Abstract
Constipation affects almost 50% of critically ill pediatric patients and is related to their morbidity and mortality. However, little attention is paid to it and it is diagnosed late and when there are already complications. The objective of this study is to develop and validate a score to identify critically ill children with high risk of constipation 48 h after admission. A single center two phase-study was carried out; the first one (retrospective observational study) to develop the score and the second one to validate it in another prospective observational study. Children between 15 days of life and 18 years old admitted to the PICU for more than 3 days were included. Demographic and clinical data during the first 48 h after PICU admission were collected. Univariate and multivariate analysis and ROC curves were used to develop and validate the score. Data from 145 patients (62.8% boys) with a mean age of 34.9 ± 7.3 months were used to develop the score. Independent factors identified to develop the score were: weight > 7 kg, admission to PICU after surgery, need of vasoconstrictors, doses of fentanyl ≥ 2 mcg/kg/h, and initiation of enteral nutrition later than 48 h after admission. Two cut-off values were identified to set low constipation risk (< 5.7 points) and high constipation risk (> 6.2 points). This score was validated in 124 patients showing a sensibility of 63.2%, specificity of 95.5% and a positive/negative predictive values (P/NPV) of 100% and 82.1% respectively to identify constipated patients. This is the first score to identify high constipation risk in critically ill children. This score is easy to apply, and internal validation has shown a PPV of 100%.
Similar content being viewed by others
Introduction
Within the last two decades, health professionals have become aware of the importance of constipation in Intensive Care Units (ICU), and constipation is now perceived to be increasingly important1,2,3,4,5. However, no standard definition has been universally accepted (children or adults)1,2,5,6,7. Rome criteria8,9 are not valid for critically ill patients because in these patients, constipation is a multifactorial disorder frequently related to sedative and vasoconstrictor drugs1,10,11,12, hypotension13 and immobility14, not a functional one15. This lack of definition is one of the main obstacles to reach an early diagnosis.
Besides, constipation diagnosis is frequently delayed due to it is considered a less severe complication in critically ill patients4,16 compared to hemodynamic, respiratory, or renal problems. However, constipation has been related in critically ill adult patients to delirium17, higher illness clinical severity13,18, longer duration of mechanical ventilation (MV)13, ventilator weaning19, ICU and hospital length of stay3,5,10,13,20,21 and higher hospital costs5. In critically ill children has been related to higher illness clinical severity1. Frequently, diagnosis is delayed until constipation is well established and complications due to constipation are already present. At this point, treatment is more difficult because of a lack of tolerance to EN and because some treatments are contraindicated when ileus is present20,22.
In pediatric patients, we found that 46.7% of children admitted to the Pediatric Intensive Care Unit (PICU) suffered from constipation1. Some independent risk factors for constipation were identified in this population: higher body weight, higher severity of illness scores, admission after surgery and treatment with vasoconstrictors1,6. In critically ill adults, sedatives, admission after surgery and late enteral nutrition (EN) were identified as independent risk factors for constipation3.
The objective of this study was to elaborate an easy clinical score from our previous data that could be applied at 48 h after admission, to identify children with high risk of constipation and to validate it in a similar population.
Methods
We used data from a previous single center study designed to describe epidemiological factors of constipation in critically ill children followed up to 30 days or the PICU discharge1. With this data, we developed a score which was capable to detect high and low constipation risk just 48 h after PICU admission. After that, we prospectively obtained another sample in the same centre for 1 year to validate our score. Our PICU is a mixed unit (medical and surgical) with 400–450 annual admissions, of which almost 50% are postoperative cardiac surgery.
Inclusion criteria were children between 15 days of life and 18 years old admitted to the PICU for more than 3 days and whose parents or legal guards signed the consent form. Children with gastrointestinal disease presented prior to admission were excluded. Children from the first study with missing data during the first 48 h after admission and those children with constipation treatment before constipation definition was settled in the second study, were also excluded. For those children re-admitted 24 h after PICU discharge, only the first PICU admission was considered.
Constipation was defined as absence of defecation for more than 3 days after PICU admission1,6,16,19. Data analyzed included age, sex, weight, diagnosis and illness severity scores at admission: Pediatric Risk of Mortality III (PRISM III), Pediatric Index of Mortality 2 (PIM2), and Pediatric Logistic Organ Dysfunction (PELOD)23,24,25, length of PICU stay, and mortality. Data during the first 48 h after admission of midazolam, fentanyl, muscle relaxant, and inotropic agents (epinephrine or norepinephrine) administered, as well as the need for invasive or non-invasive mechanical ventilation and daily volume of EN were also analyzed. EN is started, increased or decreased and delivered according to a standard protocol followed by every physician. No medications to encourage bowel movements were administered in the first 48–72 h after admission.
Data analysis was performed using the SPSS 21.0 software package (IBM SPSS Statistics, Chicago). Continuous variables are expressed as mean ± standard deviation (SD) and categorical variables as percentages. Kolmogorov–Smirnov test was used to check normality. Comparisons of continuous and categorical variables were performed using the T or χ2 test (Fisher exact test when expected frequency was < 5) respectively. Univariate analysis was initially performed to identify factors associated with constipation. ROC curves were used to establish the best cutoff values for continuous variables. Results are expressed as odds ratio (OR) with 95% confidence intervals (95% CI). Multivariate analysis was then performed using a predictive logistic backward regression model that included those variables with statistical significance in the univariate analysis to identify independent factors. With these independent factors, a clinical score was developed: each OR value was divided by the lower OR obtained in the multivariate analysis and rounded to the nearest one decimal number. ROC curves were used to assure that this approach was correct and to establish the more sensitive and specificity cutoff values for the score. Statistical significance was taken as a p value of less than 0.05.
Ethics approval and consent to participate
Both studies were approved by the local Institutional Review Body of the Hospital General Universitario Gregorio Marañón. These studies were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from all subjects (their parents or legal guards) involved in the study.
Results
Score development
One hundred and forty-five patients (62.8% boys) with a mean age of 34.9 ± 7.3 months were studied. Surgical admissions accounted for 59.3% with 84 (97.6%) of surgical admissions from cardiac surgery. During the first 48 h after admission, 87 (60%) of patients were on MV and 100 (69%) had already started EN. Vasoconstrictors (epinephrine and/or norepinephrine) were required in 40 patients (27.6%) and 29 (20%) needed neuromuscular blockers. Midazolam and fentanyl were the most used sedatives; in 83 (57.2%) and 79 (54.5%) of patients respectively.
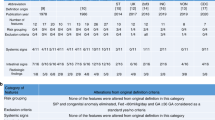
In the univariate analysis, factors more associated (OR > 3 and p < 0.06) with constipation were: weight > 7 kg, admission to PICU after surgery, risk of mortality according to PIM 2 > 4.5% at PICU admission, need of vasoconstrictors, doses of fentanyl ≥ 2 mcg/kg/h and initiation of EN more than 48 h after admission (Table 1). In the multivariate analysis, PIM 2 score was a dependent factor while the other five factors proved to be independently associated with constipation, and the score was elaborated with them (Table 1).
This score showed an area under the curve (AUC) of 0.878 with a 95% CI of 0.825–0.931 (p < 0.001) very close to the AUC of the complete multivariate analysis, 0.886 with a 95% CI of 0.835–0.938 (p < 0.001) (Fig. 1). Two cut-off values with good sensibility and specificity according to the ROC curve were identified to set low constipation risk (< 5.7 points) and high constipation risk (> 6.2 points) (Table 2).
Score validation
One hundred and twenty-three patients (56.1% boys) with a mean age of 37.5 ± 4.9 months were studied and followed up until the fourth day of PICU admission. Surgical admissions accounted for 43.9%. Median length of PICU stay was 12.6 ± 1.5 days and 8 patients (6.5%) died. During the first 48 h after admission, 58 (47.2%) of patients were on MV, 25 (20.3%) required vasoconstrictors and 91 (74%) had already started EN. Midazolam and fentanyl were also the most used sedatives in 34 (27.6%) and 37 (30.1%) of patients respectively and neuromuscular blockers were required in 16 patients (13%). Comparison between both populations is in Table 3.
Fifty-seven (46.3%) patients developed constipation during the first 4 days after PICU admission. According to the scale developed, two days after PICU admission, 37 patients would have been pointed as high constipation risk and these 37 patients finally developed constipation (Table 4).
Discussion
Constipation in is associated with important complications and high mortality rate in critically ill patients1,3,5,6,10,13,16,17,18,19,20,21. However, until now, very few pediatric studies about constipation in critically ill children have been published1,2,6. This is the first study that have developed a simply score to early diagnose this complication.
A very important barrier to performing epidemiology and treatment studies is the lack of universal diagnostic criteria for constipation1,2,7,16,18,26. International consensus about this item is focused in functional gastrointestinal disorders but there is no consensus about secondary constipation8,9,27. Moreover, constipation in critically ill patients has multiple origins, including clinical situations, drugs and environmental circumstances and is not limited to only one factor in each critical patient15,28.
Several constipation management protocols in critically ill adults have been proposed4,10,29,30 and even a risk assessment scale31 but no early diagnostic score has been developed.
Some studies in critically ill adult patients have shown the utility of protocols to identify and treat constipation early32,33,34 but there is nothing similar in the pediatric population. We have developed a simple score which can identify critically ill children with low and high risk of constipation development 48 h after PICU admission. This information could be used to start the treatment in high-risk patients early and to avoid delay in diagnosis and treatment.
Our score is based in five factors: weigh and vasoconstrictors are the most important. Older children are continent, so immobilization, a non comfortable environment and inappropriate bathrooms make it very difficult for them to maintain regular bowel movements during PICU admission1,14,35. However, this factor probably is not so important in severely ill patients with higher doses of sedatives.
The importance of vasoconstrictors could be more related to the hemodynamic and general situation (hypotension, gastrointestinal hypoperfusion and severity of illness) than to the direct effect of these drugs on the bowel motility1,10,11,13,21. Higher dosages of fentanyl are directly related to their peripheral action over mu opioid receptors, which decreases intestinal motility1,2,3,10,12. Surgery could influence constipation because of the effect of anesthetic drugs on the bowel motility. Finally late EN have been also identified as constipation risk factors in critically ill adults3,16. EN is one of the most important factors that induces bowel motility and prevents constipation.
ROC curves and AUC of multivariate analysis and score adjustment in our study were almost equal, so mathematical rounding did not change their predictive capability. The lower limit of our score showed a sensibility of 80% and it can identify non constipated patients with 79.4% reliability (negative predictive value), while the upper limit showed a specificity of 89.3% with a capacity to identify constipated patients of 85.2%.
Regarding the population collected for the scale validation, it was similar but not identical to the reference one. This new group of patients seemed to be slightly less severe since their PIM 2 scale score, length of PICU stay, need for MV, and therefore treatment with midazolam and fentanyl, continuous renal replacement therapy and extracorporeal membrane oxygenation was significantly lower than reference population values. However, the independent factors used to create the constipation risk scale were similar between both populations, especially those with more specific weight (weight and need for vasoconstrictors), except for the need of fentanyl. For this reason, we consider that the selected population was adequate for the internal validation of the constipation risk scale.
The fact that the percentage of constipation is practically identical between both populations, although they are different in some risk factors such as opiates, clinical severity, PICU stay or MV, supports the hypothesis that constipation in the critical child, is an entity with a multifactorial cause in which various factors act synergistically15,16,19,36,37,38,39.
However, our population may not be representative of children admitted to other PICUs, since a high percentage of patients with heart disease and postsurgical patients enter our population. For this reason, studies are necessary to confirm the utility of this scale in other PICUs.
The developed scale has shown, on a different population, an excellent ability to identify patients at high risk of constipation 48 h after PICU admission. This scale is simple, easy and quick to apply. With this information, the initiation of early treatment in these high-risk patients could be considered, trying to reduce complications due to delayed diagnosis and treatment. Two studies in critical adults have raised this possibility. Guardiola et al. showed how early treatment on the second day of ICU admission in mechanically ventilated patients was better than conventional treatment administered after diagnosing constipation32. Masri et al. also reached a similar conclusion but with a treatment just upon ICU admission33.
In contrast, the moderate sensitivity (64.9%) presented by our scale, means that a few patients who will eventually develop constipation, are not identified 48 h after admission. Regarding the patients who will not develop constipation, the score has a high specificity and negative predictive value also. Therefore, in low-risk patients (< 5.7 points), no intervention is necessary, but a follow up is necessary, since up to a quarter of them may be constipated at the end.
Considering that, at present, there is no other method to make an early diagnosis of constipation in critically ill children, we consider this scale is useful to identify patients with high risk of constipation. Moreover, the use of this scale can increase awareness and active surveillance of this problem by improving clinical practice and can serve as a basis for comparing risk groups and assessing the effect of various treatments that could be applied early.
Several limitations in this study should be considered. First, this is a single-centre study in a mixed PICU with a relatively low number of patients. Second, the development of the constipation risk scale, is based on pre-existing data used for another study, although the objective of both studies was similar. However, the fact that the population used for its validation was collected prospectively, this limitation can be solved. And finally, the fact that in our unit we use midazolam and fentanyl as the first line of treatment and during the first 5 days of PICU admission, means that we have developed this score according to these drugs without taking into account other sedoanalgesics or the opioid/morphine equivalent, which may limit its application in other units.
Conclusions
This is the first tool to improve constipation diagnosis in critically ill children. Our score is easy to use and can identify high risk of constipation development in our critically ill children. Internal validation has been performed but external validation should be carried out to assure its utility through further future multicenter studies. This score also opens a new line of investigation related to prophylactic treatments for constipation in critically ill children.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AUC:
-
Area under the curve
- EN:
-
Enteral nutrition
- ICU:
-
Intensive care unit
- MV:
-
Mechanical ventilation
- OR:
-
Odds ratio
- PELOD:
-
Pediatric logistic organ dysfunction
- PICU:
-
Pediatric intensive care unit
- PIM 2:
-
Pediatric index of mortality
- PRISM III:
-
Pediatric risk of mortality III
- SD:
-
Standard deviation
- 95% CI:
-
95% confidence interval
References
López, J. et al. Constipation in the critically ill child: Frequency and related factors. J Pediatr. 167, 857–861 (2015).
Smalley, N. & Vangaveti, V. Assessing the bowel function of critically ill children: A pilot study. Crit Care Resusc. 16, 202–205 (2014).
Fukuda, S. et al. Risk factors for late defecation and its association with the outcomes of critically ill patients: a retrospective observational study. J Intensive Care. 4, 33 (2016).
McPeake, J., Gilmour, H. & MacIntosh, G. The implementation of a bowel management protocol in an adult intensive care unit. Nurs Crit Care. 16, 235–242 (2011).
Ali, H. et al. Effect of constipation on outcomes in mechanically ventilated patients. Proc. (Bayl. Univ. Med. Cent.) 35, 284–290 (2022).
López, J., Solana, M. J. & López-Herce, J. Narrative review of constipation in the critically ill child. Pediatr. Med. 4, 14 (2021).
Khilnani, P., Rawal, N. & Singha, C. Gastrointestinal issues in critically Ill children. Indian J. Crit. Care Med. 24(Suppl 4), 201–204 (2020).
Benninga, M. A. et al. Childhood functional gastrointestinal disorders: Neonate/toddler. Gastroenterology 150, 1443–55 (2016).
Hyams, J. S. et al. Functional disorders: Children and adolescents. Gastroenterology 150, 1456–1468 (2016).
van der Spoel, J. I., Schultz, M. J., van der Voort, P. H. & de Jonge, E. Influence of severity of illness, medication and selective decontamination on defecation. Intensive Care Med. 32, 875–880 (2006).
Dive, A., Foret, F., Jamart, J., Bulpa, P. & Installé, E. Effect of dopamine on gastrointestinal motility during critical illness. Intensive Care Med. 26, 901–907 (2000).
Frantzides, C. T., Cowles, V., Salaymeh, B., Tekin, E. & Condon, R. E. Morphine effects on human colonic myoelectric activity in the postoperative period. Am. J. Surg. 163, 144–148 (1992).
Gacouin, A. et al. Constipation in long-term ventilated patients: Associated factors and impact on intensive care unit outcomes. Crit. Care Med. 38, 1933–1938 (2010).
Morad, M., Nelson, N. P., Merrick, J., Davidson, P. W. & Carmeli, E. Prevalence and risk factors of constipation in adults with intellectual disability in residential care centers in Israel. Res. Dev. Disabil. 28, 580–586 (2007).
Pérez-Sánchez, J. et al. Evaluation and handling of constipation in critical patients. Enferm Intensiva. 28, 160–168 (2017).
Nassar, A. P., da Silva, F. M. & de Cleva, R. Constipation in intensive care unit: Incidence and risk factors. J. Crit. Care. 24(630), e9-12 (2009).
Smonig, R. et al. Constipation is independently associated with delirium in critically ill ventilated patients. Intensive Care Med. 42, 126–127 (2016).
de Lopes, S. T., Sotero, S. & Guimarães, N. Incidence of constipation in an intensive care unit. Rev. Bras. Ter. Intensiva. 25, 87–92 (2013).
Mostafa, S. M., Bhandari, S., Ritchie, G., Gratton, N. & Wenstone, R. Constipation and its implication in the critically ill patient. Br. J. Anaesth. 91, 815–819 (2003).
Launey, Y. et al. Factors associated with time to defecate and outcomes in critically ill patients: A prospective multicentre, observational study. Anaesthesia 76, 218–224 (2021).
van der Spoel, J. I. et al. Laxation of critically ill patients with lactulose or polyethylene glycol: A two-center randomized, double-blind, placebo-controlled trial. Crit. Care Med. 35, 2726–2731 (2007).
Xing, J. H. & Soffer, E. E. Adverse effects of laxatives. Dis. Colon Rectum. 44, 1201–1209 (2001).
Pollack, M. M., Patel, K. M. & Ruttimann, U. E. PRIMSIII: An updated pediatric risk of mortality score. Crit. Care Med. 24, 743–752 (1996).
Slater, A., Shann, F. & Pearson, G. PIM2: A revised version of the Paediatric Index of Mortality. Intensive Care Med. 29(2), 278–285. https://doi.org/10.1007/s00134-002-1601-2 (2003).
Leteurtre, S. et al. Validation of the paediatric logistic organ dysfunction (PELOD) score: Prospective, observational, multicentre study. Lancet 362, 192–197 (2003).
Yoshida, T., Uchino, S. & Sasabuchi, Y. Epidemiology of constipation in critically ill patients and its impact on in-hospital mortality: A retrospective observational study. J Anesth. 36, 349–358 (2022).
Tabbers, M. M. et al. Evaluation and treatment of functional constipation in infants and children: Evidence-based recommendations from ESPGHAN and NASPGHAN. J. Pediatr. Gastroenterol. Nutr. 58, 258–274 (2014).
McClave, S. A. Nutrition, defecation, and the lower gastrointestinal tract during critical illness. Curr. Opin. Clin. Nutr. Metab. Care. 25, 110–115 (2022).
Knowles, S., McInnes, E., Elliott, D., Hardy, J. & Middleton, S. Evaluation of the implementation of a bowel management protocol in intensive care: Effect on clinician practices and patient outcomes. J. Clin. Nurs. 23, 716–730 (2014).
Oczkowski, S. J. W., Duan, E. H., Groen, A., Warren, D. & Cook, D. J. The use of bowel protocols in critically ill adult patients: A systematic review and meta-analysis. Crit. Care Med. 45, e718–e726 (2017).
Richmond, J. P. & Wright, M. E. Review of the literature on constipation to enable development of a constipation risk assessment scale. Clin. Effect Nurs. 8, 11–25 (2004).
Guardiola, B., Llompart-Pou, J. A., Ibáñez, J. & Raurich, J. M. Prophylaxis versus treatment use of laxative for paralysis of lower gastrointestinal tract in critically ill patients. J. Clin. Gastroenterol. 50, e13–e18 (2016).
Masri, Y., Abubaker, J. & Ahmed, R. Prophylactic use of laxative for constipation in critically ill patients. Ann. Thorac. Med. 5, 228–231 (2010).
Duprey, M. S. et al. Naloxegol to prevent constipation in ICU adults receiving opioids: A randomized double-bling placebo-controlled pilot trial. Crit. Care Resp. Pract. https://doi.org/10.1155/2022/7541378 (2022).
Hall, G. R., Karstens, M., Rakel, B., Swanson, E. & Davidson, A. Managing constipation using a research-based protocol. Medsurg Nurs. 4, 11–20 (1995).
Guerra, T. L., Mendonça, S. S. & Marshall, N. G. Incidence of constipation in an intensive care unit. Rev. Bras. Ter. Intensiva. 25, 87–92 (2013).
Nguyen, T. et al. Impaired gastrointestinal transit and its associated morbidity in the intensive care unit. J. Crit. Care. https://doi.org/10.1016/j.jcrc.2012.12.003 (2013).
de Azevedo, R. P. & Machado, F. R. Constipation in critically ill patients: Much more than we imagine. Rev. Bras. Ter. Intensiva. 25, 73–74 (2013).
Bishop, S. et al. Bowel motions in critically ill patients: A pilot observational study. Crit. Care Resusc. 12, 182–185 (2010).
Acknowledgements
To José María Bellón for his invaluable help with statistics. To Rocío García, Andreina Ferreira and Tatiana Vilchez and their colleagues in the UK for their English language medical editing assistance.
Funding
This study was performed with a grant support from Instituto de Salud Carlos III (PI10/1933) and Promotion and the European Regional Development Fund (ERDF), ref. RD12/0026. Primary Care Interventions to Prevent Maternal and Child Chronic Diseases of Perinatal and Development Origin Network (RICORS) RD21/0012/0011 of Instituto de Salud Carlos III.
Author information
Authors and Affiliations
Contributions
Conception: JL, CS and JL-H; Design: JL, CS and JU; Acquisition/Analysis: RG, SNF, MJS and JU; Data interpretation: JL, CS, RG and SNF; Draft preparation: JL, MJS and SNF; Review and editing: CS, JU and JL-H. All authors read and approved the submission of this version of the manuscript and all of them have agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
López, J., Sánchez, C., Fernández, S.N. et al. Development and validation of a clinical score for early diagnosis of constipation in critically ill children. Sci Rep 13, 14822 (2023). https://doi.org/10.1038/s41598-023-41674-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-41674-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.