Abstract
To compare the performance of SARC-F and SARC-CalF as screening tools for sarcopenia. Cross-sectional study with a convenience sample of 312 community-dwelling older people. Sarcopenia was defined as low handgrip strength (HGS) or low gait speed (GS ≤ 0.8 m/s). HGS was measured by dynamometry and GS by the 4-m walking speed test. For HGS, six criteria (C) were used to identify sarcopenia in men/women: CI: < 27 kg/16 kg; CII: < 35.5 kg/20.0 kg; CIII: grip over body mass index < 1.05/< 0.79; CIV: grip strength over total body fat < 1.66/< 0.65; CV: grip over bodyweight < 0.45/< 0.34; CVI: < 27 kg/16 kg and low skeletal muscle mass index (SMMI); CI and CVI defined according to the European Working Group on sarcopenia in older people and the rest according to the sarcopenia definition and outcomes Consortium. For sarcopenia screening, the SARC-F (≥ 4 points) and the SARC-CalF (≥ 11 points) were used. The kappa analysis revealed no agreement between the SARC-F and the various criteria for the identification of sarcopenia in men. The same lack of agreement was observed in women with some exceptions: CI = 0.161 ± 0.074, p = 0.020; GS = 0.209 ± 0.076, p = 0.003. Concerning the Cohen’s kappa between the SARC-Calf and the reference criteria of sarcopenia, the following coefficients were observed as significant for women: CI = 0.201 ± 0.069, p = 0.003; CII = 0.186 ± 0.064, p = 0.005; GS = 0.273 ± 0.068, p = 0.0001; and for men: CII = 0.139 ± 0.053, p = 0.021; GS = 0.223 ± 0.099, p = 0.011. ROC curves revealed the SARC-Calf with acceptable discrimination and reasonable sarcopenia predictive capacity considering a cutoff value of 10.5 in both men (AUC: 67.5%, p = 0.022; Se = 52.9%; Sp = 76.8%) and women (AUC: 72.4%, p < 0.001; Se = 63%; Sp = 68.5%) concerning GS. The SARC-CalF performed better than the SARC-F for screening sarcopenia in the population ≥ 60 years of age in the Amazonas, measured through walking slowness.
Similar content being viewed by others
Introduction
The life expectancy of the human population has been increasing worldwide, which is to be welcomed. However, this increase may not correspond to a more significant number of years of healthy life as aging is the expression of a continuous biological process associated with a decrease in the function of different bodily systems1,2,3. The loss of skeletal muscle mass and muscle function (strength and performance) with aging or from other secondary causes characterizes sarcopenia, a disease established by the International Classification of Diseases-10 code in 20164,5. Sarcopenia is associated with an increased risk of falls, fractures, physical disability, higher morbidity, and death5,6. These associations reveal the need for help and treatment services for older adults with sarcopenia in a community, institutional, or hospital context and the associated costs7. Sarcopenia can be prevented and reversed8,9. However, simple approaches capable of discriminating against suspected cases of sarcopenia are needed10.
In 2010 the European Working Group on Sarcopenia in Older People (EWGSOP) proposed an approach to diagnosing sarcopenia that combined low muscle mass with low strength or low physical performance7. The diagnosis was recently updated by the same group (EWGSOP2), evolving into an evaluation of sarcopenia in three steps: identification (low strength), confirmation (low muscle mass), and degree of severity (low physical performance), preceded by a screening questionnaire11,12. In 2020, another working group, the Sarcopenia Definition and Outcomes Consortium (SDOC), emphasizes muscle strength and physical performance for the diagnosis of sarcopenia but does not recommend the assessment of muscle mass for the diagnosis of sarcopenia because muscle mass (assessed by dual-energy x-ray absorptiometry or by bioimpedance) does not seem to be a predictor of the risk of functional disability13,14. Screening for sarcopenia, based on symptomatology and the occurrence of events is, however, the first step in assessing sarcopenia suggested by both approaches15,16. This process precedes the objective assessment in case of suspicion. To this end, the SARC-F questionnaire is the most popular.
The SARC-F questionnaire has been validated for different languages9,10,15,17,18,19 and clinical settings9,15,17,20,21 using several gold standard diagnostic modalities as a reference22,23. SARC-F is a simple, easy-to-use, 5-item sarcopenia screening questionnaire8, where five domains are included in the questionnaire: (1) Strength, (2) Assistance with walking, (3) Rising from a chair, (4) Climbing stairs, and (5) Falls24. Since 2018, SARC-F has been part of the sarcopenia diagnostic algorithm proposed by the European Working Group on Sarcopenia in Older Adults 2 (EWGSOP2)25.
However, the performance of the SARC-F for screening sarcopenia has been shown to be highly variable26, with the sensitivity for suspected cases of sarcopenia ranging from 3.9 to 95.4%27. The high variability, with poor to fair diagnostic accuracy, and greater specificity than sensitivity19,22,23,24,26,28 constitutes a limitation to correctly identifying positive cases of sarcopenia29. It is postulated that the low sensitivity of SARC-F for the suspicion of sarcopenia is because it does not require information on any muscle mass marker13,30,31. In light of this assumption, two modified versions of the SARC-F emerged with the inclusion of other markers, a more specific marker such as CalF circumference (SARC-CalF), but also less specific markers such as age and body mass index (SARC-F + EBM)24.
To identify sarcopenia symptoms the SARC-F, and SARC-CALF are instruments widely validated worldwide32. However, when compared with each other, the SARC-CalF demonstrated greater sensitivity (66.7% vs. 33.3%), high discrimination (AUC: 0.736 vs. AUC: 0.592), and a similar specificity (82.9% vs. 84.2%)24. Based on data the SARC-F can better classify non-sarcopenic than sarcopenic older adult populations33. Additionally, CalF circumference measurements (SARC-CalF) showed that this specific variable improves the screening for sarcopenia16,29,34,35. by increasing its sensitivity relative to SARC-F36,37.
However, it is necessary to analyze the performance of sarcopenia screening instruments regarding the various objective criteria for assessing muscle function (strength and performance) proposed by the different working groups. Thus, the present study aimed to compare the performance of SARC-F and SARC-CalF as approaches for the screening of sarcopenia using the criteria proposed by the EWGSOP2 and the SDOC as a reference for the diagnosis of sarcopenia in older adults from the state of Amazonas, Brazil13.
Methods
Design and study population
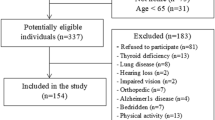
This work is based on a cross-sectional study with a convenience sample involving 312 community-dwelling older adults (64% women) living in the urban area of the city of Novo Aripuanã (Amazonas), Northern Brazil. Older adults living in rural areas were excluded from the research due to difficulty accessing the evaluation site (distance and necessary means of transport) (Fig. 1). The sample size was calculated using GPower (Heinrich-Heine-University, Düsseldorf, Germany; software 3.1.9.7)38. Calculations were based on direct logistic regression, family of z tests, considering an odds ratio of 1.5 and α = 0.05, and a computational power of 0.95. The following criteria were considered for the inclusion of participants: (a) older adults aged 60 or over living in the urban area of the city; (b) be independent in carrying out activities of daily living; (c) moderate or high level of cognitive functioning; (d) without chest pain and/or angina pectoris and limiting joint pain39. The Mini-Mental State Examination (MMSE) evaluated the cognitive criteria selection40. An MMSE ≤ 15/30 points were used to exclude the participants of study40. Before the data collection process, all procedures and potential risks were explained and informed consent forms were signed by all participants. This study was conducted in accordance with the Declaration of Helsinki41. After selecting the participants, the following evaluations were performed: sociodemographic, anthropometric, muscle function (strength and performance) and sarcopenia symptoms.
This study was approved by the Ethics Committee of the State UEA and the study was carried out in accordance with the Declaration of Helsinki and Resolution 466/12 of the National Health Council, making part of the research project: “Sarcopenic Syndrome-Physical Function, Phenotype and Quality of Life” (CAAE 74055517.9.0000.5016/Referee 2.281.400).
Sociodemography
The questionnaire from the Brazilian Association of Research Companies was used to assess the sociodemographic variables42. The questionnaire classifies individuals into five social classes, ranging from class A (those with higher purchasing power) to class E (those with lower purchasing power) based on ownership of some consumer goods, head's schooling family, and access to public services.
Anthropometric and body composition characteristics
Body height and body mass were determined using a mechanical scale with the stadiometer attached, with the older adults barefoot and wearing light clothing. The categorization of body mass index (BMI) followed the guidelines of the World Health Organization28. The CalF circumference is a marker of muscle mass and was measured with an inelastic metallic tape measure, the measurement was taken at the point of the greatest circumference with the individual seated, with the leg forming a 90° angle and feet flat on the ground30 without compressing subcutaneous tissues and was used to calculate the SARC-CalF. Skeletal muscle mass (SMM) was estimated according to Lee and colleagues43 using the corrected arm, thigh, and CalF circumferences and normalized for body height (SMMI, kg/m2). To identify participants with low SMMI, the cutoff values proposed by Walowski and colleagues were used44. The cutoff values align with those recommended by the EWGSOP (-2 SD below the healthy young adult population) but are adjusted for the BMI.
Sarcopenia identification-muscle function (strength and performance)
For the identification of sarcopenia, muscle function, namely handgrip strength and performance (gait speed), were considered according to the criteria of the EWGSOP2 and SDOC13,25. Handgrip strength was measured using a digital hand dynamometer (Camry EH10; Sensun Weighing Apparatus Group Ltd., Guangdong, China)45 following the procedures recommended by Roberts and colleagues31. The assessment was performed sitting with the elbow flexed at 90 degrees. Both the left and right arms were measured twice. Two measurements were performed for each hand alternately, and the highest value found among the four measures was used. The results were recorded in kilograms (kg). For the diagnosis of sarcopenia through the handgrip strength, six criteria were considered, the first and the sixth criteria according to the EWGSOP225 (I) < 27 kg in men and < 16 kg in women, (VI) < 27 kg in men and < 16 kg in women and low SMMI; and the remaining criteria according to SDOC13: (II) < 35.5 kg in men and < 20.0 kg in women; (III) grip over body mass index < 1.05 for men and 0.79 for women; (IV) grip strength over total body fat < 1.66 for men and < 0.65 for women; (V) grip over body weight < 0.45 for men and < 0.34 for women. The usual walking speed (criterion VII) was evaluated at a 4 m distance15. The test was performed twice, adopting the best execution time. Values below 0.8 m/s, regardless of sex, were considered indicative of decreased physical performance because it is the most consensual cutoff value by the various sarcopenia working groups, except for the International Working Group on Sarcopenia (IWGS: < 1.0 m/s)13,15,46,47.
Sarcopenia suspicion-symptoms
The signalling of possible cases of sarcopenia was performed through SARC-F and SARC-CalF. The SARC-F is a 5-item questionnaire that asks about difficulties in strength, walking, getting up from a chair, climbing stairs, and history of falls. A score ≥ 4 points on the SARC-F is suggestive of sarcopenia48. For this purpose, the translated and validated version of the SARC-F for the Brazilian population was used29. The SARC-CalF consists of the SARC-F complemented with a measurement of CalF circumference. The SARC-CalF score ranges from 0 to 20 points, with a score ≥ 11 points suggestive of sarcopenia29: men and women with CalF circumference < 34 cm and < 33 cm, respectively (suggestive of low muscle mass) receive a 10-point increase from the original SARC-F score.
Statistical analysis
All statistical analyses were performed using SPSS version 26.0 for Windows software (SPSS, Chicago, IL, USA). Data were stratified by sex and described as the absolute and relative frequency of cases (n, %) and mean + standard deviation (SD). The Chi-Square Test, the Mann–Whitney test, and Fisher’s exact test were used to compare continuous and nominal characteristics of the sample between the sexes, respectively. Data normality was verified with the Kolmogorov–Smirnov. The accuracy of the screening tools (SARC-F and SARC-CalF) was evaluated through K analysis and the area under the curve (AUC), sensitivity (Se), specificity (Sp), positive predictive value (PPV), and negative predictive value (NPV) analysis. The significance level was set at p ≤ 0.05.
Results
The sociodemographic and anthropometric characteristics, the sarcopenia symptoms, and markers of sarcopenia (muscle strength and performance) of the sample are described in Table 1. Our sample was predominantly female, aged > 70 yrs, non-literate, and of socioeconomic class D/E. Most participants were overweight (42.0%) and obese (21.2%). No sex differences were observed for sarcopenia symptoms, assessed using the SARC-F and SARC-CalF, despite differences in CalF circumference, muscle strength, and performance, with men showing better results than women in these variables.
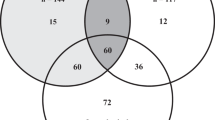
The prevalence of sarcopenia assessed through symptoms and muscle function are described in Tables 2 and 3. Sarcopenia was suspected in 12.5% of men and 21% of women when evaluated by the SARC-F (Table 2) and in 27.7% of men and e 40% of women when evaluated by SARC-CalF (Table 3). Regarding the cross-classification analysis between sarcopenia symptoms and muscle function, the kappa analysis revealed no agreement between the SARC-F and the various criteria of handgrip strength (CI–VI) and gait speed (CVII) for the identification of sarcopenia in men (Table 2): KI = 0.139 ± 0.090, p = 0.087; KII = 0.039 ± 0.034, p = 0.322; KIII = − 0.021 ± 0.072, p = 0.770; KIV = − 0.049 ± 0.082, p = 0.590; KV = 0.036 ± 0.062, p = 0.568; KVI = − 0.014 ± 0.029, p = 0.548; KVII = 0.065 ± 0.105, p = 0.486. The same lack of agreement was observed in women except for handgrip strength CI and gait speed CVII: KI = 0.161 ± 0.074, p = 0.020; KII = 0.067 ± 0.051, p = 0.200; KIII = 0.038 ± 0.045, p = 0.403; KIV = − 0.101 ± 0.063, p = 0.146; KV = 0.079 ± 0.052, p = 0.135; KVI = − 0.004 ± 0.030, p = 0.892; KVII = 0.209 ± 0.076, p = 0.003.
Concerning the kappa analysis between the SARC-CalF and the different criteria of handgrip strength and gait speed for the identification of sarcopenia, there were more agreements (Table 3). In women, agreement of SARC-CalF with handgrip strength criteria CI and CII and with the gait speed criterion CVII was observed with the following K coefficients: KI = 0.201 ± 0.069, p = 0.003; KII = 0.186 ± 0.064, p = 0.005; KIII = − 0.034 ± 0.062, p = 0.583; KIV = − 0.031 ± 0.068, p = 0.653; KV = − 0.101 ± 0.067, p = 0.130; KVI = − 0.009 ± 0.040, p = 0.815, KVII = 0.273 ± 0.068, p = 0.0001. In men, it was found concordance of SARC-CalF with the handgrip criterion CII and with the gait speed criterion CVII: KI = 0.155 ± 0.098, p = 0.099; KII = 0.139 ± 0.053, p = 0.021; KIII = − 0.032 ± 0.092, p = 0.722; KIV = − 0.053 ± 0.088, p = 0.563; KV = 0.018 ± 0.085, p = 0.833; KVI = − 0.047 ± 0.37, p = 0.183; KVII = 0.223 ± 0.099, p = 0.011. Since K values below 0.2 are considered poor, we highlight the agreement between SARC-CalF and gait speed criterion CVI in both sexes.
AUC, sensitivity, specificity, and positive and negative predictive values of SARC-F and SARC-CalF for sarcopenia screening according to different criteria of muscle function (handgrip strength and gait speed), are presented in Tables 4 and 5, respectively. The SARC-F did not reveal any ability to discriminate sarcopenia in men, regardless of the muscle function variable (muscle strength or gait speed) taken as a reference. In women, the SARC-F showed a poor discrimination ability with AUC values of 0.665 for criterion CI, 0.651 for CII, and 0.660 for CVII. When SARC-CalF was used to screen for sarcopenia in women, the corresponding AUC for the same reference criteria were 0.631 for CI, 0.641 for CII, and 0.724 for CVII. The SARC-CalF, in turn, was able to discriminate sarcopenia in men using the criteria CII (AUC: 0.676) and CVII (AUC: 0.675) as references. Generally, an AUC > 0.9 indicates exceptional discrimination, 0.7‒0.9 indicates moderate discrimination, 0.5‒0.7 indicates poor discrimination, and < 0.5 indicates result at chance49. In the significant models, the predictive power was reasonable, with the specificity consistently higher than the sensitivity and consequently higher values of NPV than PPV. Greater sensitivity for suspected sarcopenia was observed with the SARC-CalF in women with gait speed criterion CVII (Se = 63.0) and men with handgrip criterion CII (Se = 60.7) as references; the cutoff for these criteria was 10.5 pts and 4.5 pts, respectively.
Discussion
This study aimed to compare SARC-F and SARC-CalF tests as approaches for screening sarcopenia in older people. This is the first study examining these questionnaires in populations with specific characteristics, such as older adults from Amazonas. These are inexpensive, easy to administer, and minimally invasive approaches that assess the symptoms of sarcopenia (SARC-F) complemented by the CalF circumference as a possible indicator of muscle mass (SARC-CalF)10. This type of analysis is essential because there still needs to be a consensus on evaluating sarcopenia, including screening, among the different working groups dedicated to this subject7,50,51,52,53,54.
A greater suspicion of sarcopenia was observed when screening was performed with SARC-CalF: sarcopenia was detected by SARC-CalF in 27.7% of men and 40.0% of women, and SARC-F in 12.5% of men and 21.0% of women. Taking handgrip strength and gait speed as references, the prevalence of sarcopenia ranged between 15.2 and 75.0% for men and 27% and 66% for women, with the lowest prevalence associated with gait speed and the highest prevalence with handgrip in both sexes. From the analyzes carried out on the agreement between the measures for the suspicion (symptoms) and the identification (muscle function) of sarcopenia, a poor to fair diagnostic accuracy was observed in both sexes when the screening instrument was the SARC-CalF (AUC: 0.631–0.724, p < 0.01).
The SARC-F did not show any ability to discriminate against sarcopenia in men. The predictive ability of SARC-CalF was reasonable with sensitivity and specificity values above 50%, considering a cutoff value of 10.5 in both men and women when gait speed CVII was the reference criteria for muscle function. As in most studies on the ability to predict sarcopenia from SARC-F or SARC-CalF, specificity was superior to sensitivity, meaning there were few false negative results than false positive results9,15,18,24. Low sensitivity implies that many subjects with sarcopenia will not be detected if assessed using these questionnaires. Specificity relates to the test’s ability to reject subjects without a condition correctly. Therefore, if not detected from SARC-F or SARC-CalF, sarcopenia can be ruled out without further evaluation24.
The use of different approaches in this study is due to the need for more consensus regarding the most appropriate methodologies for screening and identifying sarcopenia46. In 2016, Barbosa-Silva and colleagues proposed the SARC-F + CC (or SARC- CalF score), a modified version of the SARC-F, to improve its performance34. The SARC-CalF adds an anthropometric marker (CalF circumference) to the muscle functionality markers present in the original SARC-F20,34,35,55,56. CalF circumference assessment is a simple procedure of measuring the widest part of the right CalF with a non-elastic flexible plastic tape24. In older populations, the CalF circumference is measured as the most sensitive anthropometric index of muscle mass57.
The results of this investigation are similar to the findings demonstrated in previous studies, namely (a) a greater suspicion (screening) of sarcopenia in women than in men, and no differences in the objective identification of sarcopenia (assessment) were identified16,21,58,59; (b) a higher number of cases who suspected sarcopenia, with SARC-CalF than with SARC-F11,24; (c) a better diagnostic accuracy of sarcopenia of SARC-CalF compared to SARC-F having the EWGSOP2 as the gold standard35,58,60; (d) screening instruments showed higher specificity than sensitivity11,35,56,58,60,61,62. Age is a factor that favours the development of sarcopenia since the prevalence of symptoms is higher in older people34,63,64. In addition to age, sex also seems to be a determinant for the differences in the prevalence of sarcopenia observed in older adults: a lower muscle mass and lower use of muscle during the aging process (less physical activity) are likely explanations65,66,67.
This study has several limitations, namely the sample's representativeness (age group, sex, socio-economic status, residential area). For example, most participants were women, and sex plays an essential role in sarcopenia68,69. On the other hand, we limited our cross-sectional study to a comparison of SARC-F and SARC-CalF; a comparison between different sarcopenia screening approaches to predict important health outcomes such as disability, frailty, quality of life, and mortality should be investigated in prospective studies in the future. As strengths of this work, we highlight the investigation with a peculiar and little-studied sample whose participants live in poor cities with difficult access in Brazil, where screening is even more critical for health promotion and facilitation of clinical practice. However, this is the first study that compares the diagnosis of the two main sarcopenia screening instruments in the elderly population of Amazonas, including cutoff points for (not) suspected sarcopenia (SARC-Calf = 10.5 pts). Despite the promising results found in this study, its validity will need to be confirmed in further studies.
Conclusion
Using walking slowness (≤ 8 m/s) as a reference method for identifying sarcopenia, the SARC-CalF performed better than the SARC-F for screening sarcopenia in the population ≥ 60 years of age in Amazonas, Brazil. Further studies are needed to verify this finding in other population groups and, above all, continue research to improve the performance of screening instruments.
Data availability
The data presented in this study are available upon request from the corresponding author. The data are not publicly available as they belong to a Ph.D. thesis in progress.
References
Moskalev, A. et al. Genetics and epigenetics of aging and longevity. Cell Cycle 13, 1063–1077 (2014).
Robine, J.-M. Ageing Populations: We are Living Longer Lives, But are we Healthier (United Nations, Department of Economics and Social Affairs, Population Division, 2021).
Lu, J.-L. et al. Screening accuracy of SARC-F for sarcopenia in the elderly: A diagnostic meta-analysis. J. Nutr. Health Aging 25, 172–182 (2021).
Anker, S. D., Morley, J. E. & von Haehling, S. Welcome to the ICD-10 code for sarcopenia. J. Cachexia Sarcopenia Muscle 7, 512–514. https://doi.org/10.1002/jcsm.12147 (2016).
Morley, J. E. Frailty and sarcopenia: The new geriatric giants. Rev. Invest. Clin. 68, 59–67 (2016).
Piotrowicz, K. et al. SARC-F as a case-finding tool for sarcopenia according to the EWGSOP2. National validation and comparison with other diagnostic standards. Aging Clin. Exp. Res. 33, 1821–1829 (2021).
Cruz-Jentoft, A. J. et al. Sarcopenia: European consensus on definition and diagnosis report of the European Working Group on sarcopenia in older people. Age Ageing 39, 412–423 (2010).
Malmstrom, T. K. & Morley, J. E. SARC-F: A simple questionnaire to rapidly diagnose sarcopenia. J. Am. Med. Dir. Assoc. 14, 531–532 (2013).
Bahat, G. et al. Performance of SARC-F in regard to sarcopenia definitions, muscle mass and functional measures. J. Nutr. Health Aging 22, 898–903 (2018).
Sánchez-Rodríguez, D. et al. Translation and validation of the Spanish version of the SARC-F questionnaire to assess sarcopenia in older people. J. Nutr. Health Aging 23, 518–524 (2019).
da Luz, M. C. L. et al. SARC-F and SARC-CalF in screening for sarcopenia in older adults with Parkinson’s disease. Exp. Gerontol. 144, 111183 (2021).
Hajaoui, M. et al. Sarcopenia: Performance of the SARC-F questionnaire according to the european consensus criteria, EWGSOP1 and EWGSOP2. J. Am. Med. Dir. Assoc. 20, 1182–1183. https://doi.org/10.1016/j.jamda.2019.05.021 (2019).
Bhasin, S. et al. Sarcopenia definition: The position statements of the sarcopenia definition and outcomes consortium. J. Am. Geriatr. Soc. 68, 1410–1418. https://doi.org/10.1111/jgs.16372 (2020).
Cawthon, P. M. et al. Strong relation between muscle mass determined by D3-creatine dilution, physical performance, and incidence of falls and mobility limitations in a prospective cohort of older men. J. Gerontol. Ser. A 74, 844–852 (2019).
Parra-Rodriguez, L. et al. Cross-cultural adaptation and validation of the Spanish-language version of the SARC-F to assess sarcopenia in Mexican community-dwelling older adults. J. Am. Med. Dir. Assoc. 17, 1142–1146. https://doi.org/10.1016/j.jamda.2016.09.008 (2016).
Gasparik, A., Demián, M. & Pascanu, I. Romanian translation and validation of the SARC-F questionnaire. Acta Endocrinologica (Bucharest) 16, 216 (2020).
Urzi, F., Simunic, B. & Buzan, E. Basis for sarcopenia screening with the SARC-CalF in nursing homes. J. Am. Med. Dir. Assoc. 18, 991. https://doi.org/10.1016/j.jamda.2017.07.011 (2017).
Kim, S., Kim, M. & Won, C. W. Validation of the Korean version of the SARC-F questionnaire to assess sarcopenia: Korean frailty and aging cohort study. J. Am. Med. Dir. Assoc. 19(40–45), e41. https://doi.org/10.1016/j.jamda.2017.07.006 (2018).
Ida, S. et al. Development of a Japanese version of the SARC-F for diabetic patients: An examination of reliability and validity. Aging Clin. Exp. Res. 29, 935–942. https://doi.org/10.1007/s40520-016-0668-5 (2017).
Yang, M. et al. Comparison of four sarcopenia screening tools in nursing home residents. Aging Clin. Exp. Res. 31, 1481–1489. https://doi.org/10.1007/s40520-018-1083-x (2019).
Kera, T. et al. SARC-F: A validation study with community-dwelling older Japanese adults. Geriatr. Gerontol. Int. 19, 1172–1178 (2019).
Kim, M. & Won, C. W. Sarcopenia in Korean Community-Dwelling adults aged 70 years and older: Application of screening and diagnostic tools from the asian working group for sarcopenia 2019 update. J. Am. Med. Dir. Assoc. 21, 752–758. https://doi.org/10.1016/j.jamda.2020.03.018 (2020).
Ida, S. et al. Verification of the predictive validity for mortality of the SARC-F questionnaire based on a meta-analysis. Aging Clin. Exp. Res. 33, 835–842 (2021).
Krzyminska-Siemaszko, R. et al. Comparison of diagnostic performance of SARC-F and its two modified versions (SARC-CalF and SARC-F+EBM) in community-dwelling older adults from Poland. Clin. Interv. Aging 15, 583–594. https://doi.org/10.2147/CIA.S250508 (2020).
Cruz-Jentoft, A. J. et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 48, 16–31 (2019).
Ida, S., Kaneko, R. & Murata, K. SARC-F for screening of sarcopenia among older adults: A meta-analysis of screening test accuracy. J. Am. Med. Dir. Assoc. 19, 685–689 (2018).
Ha, Y.-C. et al. SARC-F as a useful tool for screening sarcopenia in elderly patients with hip fractures. J. Nutr. Health Aging 24, 78–82 (2020).
Initiative NOE, Heart N, Lung, et al. The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. The Institute (2002).
Barbosa-Silva, T. G. et al. Enhancing SARC-F: Improving sarcopenia screening in the clinical practice. J. Am. Med. Dir. Assoc. 17, 1136–1141. https://doi.org/10.1016/j.jamda.2016.08.004 (2016).
Esparza-Ros, F., Vaquero-Cristóbal, R. & Marfell-Jones, M. International Standards for Anthropometric Assessment (International Society for the Advancement of Kinanthropometry (ISAK), 2019).
Roberts, H. C. et al. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 40, 423–429 (2011).
Krzymińska-Siemaszko, R. et al. Comparison of diagnostic value of the SARC-F and its four modified versions in polish community-dwelling older adults. Clin. Interv. Aging 24, 783–797 (2023).
Lauretani, F. et al. Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J. Appl. Physiol. (1985) 95, 1851–1860. https://doi.org/10.1152/japplphysiol.00246.2003 (2003).
Barbosa-Silva, T. G. et al. Prevalence of sarcopenia among community-dwelling elderly of a medium-sized South American city: Results of the COMO VAI? study. J. Cachexia Sarcopenia Muscle 7, 136–143. https://doi.org/10.1002/jcsm.12049 (2016).
Yang, M. et al. Screening Sarcopenia in community-dwelling older adults: SARC-F vs SARC-F combined with calf circumference (SARC-CalF). J. Am. Med. Dir. Assoc. 19, 277. https://doi.org/10.1016/j.jamda.2017.12.016 (2018).
Ito, A. et al. Changes in the screening efficacy of lower calf circumference, SARC-F score, and SARC-CalF score following update from AWGS 2014 to 2019 sarcopenia diagnostic criteria in community-dwelling older adults. J. Phys. Ther. Sci. 33, 241–245 (2021).
Kandinata, S. G. et al. Diagnostic performance of calf circumference, SARC-F, and SARC-CalF for possible sarcopenia screening in Indonesia. Sci. Rep. 13, 9824. https://doi.org/10.1038/s41598-023-36585-4 (2023).
Faul, F. et al. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191 (2007).
Rikli, R. E. & Jones, C. J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 53, 255–267. https://doi.org/10.1093/geront/gns071 (2013).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198 (1975).
Parsa-Parsi, R. W. The international code of medical ethics of the World medical Association. JAMA 328, 2018–2021 (2022).
Pesquisa-ABEP ABdEd. Critério de classificação econômica Brasil: critério Brasil. Associação Brasileira de Empresas de Pesquisa São Paulo (2019).
Lee, R. C. et al. Total-body skeletal muscle mass: Development and cross-validation of anthropometric prediction models. Am. J. Clin. Nutr. 72, 796–803 (2000).
Walowski, C. O. et al. Reference values for skeletal muscle mass–current concepts and methodological considerations. Nutrients 12, 755 (2020).
Huang, L. et al. Reliability and validity of two hand dynamometers when used by community-dwelling adults aged over 50 years. BMC Geriatr. 22, 1–8 (2022).
Chen, L.-K. et al. Recent advances in sarcopenia research in Asia: 2016 update from the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 17, 767 (2016).
Chumlea, W. C. et al. Sarcopenia: Designing phase IIb trials: International working group on sarcopenia. J. Nutr. Health Aging 15, 450 (2011).
Cao, L. et al. A pilot study of the SARC-F scale on screening sarcopenia and physical disability in the Chinese older people. J. Nutr. Health Aging 18, 277–283 (2014).
Mandrekar, J. N. Receiver operating characteristic curve in diagnostic test assessment. J. Thorac. Oncol. 5, 1315–1316 (2010).
Chen, L.-K. et al. Sarcopenia in Asia: Consensus report of the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 15, 95–101 (2014).
Fielding, R. A. et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J. Am. Med. Dir. Assoc. 12, 249–256 (2011).
Studenski, S. A. et al. The FNIH sarcopenia project: Rationale, study description, conference recommendations, and final estimates. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 69, 547–558 (2014).
Morley, J. E. et al. Sarcopenia with limited mobility: An international consensus. J. Am. Med. Dir. Assoc. 12, 403–409 (2011).
Muscaritoli, M. et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: Joint document elaborated by Special Interest Groups (SIG)“cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin. Nutr. 29, 154–159 (2010).
Bauer, J. et al. Sarcopenia: A time for action. An SCWD position paper. J. Cachexia Sarcopenia Muscle 10, 956–961. https://doi.org/10.1002/jcsm.12483 (2019).
Bahat, G. et al. Comparing SARC-F with SARC-CalF to screen sarcopenia in community living older adults. J. Nutr. Health Aging 22, 1034–1038. https://doi.org/10.1007/s12603-018-1072-y (2018).
Organization, W. H. Physical Status: The Use of and Interpretation of Anthropometry (World Health Organization, 1995).
Krzyminska-Siemaszko, R. et al. Comparison of four sarcopenia screening questionnaires in community-dwelling older adults from Poland using six sets of international diagnostic criteria of sarcopenia. PLoS ONE 15, e0231847. https://doi.org/10.1371/journal.pone.0231847 (2020).
Gade, J. et al. Validation of the Danish SARC-F in hospitalized, geriatric medical patients. J. Nutr. Health Aging 24, 1120–1127 (2020).
Bahat, G., Erdoğan, T. & İlhan, B. SARC-F and other screening tests for sarcopenia. Curr. Opin. Clin. Nutr. Metab. Care 25, 37–42 (2022).
Drey, M. et al. German version of SARC-F: Translation, adaption, and validation. J. Am. Med. Dir. Assoc. 21(747–751), e741 (2020).
Rossi, A. P. et al. Sarcopenia risk evaluation in a sample of hospitalized elderly men and women: combined use of the mini sarcopenia risk assessment (MSRA) and the SARC-F. Nutrients 13, 635 (2021).
Hashemi, R. et al. Sarcopenia and its associated factors in Iranian older individuals: Results of SARIR study. Arch. Gerontol. Geriatr. 66, 18–22 (2016).
Spira, D. et al. Prevalence and definition of sarcopenia in community dwelling older people. Z. Gerontol. Geriatr. 49, 94–99 (2016).
Mijnarends, D. M. et al. Physical activity and incidence of sarcopenia: The population-based AGES—Reykjavik study. Age Ageing 45, 614–620 (2016).
da Silva, A. T. et al. Prevalence and associated factors of sarcopenia among elderly in Brazil: Findings from the SABE study. J. Nutr. Health Aging 18, 284–290 (2014).
Bijlsma, A. et al. Defining sarcopenia: The impact of different diagnostic criteria on the prevalence of sarcopenia in a large middle aged cohort. Age 35, 871–881 (2013).
Du, Y. et al. Sex differences in the prevalence and adverse outcomes of sarcopenia and sarcopenic obesity in community dwelling elderly in East China using the AWGS criteria. BMC Endocr. Disord. 19, 1–11 (2019).
Hwang, J. & Park, S. Gender-specific risk factors and prevalence for sarcopenia among community-dwelling young-old adults. Int. J. Environ. Res. Public Health 19, 7232 (2022).
Funding
F.B. was partly supported by the Fundação para a Ciência e Tecnologia, under Grant UIDB/00447/2020 to CIPER—Centro Interdisciplinar para o Estudo da Performance Humana (unit 447). E.R.G. acknowledges support from LARSyS—Fundação para a Ciência e Tecnologia (FCT) pluriannual funding 2020–2023 (Reference: UIDB/50009/2020).
Author information
Authors and Affiliations
Contributions
Conceptualization, A.B.L. and F.B.; methodology, A.B.L. and D.H.N.; software, D.H.N.; validation, E.R.G. and F.B.; formal analysis, D.H.N and G.S.R.; investigation, A.B.L.; resources, A.B.L. and F.B.; data curation, F.B.; writing-original draft preparation, A.B.L. and D.H.N.; writing—review and editing, F.B., E.R.G., and G.S.R.; visualization, F.B., and E.R.G.; supervision, F.B. and E.R.G; project administration, A.B.L.; funding acquisition, A.B.L. and F.B. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barreto de Lima, A., dos Santos Ribeiro, G., Henriques-Neto, D. et al. Diagnostic performance of SARC-F and SARC-CalF in screening for sarcopenia in older adults in Northern Brazil. Sci Rep 13, 11698 (2023). https://doi.org/10.1038/s41598-023-39002-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-39002-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.