Abstract
Ethiopia has implemented maternity waiting homes over the last several decades; however, its utilization is low. This study aimed to assess the factors associated with knowledge of and attitude towards maternity waiting homes among pregnant women in rural Ethiopia. The baseline survey was conducted from September 15 to October 30, 2022, in rural Southern Ethiopia. Survey data were collected from 320 women in their second trimester of pregnancy. The data analysis was performed using SPSS version 25. The mean age of the participants was 27.79 (SD ± 6.242) years. Nearly two-thirds (57.5%) of the participants had no formal education and more than three-fourths (72.5%) were housewives. Only approximately one-fourth (23.75%) of the participants used maternity waiting homes. Furthermore, 33.75% had good knowledge, 28.75% had favorable attitudes, and around one-fourth (26.25%) had good male partner involvement. Age group 30 to 39 years (AOR 4.78, 95% CI 1.12–20.36), household income (AOR 6.41, 95% CI 2.78–14.81), having pregnancy intention (AOR 2.63, 95% CI 1.21–5.73), and history of obstetric complications (AOR 6.72, 95% CI 2.81–16.07) were significantly associated with good knowledge about maternity waiting homes. Similarly, age group 30 to 39 years (AOR 4.23, 95% CI 1.14–15.65), household income (AOR 7.12, 95% CI 3.26–15.55), having pregnancy intention (AOR 2.57, 95% CI 1.21–5.47), and history of obstetric complications (AOR 5.59, 95% CI 2.30–13.59) were significantly associated with favorable attitudes towards maternity waiting homes. Providing health education and promoting male partner participation through educating couples may improve women’s access to maternity waiting homes.
Similar content being viewed by others
Introduction
Globally, the maternal mortality ratio was estimated to be 223 per 100,000 live births in 2020 and majority (95%) of maternal deaths have been reported to occur in resource-limited settings1. Sub-Saharan Africa alone accounts for approximately three-fourths of maternal deaths, and the maternal mortality ratio in Ethiopia is estimated to be 401 per 100,000 live births1,2. The leading causes of maternal deaths are obstetric hemorrhage, hypertensive disorders in pregnancy, non-obstetric complications, pregnancy-related infections, and unsafe abortion3,4. Most maternal deaths owing to these causes are preventable by enabling timely access to obstetric care2,5. However, poor access to obstetric facilities due to long distances, lack of transportation, and unfavorable road conditions aggravated women’s inability to receive timely obstetric care6,7.
Increasing health facility deliveries is vital for reducing maternal and neonatal mortality8. Although health facility delivery has been promoted in Ethiopia, home delivery is still common, primarily in geographically isolated areas9. The 2019 Mini Ethiopian Demographic and Health Survey showed that 48% of live births were delivered in a health facility, and access to health facilities is mentioned to be more difficult in rural areas than in urban areas because of distance, scarce transport, and a lack of appropriate facilities10. Maternity waiting home (MWH) has been recognized as a strategy to improve maternal health outcomes by bringing women in hard-to-reach areas closer to health facilities11. MWH is a shelter located near or in a health facility where women near their delivery date can stay and be transferred to obstetric facility shortly before childbirth or earlier if complications arise12. Ethiopia has implemented MWHs for the last several decades; however, its uptake is low13,14.
Lack of awareness about MWHs, women’s perceptions of the quality of care at MWHs, poor provider interactions with women staying at MWHs, poor physical aspects of MWHs, staff shortages, and household chores are some of the important barriers to staying at MWHs15,16,17. Use of MWHs also depends largely on male partners’ decisions18,19. Furthermore, a study from Northwest Ethiopia showed that antenatal care (ANC) visits, short distance to health facilities, women’s involvement in decision making, and MWH use were found to be associated with maternal knowledge, whereas higher education status, ANC visits, and short distance to the facility were associated with maternal attitudes towards MWHs20. However, further studies are required to have a comprehensive understanding about factors associated with women’s knowledge and attitudes regarding MWHs in rural Ethiopia.
Methods and materials
Study setting
The baseline data used in this analysis were collected from Ana Lemo and Gibe districts of Hadiya Zone of southern Ethiopia from September 15 to October 30, 2022. The two districts were purposefully selected based on the availability of functional MWHs. Based on the information we obtained from the Zonal health department, the total estimated population of the two districts was 265,000 in 2021. The two districts were divided into 52 clusters/kebeles (the smallest administrative units). One cluster has an average of 5000 population. There was one primary hospital, 10 health centers, 10 MWHs and 42 health posts in the two districts including two health centers and MWHs added from an adjacent district (Misha district). The livelihood of the population mainly depends on agriculture.
Study participants
The study participants were pregnant women in the beginning of second trimesters of pregnancy (14–16 weeks of gestation) who were permanent residents of the study area, gave birth within the last 5 years preceding the current pregnancy, were living with their male partners at the time of data collection, were living ≥ 2 h of walking distance from the nearest health facility21 and had limited access to public transportation.
Background about the trial
The data source for this analysis was a baseline survey conducted prior to intervention roll-out in an ongoing cluster-randomized trial aimed to evaluate the effectiveness of health education provided to couples on improving knowledge, attitude, and uptake of MWHs: group health education, home visits and provision of take-home print materials (ClinicalTrials.gov Identifier: NCT05015023). The intervention was provided at three contact points. The first contact point was the group health education at baseline whereas the second, and third contacts were home visits. Leaflets /print health messages were provided at each contact.
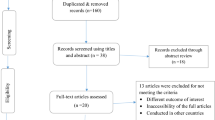
Sample size calculations
The Hooper and Bourke method for cluster randomization studies of parallel arms with repeated cross-sections was used to calculate the sample size22. To illustrate within intra-cluster correlation coefficient (ICC) and between ICC, the technique comprises the measurement of two design effects, with the product of the two being used to inflate the sample size for individual randomization. The within ICC was the correlation between any two pregnant women in the same cluster, while the between ICC was the correlation between any two pregnant women in different clusters. The first design effect (dc) attributable to cluster randomization was measured using a within ICC of 0.05 obtained from a community-based cluster randomized trial in Ethiopia23. The design effect (dc) was calculated as:
where m is the cluster size assumed to be 20 (i.e., the total number of pregnant women who were questioned in each cluster) and ρ was the within ICC.
The second design effect (dr) attributable to repeated evaluations (baseline/endline) was calculated by using the within ICC and a cluster autocorrelation coefficient (π) of 0.8022.
The second design effect (dr) was calculated as:
where \(r=\left(\frac{m\rho \pi }{{d}_{c}}\right).\)
The required sample size was then calculated by multiplying the ‘sample size assuming individual randomization’ by both design effects (dc and dr). It was calculated as:
where \(n\) represents the sample size in each of the arms i.e., intervention and control. \(a\) represents conventional multiplier (1.96) for alpha \(\left(\alpha =0.05\right)\) and \(b\) represents conventional multiplier (0.842) for power \((1-\beta =0.80)\). \({p}_{1}\) represents proportion of post-intervention users of MWH and \({q}_{1}\) represents proportion of post-intervention non-users of MWH. \({p}_{2}\) represents proportion (50%) of users of MWH taken from a study in Gurage Zone, Southwest Ethiopia24 and \({q}_{2}\) represents pre-intervention proportion of non-users of MWH. \(|{p}_{1}-{p}_{2}|\) an effect size—was an absolute change in proportion of MWH utilization after intervention. It was estimated to be 20%.
In addition, the following parameters were considered: 95% CI 80% power, 1:1 allocation ratio of intervention to control, 10% potential loss to follow up, and tabulated sample size \(({n}_{0}=199)\) required to detect a difference in two proportions at 5% significance level with 80% power in literature25. According to Hooper and Bourke, the number of clusters (K) for the sample was determined using the formula \(K=\left({n}_{0}{d}_{c}{d}_{r}\right)/m\). The final sample size was calculated by substituting the specified values into the above formula. Hence, a total of 16 clusters were needed, with an approximated final sample size of 320. The two arms each had 160 eligible pregnant women (with their male partners).
Ethics approval
Ethical approval letter was received from the IRB of Jimma University with reference number JUIRB-33/22, dated 09/02/2022. Consequently, a letter of permission was obtained from the Health Department of the Hadiya Zone, southern Ethiopia. The study participants were informed about the objective of the study, and written informed consent was obtained from each participant prior to the start of data collection. This study was registered in ClinicalTrials.gov with Identifier: NCT05015023. Link: https://clinicaltrials.gov/ct2/show/NCT05015023. All methods were performed in accordance with the relevant guidelines and regulations including the ethical guidelines of the Jimma University Ethical Review Committee and the declaration of Helsinki.
Baseline survey
The baseline survey targeted 320 pregnant women from 16 clusters. There were 160 participants in each of the two arms with an average number of 20 participants in a cluster. Structured questionnaires were used to collect data through face-to-face interviews. The questionnaires were adapted from literature such as Ethiopian Demographic and Health Surveys and a global framework for assessing male involvement in maternal health26,27. The questionnaires were prepared in English, translated into local language (Amharic) and pre-tested. The pre-test was performed on 10% of the calculated sample size in Misha Woreda, a district outside of our study sites. Next, Cronbach’s Alpha was calculated using SPSS version 25 to test internal consistency of the knowledge, attitude and male partner involvement questions and Cronbach’s Alpha value greater than 0.7 was considered reliable. The data were collected on study variables such as socio-demographic characteristics, knowledge, attitude, and health service utilizations including MWH use (Additional file 1). The principal investigator and the other two field supervisors supervised the data collection. All the participants responded to the questionnaires.
Variables of interest and measurement
The primary outcome variable was the self-reported proportion of MWH use for any pregnancy in the last 5 years whereas the secondary outcomes were knowledge of and attitudes toward MWHs. In this analysis, we aimed to assess the factors associated with knowledge and attitude towards MWHs. The proportion of MWH uptake was measured as the number of women who reported staying at MWH for at least one day for any pregnancy in the last 5 years divided by the number of women who gave birth during the same period (among the women enrolled in the trial) × 100. Knowledge was measured using 7 “Yes” or “No” questions. “Yes” was denoted by “1” and “No” was represented by “0”. Then the sum average for a respondent above the median (Y ≥ 4) was considered good knowledge and below 4 was considered poor knowledge. Attitude was measured using 5 points Likert scales (very disagree, disagree, neutral, agree, very agree). Five questions were used to measure attitude. Average scores above median were considered favorable attitude whereas average scores below median were considered unfavorable attitude.
To assess male partner involvement, we adopted a tool from a global framework for assessing male involvement in maternal health27. The global framework has 5 domains (involvement in communication, involvement in decision-making, practical support, physical support, and emotional support). Each of the 5 domains has 3–5 questions, with a total of 21 questions. We carefully adopted the tool to our context and collected the data. In this analysis, we selected 9 indicators (“Yes” or “No” questions) to measure the level of male partner involvement in maternal health. “Yes” scores above median (Y ≥ 5) were considered good male partner involvement and “Yes” scores below median (Y ≤ 4) were considered poor male involvement.
Data analysis
The data analysis was conducted using SPSS Version 25. Descriptive statistics were performed and the results were presented using text, tables, and graphs. Bivariate and multivariate logistic regression analyses were conducted to identify the factors associated with pregnant women’s knowledge of and attitude toward MWHs. In logistic regressions, crude odds ratio (COR) and adjusted odds ratio (AOR) with the corresponding 95% confidence intervals were computed to show the strength of the association. Variables with p-value < 0.25 at bivariate analysis were fitted into the multivariate analysis. In the multivariate analysis, statistical significance was declared at a p-value of < 0.05. The Hosmer–Lemeshow test was used to check the goodness of fit for the logistic regression.
Result
Sociodemographic characteristics
Three hundred-twenty participants were included in the study. Nearly three-fourths (68.75%) of the participants were aged 20–29 years, and the mean age was 27.79 (SD 6.242) years. About half (53.75%) were from the ethnic group of Hadiya. One hundred eighty-four (57.5%) participants had no formal education, and more than three-fourths (72.5%) were housewives (Table 1).
Obstetric related factors
Two hundred thirty-two (72.5%) and 224 (70%) participants reported parity and gravidity of four or fewer, respectively. Two hundred and seventy-two (85%) participants reported planned pregnancies, 40 (12.5%) reported gestational age at birth less than or equal to 37 weeks, and 88 (27.5%) reported a history of obstetric complications. Most of the deliveries (83.75%) were normal vaginal deliveries, whereas instrumental assisted and cesarean section births were 12.5% and 3.75%, respectively. Stillbirth was reported by 36 (11.25%) respondents (Table 2).
Maternal health service-related factors
The proportion of participants who received ANC (at least once) was 124 (38.75%), and 76 (23.75%) used MWH. There were 84 (26.25%) institutional deliveries and 68 (21.25%) PNC visits within two weeks after delivery. Eighty-four (26.25%) participants were assessed to have good involvement of male partners in maternal health (Table 3).
Knowledge and attitude related to MWHs
About 108 (33.75%) of the participants demonstrated good knowledge of MWHs and 92 (28.75%) had favorable attitude towards MWHs.
Factors associated with knowledge of and attitude towards MWHs
In the bivariate logistic regression, household income, pregnancy intention, and history of obstetric complications were associated with both knowledge and attitude towards MWHs. Educational status was inversely associated with knowledge and attitude whereas age was not associated with either knowledge or attitude towards MWHs. In the multivariate regression, age (30–39 years), household income, pregnancy intention (having wanted pregnancy), and history of obstetric complications were statistically associated with good knowledge of and favorable attitude towards MWHs.
Consequently, women in the age group 30–36 years (AOR 4.78, 95% CI 1.12–20.36) were nearly 5 times more likely to have good knowledge about MWHs compared to women in the age group ≥ 40 years. Women with average household monthly income below 7985 ETB (AOR 6.41, 95% CI 2.78–14.81) were 6 times more likely to have good knowledge of MWHs compared to women with household income above 7985 ETB per month. Likewise, women having wanted pregnancy (AOR 2.63, 95% CI 1.21–5.73) and those having a history of obstetric complications (AOR 6.72, 95% CI 2.81–16.07) were nearly 3 times and 7 times more likely to have good knowledge of MWHs compared to women having unwanted pregnancy and those had no history of obstetric complications, respectively (Table 4).
Furthermore, women in the age group (30–39 years) (AOR 4.23, 95% CI 1.14–15.65) were 4 times more likely to have a favorable attitude towards MWHs compared to women in the age group ≥ 40 years. Participants with household income below 7895 ETB (AOR 7.12, 95% CI 3.26–15.55) were 7 times more likely to have good attitude towards MWHs compared to those with household income above 7895 ETB. Similarly, women having wanted pregnancy (AOR 2.57, 95% CI 1.21–5.47) and those having a history of obstetric complications (AOR 5.59, 95% CI 2.30–13.59) were nearly 3 times and 6 times more likely to have good attitude towards MWHs compared to women having unwanted pregnancy and those had no history of obstetric complications, respectively (Table 5).
Discussion
This study was a cross-sectional analysis of baseline data from a cluster randomized trial conducted in rural Ethiopia. The participants were pregnant women in their second trimester. This analysis considered data collected on women’s experiences related to MWHs with the most recent pregnancy and birth before their current pregnancy. The findings showed that 33.75% had good knowledge of MWHs, 28.75% had favorable attitudes towards MWHs, 26.25% had good male partner involvement, and 23.75% used MWHs.
In this study, we found that around one-third (33.75%) of women had good knowledge about MWHs. Possible reasons that only one-third had good knowledge may be that most women who participated in this study had no formal education, low access to ANC, and poor access to health information due to long distances from health facilities. This finding is in line with studies from southern and central Ethiopia, which revealed that only 7% and 47.7% of women, respectively, had awareness about MWHs28,29. This finding contrasts another study from Ethiopia in which a significant proportion (87.7%) of the participants reported having awareness about MWHs30. We suggest one of the reasons for this difference may be the differences in health system related factors such as leadership, and access to health facilities including transportation; however, it requires further research. Furthermore, the current study showed that only 28.75% of the participants had favorable attitude towards MWHs. Possible reasons for this low-level attitude towards MWH may be poor ANC attendance, low institutional delivery practice, lack of awareness about MWH, and a low level of male partners’ participation in maternal health. Likewise, another study showed that less than half (48.8%) of women had favorable attitude towards using MWHs31, though this is still far from our finding. In contrast, a study showed that more than two-thirds (65.3%) of women had favorable attitude towards MWHs32. The possible reason for these differences may be sociodemographic or health system related factors.
The study revealed that the MWH utilization was 23.75%. The reasons for this low utilization of MWHs may be the low levels of good knowledge and favorable attitudes toward MWHs among the participants. Poor involvement of male partners in maternal health might also have affected women’s access to MWHs, as males are the main decision makers. In support of this, other studies from Ethiopia found that the MWH uptake was low33,34. The reason for this may be the observed similarity in participants educational status (i.e., majority of the participants had no formal education) in study settings; however, this requires further investigation. In contrast, another study from the Sidama Zone, Ethiopia, showed that more than two-thirds (67.25%) of women used MWHs30. One reason for this significant variance may be the differences in the level of awareness of MWHs. For example, in our study, only one-third of the women had good knowledge of MWHs, whereas in the above-mentioned study from the Sidama Zone30, more than three-fourths reported that they were aware of MWHs. Furthermore, a systematic review revealed that a lack of knowledge about MWHs was one of the reasons for the poor utilization of MWHs35. This finding implies that a lack of awareness may affect women’s access to MWHs. Therefore, improving maternal knowledge and attitude regarding MWH may improve access to MWHs among pregnant women in rural Ethiopia.
The current study showed that educational status was inversely associated with knowledge and not associated with attitudes towards MWHs. This might imply that those who have some formal schooling may have less concerns to the MWH services or were not using MWHs. This is consistent with findings from a study in Ethiopia31 whereas it contrasts with a study from Somaliland36. Further studies are needed to justify why having no or lower educational status was found to be associated with the knowledge of MWHs. Besides, in the current study, a history of obstetric complications and pregnancy intention (wanted pregnancy) were associated with knowledge of and attitudes toward MWHs. One reason may be that women who experienced pregnancy-related complications had painful experiences and, therefore, developed better health-seeking behavior and preferred to stay near health facilities to seek immediate obstetric care for their current pregnancy. Moreover, women who want to get pregnant may also have a better attitude towards staying at MWH, as they need newborns. Similarly, other studies have shown that a history of complications in previous childbirth and pregnancy intention was associated with the intention to use MWHs28. Educating women to have a planned pregnancy and providing them with information about MWH during health care visits may improve maternal knowledge and attitude towards MWHs. This may in turn improve maternal and newborn health outcomes by improving women’s access to MWHs.
Limitations of the study
Recall bias may have affected our findings. Because the participants were asked about their experiences of last childbirth.
Conclusion and recommendation
The majority of participants had poor knowledge of MWHs, unfavorable attitudes toward MWHs, and poor male partner involvement. The utilization of MWHs is low. Age, household income, pregnancy intention, and history of obstetric complications were associated with knowledge and attitude towards MWHs. Providing health education may improve women’s awareness and attitude towards MWHs. Age group and level of household income should be considered in planning and implementing MWH related behavioral interventions. Promoting male partner participation through educating couples may improve women’s access to MWHs.
Data availability
The data will be made available from the corresponding author up on request.
References
World Health Organization. Trends in maternal mortality 2000 to 2020: Estimates [internet]. WHO, Geneva. [cited 2023 June 25]. https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/.
World Health Organization. An evidence brief on maternal mortality [internet]. WHO, 2019. [cited 2022 Nov 18] https://apps.who.int/iris/bitstream/handle/10665/329886/WHO-RHR-19.20-eng.pdf.
Musarandega, R., Nyakura, M., Machekano, R., Pattinson, R. & Munjanja, S. P. Causes of maternal mortality in sub-Saharan Africa: A systematic review of studies published from 2015 to 2020. J. Glob. Health. https://doi.org/10.7189/jogh.11.04048 (2021).
Berhan, Y. & Berhan, A. Causes of maternal mortality in Ethiopia: A significant decline in abortion related death. Ethiop. J. Health Sci. 24(8), 15–28. https://doi.org/10.4314/ejhs.v24i0.3S (2014).
Soma-Pillay, P. & Pattinson, R. C. Barriers to obstetric care among maternal near-misses. S. Afr. Med. J. 106(11), 1110–1113. https://doi.org/10.7196/SAMJ.2016.v106i11.10726 (2016).
Acevedo, P., Martinez, S., Pinzon, L., Sanchez-Monin, E. & Winters, S. Distance as a barrier to obstetric care among indigenous women in Panama: A cross-sectional study. BMJ Open 10(3), 1–11. https://doi.org/10.1136/bmjopen-2019-034763 (2020).
Alemayehu, M., Yakob, B. & Khuzwayo, N. Barriers and enablers to emergency obstetric and newborn care services use in Wolaita Zone, Southern Ethiopia: A qualitative case study. BMC Public Health https://doi.org/10.1186/s12889-022-14504-y (2022).
Yaya, Y., Eide, K. T., Norheim, O. F. & Lindtjørn, B. Maternal and neonatal mortality in Southwest Ethiopia: Estimates and socio-economic inequality. PLoS ONE https://doi.org/10.1371/journal.pone.0096294 (2014).
Chernet, A. G., Dumga, K. T. & Cherie, K. T. Home delivery practices and associated factors in Ethiopia. J. Reprod. Infertil. 20(2), 102–108 (2019).
Ethiopian Public Health Institute (EPHI), ICF. Ethiopia Mini Demographic and Health Survey 2019: final report [internet]. 2021. 1–207. [cited 2023 June 24] https://dhsprogram.com/pubs/pdf/FR363/FR363.pdf.
Perosky, J. E. et al. Maternity waiting homes as an intervention to increase facility delivery in rural Zambia. Int. J. Gynecol. Obstet. 146(2), 266–267. https://doi.org/10.1002/ijgo.12864 (2019).
World Health Organization. Maternity waiting homes: a review of experiences [Internet]. WHO. 1996:40. [cited 2022 Nov 12] https://apps.who.int/iris/handle/10665/63432.
Gaym, A., Pearson, L. & Soe, K. W. W. Maternity waiting homes in Ethiopia: Three decades experience. Ethiop. Med. J. 50(3), 209–219 (2012).
Kassa, B. G., Ayele, A. D., Belay, H. G., Mihiretie, G. N. & Worke, M. D. Utilisation of maternity waiting homes and its associated factors in Ethiopia: Systematic reviews and meta-analysis. Clin. Epidemiol. Glob. Health. https://doi.org/10.1016/j.cegh.2021.100891 (2021).
Gurara MK, Jacquemyn Y, Ukke GG, Geertruyden J-P Van, Draulans V. Benefits, barriers and enablers of maternity waiting homes utilization in Ethiopia: An integrative review of national implementation experience to date. (2021). https://doi.org/10.1186/s12884-022-04954-y.
Gurara, M. K., Geertruyden, J.-P., Jacquemyn, Y. & Draulans, V. Stakeholders perspectives on the implementation of maternity waiting homes in rural Ethiopia: A qualitative study. Res. Sq. https://doi.org/10.21203/rs.3.rs-971096/v1 (2021).
Nigussie, T. et al. Maternity waiting facilities for improving maternal and neonatal outcome in low-resource countries. PLoS ONE 13(1), 1–8. https://doi.org/10.1002/14651858.CD006759.pub2 (2019).
Kebede, K. M. & Mihrete, K. M. Factors influencing women’s access to the maternity waiting home in rural Southwest Ethiopia: A qualitative exploration. BMC Pregnancy Childbirth. 20(1), 1–12. https://doi.org/10.1186/s12884-020-02988-8 (2020).
Jody, R. L., Anna, C. W. & Michelle, L. M. S. R. Promoting access: The use of maternity waiting homes to achieve safe motherhood. Midwifery 29(10), 16. https://doi.org/10.1016/j.midw.2013.07.020 (2013).
Anteneh, T. A. et al. Knowledge and attitude of women towards maternity waiting homes and associated factors among women who gave birth in the last twelve months in Dega Damot district, northwest Ethiopia. Front. Glob. Women’s Health. 4, 1–10. https://doi.org/10.3389/fgwh.2023.988328 (2023).
Lori, J. R. et al. Increasing facility delivery through maternity waiting homes for women living far from a health facility in rural Zambia: A quasi-experimental study. BJOG Int. J. Obstet. Gynaecol. 128(11), 1804–1812. https://doi.org/10.1111/1471-0528.16755 (2021).
Hooper, R. & Bourke, L. Cluster randomised trials with repeated cross sections: Alternatives to parallel group designs. BMJ https://doi.org/10.1136/bmj.h2925 (2015).
Alemayehu, M., Medhanyie, A. A., Reed, E. & Bezabih, A. M. Use of community-based intervention to promote family planning use among pastoralist women in Ethiopia: Cluster randomized controlled trial. medRxiv. https://doi.org/10.1101/2020.05.29.20117093 (2020).
Getachew, B., Liabsuetrakul, T. & Gebrehiwot, Y. Association of maternity waiting home utilization with women’s perceived geographic barriers and delivery complications in Ethiopia. Int. J. Health Plann. Manag. 35(1), e96–e107. https://doi.org/10.1002/hpm.2940 (2020).
Campbell, M. J., Julious, S. A. & Altman, D. G. Estimating sample sizes for binary, ordered categorical, and continuous outcomes in two group comparisons. BMJ 311(7013), 1145. https://doi.org/10.1136/bmj.311.7013.1145 (1995).
Central Statistical Agency/CSA/Ethiopia and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF (2016).
Galle, A., Griffin, S., Osman, N., Roelens, K. & Degomme, O. Towards a global framework for assessing male involvement in maternal health: Results of an international delphi study. BMJ Open https://doi.org/10.1136/bmjopen-2021-051361 (2021).
Vermeiden, T. et al. Factors associated with intended use of a maternity waiting home in Southern Ethiopia: A community-based cross-sectional study. BMC Pregnancy Childbirth. 18(1), 1–9. https://doi.org/10.1186/s12884-018-1670-z (2018).
Dereje, S., Yenus, H., Amare, G. & Amare, T. Maternity waiting homes utilization and associated factors among childbearing women in rural settings of Finfinnee special zone, central Ethiopia: a community based cross-sectional study. PLoS ONE 17, 1–12. https://doi.org/10.1371/journal.pone.0265182 (2022).
Tenaw Z, Fikre R, Gemeda H, Astatkie A. Determinants of maternity waiting home utilization in Sidama Zone, Southern Ethiopia: a cross-sectional study. PLoS One. 2022;17(3 March):3–11. doi:https://doi.org/10.1371/journal.pone.0264416
Yismaw, W. et al. Intention to use maternal waiting homes and related factors among pregnant women in Metu Woreda. Western Ethiopia. Ethiop J Health Sci. 32(5), 875–884. https://doi.org/10.4314/ejhs.v32i5.2 (2022).
Endayehu, M., Yitayal, M. & Debie, A. Intentions to use maternity waiting homes and associated factors in Northwest Ethiopia. BMC Pregnancy Childbirth. 20(1), 1–10. https://doi.org/10.1186/s12884-020-02982-0 (2020).
Anagaw, T. F., Debela, Y., Asresie, M. B., Wasihun, Y. & Bogale, E. K. Maternity waiting home use and associated factors among mothers in Northwest Ethiopia: The application of the integrated behavioral model. Ethiop. J. Health Dev. https://doi.org/10.20372/ejhd.v36i2.5183 (2022).
Shiferaw, M. M., Tiguh, A. E., Kebede, A. A. & Taye, B. T. Utilization of maternal waiting home and associated factors among women who gave birth in the last one year, Dabat district, Northwest Ethiopia. PLoS ONE 17, 1–14. https://doi.org/10.1371/journal.pone.0271113 (2022).
Penn-Kekana, L. et al. Understanding the implementation of maternity waiting homes in low- and middle-income countries: A qualitative thematic synthesis. BMC Pregnancy Childbirth. 17(1), 1–12. https://doi.org/10.1186/s12884-017-1444-z (2017).
Aden, M., Azale, T. & Tadie, C. Intention to use and predictors of use of maternity waiting home among pregnant women in Hargeisa City Health Centers, Somaliland. Patient Prefer Adherence. 16(June), 1595–1603. https://doi.org/10.2147/PPA.S358952 (2022).
Acknowledgements
We thank Jimma University, Institute of Health, for the ethical approval and financial support. Second, we thank the staff of the Hadiya Zone Health Department and all the study participants for their cooperation. Third, we thank Mizan Tepi University Teaching Hospital for giving us a vehicle (Land Cruiser Pickup) for this study, without which data collection could have been difficult. Finally, we thank our driver, Mintesinot Shimelis Mekuria, for his great commitment and best driving skills throughout the rural areas, which was adventurous.
Funding
This study was partially financed by Jimma University. However, Jimma University had no role in the design, data collection, data analysis or dissemination of the study findings.
Author information
Authors and Affiliations
Contributions
T.Y., H.G., and T.B. conceived the study and designed the methodology. T.Y. supervised the data collection, entered the data, performed the data analysis, and prepared the draft manuscript. H.G., M.H., and T.B. critically reviewed and provided comments on the draft manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yarinbab, T.E., Gesesew, H.A., Harrison, M.S. et al. Factors associated with knowledge and attitude towards maternity waiting homes among pregnant women: baseline results from a cluster-randomized trial in rural Ethiopia. Sci Rep 13, 11854 (2023). https://doi.org/10.1038/s41598-023-39029-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-39029-1
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.