Abstract
The aim of this study was to evaluate how the Charlson Comorbidity Index (CCI) scores contribute to early recovery and 2-year mortality in elderly patients undergoing surgical treatment of inter-trochanteric fractures. 60 cases with unilateral intertrochanteric fracture were retrospectively analyzed and divided into Low-CCI group (CCI: 1–4) or high-CCI groups (CCI: 5–6). All the patients’ electronic hospital records were reviewed. The preoperative situations (demographic data, comorbidities and fracture conditions), perioperative situations (wait time, operation time, implant choice, blood loss, transfusion or not) and postoperative situations (complications, first time out of bed, function about 1-/2- week and 2-year mortality) were recorded. 51.67% were in low-CCI group and 48.33% in high-CCI group. The survival rates in low- and high-CCI group were 93.5% and 86.2% respectively. According to the functional results of 1- or 2- week after operation, no significant difference was found (P = 0.955, 0.140). Log-rank analysis showed that the main prognostic factors were blood loss, first time out of bed and complication (P < 0.05). Multivariate analysis confirmed that complication and first time out of bed were significant factor on survival rate (P = 0.029, 0.010). Charlson comorbidity index maybe not the indicator of 2-year mortality in older patients with intertrochanteric fractures. In order to improve the prognosis, more attentions should be paid to reduce the complications and encourage postoperative earlier excise out of bed.
Similar content being viewed by others
Introduction
As a common fracture in elderly people, the intertrochanteric fracture comprises about 8–10% of all fractures1. Although fracture is not the direct cause of death, it can induce a progressive deterioration of physical condition and increase the mortality. The mortality of intertrochanteric fractures displays a rising trend due to increased life expectancy and osteoporosis2.
Surgery usually supplies an earlier mobilization to reduce complications and mortality, and improves the independent living ability in older patients3. To now, surgery at the earliest opportunity has being the main choice for intertrochanteric fractures, but the relative higher mortality is still a major concern to our clinicians. The trauma reaction, physiological decline and underlying diseases are still the important issues requiring our emphasizing4. Considering the difficulty and complexity, understanding the risk factors of mortality is very important for supplying safer and better treatment.
Charlson comorbidity index (CCI) is a system assigned to weigh the morbidity, which is used to assess the probability of survival5. Previous researches have confirmed that CCI is an important tool to predict the prognosis (30-, 90-days mortality) of patients with hip fractures6. Haentjens et al. used life-table method and found that women and men (older than 80 years old) having a hip fracture often brought them with excess annual mortality at 1, 2, 5 and 10 years after injury7. Considering the following deleterious effects of hip fractures, earlier evaluating the risk factors about the mid- to long-term mortality are very important.
The aim of this present study was to evaluate the role of Charlson comorbidity index (CCI) on 2-year mortality in older patients with intertrochanteric fractures. In addition, we investigated other main risk factors influencing the prognosis.
Materials and methods
This retrospective study was designed and approved by the Ethics Review Committee of Juntendo University. All methods were performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from all patients.
From Jan. 2013 to Dec. 2017, 71 patients with intertrochanteric fractures were retrospectively analyzed. Of them, 11 patients were excluded: 7 patients with conservative treatment, 2 patients with multiple fractures and 2 patients under 65.
60 patients, ASA I-IV, aged 65–100 (average, 81.70 ± 8.13), BMI 14.7–29.42 (average, 21.34 ± 3.45), unilateral intertrochanteric fractures were analyzed finally. Of them, 17 males and 43 females. The preoperative wait time was 2–21 (average, 7.37 ± 3.83) days. The fractures were classified according to AO/ASIF system, in which 25 type A1 fractures, 33 type A3 fractures and 2 type A3 fractures. All the enrolled patients got surgery with intramedullary nail (59 cases) or dynamic hip screw (only 1 case). The CCI score was assessed first and divided the enrolled patients into Low-CCI group (n = 31; CCI: 1–4) and High-CCI group (n = 29; CCI: 5–6).
The inclusion criteria were aged over 65; unilateral intertrochanteric fractures with surgery; no other diseases before affecting the lower limb function; a complete clinical data. Some patients were excluded if they were younger than 65; if they chose conserve therapy; if they had pathological fractures; if they had diseases before affecting the lower limb function; if their clinical data defected.
No significant correlation was found in age, gender, side, AO type, stability, low limber surgery, preoperative wait time, complication, transfusion, implant style, ASA classification, wait days, blood loss, comorbidities, operation time and first time out of bed (P > 0.05, Table 1).
The operations were performed by the same team major in hip. According to the regime of our rehabilitation, the physiotherapist would help patients to mobilize from the second day after operation. The patients attended rehabilitation twice a day. If possible, they would excise out of bed as early as possible (usually the second day after operation). The following rehabilitation projects mainly based on patients’ own physical conditions to accelerate muscle strength, limb coordination and body balance recovery.
Study clinical parameters
Follow-up was defined from the operation day. 2-year mortality was defined the survival rate of all enrolled patients at 2 year.
The preoperative situations (demographic data and comorbidities), perioperative situations (wait time, operation time, implant choice, blood loss, transfusion or not) and postoperative situations (complications, first time out of bed and 2-year mortality) were got from the patients’ electronic hospital records. And all the data was manual reviewed independently by two different researchers.
Radiographic evaluation
The fracture classification and stability8 were assessed independently by two different radiologists using PACS system.
Functional evaluation
Functional result at 1-week or 2-week: The function was evaluated by two doctors based on rehabilitation record. The classifications listed as follow: no walking (The patients couldn’t walk even with a walker), walking with walker (The patients could walk with a walker), walking with stick (The patients could walk with a stick) and self-walking (The patients could walk without any help).
Statistical analysis
SPSS 24.0 (SPSS Inc, Chicago, IL, USA) was employed for all statistical analyses. Kolmogorov–Smirnov test was used to assess the normality distribution of continuous variables. Mean (standard deviation) or median (interquartile range) were used as appreciate. The t-test or χ2 test were used to evaluate difference or association between groups. The relationships between the survival and possible risk factors were assessed by univariate log rank test, Cox’s proportional hazards regression model with a forward conditional stepwise procedure was employed to determine the acting factors. Kaplan–Meier curves were plotted to assess the differences in 2-year mortality. The significance level was set at P < 0.05.
Results
All 60 patients got followed-up and bone united uneventfully. Of them, 51.67% were in low-CCI group and 48.33% in high-CCI group. All survival data were available and the survival rates in low- and high-CCI group were 93.5%, 86.2% respectively (Fig. 1). Three complications were found postoperatively. One patient got urinary tract infection and was cured by antibiotic treatment. Two others had pressure sore, and the wound healed after dressing change. No other secondary displacement, superficial or deep infection was found.
The earlier postoperative functional results of the low- and high-CCI groups
According to the functional results of 1- or 2- week after operation, no significant difference was found between low- and high-CCI groups (P = 0.955, 0.140, Table 2). The first time out of bed postoperatively is 1.29 ± 0.79 days.
At 1 week after operation, only 3 patients (5.0%, Table 2) could walk by themselves, 17 patients (28.3%, Table 2) couldn’t walk, and others needed the help of walker or stick. At 2 weeks after operation, 13 patients (21.7%, Table 2) could walk by themselves, only 5 patients (8.3%, Table 2) couldn’t walk, and others needed the help of walker or stick.
The prognostic factors and survival postoperatively
Log-rank analysis showed that the main prognostic factors were blood loss, first time out of bed and complication (P < 0.05, Table 3). No significant correlation was found with other factors (P > 0.05, Table 3).
Multivariate analysis of prognostic factors in patients with intertrochanteric fractures
Multivariate analysis confirmed that complication and first time out of bed were significant factor on survival rate (P = 0.029, 0.010, Table 4).
Discussion
Surgery at the earliest opportunity has being the main choice for intertrochanteric fractures in older patients. However, the relative higher mortality is still a major concern to our clinicians. Schurch et al. proposed a prospective survey of hip fracture and found that the 1-year mortality reached to 23.8%. Only 62.6% patients returned to their previous living after one year, and more care-intensive environment were still needed in 17.9% patients9. Kusen et al. implemented a multidisciplinary care pathway to improve the prognosis of older Patients with traumatic hip fractures. And they found that it could significantly reduce the mortality by 2.9% at 30 days, 3.4% at 90 days and 0.1% at 1 year10. Understanding and processing the risk factors of mortality in time maybe a prefer choice to reduce postoperative mortality. Our study demonstrated that the overall mortality rate was just 10.0%. Only three complications (1 urinary tract infection and 2 pressure sores) were found postoperatively. No other secondary displacement, superficial or deep infection was found.
Charlson comorbidity index (CCI)
CCI was a most widely comorbidity measure method used to assess the probability of survival. Previous research had confirmed that CCI was an important tool to predict the prognosis (30-, 90-days mortality) of patients with hip fractures. What’s more, the CCI had been confirmed to predict in-hospital mortality and readmission after orthopaedic surgery accurately11,12.
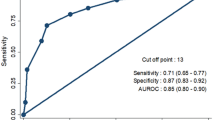
Considering the following deleterious effects of hip fractures, earlier evaluating the risk factors about the mid- to long-term mortality are very important. Lei Jiang et al. retrospective analyzed 1057 hip fracture patients aged above 60 years and found that Charlson comorbidity index was correlated with 5-year mortality after surgery13. In proximal humerus fractures, patients with high CCI (≥ 5) had a higher mortality risk 4.6 (95% CI [2.4–9.0]) compared to those with CCI < 5. According to the ROC curve analysis, the previous study confirmed the optimal cutoff value for the CCI was ≥ 3.5 for death after hip fracture surgery14. In this present study, we divided the enrolled patients into two groups: Low-CCI group (n = 31; CCI: 1–4) and High-CCI group (n = 29; CCI: 5–6). We analyzed the risk factors about 2-year mortality in older patients with intertrochanteric fractures. But no significant relationship was found between CCI and mortality rate in this present study. Maybe small sample size and age composition were main influence factors. The average age of all enrolled patients was 81.7 ± 8.1 years old, and patients ≥ 80 was about 63.9% (39/61).
Gilbert et al. had got the similar conclusion and thought that high comorbidity index was not related with high morbidity and mortality15. But they also pointed out that constrained total hip arthroplasty provided better function to the elderly patients with intertrochanteric fractures. Palanisamy et al. compared the functional outcomes in geriatric hip fractures between different implants. The final results showed that in patients with high CCI, THR usually provided faster recover16. Whether CCI combined with other factors can bring better clinical significance? It remains to be further studied in future.
Complications
Compared with intra-capsular fracture, patients with intertrochanteric fractures usually accompanied with increased blood loss17. It’s a potential reason for hypotension and hemodynamic disturbance during perioperative period. These fluctuations predisposed the higher complication rate. Chen et al. analyzed the risk factors for 1-year mortality in patients with acute hip surgery and strongly recommended that controlling and co-caring postoperative complications could significantly reduce the mortality18.
In our present study, multivariate analysis confirmed that complication was a significant factor on survival rate. Other studies had also got the similar conclusions. Zhao et al. performed a multivariate analysis and found that BNP, APACHE II score and complications after fracture were reference indexes for predicting perioperative mortality in elderly patients with intertrochanteric fracture19. Therefore, it is very important to control complications during perioperative period.
First-time out of bed
Earlier mobilization has been regarded as an important factor for better function after lower limb surgery. It can reduce complications and improve the independent living ability in older patients20. In present study, the mean first time out of bed postoperatively was 1.29 ± 0.79 days under the guidance of physiotherapist. The earlier weight-bearing time was much shorter than others’ reports. Duymus et al compared the result of intra- and extramedullary implants in treatment of intertrochanteric fractures and found that proximal femoral nail had better clinical results. The full weight-bearing time was significantly reduced to 1.25 ± 0.40 months21.
Our multivariate analysis confirmed that first time out of bed was a significant factor on survival rate. And we thought earlier weight-bearing is a better method to reduce the rate of complications and mortalities. Some surgeons worried that earlier weight bearing would bring a higher implant failure rate, but our follow-up study didn’t lead to a higher failure rate. In our hospital, the physiotherapists usually help patients weight bearing from the second day after operation if permitted. And the rehabilitation content was adjusted simply according to the actual situation of each patient. Early mobilization can accelerate muscle strength, limb coordination and body balance recovery. Of course, the lower BMI in Japan may have some impact on higher failure rate. To now, there is no sufficient evidence to determine the better weight bearing time. Further studies are needed to be conducted to express it and related risk factors.
At present, there is another view that arthroplasty was a prefer choice for older patients with intertrochanteric fractures. It provided an earlier weight bearing and better functional prognosis22. However, there is still controversial about arthroplasty or internal fixation23.
Limitations
Some limitations could be found in this study. First, it’s a retrospective study with small sample size. The small size reduced the power but provided our own real experience. Second, as a large private hospital, frequently-used hip function scoring standards were not regularly registered. And we used our own semi-quantitative based on the patients’ electronic hospital records. Third, due to Japanese medical system, not all patients were died in our hospital. The concrete causes of death were still uncertain Fourth, this retrospective study just came from our own hospital, and multicenter and more sample studies are necessary in future.
Conclusion
Therefore, Charlson comorbidity index maybe not the indicator of 2-year mortality in older patients with intertrochanteric fractures. In order to improve the prognosis, more attentions should be paid to reduce the complications and encourage postoperative earlier excise out of bed.
Data availability
All data generated or analyzed during this study are included in this published article and are available from the corresponding author on reasonable request.
References
Komur, B. et al. Evaluation of gamma nails in intertrochanteric fractures of femur and modified technique for removal. Open Access Libr J. 2, e2174 (2015).
Ha, Y. C. et al. Trend in hip fracture incidence and mortality in Korea: A prospective cohort study from 2002 to 2011. J. Korean Med. Sci. 30(4), 483–488 (2015).
Valera, M., Bonifacio, L. & Basman, S. Outcome of surgery for unstable intertrochanteric fractures in octogenarians. Malays. Orthop. J. 8(1), 26–31 (2014).
American Academy of Orthopaedic Surgeons. Management of Hip Fractures in the Elderly: Evidence-Based Clinical Practice Guideline. http://www.aaos.org/research/guidelines/HipFxGuideline.pdf.
Charlson, M., Szatrowski, T. P., Peterson, J. & Gold, J. Validation of acombined comorbidity index. J. Clin. Epidemiol. 47(11), 1245–1251 (1994).
Kirkland, L. L. et al. The Charlson comorbidity index score as a predictor of 30-day mortality after hip fracture surgery. Am. J. Med. Qual. 26(6), 461–467 (2011).
Haentjens, P. et al. Meta-analysis: Excess mortality after hip fracture among older women and men. Ann. Intern. Med. 152(6), 380–390 (2010).
Cho, Y. C. et al. Three-dimensional CT improves the reproducibility of stability evaluation for intertrochanteric fractures. Orthop. Surg. 10(3), 212–217 (2018).
Schurch, M. A. et al. A prospective study on socioeconomic aspects of fracture of the proximal femur. J. Bone Miner. Res. 11, 1935–1942 (1996).
Kusen, J. Q. et al. The implementation of a Geriatric Fracture Centre for hip fractures to reduce mortality and morbidity: An observational study. Arch. Orthop. Trauma Surg. 139(12), 1705–1712 (2019).
Neuhaus, V., King, J., Hageman, M. G. & Ring, D. C. Charlson comorbidity indices and in-hospital deaths in patients with hip fractures. Clin. Orthop. Relat. Res. 471(5), 1712–1719 (2013).
Voskuijl, T., Hageman, M. & Ring, D. Higher Charlson comorbidityindex scores are associated with readmission after orthopaedicsurgery. Clin. Orthop. Relat. Res. 472(5), 1638–1644 (2014).
Jiang, L. et al. Charlson comorbidity index predicts 5-year survivorship of surgically treated hip fracture patients. Geriatr. Orthop. Surg. Rehabil. 21, 9. https://doi.org/10.1177/2151459318806442 (2018).
Fernández-Cortiñas, A. B. et al. Is the Charlson comorbidity index a good predictor of mortality and adverse effects in proximal humerus fractures?. Orthop. Traumatol. Surg. Res. 105(2), 301–305 (2019).
Maroun, G. et al. High comorbidity index is not associated with high morbidity and mortality when employing constrained arthroplasty as a primary treatment for intertrochanteric fractures in elderly patients. Eur. J. Orthop. Surg. Traumatol. 29, 1009–1015 (2019).
Palanisamy, A. M. et al. Fixation versus replacement in geriatric hip fractures: Does functional outcome and independence in selfcare difer?. Geriatr. Orthop. Surg. Rehabil. 6(4), 258–262 (2015).
Smith, G. H., Tsang, J., Molyneux, S. G. & White, T. O. The hidden blood loss after hip fracture. Injury 42(2), 133–135 (2011).
Chen, C. H. et al. Impact of orthogeriatric care, comorbidity, and complication on 1-year mortality in surgical hip fracture patients: An observational study. Medicine 98(47), e17912 (2019).
Zhao, F. et al. Analysis of risk factors for perioperative mortality in elderly patients with intertrochanteric fracture. Eur. J. Orthop. Surg. Traumatol. https://doi.org/10.1007/s00590-018-2285-9 (2018).
Luciani, D. et al. The importance of rehabilitation after lower limb fractures in elderly osteoporotic patients. Aging Clin. Exp. Res. 25(1), 113–115 (2013).
Duymus, T. M. et al. Comparison of intra- and extramedullary implants in treatment of unstable intertrochanteric fractures. J. Clin. Orthop. Trauma. 10(2), 290–295 (2019).
Yoo, J. I. et al. Early rehabilitation in elderly after arthroplasty versus internal fixation for unstable intertrochanteric fractures of femur: systematic review and meta-analysis. J. Korean Med. Sci. 32(5), 858–867 (2017).
Parker, M. J. & Handoll, H. H. Replacement arthroplasty versus internal fixation for extracapsular hip fractures in adults. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD000086.pub2 (2006).
Author information
Authors and Affiliations
Contributions
X.J. and Y.J. wrote the main manuscript. H.Y. and T.B. designed the study and managed overall process. Z.X. and T.W. undertook data management and statistical analysis. S.B. and K.K. contributed to data management and literatures review. All authors have approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jianda, X., Homma, Y., Jinnai, Y. et al. Relationship between Charlson comorbidity index, early recovery and 2-year mortality in elderly patients undergoing surgical treatment of inter-trochanteric fractures: a retrospective analysis. Sci Rep 11, 17195 (2021). https://doi.org/10.1038/s41598-021-96765-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-96765-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.