scores from “before” to “current” (“now”). Larger changed scores on positive and negative items indicated positive and negative impacts, respectively.
Data analysis
Descriptive statistics were conducted at both item- and sub-domain levels on “illness impact” (“current”—“before”) (range: -4 to 4); that is, response to “How true is this now, since your illness?”—response to “How true was this before your illness?” Effect size (ES; mean of impact divided by standard deviation) was used to estimate the averaged magnitudes and direction of impacts. An ES is considered trivial when the absolute value < 0.1, small when ES is between 0.1 and 0.3, moderate when ES is between 0.3 and 0.5, and large when ES ≧ 0.537. The coefficient of variation (CV; standard deviation divided by the impact mean) was used to estimate the variability of responses on individuals. An item with high variability implies its potential to capture a wide range of differences in individual responses to this item that are often overlooked during the averaging process38. Items with absolute CVs > 10 are considered to have significant variability39.
Analyses of variance (ANOVA) were used to investigate the potential factors associated with impacts, including age (< 50, 50–65, 65+), gender (male vs. female), ethnicity (White vs. non-White), relationship status (having vs. not, significant other including married, living with a partner), education (≦ high school vs. ≧ some college), and family income (< 20 K, 20–50 K, 50–100 K, > 100 K). Post-hoc (Tukey’s pairwise) comparisons were followed if overall a demographic variable was significant (p < 0.05).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Results
Participants
Cancer survivors were primarily White (86.2%), married or living with a partner (75.4%), had at least some college education (84.2%), and had a household income higher than $50,000 (66.0%; 10.3% < 20 K, 23.7% 20–50 K, 37.6% 50–100 K, 28.4% > 100 K). They had an average age of 60.4 ± 11.4 years (20.4% < 50, 44% 50–65, 35.6% 65 +), 51.6% were male, 30.3% were full-time employed, and 36.2% were retired. Most survivors (87.5%) affiliated with a religion and expressed that religious affiliation was important to them (77.6%). Survivors had a wide range of cancer diagnoses, including breast (24.4%), colorectal (17.1%), prostate (15.7%), and lung (10.2%). The average time since cancer diagnosis was 4.7 ± 5.1 years (16.3% < 1 year, 32.3% > 5 years); 21.0% had experienced a cancer recurrence. Regarding treatment, 58.9% had received no treatment within the past month, 21.6% received chemotherapy, and 7.1% received radiation therapy. Most survivors reported normal daily activity with either no symptoms (54.0%) or some that did not require bed rest during the waking day (34.6%).
Descriptive statistics
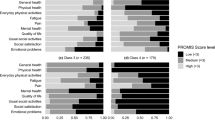
Descriptive statistics and CV and ES of impact scores are shown in Tables 1 and 2 for positive and negative measures, respectively. At the item level, means of impact scores were 0.26 (range − 0.10 to 0.66) and 0.23 (range − 0.54 to 0.77) for positive and negative items, respectively. For items capturing positive aspects, patients reported the largest change since cancer diagnosis on “I see what is really important in my life” (Sp12; impact score = 0.66), followed by ”I am aware of the love and support available from other people” (SI05; impact score = 0.62), and “I am comfortable receiving help from others” (SI07; impact score = 0.59). For those capturing negative aspects, patients reported the largest change since cancer diagnosis on “I fear what will happen in the future” (SR06; impact score = 0.77), followed by “I worry about the future” (SR01; impact score = 0.73) and “Worry about my health interferes with my life” (SR05; impact score = 0.73). At the sub-domain level, survivors reported almost no impact on positive SC (mean = 0.06) and negative Sp (mean = 0.07), yet large impacts on positive SI (mean = 0.39) and negative SR (means = 0.33). These results corresponded to the results at the item level. It was noted that patients reported minimal impacts on positive SC and negative Sp, where 10 (of 11) and 8 (of 10) items had an absolute impact mean≦ 0.2 for positive SC and negative Sp items, respectively.
Standardized impacts—effect size
As shown in Tables 1 and 2, the overall ES means (SDs) were 0.30 (± 0.23) and 0.23 (± 0.25 for positive and negative impacts, respectively. Among all 86 positive and negative items, 26 (30.2%) items and 15 (17.4%) items had moderate or strong impacts (absolute ES value ≥ 0.3) towards a positive and negative direction, respectively. This suggests survivors generally reported more positive than negative impacts from their cancer experiences. At the sub-domain level, survivors reported small or moderate impacts towards a positive direction on positive SI (mean ES = 0.47), positive SR (ES = 0.27), and positive Sp (mean ES = 0.37). A negligible impact was reported on positive SC (mean ES = 0.07). Survivors reported small impacts towards a negative direction on all negative sub-domains: SC (mean ES = 0.27), SI (mean ES = 0.27), SR (mean ES = 0.29), and Sp (mean ES = 0.11). These results supported our previous findings that positive and negative impacts coexisted with different strengths across sub-domains26.
At the item level, for positive items, thirteen larger positive ES (see Fig. 2) suggested that survivors had more appreciation of their physical health (SC06, ES = 0.45), life (Sp03, ES = 0.50), important things in life (Sp12, ES = 0.70) and people in their life (SI08, ES = 0.66); found more love and support from others (SI05, ES = 0.64), more compassion (SI02, ES = 0.52), more strength in prayer (Sp11, ES = 0.46) and close to God (Sp10, ES = 0.45); realized who their friends are (SI06, ES = 0.59); they were more comfortable asking others for help (SI03, ES = 0.53), receiving help (SI07, ES = 0.64), and expressing emotion (SR01, ES = 0.50); and took better care of themselves (SR08, ES = 0.60) after the cancer diagnosis. For negative items, ten larger positive ES (see Fig. 3) indicated that survivors experienced greater worry (SR01, SR05, SR09, ES > 0.58), fear (SR06, ES = 0.64), helplessness (SC09, ES = 0.45), distress and nervousness (SR04, SR10, ES > 0.49), and feelings of guilt and being a burden (SI01, SI05, SI08, ES > 0.43) after their illness as compared to before.
Variability of items
The variability of impact scores was small across all sub-domains with CVs < 10. It was noticed that 15 items (9 positive and 6 negative) had an absolute mean ≦ 0.1 but had an absolute CV greater than 10. Of these 9 positive items, 6 were positive Self-Concept items. These findings suggest significant individual variations on these items. However, changes in individual participants were inconsistent in direction resulting in the mean offsets impact changes in positive and negative directions.
Influential factors of illness impact
Analyses of variance (ANOVA) showed significant results on age, gender, education, and income factors (p < 0.05). The following post-hoc comparison results are presented in Table 3. Age was a significant factor in 7 of 8 sub-domains across negative and positive impacts; younger survivors reported higher positive and negative impacts. Gender was a significant factor only in four positive subdomains but not in negative ones; women had higher positive impact scores than men. Survivors with higher education levels tended to have higher positive SI impact scores. Survivors with a lower family income had higher negative SI and negative SR impact scores. No significant effects were observed on ethnicity and relationship status.
Discussion
The experience of cancer can be devastating but can also bring an opportunity for personal growth and new perspectives on life40,41,42,43,44. In this study, we examined the psychosocial impacts of cancer and its treatment using concepts raised by cancer survivors, which were then formatted to capture the psychosocial impacts due to cancer diagnosis in depth. Our results indicated positive and negative psychosocial impacts coexisted, coinciding with the literature26, 40,41,42,43,44,45. We suggest that interventions should consider both positive and negative impacts. Our findings can serve as a foundation to develop targeted, individualized interventions for whom increasing facilitators are needed by emphasizing positive impacts and minimizing barriers are needed by focusing on decreasing negative impacts.
Survivors reported different levels of impact upon contents addressed by individual items. A brief form that consists of items with large ES can be created for measuring survivor psychosocial impacts upon cancer if administering full-length PROMIS Psychosocial Illness Impact item banks or computerized adaptive tests is not feasible. Past research proposed three important facets of impact from severely stressful life events: self-perceptions, social relationships, and personal growth and life priorities42,43,44, 46. Tedeschi and Calhoun47 studied individual growth after encountering trauma such as cancer using Posttraumatic Growth Inventory. They found five factors: a greater appreciation of life, a changed sense of priorities, warmer and more intimate relationships, a greater sense of personal strength, and recognition of new possibilities or paths for one's life and spiritual development. Our results confirm these findings. Particularly, we found that survivors reported more social support (mean ES = 0.47 for positive items) and better spiritual well-being (mean ES = 0.37 for positive items) but had relatively more challenges with stress (mean ES = 0.29 for negative items) and worse self-concept (mean ES = 0.27 for negative items). These findings were also supported by Park and Blank’s study, in which cancer survivors reported larger positive impacts than negative ones43. However, their measure was not limited to psychosocial impact.
Individual differences were noted on 15 items with absolute CVs > 10, most related to positive SC. This result indicates that compared with other items, these SC items with larger CV reflected that the participants had more relative variation, either decrease or increase in their perception of "self" before/after the disease diagnosis. Yet the different directions of these item impact scores were canceled at the sub-domain level resulting in negligible impact scores. As items with larger CVs have the potential to discriminate against survivors with different levels of impact, these items could be considered candidates to detect individual differences over time. However, we should use CVs with caution. When the denominator (i.e., impact mean) is close to zero, the CV becomes very sensitive to small changes in the mean48. This condition occurs when participants’ impact scores show variation, but positive and negative scores offset the mean of impact scores.
Our results on age, gender, and income level are consistent with the literature43, 45, 47, 49,50,51,52,53,54,55. We found younger survivors reported greater life disruptions yet simultaneously reported a more positive attitude towards the disease. Female survivors reported a more positive attitude, but there is no gender difference in negative attitudes toward the disease. Survivors with lower income report more negative psychosocial impacts from cancer. However, the literature does not provide a consistent pattern about education, ethnicity, and relationship status in the psychosocial impacts of cancer45, 50, 52, 54, 55. Our study found survivors with higher education have a more positive attitude toward the disease. No significant differences were found in ethnicity and relationship status. Future studies on different sample groups should be conducted to evaluate the replicability of our findings.
This study had some limitations. Our sample was not nationally representative; there was an over-representation of well-educated and White survivors. Replication of our results with a more diverse set of survivors is needed. Another limitation is that we relied on survivors to recall their experiences before diagnosis, as it is not practical to conduct a prospective study, enrolling people before a cancer diagnosis. We attempted to minimize recall bias by implementing an appropriate question format by asking survivors to answer each item content with a before/after format; subsequently, the “before” question could be the reference for the “current” question. Our sample had an average time since cancer diagnosis of 4.7 years; thus, the recall accuracy was questionable. Future studies that evaluate psychosocial impacts at different stages of the disease continuum longitudinally, e.g., every year or every six months post-diagnosis, should be conducted to establish trajectory patterns of impact over time. In addition, we collected in this study from participants' self-reported perceived change, which might not be their veridical change. Boals and colleagues distinguished perceived and veridical stress-related growth and presented four possible constructs to shape perceived growth: (a) adherence to a cultural script, (b) reappraisal coping through secondary control or self-enhancement; (c) changes in narrative identity; and (d) violation of post-recovery expectations56. In other words, participants' perceived responses might be influenced by their cultures; they regulate their beliefs and reaction to fit the world's expectations by secondary control; they maintain personal continuity over time to face adverse experiences by autobiographical reasoning; and they attribute their experience by a convincing explanation. Perceived change may be a mix of these possible constructs. Future studies are needed to evaluate the replicability of our findings.
This study result may have implications for strategies in managing cancer survivors to promote their healthy adjustment to cancer throughout the disease continuum. The clinical focus of this research includes the impacts of cancer on self-concept, stress responses, social relationships, and spirituality; for example, to promote survivors’ quality of life after a cancer diagnosis, clinical practitioners can facilitate survivors’ positive consequences and alleviate negative ones.
In conclusion, this study expanded our prior work on the development of positive and negative psychosocial impact measures by requesting cancer survivors to report psychosocial impacts comparing before and after their cancer diagnosis26. Further, measures independently assessing the positive and negative psychosocial sequelae of illness allow for a more comprehensive measurement of how cancer affects individuals over time. Understanding these impacts sets the stage for developing interventions that can enhance the quality of life for survivors.
Data availability
The dataset can be accessed through the Healthmeasure Dataverse repository at https://dataverse.harvard.edu/dataverse/HealthMeasures.
References
American Cancer Society [homepage on the internet]. Managing Cancer as a Chronic Illness [Cited 2022 Jan. 3]. Available from https://www.cancer.org/treatment/survivorship-during-and-after-treatment/long-term-health-concerns/cancer-as-a-chronic-illness.html.
Cordova, M. J. et al. Frequency and correlates of posttraumatic-stress-disorder like symptoms after treatment for breast cancer. J. Consult. Clin. Psychol. 63(6), 981–986 (1995).
Derogatis, L. R. et al. The prevalence of psychiatric disorders among cancer patients. JAMA 249(6), 751–757 (1983).
Kornblith, A. B. Psychosocial adaption of cancer survivors. In Psych-Oncology (ed. Holland, J. C.) 223–254 (Oxford University Press, 1998).
Moyer, A. & Salovey, P. Psychosocial sequelae of breast cancer and its treatment. Ann. Behav. Med. 18, 110–125 (1996).
Stanton, A. L., Collins, C. A. & Sworowski, L. A. Adjustment to chronic illness: Theory and research. In Handbook of Health Psychology (eds Baum, A. et al.) 387–403 (Lawrence Erlbaum Associates, 2001).
Zabora, J., BrintzenhofeSzoc, K., Curbow, B., Hooker, C. & Piantadosi, S. The prevalence of psychological distress by cancer site. Psychooncology 10(1), 19–28 (2001).
Hewitt, M., Greenfield, S., & Stovall, E. From cancer patient to cancer survivor: Lost in transition. In American Society of Clinical Oncology and Institute of Medicine Symposium. (National Academies Press, Washington, D.C., 2006). https://doi.org/10.17226/11613
Adler, N.E., & Page, A. Institute of Medicine Committee on Psychosocial Services to Cancer Patients/Families in a Community. In Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs (National Academies Press, Washington, DC, 2008).
Reuben, S. H. Living beyond cancer: Finding a new balance. President’s cancer Panel 2003–2004 annual report (National Cancer Institute, Bethesda, MD, 2004).
Seligman, M. E. P. Positive psychology, positive prevention, and positive therapy. In Handbook of Positive Psychology (eds Snyder, C. R. & Lopez, S. J.) (Oxford University Press, 2002).
Seligman, M. E. P. Authentic Happiness: Using the New Positive Psychology to Realize Your Potential for Lasting Fulfillment (Free Press, 2002).
Andrykowski, M. A., Brady, M. J. & Hunt, J. W. Positive psychosocial adjustment in potential bone marrow transplant recipients: Cancer as a psychosocial transition. Psychooncology 2, 261–276 (1993).
Bellizzi, K. M. Expressions of generativity and posttraumatic growth in adult cancer survivors. Int. J. Aging. Hum. Dev. 58(4), 267–287 (2004).
Bellizzi, K. M. & Blank, T. O. Predicting posttraumatic growth in breast cancer survivors. Health Psychol. 25(1), 47–56 (2006).
Cordova, M. J., Cunningham, L. L., Carlson, C. R. & Andrykowski, M. A. Posttraumatic growth following breast cancer: A controlled comparison study. Health Psychol. 20(3), 176–185 (2001).
Park, C. L. & Lechner, S. C. Measurement issues in assessing growth following stressful life experiences. In Handbook of Posttraumatic Growth: Research and Practice (eds Calhoun, L. G. & Tedeschi, R. G.) 47–67 (Lawrence Erlbaum Associates, 2006).
Petrie, K. J., Buick, D. L., Weinman, J. & Booth, R. J. Positive effects of illness reported by myocardial infarction and breast cancer patients. J Psychosom. Res. 47, 537–543 (1999).
Sears, S. R., Stanton, A. L. & Danoff-Burg, S. The yellow brick road and the emerald city: Benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychol. 22(5), 487–497 (2003).
Tedeschi, R. G., Park, C. L. & Calhoun, L. G. Posttraumatic growth: Positive change in the aftermath of crisis. In The LEA Series in Personality and Clinical Psychology (Lawrence Erlbaum Associates, 1998).
Tomich, P. L. & Helgeson, V. S. Five years later: A cross-sectional comparison of breast cancer survivors with healthy women. Psychooncology 11(2), 154–169 (2002).
Tomich, P. L. & Helgeson, V. S. Is finding something good in the bad always good? Benefit finding among women with breast cancer. Health Psychol. 23(1), 16–23 (2004).
Tedeschi, R. G. & Calhoun, L. G. Trauma and Transformation: Growing in the Aftermath of Suffering (Sage, 1995).
Cella, D. et al. The patient-reported outcomes measurement information system (PROMIS): Progress of an NIH roadmap cooperative group during its first two years. Med. Care 45(5 Suppl 1), S3–S11 (2007).
PROMIS Instrument Development and Validation Scientific Standards Version 2.0 (revised May 2013). https://www.mcgill.ca/can-pro-network/files/can-pro-network/promisstandards_vers2.0_final.pdf.
Lai, J. S., Garcia, S. F., Salsman, J. M., Rosenbloom, S. & Cella, D. The psychosocial impact of cancer: Evidence in support of independent general positive and negative components. Qual Life Res. 21(2), 195–207 (2012).
Salsman, J. M., Garcia, S. F., Lai, J. S. & Cella, D. Have a little faith: Measuring the impact of illness on positive and negative aspects of faith. Psychooncology 21(12), 1357–1361 (2012).
Yao, G. Research on Cancer Patients’ Positive and Negative Psychosocial Impacts: Validation of the Psychometric Properties of the PROMIS Psychosocial Illness Impact Scale (National Taiwan University, 2018).
Lai, J. S. et al. Parent-reported cognitive function is associated with leukoencephalopathy in children with brain tumors. Qual. Life Res. 26(9), 2541–2550. https://doi.org/10.1007/s11136-017-1583-8 (2017).
Schover, L. R. The impact of breast cancer on sexuality, body image, and intimate relationships. CA Cancer J. Clin. 41(2), 112–120. https://doi.org/10.3322/canjclin.41.2.112 (1991).
Sharpe, L., Patel, D. & Clarke, S. The relationship between body image disturbance and distress in colorectal cancer patients with and without stomas. J. Psychosom. Res. 70(5), 395–402. https://doi.org/10.1016/j.jpsychores.2010.11.003 (2011).
Life after Cancer: Social & Emotional Impacts of Cancer. MD Anderson cancer center, The University of Texas. https://www.mdanderson.org/patients-family/life-after-cancer/social-emotional-impacts.html (2023).
Pereira, M. A., Araújo, A., Simões, M. & Costa, C. Influence of psychological factors in breast and lung cancer risk: A systematic review. Front Psychol. 12, 769394. https://doi.org/10.3389/fpsyg.2021.769394 (2022).
Burger, J. et al. Reporting standards for psychological network analyses in cross-sectional data. Psychol. Methods 28, 806–824 (2023).
Agha, R., Mathew, G., & STROCSS Group. STROCSS 2021: Strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int. J. Surg. 37, 106165 (or) Ann. Med. Surg. (Lond.). 72, 103026. PMID: 34820121 (2021).
Boursier, J. et al. An extension of STARD statements for reporting diagnostic accuracy studies on liver fibrosis tests: the Liver-FibroSTARD standards. J. Hepatol. 62(4), 807–815 (2015).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences 2nd edn. (Lawrence Erlbaum, 1988).
Everitt, B. The Cambridge Dictionary of Statistics (Cambridge University Press, 1998).
Zady, M. F. Z-4: Mean, standard deviation, and coefficient of variation, Z-Stats/Basic Statistics. https://www.westgard.com/lesson34.htm#6 (2023).
Castellano-Tejedor, C. et al. Perceived positive and negative consequences after surviving cancer and their relation to quality of life. Scand. J. Psychol. 56, 306–314 (2015).
Engvall, G., Cernvall, M., Larsson, G., von Essen, L. & Mattsson, E. Cancer during adolescence: Negative and positive consequences reported three and four years after diagnosis. PLoS ONE 6(12), e29001 (2011).
Lehmann, V. et al. Negative and positive consequences of adolescent cancer 10 years after diagnosis: An interview-based longitudinal study in Sweden. Psychooncology 23(11), 1229–1235 (2014).
Park, C. L. & Blank, T. O. Associations of positive and negative life changes with well-being in young and middle-aged adult cancer survivors. Psychol. Health. 27(4), 412–429 (2012).
Schroevers, M. J., Kraaij, V. & Gamefski, N. Cancer patients’ experience of positive and negative changes due to the illness: Relationships with psychological well-being, coping, and goal reengagement. Psychooncology 20, 165–172 (2011).
Costa, D. S. J. et al. The impact of cancer on psychological and social outcomes. Aust Psychol. 51, 89–99 (2016).
Updegraff, J. A. & Taylor, S. E. From vulnerability to growth: Positive and negative effects of stressful life events. In Loss and Trauma: General and Close Relationship Perspectives (eds Harvey, J. & Miller, E.) 3–28 (Brunner-Routledge, 2000).
Tedeschi, R. G. & Calhoun, L. G. The posttraumatic growth inventory: Measuring the positive legacy of trauma. J. Trauma Stress. 9, 455–471. https://doi.org/10.1007/bf02103658 (1996).
Hayes, A. Co-efficient of Variation Meaning and How to Use It. https://www.investopedia.com/terms/c/coefficientofvariation.asp (2023).
Bellizzi, K. M. et al. Positive and negative psychosocial impact of being diagnosed with cancer as an adolescent or young adult. Cancer 118(20), 5155–5162 (2012).
Rowlands, I. J. et al. Australian National Endometrial Cancer Study Group Predicting positive and negative impacts of cancer among long-term endometrial cancer survivors. Psychooncology 22(9), 1963–1971 (2013).
Groarke, A., Curtis, R. & Kerin, M. Global stress predicts both positive and negative emotional adjustment at diagnosis and post-surgery in women with breast cancer. Psychooncology 22(1), 177–185 (2013).
Bouskill, K. & Kramer, M. The impact of cancer and quality of life among long-term survivors of breast cancer in Austria. Support Care Cancer. 24, 4705–4712 (2016).
Zebrack, B. J. & Landier, W. The perceived impact of cancer on quality of life for post-treatment survivors of childhood cancer. Qual. Life Res. 20(10), 1595–1608 (2011).
Zebrack, B. J. et al. Perceived positive impact of cancer among long-term survivors of childhood cancer: a report from the childhood cancer survivor study. Psychooncology 21(6), 630–639 (2012).
Benedict, C. et al. Positive and negative mood in men with advanced prostate cancer undergoing androgen deprivation therapy: Considering the role of social support and stress. Psychooncology 24(8), 932–939 (2015).
Boals, A., Jayawickreme, E. & Park, C. L. Advantages of distinguishing perceived and veridical growth: recommendations for future research on both constructs. J. Posit. Psychol. 18(5), 773–783. https://doi.org/10.1080/17439760.2022.2109200 (2022).
Funding
This project was supported by the National Cancer Institute (CA60068, PI: David Cella) and the National Institutes of Health through the NIH Roadmap for Medical Research (5U54 AR057951, PI: David Cella) and the HealthMeasures (U2C CA186878; PI: David Cella). Dr. Yao was supported by the senior research grant from Fulbright Taiwan and the Ministry of Science and Technology (MOST), Taiwan (105-2918-I-002-006, 106-2410-H-002 -081 –SSS, 108-2410-H-002-100-, 109-2410-H-002-091-SS2), and National Science & Technology Council (NSTC), Taiwan (111-2410-H-002-159-MY2).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. J.S.L., S.F.G., S.Y., and D.C. developed PROMIS Psychosocial Illness Impact item banks. G.Y. designed this study and performed all statistical analyses. G.Y. and J.S.L. wrote the first draft of the manuscript and all authors commented on previous versions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yao, G., Lai, JS., Garcia, S.F. et al. Positive and negative psychosocial impacts on cancer survivors. Sci Rep 13, 14749 (2023). https://doi.org/10.1038/s41598-023-41822-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-41822-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.