Abstract
To investigate the clinical effects of specific Unified Classification System B (UCS B)-lesser trochanter periprosthetic fractures and determine whether they occur only with non-cemented stems. A retrospective analysis of 28 patients with specific UCS B2 fractures who underwent two surgical treatments, longer stem revision and internal fixation (LSRIF) and open reduction and internal fixation (ORIF), was performed. The patients were assessed at 1, 3, 6, 12, and 24 months and annually thereafter. Fracture healing, complications, Harris Hip Score (HHS), and the Short Form Health Survey questionnaire (SF-36) quality of life score were assessed at each follow-up. At the time of the last follow-up, seven patients had been lost: three were lost to contact, two died, and two were hospitalised elsewhere and unavailable for follow-up. The remaining 21 patients were followed for an average of 49.3 ± 15.4 (range: 24–74.4) months. Their average fracture healing time was 13.5 ± 1.1 (12–15.4) weeks. Complications included three cases (10.71%) of thrombus, one (3.57%) of heart failure, and one (3.57%) of pulmonary infection. There were no revisions due to prosthesis loosening, subsidence, or infection. At the last follow-up, the HHS, SF-36 mental score, and SF-36 physical score were recorded, LSRIF vs. ORIF (82.9 ± 6.6 vs. 74.7 ± 3.9, p = 0.059; 50.9 ± 7.6 vs. 38 ± 1.4, p = 0.012, and 51.7 ± 8.4 vs. 39.7 ± 3.4, p = 0.032, respectively). Specific UCS B2 fractures mostly occur with non-cemented stems. LSRIF with cables is the main treatment, while ORIF is an option for those elderly in poor condition.
Similar content being viewed by others
Introduction
Periprosthetic femur fracture (PPFF) is an acute complication that often occurs after hip arthroplasty. Due to the increasing use of arthroplasty surgery and the aging population, the incidence of PPFF is increasing1,2,3,4.
The Vancouver Classification System (VCS)5 and subsequent Unified Classification System (UCS)6 were intended as simple systems for classifying fractures and guiding management. However, these two classifications do not include some special types of fracture. For example, Van Houwelingen and Duncan7 reported a type of periprosthetic fracture of the lesser trochanter that involved a segment of the proximal medial femoral cortex. This fracture is easily misidentified as an ALT fracture, but is actually type B2. Consequently, it is called a “pseudo ALT” or “new B2” fracture. Pseudo ALT fractures often occur in non-cemented stems7,8,9,10,11; the mechanism may involve an occult fracture resulting from surgical insertion, and the fractures occur during early weight-bearing rehabilitation.
To assess the importance to this type of fracture and improve the surgical outcome, we hypothesized pseudo ALT fractures occur only with non-cemented stems and examined how different surgical treatments of pseudo ALT fractures affect the clinical outcome.
Materials and methods
This study was approved by the Hospital Ethics Committee. All methods were carried out in accordance with relevant guidelines and regulations. All X-rays were preoperatively evaluated by two senior doctors to confirm the type of fracture. Any disagreement between two doctors was resolved by a third doctor. The final determination of whether the prosthesis was loose was made during the operation.
Inclusion and exclusion criteria
The inclusion criteria were confirmed pseudo ALT fractures on X-ray, surgical treatment, and complete clinical records and follow-up. Exclusion criteria were a combined (or suspected) infection, ipsilateral lower-extremity neurovascular injury, conservative (non-surgical) treatment, and incomplete follow-up.
Patient-related information
A search of the hospital database from January 2010 to July 2020 identified 28 patients. The patients’ basic data were collected, including gender, age, preoperative physical condition, surgical index, and type of stem.
Treatment methods
Two treatment methods were adopted. Longer stem revision and internal fixation (LSRIF) with cables was applied in 24 cases (Figs. 1 and 2). Open reduction and internal fixation (ORIF) with cables was done in four cases (Fig. 3). The choice of surgical treatment was based on the patient’s physical condition. The standard treatment was LSRIF, while ORIF was chosen if the patient was in poor condition and could not tolerate LSRIF.
Case 8, an 81-year-old woman. (A) Anterior–posterior radiograph after hemi-arthroplasty. (B) After a fall in the ward, the continuity of the left medial femoral cortex was disrupted on anterior–posterior and lateral radiographs. (C) Postoperative anterior–posterior radiograph shows the patient with a longer stem revision and internal fixation with cables.
Anticoagulant therapy with low-molecular-weight heparin was given postoperatively. Rehabilitation was based on the patient’s physical condition. Patients were allowed early weight bearing when the circumstances permitted; otherwise, they exercised in bed.
Follow-up
All patients were followed as outpatients at 1, 3, 6, 12, and 24 months and yearly thereafter. All surviving patients with complete follow-up were analysed. Fracture healing and the position of the prosthesis loosening were evaluated by X-rays at each visit. The Harris Hip Score (HHS)12 and Short Form Health Survey questionnaire (SF-36) quality of life score13 were also recorded. Fracture healing was assessed in terms of local tenderness, longitudinal percussion pain on the injured leg, local abnormalities, and blurred fracture lines with continuous callus passing through the fracture line on X-ray at the last follow-up. The fracture healing time was defined as the time from the second postoperative day to the end of follow-up if there were no special circumstances.
Statistical analysis
The data were analysed using SPSS software (ver. 22.0; SPSS Inc., Chicago, IL, USA). Data are expressed as mean ± standard deviation (SD). The groups were compared using t-tests. Count data are expressed as numbers or percentages. P-values < 0.05 were considered significant.
Ethical approval
Approved by the Ethics Committee of the First Affiliated Hospital of Zhejiang Chinese Medicine University, Ethics No. 2016-K-143-01.
Informed consent
Informed consent was obtained from all participants.
Results
Postoperative pseudo ALT fractures were seen in 28 patients (7 males [25% and 21 females [75%]). The age of the patients at surgery was 73.7 (range: 52–92) years. Of the cases, 27 (96.43%) occurred with non-cemented stems, and 1 (3.57%) with cemented stems (Fig. 4). The basic patient data are summarised in Table 1.
Case 1, an 82-year-old man underwent left hemi-arthroplasty with a cemented stem because of a left femoral neck fracture. (A–B) Two intraoperative radiographs taken with a C-arm machine. (C) After a fall, the continuity of the left medial femoral cortex was interrupted on an anterior–posterior radiograph. (D) Postoperative anterior–posterior radiograph after longer stem revision and internal fixation with cables.
At the time of the last follow-up, three patients were lost to contact, two died, and two were hospitalised elsewhere. The remaining 21 patients were followed for 49.3 ± 15.4 (24–74.4) months. These patients had a fracture healing time of 13.5 ± 1.1 (12–15.4) weeks.
Postoperative complications included thrombus in three cases (10.71%) and heart failure and pulmonary infection in one case each (both 3.57%). The patients with postoperative thrombosis all recovered on treatment with low-molecular-weight heparin. There were no revisions for prosthesis loosening, subsidence, or infection. The HHS and SF-36 scores were obtained scores those with complete follow-up (Table 2).
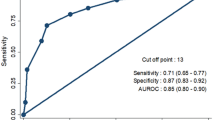
Of the 21 patients who completed follow-up, 18 (85.71%) underwent LSRIF and 3 (14.29%) underwent ORIF. At the last follow-up, the LSRIF and ORIF groups had an HHS of 82.9 ± 6.6 (range: 68–92) and 74.7 ± 3.9 (range: 71–80) (p = 0.059), SF-36 mental scores of 50.9 ± 7.6 (range: 38–64) and 38 ± 1.4 (range: 37–40) (p = 0.012), and SF-36-physical scores of 51.7 ± 8.4 (range: 36–67) and 39.7 ± 3.4 (range: 35–43), respectively (p = 0.032) (Table 3).
Discussion
The VCS divides fractures into three subtypes. Type A consists of fractures in the greater (AGT) and lesser (ALT) trochanteric areas. Type B fractures involve the metaphyseal or diaphyseal femur around the prosthetic stem: type B1 fractures occur around a stable stem; B2 fractures involve a loose stem with good bone quality; and B3 fractures involve bone loss. Type C fractures occur distal to the stem.
The UCS expanded and updated the VCS by adding three types. Type D is a femoral fracture occurring after hip or knee arthroplasty. Type E is a fracture of both the acetabulum and femur after hip arthroplasty. Type F is a fracture of the acetabulum after hemi-arthroplasty of the hip4,6 (Table 4).
However, some special fractures are not included. For example, a pseudo ALT/new B2 fracture occurs at the lesser trochanter extending into the medial cortex of the proximal femur7,8, 14,15,16,17,18 (Table 5). Consequently, modified classifications based on the VCS and UCS were proposed. Capello et al. proposed “A1 and A2” for well-fixed or loose stems in category A8. Huang et al. classified type B2 as B2PAGT and B2PALT, representing greater trochanter fractures including a segment of the proximal lateral femoral cortex and lesser trochanter fractures including a segment of the proximal medial femoral cortex, respectively15. Egrise et al. subdivided Vancouver B-lesser trochanter fractures (VB-LT) into stable (VB-LT1) and unstable (VB-LT2) fractures9. These are all actually B2/pseudo ALT fractures.
Pseudo ALT fractures often occur with non-cemented stems, especially tapered stems7,10,11. This may be due to an unrecognised intraoperative fracture that is subsequently displaced under load or during rehabilitation7,8,9,15, 16. Capello et al. reported nine newly described “clamshell” fractures that might be related to unrecognised fractures during operation and believed that they were directly related to the geometry of the tapered stem used8. Huang et al. mentioned that this type of fracture occurred at the lesser trochanter, including a segment of the proximal medial femoral cortex, and was associated with destabilisation of the stem15. Karam et al. showed that such fractures were significantly associated with non-cemented supports with an anatomical wedge-shaped design16. Egrise et al. thought this type of fracture can occur intraoperatively or in the early postoperative period with non-cemented implants, and is an occult intraoperative fracture9.
In our series, 27 patients with non-cemented stems (96.43%) sustained a PPFF. The mechanism was as described above. One fracture involved a cemented stem (3.57%); this patient had osteoporosis and it might have been an occult fracture that was not found intraoperatively.
There are three common treatments for new B2 fractures in PPFF: LSRIF, ORIF, and conservative treatment. When Van Houwelingen and Duncan recognised an undisplaced cortical crack, they performed cerclage cable fixation and revision with a longer stem, with protected weight-bearing for 6 weeks7. Capello et al. reported nine cases of pseudo ALT fracture caused by non-cemented femoral stems. They treated three cases conservatively without surgery because the stem subsidence stabilised during rehabilitation; the remaining six were treated by removing the loose stems and fixing the fracture and all healed well8; the remaining six were treated by removing the loose stems and fixing the fracture and all healed well8. Karam et al. adopted wedge-shaped (10 cases) and straight (20 cases) fixation treatments16. Egrise et al. treated nine VB-LT1 and six VB-LT2 in patients in poor health nonoperatively, 13 VB-T2 stems with exchange and cerclage, three with isolated stem exchange, and two with internal fixation by cerclage9. Huang et al.15 and González-Martín et al.17 treated this type with LSRIF.
In this study, of the 21 patients with complete follow-up, 18 underwent LSRIF and ORIF was used in 3 cases. The patient outcomes were determined by postoperative fracture-healing and functional assessment scores (HHS and SF-36). LSRIF had the better curative effect, not only in terms of the above but also from the average healing time of 13.4 ± 1.1 weeks. The LSRIF patients were aged 71.8 ± 10.9 (52–86) years and were younger than the ORIF patients (88 [range: 85–91] years). The mental and physical SF-36 scores were better with LSRIF (50.9 ± 7.6 and 51.7 ± 8.4, respectively) than with ORIF (38 ± 1.4 and 39.7 ± 3.4, respectively); we attributed this to the patients’ age and clinical condition. The HHS exceed 70 in all patients except case 1 (Table 2), indicating good functional recovery after surgery. The HHS of case 1 was 68, which we attributed to the patient’s poor basic condition and severe osteoporosis. Moreover, revision surgery with a cemented stem was more difficult than conventional LSRIF. Compared with LSRIF, ORIF is less invasive and is a suitable choice for the elderly with poor physical condition and low living needs3. Smitham et al. confirmed that the anatomical reduction and ORIF of type B2 fractures should be considered an appropriate treatment for frail elderly patients with a PPFF around cemented polished double-tapered stems14.
This study has some limitations. The patients were from a single hospital, limiting the generalisability of the results. Given the retrospective nature of the study, multicentre prospective research is needed.
Conclusion
Pseudo ALT fractures result mainly from unrecognised occult fractures intraoperatively and improper exercise postoperatively. They involve a posteromedial cortical fragment around the lesser trochanter and mainly occur with non-cemented stems. While the main treatment is LSRIF with cables/plates, simple ORIF can achieve good healing, especially for elderly patients in poor general condition.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Abdel, M. P., Watts, C. D., Houdek, M. T., Lewallen, D. G. & Berry, D. J. Epidemiology of periprosthetic fracture of the femur in 32644 primary total hip arthroplasties—A 40-year experience. Bone Joint J. 98-B, 461–467. https://doi.org/10.1302/0301-620X.98B4.37201 (2016).
Abdel, M. P., Watts, C. D., Houdek, M. T., Lewallen, D. G. & Berry, D. J. Epidemiology of periprosthetic femoral fractures in 5417 revision total hip arthroplasties—A 40-year experience. Bone Joint J. 98-B, 468–474. https://doi.org/10.1302/0301-620X.98B4.37203 (2016).
Fenelon, C. et al. Breaking bad: A comparative descriptive analysis of periprosthetic fractures around cemented and uncemented femoral stems. J. Arthroplasty. 34(8), 1783–1786. https://doi.org/10.1016/j.arth.2019.03.051 (2019).
Schopper, C. et al. The race for the classification of proximal periprosthetic femoral fractures: Vancouver vs Unified Classification System (UCS)—A systematic review. BMC Musculoskelet. Disord. 23(1), 280. https://doi.org/10.1186/s12891-022-05240-w (2022).
Duncan, C. P. & Masri, B. A. Fractures of the femur after hip replacement. Instr. Course Lect. 44, 293–304 (1995).
Duncan, C. P. & Haddad, F. S. The unified classification system (UCS): improving our understanding of periprosthetic fractures. Bone Joint J. 96-B(6), 713–716. https://doi.org/10.1302/0301-620X.96B6.34040 (2014).
Van Houwelingen, A. P. & Duncan, C. P. The pseudo A(LT) periprosthetic fracture: It’s really a B2. Orthopedics 34(9), e479–e481. https://doi.org/10.3928/01477447-20110714-27 (2011).
Capello, W. N., D’Antonio, J. A. & Naughton, M. Periprosthetic fractures around a cementless hydroxyapatite-coated implant: A new fracture pattern is described. Clin. Orthop. Relat. Res. 472(2), 604–610. https://doi.org/10.1007/s11999-013-3137-x (2014).
Egrise, F., Gastaud, O., Cointat, C., Raffaelli, A. & Tabutin, J. Identification and treatment of potentially destabilizing Vancouver B-lesser trochanter periprosthetic fracture (“New B2”): A 33-case series. Orthop. Traumatol. Surg. Res. 08(6), 103357. https://doi.org/10.1016/j.otsr.2022.103357 (2022).
Watts, C. D., Abdel, M. P., Lewallen, D. G., Berry, D. J. & Hanssen, A. D. Increased risk of periprosthetic femur fractures associated with a unique cementless stem design. Clin. Orthop. Relat. Res. 473(6), 2045–2053. https://doi.org/10.1007/s11999-014-4077-9 (2015).
Berend, K. R. et al. Cerclage wires or cables for the management of intraoperative fracture associated with a cementless, tapered femoral prosthesis: results at 2 to 16 years. J. Arthroplasty. 19(7 Suppl 2), 17–21 (2004).
Harris, W. H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Joint Surg. Am. 51, 737–755 (1969).
Tarlov, A. R. et al. The Medical Outcomes Study. An application of methods for monitoring the results of medical care. JAMA 262, 925–930 (1989).
Smitham, P. J. et al. Vancouver B2 peri-prosthetic fractures in cemented femoral implants can be treated with open reduction and internal fixation alone without revision. J. Arthroplasty. 34(7), 1430–1434. https://doi.org/10.1016/j.arth.2019.03.003 (2019).
Huang, J. F. et al. Modification of the Unified Classification System for periprosthetic femoral fractures after hip arthroplasty. J. Orthop. Sci. 23(6), 982–986. https://doi.org/10.1016/j.jos.2018.07.014 (2018).
Karam, J., Campbell, P., Desai, S. & Hunter, M. Periprosthetic proximal femoral fractures in cemented and uncemented stems according to Vancouver classification: Observation of a new fracture pattern. J. Orthop. Surg. Res. 15(1), 100. https://doi.org/10.1186/s13018-020-01619-4 (2020).
González-Martín, D. et al. New sub-classification of vancouver B2 periprosthetic hip fractures according to fracture pattern. Injury 53(3), 1218–1224. https://doi.org/10.1016/j.injury.2021.10.026 (2022).
Huang, J. F. et al. The reliability and validity of the Unified Classification System of periprosthetic femoral fractures after hip arthroplasty. Acta Orthop. Belg. 82(2), 233–239 (2016).
Funding
This work was supported by Hua Jiang Famous Expert Inheritance Studio of Traditional Chinese Medicine (GZS2021020).
Author information
Authors and Affiliations
Contributions
W.Q.Z.: Designed the study, Wrote the text, Approved the final version for submission. X.S.L.: Prepared the figures, analyzed and confirmed the data, Approved the final version for submission. M.Q.F.: Cases collected, Collected and analyzed the data, Approved the final version for submission. Z.Y.Y.: Cases collected, Collected and comfirmed the data, Approved the final version for submission. Z.F.S.: Collected and confirmed the data, Approved the final version for submission. P.J.T.: Collected and analyzed the data, Approved the final version for submission. J.F.H.: Designed the study, Wrote the text, Prepared the figures, Approved the final version for submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhao, WQ., Li, XS., Fan, MQ. et al. Surgical treatment of specific Unified Classification System B fractures: potentially destabilising lesser trochanter periprosthetic fractures. Sci Rep 13, 14330 (2023). https://doi.org/10.1038/s41598-023-41698-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-41698-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.