Abstract
Tobacco smoking is carcinogenic to humans. Besides cigarettes, the most common form of tobacco smoking, there was sparse evidence of waterpipe’s carcinogenicity-induced nasopharyngeal cancer (NPC). This study investigated the association between waterpipe smoking and NPC mortality. Our study followed up with 20,144 eligible man participants from nine northern Vietnam communes between 2007 and 2019. Face-to-face interviews were conducted to gather data on exclusive waterpipe and cigarette smoking and dietary intake using structured semi-quantitative food frequency and lifestyle questionnaires. Nasopharyngeal cancer was determined by accessing the medical records at the state health facilities. We estimated the Cox proportional hazard ratio and 95% confidence intervals, HR (95% CI). The proportion of never smokers, exclusive waterpipe, exclusive cigarette, and dual waterpipe and cigarette smokers was 55.8%, 14.5%, 16.6%, and 13.1%, respectively. Exclusively waterpipe smokers increased the risk of NPC death compared to exclusively cigarette smokers, HR (95% CI): 4.51 (1.25, 16.31), p = 0.022. A dose-dependent positive relationship between NPC and exclusive waterpipe smoking was significantly seen for higher intensity HR (95% CI): 1.35 (1.07, 1.71), earlier age of smoking initiation HR (95% CI): 1.26 (1.06, 1.50), longer duration HR (95% CI): 1.31 (1.04, 1.66), and the cumulative number of a smoke lifetime HR (95% CI): 1.37 (1.08, 1.74). We observed a significant positive association between exclusive waterpipe smoking and NPC in men. The findings suggested that waterpipe smoking is likely more harmful than cigarettes in developing this cancer. A firm tobacco control against waterpipe smoking is highly recommended.
Similar content being viewed by others
Introduction
Nasopharyngeal cancer (NPC) is rare worldwide, with an incident rate of under 1 per 100,000 population per year1. The incidence rate in men is double or triple that in women1. However, in the Cantonese population of southern China, substantially higher rates are reported1. Intermediate rates are found in indigenous people in Southeast Asia, the Arctic region, North Africa, and the Middle East1. In 2018, 85% of an estimated 129,079 incident cases of NPC were diagnosed in Asia1. In Southeast Asia, NPC ranked 9th among incident cancers and 8th among cancer deaths1. In China, the highest-risk population belongs to the southeastern Chinese province of Guangdong, the Cantonese-speaking population2. In Southeast Asia, NPC risk appears higher in the Chinese3. In the United States and Singapore, rates are highest among the Chinese1. NPC ranked 9th most common cancer in Vietnam, with 6040 new cases in 20204. There is an unclear association between race and ethnicity and NPC incidence.
NPC is classified histologically as keratinizing squamous cell carcinoma (type I); differentiated nonkeratinizing carcinoma (type II); undifferentiated nonkeratinizing carcinoma (type III); or basaloid squamous cell carcinoma, a rare subtype5. Undifferentiated carcinoma (type III) comprises over 95% of the NPC cases in high-incidence regions, while differentiated carcinoma (type I) is predominant in low-incidence areas6.
Risk factors of NPC updated in recent studies include Cantonese ethnicity, man sex, Epstein–Barr virus (EBV) infection, a family history of NPC, high consumption of salt-preserved fish, low intake of fresh vegetables and fruits intake, smoking, and some human leukocyte antigen (HLA) class I alleles7.
IARC Working Groups reported sufficient evidence in humans for the carcinogenicity of tobacco smoking8. Tobacco smoking is classified into group 1 carcinogens to humans. Substantial evidence showed a causal relationship between tobacco smoking and cancers of the lung9 and oral cavity10. Cohort studies reported a positive association between cigarette smoking and NPC in the U.S., Taiwan, and Singapore but inconclusion in the U.K. populations11,12,13,14,15. However, waterpipe tobacco smoking was not examined in these studies.
Besides cigarette smoking, waterpipe is an older form of tobacco smoking. Among men, Vietnam has the highest rate of waterpipe tobacco smoking, followed by China and Malaysia16. Vietnamese waterpipe is made of bamboo, metal, or porcelain with structures and directions similar to the ones used in China16. Waterpipe smoking in Vietnam is more prevalent in the older, rural, less educated man population16. According to the National Health Survey in Vietnam, the prevalence of man smokers was 51.2%. Among man smokers, most of them smoked cigarettes only (69.1%), followed by Vietnamese WPT only (23.2%) and both products (7.7%) in 2001–200217.
Evidence of the relationship between cigarette and waterpipe smoking and NPC is generally limited. Thus, our study aimed to investigate the relationship between cigarette and waterpipe smoking and NPC mortality after adjusting for confounding factors.
Methods
Study design and population
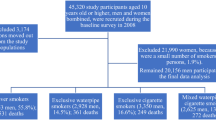
In 2007, 52,325 individuals from 12,746 households were recruited into our prospective cohort study. They belonged to nine communes in Hung Yen, Phu Pho, and Hanoi in Northern Vietnam. A questionnaire on exclusive waterpipe and cigarette smoking, demographic characteristics, dietary intake, fridge availability, cooking methods, and alcohol consumption was used to ask the participants. Then, we followed up on all the causes of death using medical records collected at the state health facilities. Deaths caused by cancer were coded based on ICD-10. Participants with (1) no history of cancer and (2) presence at the research location through the investigation period were included in our prospective cohort study. After over 12 years of follow-up, 7182 participants aged under 10-year-old and loosed follow-up 2997 persons due to migration were excluded. We excluded 21,990 women because there were two small numbers of smokers (418 persons, 1.9%), Fig. 1. Finally, the data of 20,144-man participants with 39 NPC mortality cases were examined in the present study.
Exposure assessment
Trained students of Hanoi Medical University conducted face-to-face interviews with participants. We used a structured questionnaire to obtain information about tobacco consumption in the participants who have already smoked at least one waterpipe tobacco and cigarette entirely in their lifetime.
Smoking status was categorized into three groups: (1) never-smokers: participants who never smoked any cigarette or waterpipe during their lifetime; (2) former smokers: participants who smoked a cigarette or waterpipe in the past but had quit at the time of the interview; and (3) current smokers: participants who currently smoked cigarette or waterpipe at the time of the interview.
Our study also collected smoking data on intensity, duration, and ages at started smoking. Both current and ex-smokers were asked how many smokes per day. The number of smokes was categorized into never, less than 21 per day, and over 20 per day. For participants who didn’t smoke daily but occasionally during the week, the average daily smoking, calculated by the total amount of tobacco in 1 week divided by 7 days, was used. Duration of smoking (in years) was classified into never, less than 21 years, and over 20 years. Age at started smoking was categorized into never, over 20 years old, and less than 21 years old. The cumulative number of a smoke lifetime was calculated by average daily smoking (365 days) multiplied by the duration of smoking (year). This index was categorized into never, less than 201 times, and over 200 times.
Outcome ascertainment
The permanently appointed health workers collected NPC mortality and other causes of death monthly, including a medical doctor at each state commune health station. The underlying causes of death, the immediate cause of death, and contributing cause of death were determined by linking medical records available at the state commune health station (CHS), district hospital, provincial hospital, and other health facilities, or death certificates issued by the hospital where the patients had died. Within the first month of the death, the CHS of each commune in Vietnam received reports of all death cases from each family and clarified the underlying cause of death. Then, the CHS coded the cause of death according to ICD-1018. The malignant neoplasm of the nasopharynx was coded as C1118. In cases of dying at home without medical records in any hospital, validated WHO verbal autopsies were applied to determine the cause of death. A verbal autopsy is an interview with family members and caregivers of the deceased using a structured questionnaire to elicit signs and symptoms and other important information that can be used to determine the most likely cause of death19. Staff involved in the study followed the coding guidelines to apply ICD-10 rules to the diagnoses resulting from such an autopsy19. In populations lacking vital registration and medical certification, including Vietnam, this technique has become the primary source of information about causes of death19. Additionally, it was reported that verbal autopsies' sensitivity and positive predictive value reached 75 to 100% in the Vietnamese population20.
Follow-up and censoring of study participants
The follow-up of our study ended on December 31, 2019. Follow-up time in person-years was calculated from the baseline to the date of death from any cause, including NPC, the date the participant left the study areas, or the end of the follow-up period, whichever came first. In the current study, 217,531 person-years were estimated as the total for 20,144 men.
Covariate information
Our study adjusted for potential confounding factors suggested in the previous studies6,7. Covariates in this study include age; sex; education level; fridge availability at the household (represented socio-economic status); body mass index (BMI); alcohol consumption; total energy (kcal/day), protein (g/day), lipid (g/day), and carbohydrate (g/day) intake. The age (years) of the study population was categorized as follows (10–19, 20–29, 30–39, 40–49, 50–59, 60–69, 70–79, and 80+). Education level was classified into three groups: < 6 years (primary school or lower), 7+ years (secondary school or higher), and unknown. According to the recommendation of the World Health Organization for the Asian population, BMI was categorized into underweight (< 18.5 kg/m2), average (18.5–< 23 kg/m2), and overweight (23+ kg/m2)21. Fridge availability was either a “yes” or “no.” This index also indicated the participants’ economic status. Alcohol consumption was also classified as “yes” (ever consumed alcoholic drinks) or “no” (never consumed alcoholic beverages).
A validated semi-quantitative food frequency questionnaire (SQFFQ) was applied to the face-to-face interview to assess each food item's consumption frequency (using a specific portion size) over the last 12 months. SQFFQ was validated for evaluating nutrient intake in the general population in Northern Vietnam in 201722. Frequency of information was categorized into nine groups: never or < 1/month, 1–3/month, 1/week, 2–4/week, 5–6/week, 1/day, 2–3/day, 4–5/day, and ≥ 6/day. The Vietnam Food Composition Table was used to compute the nutrient composition23. Nutrient intake, including total energy, protein, lipid, and carbohydrate, was calculated by multiplying the nutrient composition of foods by the average daily intake and the reported frequency per year24.
Statistical analysis
Cox proportional hazard regression analysis was used to calculate hazard ratios (HR) and corresponding 95% confidence intervals (95% CI) to assess the association between exclusive waterpipe, exclusive cigarette, and NPC mortality. Never Smokers was used as a reference group. We used the Kaplan–Meier method to determine the survival estimates of waterpipe smoking compared to exclusive cigarette smoking. All tests were two-sided, and a p-value of less than 0.05 was accepted as statistically significant. In multivariable-adjusted models, the dose–response relationship was investigated using the trend test.
Ethics approval and consent to participate
The authors confirm following the study protocol that was approved by the Ethics Committee of IRB-Hanoi Medical University, Vietnam, for ethics in biomedical research implementation (Approval number NCS33/HMU-IRB dated 29 March 2019) and the IRB-International University of Health and Welfare, Japan (Approval number 21-Ig-92 dated 21 August 2021). The study is performed without intervention, a secondary analysis using existing data. We used the method of anonymous. Data is saved into a USB and private computer hard disk with a password. The principal investigator keeps the USB and computer secure and will not allow others to go through them except research team members. The data will be saved for 10 years after publication.
All methods were performed and carried out following relevant ethical guidelines and Vietnam's national regulations. We obtained written informed consent from all 12,746 households and their family members of 52,325 participants. All answers about smoking habits, diet-related factors, and family history will be anonymous by numbers.
Results
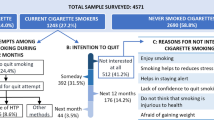
Among 20,144-man participants, the proportion of never smokers, exclusive waterpipe smokers, exclusive cigarette smokers, and dual waterpipe and cigarette smokers was 55.8%, 14.5%, 16.6%, and 13.1%, respectively. NPC death was 39-man cases and seven-woman cases. The proportion of women smokers was 1.9%, and they were excluded from the final analysis, Fig. 1. Survival estimates among exclusive waterpipe smokers were lowest compared to those of exclusive cigarette smokers. Dual cigarette and waterpipe smokers had an intermediate risk of decreased survival estimates, Fig. 2.
A null association between dual cigarette and waterpipe smoking and NPC mortality was seen according to intensity and years of smoking. Smoking before 21 significantly increased the risk of NPC, multivariable-HR (95% CI): 5.07 (1.57, 16.39), Table 1. A null association between exclusive cigarette smoking and NPC mortality was observed by the exposure to smoking intensity, duration, age of smoking initiation, and cumulative number of smoking lifetime, Table 2. A strong positive association between exclusive waterpipe smoking and NPC mortality according to intensity, duration, age of smoking initiation, and cumulative number of smoking lifetime. Per increment level of these exposures, respectively, multivariable-HR (95% CI): 1.35 (1.07, 1.71), p = 0.011; Multivariable-HR (95% CI): 1.26 (1.06, 1.50), p = 0.011; Multivariable-HR (95% CI): 1.31 (1.04, 1.66), p = 0.022 and Multivariable-HR (95% CI): 1.37 (1.08, 1.74), p = 0.011 were estimated, Table 3. Compared to exclusive cigarette smokers, exclusive waterpipe smokers significantly elevated the risk of NPC, multivariable-HR (95% CI): 4.51 (1.25, 16.31), p = 0.022. Dual cigarette and waterpipe smokers also increased the risk of NPC but insignificant, multivariable-HR (95% CI): 2.66 (0.66, 10.70), p = 0.167, Table 4.
Discussion
We observed a decrease in survival estimates and a significantly higher mortality rate of NPC among exclusive waterpipe smokers than exclusive cigarette smokers. Compared to never smoking, a strong positive association between exclusive waterpipe smoking and NPC mortality according to intensity, duration, age of smoking initiation, and cumulative number of smoking lifetime was also reported.
The association between cigarette smoking and NPC mortality remains limited. Friborg et al. conducted a prospective study on Singapore Chinese, the high-risk population that comprised the majority of undifferentiated NPCs (nearly 90%)14. This cohort study also did not report a statistically increased risk of NPC among current cigarette smokers compared with never smokers. The difference in the effect of smoking on NPC risk might depend on the histological type of NPC. In a recent study, undifferentiated carcinoma, which is the most common type of NPC in high-risk areas, seemed more strongly related to EBV infection other than cigarette smoking25. A lot of viral oncogenes related to EBV have been documented, such as Epstein–Barr nuclear antigen 1 (EBNA1), EBV-encoded small RNA 1/2 (EBER1/2), and Latent membrane protein 1 (LMP1)25. On the other hand, the hazard risk of cigarette smoking was found to be higher for differentiated than undifferentiated NPC26,27,28. Unlike undifferentiated NPC, differentiated NPC only accounts for a minor portion of NPC cases in such a high-risk population as Vietnam6. Wan-Lun Hsu et al. reported that EBV and cigarette smoking correlate with NPC25. In experimental studies, to develop nasopharyngeal carcinoma, EBV latent infection needs to be established on genetically altered or inflammatory nasopharyngeal epithelial cells15,29. Smoking may initiate the EBV-mediated carcinogenic process by damaging DNA through many pathways similar to smoking-induced lung cancer8. Mutations in KRAS and TP53 are well-known in smoking-related lung cancers8.
To the best knowledge, our study is the only one that reported the association between exclusive waterpipe and NPC. Regarding a similar Arabian waterpipe called shisha, there is only one case–control analysis of the relationship between shisha smoking and NPC. Feng et al. reported a null association between Shisha smoking and NPC with an odds ratio of 0.49 (95% CI 0.20–1.23)30. This case–control study might be suffered from a recall bias when the proportion of ever Shisha smoking was only 2% (9/450 NPC cases).
Waterpipe smoking was reported to be associated with oral cancer, oesophageal cancer, urinary bladder cancer, especially respiratory diseases, and lung cancer, regarding long-term health hazards31. There is evidence of the association between waterpipe smoking and chronic obstructive pulmonary disease32. This disease is strongly associated with lung cancer. Other head and neck cancers, such as oral cancer, are reported to have a positive association with waterpipe smoking33,34.
Waterpipe is believed to be safer than cigarette smoking for a long time because the smoke is filtered through a column of water before being inhaled. However, even passing through water, the eliminated concentration of toxins is limited. It is reported that a single waterpipe session exposes the smoker to 3–9 times the CO, 1.7 times the nicotine, 8–15 times PAHs, 6–9 times formaldehyde, as well as heavy metals such as Arsenic, Chromium, and Lead when compared to cigarette smoking35. Moreover, waterpipe tobacco involves Nicotiana rustica leaves that contain a higher level of nicotine (9%) than cigarettes (1–3%)36. Additionally, tobacco is indirectly heated at a lower temperature. These toxic substances produced by waterpipe smoking may be different from or even more hazardous than cigarettes.
There is no precise mechanism explaining the relationship between waterpipe and NPC. Over 60 carcinogens can covalently bind to DNA directly or after metabolism, forming DNA adducts8. DNA adducts are central to chemical carcinogenesis because they can cause miscoding and permanent mutations8. Aside from this significant pathway, though not carcinogenic, high exposure to nicotine in waterpipe smokers may facilitate carcinogenesis by activating serine/threonine kinase Akt (also known as protein kinase B), protein kinase A, and other changes8. PAHs and nitrosamines may account for some base-substitution mutagenicity8. In addition, waterpipe smoking increased transmittable risk due to the shared pipe among smokers. Waterpipe-mediated EBV infection has been cautioned by WHO37. Again, EBV infection is an important risk of NPC25. These factors suggest that waterpipes may be more hazardous to health than cigarettes.
This study has many strengths. First, this is a prospective cohort study performed in a high-risk population. The subgroup analyses of various smoking habits, such as smoking status, intensity, duration, age of smoking initiation, and the cumulative amount of smoking, produced a precise quantification of the relationship between tobacco and NPC mortality. Exclusive cigarette, exclusive waterpipe, and dual cigarette and waterpipe smoking were stratified to estimate how the mortality hazard rate differs by smoking type. Second, advanced adjustment variables for age, sex, education level, available fridge, BMI, alcohol consumption, total energy intake, protein intake, lipid intake, and carbohydrate intake were included.
Our study has certain limitations. First, histological types of NPC cases and EBV infection status were not assessed. Further studies should investigate the relationship between cigarette and waterpipe smoking, EBV, and NPC. Second, our study analyses Vietnamese men in the high-risk population only. Therefore, our findings may not be generalized to women and people not in endemic regions. Third, although the general sample of this cohort is large, the NPC death cases are limited. This is an attribute of the low incidence of this type of cancer. Further investigations, such as case–control studies and review papers, are needed to enhance the evidence of this association. Lastly, mortality was used as an outcome determination, which may underestimate the association between smoking and NPC.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- NPC:
-
Nasopharyngeal cancer
- BMI:
-
Body mass index
- OR (95% CI) :
-
Odds ratio (95% confidence interval)
- SQFFQ:
-
Semi-quantitative food frequency questionnaire
- EBV:
-
Epstein–Barr virus
- CHS:
-
Commune health station
References
Chang, E. T., Ye, W., Zeng, Y. X. & Adami, H. O. The evolving epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol. Biomark. Prev. 30(6), 1035–1047. https://doi.org/10.1158/1055-9965.EPI-20-1702 (2021).
Li, C. C., Yu, M. C. & Henderson, B. E. Some epidemiologic observations of nasopharyngeal carcinoma in Guangdong, People’s Republic of China. Natl. Cancer Inst. Monogr. 69, 49–52 (1985).
Wee, J. T., Ha, T. C., Loong, S. L. & Qian, C. N. Is nasopharyngeal cancer really a “Cantonese cancer”?. Chin. J. Cancer 29(5), 517–526. https://doi.org/10.5732/cjc.009.10329 (2010).
World Health Organization. GLOBOCAN 2020 Viet Nam (2020).. Retrieved from https://gco.iarc.fr/today/data/factsheets/populations/704-viet-nam-fact-sheets.pdf, access Jan 1st, 2023.
Thompson, L. D. Update on nasopharyngeal carcinoma. Head Neck Pathol. 1(1), 81–86. https://doi.org/10.1007/s12105-007-0012-7 (2007).
Chang, E. T. & Adami, H. O. The enigmatic epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol. Biomark. Prev. 15(10), 1765–1777. https://doi.org/10.1158/1055-9965.EPI-06-0353 (2006).
Wu, L., Li, C. & Pan, L. Nasopharyngeal carcinoma: A review of current updates. Exp. Ther. Med. 15(4), 3687–3692. https://doi.org/10.3892/etm.2018.5878 (2018).
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Personal Habits and Indoor Combustions. International Agency for Research on Cancer (2012) (IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 100E). TOBACCO SMOKING. https://www.ncbi.nlm.nih.gov/books/NBK304395/
Flanders, W. D., Lally, C. A., Zhu, B. P., Henley, S. J. & Thun, M. J. Lung cancer mortality in relation to age, duration of smoking, and daily cigarette consumption: Results from Cancer Prevention Study II. Cancer Res. 63(19), 6556–6562 (2003).
Blot, W. J. et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 48(11), 3282–3287 (1988).
Liaw, K. M. & Chen, C. J. Mortality attributable to cigarette smoking in Taiwan: A 12-year follow-up study. Tob. Control 7(2), 141–148. https://doi.org/10.1136/tc.7.2.141 (1998).
Chow, W. H. et al. Tobacco use and nasopharyngeal carcinoma in a cohort of US veterans. Int. J. Cancer 55, 538–540. https://doi.org/10.1002/IJC.2910550403 (1993).
Doll, R., Peto, R., Boreham, J. & Sutherland, I. Mortality from cancer in relation to smoking: 50 years observations on British doctors. Br. J. Cancer 92(3), 426–429. https://doi.org/10.1038/sj.bjc.6602359 (2005).
Friborg, J. T. et al. A prospective study of tobacco and alcohol use as risk factors for pharyngeal carcinomas in Singapore Chinese. Cancer 109(6), 1183–1191. https://doi.org/10.1002/cncr.22501 (2007).
Hsu, W. L. et al. Independent effect of EBV and cigarette smoking on nasopharyngeal carcinoma: A 20-year follow-up study on 9,622 men without family history in Taiwan. Cancer Epidemiol. Biomark. Prev. 18(4), 1218–1226. https://doi.org/10.1158/1055-9965.EPI-08-1175 (2009).
Duc, T. Q. et al. Waterpipe smoking and lung cancer: A review. Int. J. Recent Sci. Res. 9(7), 27983–27990. https://doi.org/10.24327/ijrsr.2018.0907.2371 (2018).
le Xuan, T. T. et al. Prevalence of waterpipe tobacco smoking among population aged 15 years or older, Vietnam, 2010. Prev. Chronic Dis. 10, E57. https://doi.org/10.5888/pcd10.120100 (2013).
World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision (World Health Organization, 2016).
World Health Organization. Verbal Autopsy Standards: Ascertaining and Attributing the Cause of Death (World Health Organization, 2007).
Tran, H. T., Nguyen, H. P., Walker, S. M., Hill, P. S. & Rao, C. Validation of verbal autopsy methods using hospital medical records: A case study in Vietnam. BMC Med. Res. Methodol. 18(1), 43 (2018).
World Health Organization Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363(9403), 157–163 (2004).
Le, T. N. et al. Reproducibility of a designed semi-quantitative food frequency questionnaire in general populations in North Vietnam. Southeast Asian J. Sci. 6, 191–200 (2018).
Ministry of Health. Vietnamese food composition table (2000) (Medical Publishing House, 2007). https://www.fao.org/fileadmin/templates/food_composition/documents/pdf/VTN_FCT_2007.pdf
Willett, W. Total Energy Intake: Implications for Epidemiologic Analyses in Nutritional Epidemiology (Oxford University, 2013).
Tsang, C. M. & Tsao, S. W. The role of Epstein–Barr virus infection in the pathogenesis of nasopharyngeal carcinoma. Virol. Sin. 30(2), 107–121. https://doi.org/10.1007/s12250-015-3592-5 (2015).
Polesel, J. et al. Tobacco smoking, alcohol drinking, and the risk of different histological types of nasopharyngeal cancer in a low-risk population. Oral Oncol. 47(6), 541–545. https://doi.org/10.1016/j.oraloncology.2011.03.017 (2011).
Sasco, A. J., Secretan, M. B. & Straif, K. Tobacco smoking and cancer: A brief review of recent epidemiological evidence. Lung Cancer (Amsterdam, Netherlands) 45(Suppl 2), S3–S9. https://doi.org/10.1016/j.lungcan.2004.07.998 (2004).
Xue, W.-Q., Qin, H.-D., Ruan, H.-L., Shugart, Y. Y. & Jia, W.-H. Quantitative association of tobacco smoking with the risk of nasopharyngeal carcinoma: A comprehensive meta-analysis of studies conducted between 1979 and 2011. Am. J. Epidemiol. 178(3), 325–338. https://doi.org/10.1093/aje/kws479 (2013).
Young, L. S. & Dawson, C. W. Epstein–Barr virus and nasopharyngeal carcinoma. Chin. J. Cancer 33(12), 581–590. https://doi.org/10.5732/cjc.014.10197 (2014).
Feng, B. J. et al. Cannabis, tobacco, and domestic fumes intake are associated with nasopharyngeal carcinoma in North Africa. Br. J. Cancer 101(7), 1207–1212. https://doi.org/10.1038/sj.bjc.6605281 (2009).
World Health Organization. Waterpipe Tobacco Smoking: Health Effects, Research Needs and Recommended Actions by Regulators (World Health Organization, 2005).
El-Zaatari, Z. M., Chami, H. A. & Zaatari, G. S. Health effects associated with waterpipe smoking. Tob. Control 24(Suppl 1), i31–i43. https://doi.org/10.1136/tobaccocontrol-2014-051908 (2015).
Dangi, J., Kinnunen, T. H. & Zavras, A. I. Challenges in the global improvement of oral cancer outcomes: Findings from rural Northern India. Tob. Induced Dis. 10, 5. https://doi.org/10.1186/1617-9625-10-5 (2012).
Ali, A. A. Histopathologic changes in oral mucosa of Yemenis addicted to water-pipe and cigarette smoking in addition to takhzeen al-qat. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 103(3), e55–e59. https://doi.org/10.1016/j.tripleo.2006.10.008 (2007).
Maziak, W. The waterpipe: An emerging global risk for cancer. Cancer Epidemiol. 37(1), 1–4. https://doi.org/10.1016/j.canep.2012.10.013 (2013).
She, J. et al. Chinese water-pipe smoking and the risk of COPD. Chest 146(4), 924–931. https://doi.org/10.1378/chest.13-1499 (2014).
Meleigy, M. Waterpipe and communicable diseases link, says WHO. Lancet Infect. Dis. 7(7), 448. https://doi.org/10.1016/S1473-3099(07)70150-0 (2007).
Acknowledgements
The authors would like to thank all the participants in the three northern provinces of Vietnam for the time and effort they devoted to this study. The Vietnam Ministry of Science and Technology supported the survey for 2006–2011 and 2017–2019. When preparing this manuscript, Ngoan Tran LE is affiliated with the International University of Health and Welfare, School of Medicine, Dept. of Public Health.
Author information
Authors and Affiliations
Contributions
All authors reviewed the manuscript and contributed revisions. H.D.K., T.G.N., D.T.T.T., K.X.N., S.I., and N.T.L. were mainly responsible for drafting, revision, and analysis. H.D.K., K.X.N., and N.T.L. were principally responsible for data collection. T.G.N., D.T.T.T., K.X.N., and N.T.L. extracted data and were mainly responsible for managing and analyzing data. T.G.N., D.T.T.T., and N.T.L. were major contributors to writing the manuscript. All authors approved the version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nguyen, T.G., Kieu, H.D., Truong, D.T.T. et al. Exclusive waterpipe smoking and the risk of nasopharynx cancer in Vietnamese men, a prospective cohort study. Sci Rep 13, 13237 (2023). https://doi.org/10.1038/s41598-023-40253-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-40253-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.