Abstract
Vaccines play a crucial role in preventing infections in patients with multiple sclerosis (MS), although concerns have been raised about potential worsening of the underlying disease. To investigate this, we conducted a prospective, multicentre, non-randomized observational study assessing changes in disease activity, safety, and clinical tolerability of vaccination in 222 MS patients on disease-modifying drugs. The majority of patients were female (76.6%) and 89.6% had relapsing–remitting MS. The vaccines administered were primarily seasonal influenza (56.3%) or tetanus-based vaccines (33.8%). Disease activity, as measured by annualized relapse rate, decreased significantly from 0.64 the year prior to vaccination to 0.38 in the following year. Moreover, the extended disability status scale remained stable within six months after vaccination in comparison to pre-vaccination values. Side effects were reported in 19.2% of vaccinated subjects, most commonly local side effects (65.2%) or flu-like symptoms (34.8%). Our findings suggest that standard non-live vaccines are safe and well-tolerated in MS patients and do not negatively impact disease activity.
Similar content being viewed by others
Introduction
Preventive vaccination plays an important role in the management of health issues, especially when caring for people with multiple sclerosis (MS)1,2. Infectious episodes and fever may lead to the deterioration of MS disease contributing to increased mortality rates compared to the normal population3. Prevention of infections is an important measure of medical care for patients with MS4,5. Patients and treating physicians have previously been concerned about reports of possible detrimental effects of vaccinations on the course of MS6,7. This may still lead to vaccine hesitancy in MS patients despite studies revealing that non-live vaccines are safe and treatment guidelines recommend consequent vaccination in these patients8,9.
The aim of this study was to evaluate the safety, tolerability, and MS disease activity following generally recommended vaccines in MS in a real-world situation.
Patients, material and methods
This prospective, multicentre, non-randomized observational study at specialized outpatient MS care centres included MS patients aged 18 to 70 years who had been on disease-modifying treatment (DMT) for at least six months and who had an indication for recommended preventive vaccination10. We excluded all patients with MS relapse or other disease activity during the previous six months before vaccination. Routine MRI evaluation was not planned in this study protocol.
Participation in this study was offered to all patients who received licensed vaccinations on a routine basis. Details of MS disease, medical history, baseline characteristics and clinical examination were collected. Subjects received the respective vaccination in the deltoid muscle in an open-label manner. Subjects had follow-up visits after 1, 3, 6 and 12 months between 2010 and 2013. Local and systemic adverse events were registered at the first follow-up visit 4 weeks after vaccination. Data of pre-vaccination disease activity was collected from clinical records in a retrospective manner. MS relapse activity as well as expanded disability status scale (EDSS) after vaccination were monitored throughout follow-up visits prospectively. Relapses were confirmed by the treating neurologists and medical evaluation according to national guidelines following routine patient management and medical practice.
The evaluation of the immune response to influenza and tick-born encephalitis (TBE) vaccines of patients presented in this study have previously been published11,12.
All statistical analyses were performed using Prism 9 (9.1.2, GraphPad Software). Values were expressed as mean ± standard deviation. Mann–Whitney U-test was used to compare annualized relapse rates. All reported p-values are two-sided; values of 0.05 or less were considered to indicate statistical significance.
The study was approved by the local ethics committee (Rostock HV 2010-0002) and registered at ClinicalTrials.gov (NCT02275741). The study was conducted in accordance with the International Conference on Harmonization Guidelines for Good Clinical Practice, the Declaration of Helsinki and all applicable national laws. Informed written consent was obtained from all participants before entry into the study.
Results
In total 222 patients with MS were included in this analysis. The baseline characteristics of this cohort are summarized in Table 1. The majority of included subjects were female (76.6%), and most of the patients were affected by RR-MS (89.6%) and had a mean duration of disease of 8.5 ± 6.9 years. The mean EDSS score at vaccination was 2.3 ± 1.9.
The majority of subjects received interferon-beta therapy (47.8%) at vaccination; other applied DMTs were glatiramer acetate (23.4%), natalizumab (11.7%), fingolimod (5.9%). Of the subjects 56.3% received seasonal influenza vaccination, 33,8% received tetanus-based vaccination, 9.0% had a TBE vaccination. The other subjects were vaccinated against various other transmittable diseases, among them hepatitis A or B and typhoid fever.
After vaccination 6 subjects had a relapse in the first month (3.3%), among those, 3 (1.6%) subjects within the first week, 1 (0.5%) during the third week and 2 (1.1%) during the fourth week. Within the second and third month after vaccination 6 (3.3%) and 5 (2.7%), respectively had relapses (Fig. 1).
Over all, 14 relapses during day 7 and 90 following vaccination (7.6%) were reported. Between day 7 and 90 after vaccination relapses occurred in 9/125 (7.2%) patients after influenza, 4/75 (5.3%) after tetanus-based, and 1/20 (5.0%) after tic borne encephalitis vaccination, resulting in annualized relapse rates of 0.29, 0.21, and 0.2 respectively.
In 8/106 (7.6%) patients treated with interferon-beta and in 3/52 (5.8%) patients treated with glatiramer acetate relapses occurred between day 7 and 90 after vaccination, resulting in annualized relapse rates of 0.30 and 0.23, respectively.
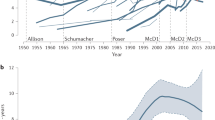
The annualized relapse rate decreased from 0.69 to 0.45 during the 2 years before vaccination (p < 0.05). In the year following vaccination the annualized relapse rate (0.4) was not significantly changed (p > 0.05) compared to the preceding year (Fig. 2).
Annualised relapse rate. Mean annualised relapse rates in the study population during 2 years before vaccination and 1 year after vaccination, error bars show standard error of means. Means between year −1 and year +1 are not significantly different, p (year −1 vs. year +1) is > 0.05 (Mann–Whitney U test).
EDSS score was not significantly different during 24 months before vaccination and within 6 months after vaccination (Fig. 3). Over all the EDSS was higher, though not significantly changed, 12 months after vaccination (2.4) compared to the EDSS at vaccination (2.3, p = 0.35).
Adverse events following vaccination were documented in 40 patients (20.2%), among them 24 reported local and 21 reported systemic adverse events (Table 1). Most of the reported adverse effects were mild and subsided within the first week. Except for local pain at the injection site that was rated as severe in one subject, all other local side effects were mild. Flu-like symptoms were the most commonly reported systemic side effects, of these 2 (13.3%) were severe, 7 (46.7%) were moderate and 6 (40.0%) mild (Table 2).
Following influenza vaccination 12/125 (9.6%) had local and 13/125 (10.4%) had systemic adverse events, among them three patients had both, local and systemic side effects. In tetanus-based vaccine recipients 11/75 (14.7%) had local and 6/75 (8.0%) had systemic adverse events, among those, one patient had both, local and systemic adverse events. Following tick-borne vaccination 3/20 (15.0%) had local side effects, 2/20 (10.0%) had systemic reactions and one had both, local and systemic reactions.
In patients treated with interferon-beta 14/106 (13.2%) had local and 12/106 (11.3%) had systemic adverse events, among them two patients had both, local and systemic side effects.
In patients treated with glatiramer acetate 9/52 (17.3%) had local and 5/52 (9.6%) had systemic adverse events, among them three patients had both, local and systemic side effects.
Discussion
The fear of possible adverse effects of vaccination in general and specific to people with MS, like increased relapse activity and progression (EDSS), might occasionally lead to vaccine hesitancy in MS patients and their physicians7,13,14,15,16.
The focus of this study was to analyse possible MS specific effects and other adverse events following vaccination. Since MS develops changes in long term, we have evaluated subjects with MS during one year before and after vaccination. This enables to determine changes in relapse-rate and EDSS and may provide a better insight into relapse timing and possible association to vaccination in a real-world situation.
The analyzed real-world study population represents a cohort of out-patients with MS suitable for vaccination in a typical gender and age distribution17,18,19. The studied population had stable disease with annualised relapse rates of 0.69 and 0.45 during the 2 years before vaccination. Notably, the annualised relapse-rates were high in this study population before vaccination. This might reflect a selection bias towards people with MS and higher disease activity treated at the involved specialised MS clinics19,20,21. The reduction of the relapse reflects the effects of the established and ongoing DMT22,23,24. In the year following vaccination the annualized relapse rate (0.4) was not significantly changed compared to the time before vaccination. This implies, that routine vaccination does not negatively impact the annualized relapse rates in MS patients which has been shown in in previous studies as well25,26. One has to keep in mind that only inactivated, non-live vaccines have been used in our study. Other studies have hinted a possible increase in relapse rates after live vaccines, such as yellow fever13, though this was not confirmed in a recent study27.
The EDSS, a marker of disease progression in MS that is rarely reported in the context of vaccination, showed a mild over-all increase during the study period of 3 years, corresponding to a MS cohort with mean disease duration of 8.5 years28,29. During 12 months after vaccination the EDSS did not significantly change in comparison to the EDSS at vaccination.
Local and systemic adverse events of vaccination in the general population are extensively studied before licensing of vaccines and are generally assessed using subject diaries and short term follow-up visits in vaccination studies. This study did not focus on short-lived expected adverse events and thus did not use diaries, but relied on reporting of adverse events at close and structured follow-up visits. Therefore one may expect a reporting bias, since minor side effects may be underreported at retrospective documentation30,31. Nevertheless, the reported adverse events were rare and generally mild. Should severe cases of adverse events have occurred one may expect, that these events would have been reported despite a possible recall bias.
On the one hand this prospective multicentre study shows that vaccine side effects in patients with MS do not present any particular quantitative or qualitative safety signals compared with the general population. On the other hand, the disease activity of MS is not negatively affected by non-live vaccines. This also seems true for novel mRNA-based SARS-CoV2 vaccines in patients with MS32,33,34,35,36, though long-term evaluations are pending14.
We feel this study may contribute to overcome possible vaccine hesitancy in MS patients and their treating physicians37,38 by documenting low rates of adverse events following-routine vaccinations comparable to the expected spectrum of side effects in the general population.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Farez, M. F. et al. Practice guideline update summary: Vaccine-preventable infections and immunization in multiple sclerosis: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 93(13), 584–594. https://doi.org/10.1212/wnl.0000000000008157 (2019).
Loebermann, M. et al. Vaccination against infection in patients with multiple sclerosis. Nat. Rev. Neurol. 8(3), 143–151. https://doi.org/10.1038/nrneurol.2012.8 (2012).
Manouchehrinia, A., Tanasescu, R., Tench, C. R. & Constantinescu, C. S. Mortality in multiple sclerosis: Meta-analysis of standardised mortality ratios. J. Neurol. Neurosurg. Psychiatry 87(3), 324–331. https://doi.org/10.1136/jnnp-2015-310361 (2016).
D’Hooghe, M. B., Nagels, G., Bissay, V. & De Keyser, J. Modifiable factors influencing relapses and disability in multiple sclerosis. Multiple Scler. (Houndmills, Basingstoke, England) 16(7), 773–785. https://doi.org/10.1177/1352458510367721 (2010).
Winkelmann, A., Loebermann, M., Reisinger, E. C., Hartung, H. P. & Zettl, U. K. Disease-modifying therapies and infectious risks in multiple sclerosis. Nat. Rev. Neurol. 12(4), 217–233. https://doi.org/10.1038/nrneurol.2016.21 (2016).
Witman Tsur, S., Adrian Zaher, E., Tsur, M., Kania, K. & Kalinowska-Łyszczarz, A. Current immunological and clinical perspective on vaccinations in multiple sclerosis patients: are they safe after all? Int. J. Mol. Sci. 22(8). https://doi.org/10.3390/ijms22083859 (2021).
Zrzavy, T. et al. Vaccination in multiple sclerosis: Friend or foe?. Front. Immunol. 10, 1883. https://doi.org/10.3389/fimmu.2019.01883 (2019).
Geoghegan, S., O’Callaghan, K. P. & Offit, P. A. Vaccine safety: Myths and misinformation. Front. Microbiol. 11, 372. https://doi.org/10.3389/fmicb.2020.00372 (2020).
Hapfelmeier, A., Gasperi, C., Donnachie, E. & Hemmer, B. A large case–control study on vaccination as risk factor for multiple sclerosis. Neurology 93(9), e908–e916. https://doi.org/10.1212/wnl.0000000000008012 (2019).
STIKO. Empfehlungen der Ständigen Impfkommission beim Robert Koch-Institut 2023. Epidemiol. Bull. 4, 1–67 (2023).
Winkelmann, A., Metze, C., Frimmel, S., Reisinger, E.C., Zettl, U.K.& Loebermann, M. Tick-borne encephalitis vaccination in multiple sclerosis: A prospective, multicenter study. Neurol. Neuroimmunol. Neuroinflamm. 7(2). https://doi.org/10.1212/nxi.0000000000000664 (2020).
Metze, C. et al. Immunogenicity and predictors of response to a single dose trivalent seasonal influenza vaccine in multiple sclerosis patients receiving disease-modifying therapies. CNS Neurosci. Ther. 25(2), 245–254. https://doi.org/10.1111/cns.13034 (2019).
Farez, M. F. & Correale, J. Yellow fever vaccination and increased relapse rate in travelers with multiple sclerosis. Arch. Neurol. 68(10), 1267–1271. https://doi.org/10.1001/archneurol.2011.131 (2011).
Frahm, N. et al. SARS-CoV-2 vaccination in patients with multiple sclerosis in Germany and the United Kingdom: Gender-specific results from a longitudinal observational study. Lancet Region. Health Eur. 22, 100502. https://doi.org/10.1016/j.lanepe.2022.100502 (2022).
Heidler, F. et al. Vaccination willingness in association with personality traits in patients with multiple sclerosis in the course of SARS-CoV-2 pandemic. Sci. Rep. 12(1), 15147. https://doi.org/10.1038/s41598-022-18912-3 (2022).
Heidler, F. et al. Vaccination setting of patients with autoimmune diseases in times of severe acute respiratory syndrome coronavirus type 2 pandemic using the example of multiple sclerosis patients: A longitudinal multicenter study. Eur. Neurol. 85(2), 104–111. https://doi.org/10.1159/000519582 (2022).
Leray, E., Moreau, T., Fromont, A. & Edan, G. Epidemiology of multiple sclerosis. Rev. Neurol. 172(1), 3–13. https://doi.org/10.1016/j.neurol.2015.10.006 (2016).
Flachenecker, P. et al. Multiple sclerosis registry in Germany: Results of the extension phase 2005/2006. Deutsches Arzteblatt Int. 105(7), 113–119. https://doi.org/10.3238/arztebl.2008.0113 (2008).
Ohle, L. M. et al. Chances and challenges of a long-term data repository in multiple sclerosis: 20th birthday of the German MS registry. Sci. Rep. 11(1), 13340. https://doi.org/10.1038/s41598-021-92722-x (2021).
Flachenecker, P. et al. Multiple sclerosis in Germany: Updated analysis of the German MS Registry 2014–2018. Fortsch. Neurol.-Psychiatr. 88(7), e1. https://doi.org/10.1055/a-1248-5258 (2020).
Stuke, K. et al. Symptomatology of MS: Results from the German MS Registry. J. Neurol. 256(11), 1932–1935. https://doi.org/10.1007/s00415-009-5257-5 (2009).
Rommer, P. & Zettl, U. K. Treatment options in multiple sclerosis and neuromyelitis optica spectrum disorders. Curr. Pharm. Des. 28(6), 428–436. https://doi.org/10.2174/1381612827666210920151231 (2022).
Wiendl, H. et al. Multiple Sclerosis Therapy Consensus Group (MSTCG): Position statement on disease-modifying therapies for multiple sclerosis (white paper). Ther. Adv. Neurol. Disord. 14, 17562864211039648. https://doi.org/10.1177/17562864211039648 (2021).
Wiendl, H., Gold, R. & Zipp, F. Multiple sclerosis therapy consensus group (MSTCG): Answers to the discussion questions. Neurol. Res. Pract. 3(1), 44. https://doi.org/10.1186/s42466-021-00140-1 (2021).
Confavreux, C., Suissa, S., Saddier, P., Bourdès, V. & Vukusic, S. Vaccinations and the risk of relapse in multiple sclerosis. Vaccines in Multiple Sclerosis Study Group. N. Engl. J. Med. 344(5), 319–326. https://doi.org/10.1056/nejm200102013440501 (2001).
Otero-Romero, S., Ascherio, A. & Lebrun-Frénay, C. Vaccinations in multiple sclerosis patients receiving disease-modifying drugs. Curr. Opin. Neurol. 34(3), 322–328. https://doi.org/10.1097/wco.0000000000000929 (2021).
Huttner, A., Eperon, G., Lascano, A.M., Roth, S., Schwob, J.M., Siegrist, C.A. et al. Risk of MS relapse after yellow fever vaccination: A self-controlled case series. Neurol. (R) Neuroimmunol. Neuroinflamm. 7(4). https://doi.org/10.1212/nxi.0000000000000726 (2020).
Rommer, P. S. et al. Symptomatology and symptomatic treatment in multiple sclerosis: Results from a nationwide MS registry. Multiple Scler. (Houndmills, Basingstoke, England). 25(12), 1641–1652. https://doi.org/10.1177/1352458518799580 (2019).
Ellenberger, D. et al. Is benign MS really benign? What a meaningful classification beyond the EDSS must take into consideration. Multiple Scler. Relat. Disord. 46, 102485. https://doi.org/10.1016/j.msard.2020.102485 (2020).
Lopez-Gonzalez, E., Herdeiro, M. T. & Figueiras, A. Determinants of under-reporting of adverse drug reactions: A systematic review. Drug Saf. 32(1), 19–31. https://doi.org/10.2165/00002018-200932010-00002 (2009).
Rosenthal, S. & Chen, R. The reporting sensitivities of two passive surveillance systems for vaccine adverse events. Am. J. Public Health 85(12), 1706–1709. https://doi.org/10.2105/ajph.85.12.1706 (1995).
Achiron, A. et al. Humoral immune response to COVID-19 mRNA vaccine in patients with multiple sclerosis treated with high-efficacy disease-modifying therapies. Ther. Adv. Neurol. Disord. 14, 17562864211012836. https://doi.org/10.1177/17562864211012835 (2021).
Di Filippo, M., Cordioli, C., Malucchi, S., Annovazzi, P., Cavalla, P., TorriClerici, V. et al. mRNA COVID-19 vaccines do not increase the short-term risk of clinical relapses in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry. https://doi.org/10.1136/jnnp-2021-327200 (2021).
Achiron, A., Dolev, M., Menascu, S., Zohar, D.N., Dreyer-Alster, S., Miron, S. et al. COVID-19 vaccination in patients with multiple sclerosis: What we have learnt by February 2021. Multiple Scler. (Houndmills, Basingstoke, England) 2021, 13524585211003476. https://doi.org/10.1177/13524585211003476 (2021).
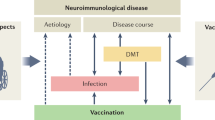
Winkelmann, A., Loebermann, M., Barnett, M., Hartung, H. P. & Zettl, U. K. Vaccination and immunotherapies in neuroimmunological diseases. Nat. Rev. Neurol. 18(5), 289–306. https://doi.org/10.1038/s41582-022-00646-5 (2022).
Monschein, T. et al. Vaccination and multiple sclerosis in the era of the COVID-19 pandemic. J. Neurol. Neurosurg. Psychiatry 92(10), 1033–1043. https://doi.org/10.1136/jnnp-2021-326839 (2021).
Langhorst, S.E., Frahm, N., Hecker, M., Mashhadiakbar, P., Streckenbach, B., Baldt, J. et al. Vaccination coverage against tetanus, diphtheria, pertussis and poliomyelitis and validity of self-reported vaccination status in patients with multiple sclerosis. J. Pers. Med. 12(5). https://doi.org/10.3390/jpm12050677 (2022).
Streckenbach, B. et al. General vaccination willingness and current vaccination status in relation to clinical and psychological variables in patients with multiple sclerosis. Vaccine. 40(23), 3236–3243. https://doi.org/10.1016/j.vaccine.2022.04.012 (2022).
Acknowledgements
The authors would like to thank Ina Schröder for her continuous help with all aspects of this study and her expertise in patient care. We thank our colleagues from NeuroTransData (NTD) for contributing patients.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the conception of the work and have approved the submitted version; A.W. and C.M. performed the data acquisition; A.W., U.K.Z. and M.L. analysed and interpreted the data; A.W. and M.L. have drafted the work. All authors have agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Competing interests
A. Winkelmann reports personal compensation from Bayer Healthcare, Celgene, Merck, Novartis, Sanofi Genzyme, and Teva. C. Metze reports no disclosures. U. K. Zettl received speaking fees, travel support and financial support for research activities from Alexion, Almirall, Bayer, Biogen, Merck Serono, Novartis, Octapharm, Roche, Sanofi Genzyme, Teva and as well as EU, BMBF, BMWi, and DFG. None resulted in a conflict of interest. M. Loebermann reports personal compensation from Gilead, Janssen, Pfizer and Sanofi and research support from Cempra, Correvio, Pfizer, Sanofi, Schering, Seqirus, Themis Bioscience, Valneva and Vectura.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Winkelmann, A., Metze, C., Zettl, U.K. et al. Side effects following vaccination in multiple sclerosis: a prospective, multi-centre cohort study. Sci Rep 13, 14480 (2023). https://doi.org/10.1038/s41598-023-41271-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-41271-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.