Abstract
Human epidermal growth factor receptor 2 (HER2/ERBB2) factor is known to be implicated in many malignancies and the potential of it as a prognostic biomarker was reported years ago. Molecular subtypes of HER2/ERBB2 negative and positive with distinct clinical outcomes have been identified in recent years; however, it is still under investigation for bladder cancer. This study evaluates the biological and prognostic significance of RAD21, RAD50 and BARD1 (homologous recombination biomarkers) mRNA levels with ERBB2 low and high expression to explore their impact on bladder cancer patient survival and cancer aggressiveness. The expression of ERBB2, RAD21, RAD50 and BARD1 mRNA levels was assessed in The Cancer Genome Atlas (TCGA) bladder cancer dataset along with four validation cohorts. Outcome analysis was evaluated using disease-free survival (DFS) and overall survival (OS). Univariate and multivariate analysis were used to evaluate the relationship between RAD21, RAD50, BARD1 and ERBB2 expression and clinicopathological variables. A significant increase in mRNA expression levels of RAD21, RAD50 and BARD1 was noticed in ERBB2-low patients compared to ERBB2-high patients. This overexpression of the homologous recombination repair transcripts was associated with poor outcome in ERBB2-low tumors, not in ERBB2-high tumors. Furthermore, the combined expression of high RAD21/RAD50, high RAD21/BARD1 or high RAD50/BARD1 were significantly associated with worse DFS and a better outcome for those with low co-expression in the ERBB2-low cohort. High expression of either RAD21/RAD50 or RAD21/BARD1 in ERBB2-low cohort associated with higher chance of metastasis. In addition, gene expression of BARD1 alone or in combination with RAD50 acted as an independent prognostic factor for worst survival. The data presented in this study reveal a connection between RAD21, RAD50, BARD1 and ERBB2 and patient survival. Importantly, it provided novel findings and potential prognostic markers, particularly in ERBB2-low bladder cancer.
Similar content being viewed by others
Introduction
Bladder cancer, is the 10th most common type of cancer globally, with an estimated 600,000 diagnosed cases and over 200,000 deaths annually according to the latest GLOBOCAN report1. It remains as one of the most challenging cancers to diagnose, as diagnosis is mainly confirmed through an invasive procedure called cystoscopy2,3. Bladder cancer can be clinically stratified into a three-stage spectrum; non-muscle invasive bladder cancer (NMIBC), where the disease is affecting the inner layer of the bladder. Then, muscle-invasive bladder cancer (MIBC), where the bladder muscle tissue is affected as well. Finally, at the end of the spectrum is metastatic, which happens when the disease spread to the adjacent lymph nodes and other organs. Treatment for bladder cancer include surgery, radiation, chemotherapy, immunotherapy and targeted therapy4. Deciding on the best treatment course relay heavily on the clinical spectrum in which the case lies on, in addition to the associated molecular characteristics. One tool to characterize cancer cases is through biomarkers. A set of bladder cancer associated biomarkers are being investigated and assigned to different prognostic outcomes. These markers can be used to indicate disease metastasis or recurrence, as well as response to certain treatment5.
Human epidermal growth factor receptor 2 (HER2/ERBB2) is a member of the epithelial growth factor receptor family, a group of transmembrane receptor tyrosine kinases. This family of receptors play a role in cell proliferation, survival and mobility6. The overexpression of HER2 is known to be implicated in a number of malignancies, including breast and gastroesophageal cancers where HER2 targeted drugs are currently approved7. For bladder cancer, HER2 is still under investigation as a diagnostic, prognostic and targeted therapy approach8. A growing body of literature is reporting on the association between HER2 overexpression in bladder cancer and poor prognosis and clinical outcomes, in addition to the possible benefits of HER2-targeted therapies9,10,11,12. However, there are also contradictory reports on this matter owing to several factors including tumor grade and heterogeneity, as well as study methodology and patient selection13,14,15. This instigates the importance of further assessing HER2/ERBB2 in the context of bladder cancer from different angles. This will allow for a better understanding of the over- and under-expression pattern, other linked biomarkers such as RAD21, RAD50 and BARD1, which are investigated in this study, and effective targeting mechanisms.
RAD21 is an essential gene that encodes a homologous recombination repair protein, this protein is a part of a multi-subunit cohesin complex (RAD21, SMC3, SMC1A and STAG1/2). Cohesin facilitates cohesion between replicated sister chromatids, plays a role in regulating gene expression and promotes accurate DNA repair through homologous recombination pathway. Just over a decade ago, cohesin mutations were found to be associated with cancer. Now, increasing evidence is showing that cohesin is in fact among the most commonly mutated protein complexes in cancers, including bladder cancer16,17,18,19. Of the four cohesin complex subunits; RAD21 is the most commonly overexpressed in cancers20. It was reported that RAD21 contributes to telomere maintenance, thus variants could lead to indefinite cell replication, which is a key characteristics in tumorigenicity21. RAD21 overexpression was implicated in different types of cancers including colorectal22, lung23, cervical24 ovarian25 prostate26 and breast cancer, where RAD21 overexpression was reported to confer poor prognosis and resistance to chemotherapy in HER2 mutant breast cancer patients27. It was also reported that RAD21 was overexpressed in bladder cancer tissues, it was proposed that RAD21 overexpression affected the RAD21 co-expressed cell cycle regulatory genes, which in turn affected cell cycle processes and contributed to tumorigenicity28.
RAD50 is a subunit of the MRN complex (MRE11/RAD50/NBS1), which plays a pivotal role in cellular response to DNA double-strand breakage by homologous recombination repair29. Defects in cellular responses to DNA damage instigate genome instability, which is a hallmark of cancer30. Mutations in the MRN complex, including RAD50 is implicated in tumorigenicity. For example, mutation in RAD50 was reported to be significantly associated with endometrioid endometrial carcinoma31. In breast cancer, RAD50 mutations is not associated with increased risk, but it is associated with shorten survival32. Low RAD50 expression was also associated with poor survival in colorectal mucinous adenocarcinoma patients33 and in postoperative early stage/low-grade rectal cancer patients, as low RAD50 expression was associated with perineural invasion34. In outcome of radiotherapy investigation, low MRN complex expression is associated with high histologic grade and estrogen receptor negativity. In addition to indication of poor radiotherapy efficiency in early breast cancer patients35. Whereas another study that examined RAD50 reported that upregulation of RAD50 had the strongest correlation with radioresistance in lung cancer patients36. For bladder cancer, the expression of the MRE11 subunit was reported to predict radio therapy outcomes, as high expression was associated with better survival37,38,39, although the role of RAD50 is yet to be elucidated.
Breast cancer 1 gene (BRCA1) is one of the most implicated genes in hereditary breast and ovarian cancers. The BARD1 gene is a BRCA1-associated RING domain 1 protein coding gene, which interacts with BRCA1 to repair damaged DNA40. Both of BARD1 and BRCA1 participates in homologous recombination repair pathway41. Therefore, mutations in BARD1 as well as BRCA1 will disrupt the BARD1-BRCA1 interaction, and therefore DNA damage repair. This instigates the importance of investigating BARD1 mutations, especially in BRCA1 mutation-negative cancers42. Furthermore, besides the BRCA1-dependant pathway, BARD1 was also found to play a role in tumor suppression via a BRCA1-independent pathways, such as the TP53-dependent pathway for apoptotic signaling43. Variants in the BARD1 gene were linked to breast cancer as well44,45,46. BARD1 variants were also linked to a number of non-breast, non-gynecological cancers47. For bladder cancer, there is not much literature on the matter. However, one recent study reported homologous recombination deficiency; one BARD1-deficient sample in three urothelial bladder tumor cohorts, compared to four BRCA2, three BRCA1 and two RBBP8-deficient samples48.
In the current study, we aimed to investigate the co-expression of RAD21, RAD50 and BARD1 mRNA levels in relation to ERBB2 low and high expression. This is done to explore their impact on bladder cancer patient survival and cancer aggressiveness. Then, in order to identify the relationship, overlapping genes and functional enrichment pathways between our homologous recombination targets and ERBB2 we constructed gene interaction network. Altogether, interpretation of the altered expression, prognostic and gene network relationship of our targets may reveal new insights into the prognostic knowledge of bladder cancer.
Materials and methods
Study cohorts and data analysis
In this retrospective study The Cancer Genome Atlas (TCGA) bladder cancer dataset was used as the main cohort along with four validation cohorts. Cohort one; TCGA datasets consist of 413 patients with MIBC and matched normal samples. Data were examined using UALCAN a publicly available interactive online portal (http://ualcan.path.uab.edu/index.html)49 and cBioPortal (https://www.cbioportal.org/) originally from Bladder Cancer (TCGA, Cell 2017). In this cohort, mRNA expression z-scores (RNA Seq V2 RSEM) were measured by Agilent microarray50,51,52. Cohort two; Memorial Sloan Kettering Cancer Center dataset (MSK, J Clin Onco 2013), this cohort consist of 97 high grade bladder urothelial carcinoma53. Cohort three; GSE31684 (Platform GPL570) from the Gene Expression Omnibus (GEO) database (https://www.ncbi.nlm.nih.gov/gds/). This cohort consist of 93 primary bladder cancer samples analyzed with Affymetrix Human Genome U133 Plus 2.0 Array. 68.82% of the patients in this cohort were over 65 years old and 31.18% where 65 year old or younger. Also, 73.12% where males vs. 26.88% female, with 93.55% of patients with high grade tumors and 6.45% with low grade. Tumor stages were as follow; 70.97% T4–T2 and 29.03% T1–Ta54,55. Cohort four; GSE48075 (Platform GPL6947) from GEO, consists of 142 primary bladder tumors (73 MIBC and 69 NMIBC) with tumor stages of 51.41% T4–T2 and 48.59% T1–Ta. Samples analyzed with Illumina HumanHT-12 V3.0 expression beadchip56,57. Cohort five; E-MTAB-4321 from ArrayExpress (https://www.ebi.ac.uk/biostudies/arrayexpress) which consists of 476 primarily early-stage urothelial carcinoma (460 NMIBC), samples analyzed by sequencing assay. 64.50% of the patients in this cohort were over 65 years old and 35.50% where 65 years old or younger. In addition, 77.10% of the whole cohort were male and 22.90% were female. Low grade tumors constituted 58.19% whereas high grade were 40.34%. Tumor stages of the whole cohort were as follow; 96.64% of patients Ta–T1 and 3.36% T2–T458.
The different expressions of RAD21, RAD50 and BARD1 across all five cohorts were investigated based on the median cut-off point of ERBB2 data of each cohort. Therefore, patients with ERBB2 expression values lower than the median cut-off point were considered as ERBB2-low patients. Then the total gene expression of each targeted genes was investigated further in these sub-cohorts of ERBB2 low and high.
Gene–gene interaction network construction and analysis
For gene–gene interaction network between RAD21, RAD50, BARD1 and ERBB2 we used the GeneMANIA Cytoscape plugin (https://apps.cytoscape.org/apps/genemania)59,60. Interaction network covering; physical interactions, co-expression, co-localization, genetic interactions, pathway and shared protein domains. With max 100 genes interaction and max attributes. Network structure was visualized by Cytoscape (https://cytoscape.org/)61. To further analyze and calculate the topology parameters (Node degrees, Betweenness centrality and Closeness centrality) of the network, NetworkAnalyzer62, a plugin in Cytoscape, was applied.
Gene ontology (GO) functional and pathway enrichment analysis
To provide Gene Ontology analysis we used the Database for Annotation, Visualization and Integrated Discovery tool (DAVID; latest version Dec. 2021: https://david.ncifcrf.gov/home.jsp). This tool includes biological process, molecular function, cellular component and also Kyoto Encyclopedia of Gene and Genomes (KEGG) pathway analysis63. Enrichment analysis was performed with the threshold of p < 0.05.
Statistical analyses
Data analysis were performed using JMP Pro 15 (SAS Institute Inc., USA). For the prognostic significance survival curves, Kaplan–Meier method was used with log-rank comparison for significance testing. In the univariate analysis, Chi-square test (χ2) was used to evaluate the relationship between RAD21, RAD50, BARD1 and ERBB2 expression and clinicopathological variables. In multivariate analysis, to emphasize on RAD21, RAD50, BARD1 and ERBB2 interaction, a Cox proportional hazard model was used for the multivariate survival analysis including all potential confounder factors. The proportional hazards assumption was checked, the relationship between log cumulative hazard and a covariate was linear. Where appropriate, two-tailed Student’s t-test was performed using GraphPad Prism (version 9.5.0, USA). All differences were considered statistically significant at p < 0.05, p values were two-sided; all confidence intervals were at 95%.
Results
Expression of ERBB2, RAD21, RAD50 and BARD1 in bladder tissues
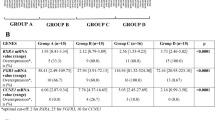
We initially compared the total expression levels of ERBB2, RAD21, RAD50 and BARD1 mRNA in normal and tumor bladder tissues with bioinformatics analyses using the TCGA database (Cohort one). The cohort consists of 413 patients with MIBC and matched normal samples, the TCGA datasets were previously described64. The data revealed a significantly high mRNA expression levels of ERBB2 and RAD21 in tumor tissues compared to normal; median = 6.888 tumor vs. 6.299 normal; p < 0.0001 and median = 6.408 tumor vs. 6.043 normal; p = 0.034, Fig. 1A respectively. RAD50 and BARD1 mRNA levels showed no significant difference between tumors and the respective normal tissues (Fig. 1A). Interestingly, when we sub grouped patients according to ERBB2 status (ERBB2-low and ERBB2-high), we found that RAD21, RAD50 and BARD1 expression levels increased significantly in ERBB2-low patients compared to ERBB2-high patients. Figure 1B, shows RAD21 expression median = 0.02 in ERBB2-low compared to RAD21 median = − 0.07 in ERBB2-high; p < 0.0001. RAD50 expression median = 0.12 in ERBB2-low compared to RAD50 median = − 0.02 in ERBB2-high; p < 0.0001. BARD1 expression median = 0.21 in ERBB2-low compared to BARD1 median = 0.08 in ERBB2-high; p < 0.0001. We validated this finding with Cohort two from MSK dataset (Fig. 1C). As expected, total RAD21 in ERBB2-low cohort increased significantly to the same in ERBB2-high cohort (median = 0.29 vs. median = − 0.34; p < 0.0001). Total RAD50 expression in ERBB2-low patients was higher compared to RAD50 in ERBB2-high cohort (median = 0.20 vs. median = − 0.09; p < 0.0001). The same significant trend was shown with BARD1 expression in different ERBB2 status (median = 0.01 vs. median = − 0.24; p < 0.0001). The second validation dataset (Fig. 1D), Cohort three from GEO-GSE31684 confirmed the elevated expression of the three homologous recombination mRNAs in different ERBB2 status. Data confirmed significant increase of RAD21, RAD50 and BARD1 expression in ERBB2-low patients compared to ERBB2-high patients as follow: total RAD21 (median = 9.81 vs. median = 9.00; p = 0.0001), total RAD50 (median = 9.00 vs. median = 8.70; p = 0.0102) and total BARD1 (median = 6.81 vs. median = 5.45; p < 0.0001).
(A) Boxplot of the mRNA expression levels of ERBB2, RAD21, RAD50 and BARD1 in bladder cancer tissue, along with matching normal tissue. (B) TCGA dot plot showing the mRNA expression levels of ERBB2 in bladder cancer patients, and RAD21, RAD50 and BARD1 expressions at different ERBB2 levels. (C) MSK dot plot showing the mRNA expression levels of ERBB2 in bladder cancer patients, and RAD21, RAD50 and BARD1 expressions at different ERBB2 levels. (D) GEO-GSE31684 dot plot showing the mRNA expression levels of ERBB2 in bladder cancer patients, and RAD21, RAD50 and BARD1 expressions at different ERBB2 levels. *p < 0.05, **p < 0.01, ***p < 0.001 and ****p < 0.0001. All data were analyzed using the two-tailed Student’s t-test.
Association between homologous recombination repair transcripts (RAD21, RAD50 and BARD1) with ERBB2 and survival
The potential prognostic value of RAD21, RAD50 and BARD1 mRNAs expression in different ERBB2 status was assessed using the largest bladder TCGA dataset (Cohort one). In the whole cohort RAD21 expression alone did not influence survival on the disease-free survival (DFS) (p = 0.085; Fig. 2A) and in ERBB2-high cohort (p = 0.991; Fig. 2C). High RAD21 mRNA was significantly associated with poor survival in the ERBB2-low cohort (p = 0.031; Fig. 2B). Poor survival of high RAD21 mRNA was also associated with ERBB2-low cohort of the overall survival (OS), with 5-year OS rate of 34.7% high vs. 40.4% with low RAD21, though not significant (Additional file 1: Fig. S1A–C). In additional cohorts of bladder cancer, patients with high RAD21 mRNA in the ERBB2-low cohorts showed tendency toward poor survival [Cohorts: Cohort four (GEO-GSE48075; with 5-year survival rates of 29.9% high vs. 53.7% low RAD21) and Cohort five the NMIBC (E-MTAB-4321; with 5-years survival rates of 83.3% high vs. 91.4% low RAD21)]; (Additional file 1: Fig. S2A,B, respectively). RAD50 transcript level (Cohort one) did not influence survival in the whole cohort (p = 0.085; Fig. 2D) and in ERBB2-high cohort (p = 0.971; Fig. 2F). Though high RAD50 mRNA was significantly associated with poor survival in the ERBB2-low cohort (p = 0.007; Fig. 2E). High RAD50 mRNA expression also showed tendency toward poor survival in the ERBB2-low cohort of the OS, with 5-year OS rate of 30.5% high vs. 44.6% with low RAD50, though not significant (Additional file 1: Fig. S1D–F). This finding was validated in Cohort three, showing poor recurrence free survival for patients with high RAD50 mRNA in ERBB2-low cohort (5-year survival rate of 38.7% high RAD50 vs. 71.4% low RAD50) compared to the whole cohort, or ERBB2-high cohort (Additional file 1: Fig. S3A). High BARD1 mRNA was significantly associated with poor DFS in the whole cohort (p = 0.003; Fig. 2G) and in ERBB2-low cohort (p = 0.001; Fig. 2H), but not in ERBB2-high cohort (p = 0.550; Fig. 2I). The same tendency toward poor survival was detected in Cohort one (5-year OS rate of 31.1% high vs. 45.0% with low BARD1) and Cohort four between high BARD1 and low ERBB2 patients, with 5-year OS rate of 23.5% high vs. 49.9% with low BARD1 (Additional file 1: Figs. S1G–I and S3B).
Kaplan–Meier analysis for bladder cancer data; Disease free survival (DFS) of RAD21 mRNA expression in (A) whole cohort, (B) ERBB2-Low cohort, (C) ERBB2-High cohort. DFS of RAD50 mRNA expression in (D) whole cohort, (E) ERBB2-Low cohort, (F) ERBB2-High cohort. DFS of BARD1 mRNA expression in (G) whole cohort, (H) ERBB2-Low cohort, (I) ERBB2-High cohort.
Furthermore, investigating the homologous recombination repair transcripts (RAD21, RAD50 and BARD1) with each other revealed that combined expression of high RAD21/high RAD50 significantly associated with worst DFS and better outcome for those with low RAD21/low RAD50 in the ERBB2-low cohort (p = 0.017; Fig. 3B). No significant different in the whole cohort and in the ERBB2-high cohort (Fig. 3A,C). Data also showed a tendency toward poor OS with high RAD21/high RAD50 (5-year OS of 29.5%) and better with low RAD21/low RAD50 (5-year OS of 45.4%) in ERBB2-low patients, but the trend was not significant (Additional file 1: Fig. S4A–C). Similarly, combined high RAD21/high BARD1 associated significantly with worst outcome in the whole cohort and ERBB2-low cohort (p = 0.031, p = 0.005; Fig. 3D,E; respectively). Whereas, no significant association was found in the ERBB2-high patients (Fig. 3F). High RAD21/high BARD1 showed a tendency toward poor OS with 5-year of 29.2% vs. 42.5% with low RAD21/low BARD1 in ERBB2-low cohort (Additional file 1: Fig. S4D–F). Then again, low RAD50/ low BARD1 mRNA expression showed a significantly better DFS compared to other subgroups in the whole cohort and in the ERBB2-low cohort (p = 0.019, p = 0.004; Fig. 3G,H; respectively). The OS was also better with 51.5% 5-year rate vs. 31.1% with high RAD50/high BARD1, though not significant (Additional file 1: Fig. S4G,H). Finally, no significant DFS and OS differences were found in any group among the ERBB2-high cohort (Fig. 3I and Additional file 1: Fig. S4I).
Kaplan–Meier analysis of bladder cancer data; Disease free survival (DFS) of RAD21/RAD50 mRNA expression in (A) whole cohort, (B) ERBB2-Low cohort, (C) ERBB2-High cohort. DFS of RAD21/BARD1 mRNA expression in (D) whole cohort, (E) ERBB2-Low cohort, (F) ERBB2-High cohort. DFS of RAD50/BARD1 mRNA expression in (G) whole cohort, (H) ERBB2-Low cohort, (I) ERBB2-High cohort.
RAD21, RAD50 and BARD1 mRNA levels and clinicopathological features
To further evaluate the impact of RAD21, RAD50 or BARD1 mRNAs with ERBB2 status on the clinicopathological variables, we used the TCGA database (Cohort one). We previously described the ERBB2 distribution of the clinicopathological characteristics of this cohort64. Univariate analysis data indicate that in ERBB2-high cohort mRNA expression of RAD21 low was significantly associated with tumor grade (p = 0.011). Also, BARD1 low was significantly associated with tumor grade (p = 0.04) and non-papillary tumor shape (p = 0.037). However, no association was observed in ERBB2-low cohort (Table 1).
Table 2 summarizes the association between the co-expression of the homologous recombination repair transcripts with ERBB2 and the clinicopathological features. Analyzing the combined high expression of either RAD21/RAD50 or RAD21/BARD1 in ERBB2-low cohort had a significant association with higher chance of metastasis (p = 0.011). On the other hand, low expression of RAD50/BARD1 in ERBB2-low cohort had a significant association with higher tumor stages (p = 0.013). The high expression of RAD50/BARD1 correlated significantly with papillary tumor shape (p = 0.035) (Table 2). No significant association with any co-expression was observed in ERBB2-high cohort (Additional file 2: Table S1).
Multivariate analysis of RAD21, RAD50 or BARD1 mRNAs expression alone or in combination was conducted. This was done to investigate whether the expressions are an independent prognostic factor. As shown in Table 3, multivariate analyses of the above factors together with tumor stage were conducted. BARD1 mRNAs expression was an independent prognostic factor for worse DFS in the ERBB2-low cohort (p = 0.047, Hazard ratio 1.812, 95% CI 1.009–3.330), but not in ERBB2-high cohort. Similarly, in the ERBB2-low cohort combination of RAD50/BARD1 mRNA expression was an independent factor for poor DFS (p = 0.008, Hazard ratio 1.378, 95% CI 1.088–1.760). Whereas tumor stage was an independent prognostic factor for poor DFS in ERBB2-high cohort (< 0.001, Hazard ratio 1.295, 95% CI 1.154–1.458).
Gene interaction network of RAD21, RAD50, BARD1 and ERBB2
A gene interaction network was constructed for the three homologous recombination repair transcripts (RAD21, RAD50 and BARD1) and ERBB2. This was done to identify the most related genes network between our targets. The network was constructed using the GeneMANIA Cytoscape plugin59. Our network was based on the top 100 genes showing 104 nodes and 2239 interactions (Fig. 4A and Additional file 2: Table S2). Interaction percentages in the network were: 82.19% physical interactions, 8.40% co-expression, 3.78% co-localization, 2.99% genetic interactions, 2.01% pathway and 0.64% shared protein domains. In addition, a network interaction was analyzed illustrating the node degrees, betweenness centrality and closeness centrality with Network analyzer of the 100 top genes, as shown in Table 4.
(A) Gene–Gene interaction network demonstrating 100 overlapping genes, along with ERBB2, RAD21, RAD50 and BARD1. (B) GO functional enrichment and KEGG pathway analyses of the all-overlapping genes, ERBB2, RAD21, RAD50 and BARD1. The top significant enriched GO annotation Molecular Function, Biological Process, Cellular Component, KEGG pathway analyses.
Functional and pathway enrichment analyses
The functional enrichment pathways of the RAD21, RAD50, BARD1 and ERBB2 were investigated using DAVID software to identify significant GO categories and KEGG pathways. In the molecular function of GO; majority of genes involved in protein binding along with ERBB2, RAD21 and BARD1. ERBB2 and RAD50 appears in both functions of identical protein binding and ATP binding. Likewise, protein heterodimerization activity showed BARD1 and ERBB2. In the cellular component of GO; most genes are enriched in nucleus along with our four target genes. Cytosol shows ERBB2 and RAD21. RAD21, RAD50 and BARD1 were also found in more functions and pathways involves in; cytoplasm, nucleoplasm, plasma membrane, site of double-strand break and macromolecular complex. In the biological process of GO results were; positive regulation of kinase activity involved both ERBB2 and RAD50. Negative regulation of apoptotic process involved ERBB2 and BARD1. DNA repair, cellular response to DNA damage stimulus, double-strand break repair, cell division and more are suggested to be regulates indirectly with our targeted genes. In the KEGG pathway enrichment analysis data demonstrated that; homologous recombination, ERBB signaling pathway, cell cycle, PI3K-Akt signaling pathway, microRNAs in cancer and pathways in cancer were associated with RAD21, RAD50 and BARD1 (Fig. 4B and Additional file 2: Table S3).
Discussion
Several studies have highlighted the important role of homologous recombination factors (RAD21, RAD50 and BARD1) in cancer progression, aggressiveness and genomic instability in many cancer types22,24,28,43,65,66. Though, these factors remain largely unexplored especially in bladder cancer. We recently highlighted the interplay between ATM (one of the homologous recombination factors) and ERBB2 in bladder cancer patients64. In the current study, we observed a significant overexpression of ERBB2 in bladder cancer tissues compared to normal. This overexpression was in agreement with many published studies that showed overexpression of ERBB2 in solid cancers, serving as a prognostic and predictive biomarker especially in breast, gastric, colorectal and bladder cancer67,68,69,70. Kiss et al., reported that ERBB2 amplification is not always associated with HER2 overexpression in bladder cancer, and HER2 overexpression was observed without gene amplification. Suggesting that both HER2 protein and ERBB2 gene expressions are regulated by different mechanisms71. In this current investigation we examined RAD21, RAD50 or/and BARD1 co-expression with different status of ERBB2 expression and assessed their prognostic and clinical significance in bladder cancer.
Published data reported that RAD21 mRNA amplification correlates with gene copy number in grade 3 luminal, basal and HER2 subtypes of breast cancer. Also, RAD21 protein overexpression correlates strongly with gene amplification27. This overexpression was implicated in many cancer types and associate with poor outcomes in patients22,23,24,25,26. Similarly, RAD21 mRNA was upregulated in bladder cancer tissues compared to normal tissues, also an increase in mRNA level was detected in late-stage bladder cancer cell lines28. In agreement with previous data, our data showed significant upregulation of RAD21 expression in bladder cancer tissues compared to normal. To investigate the relation between RAD21 and ERBB2 expression, we sub-grouped all patients cohorts according to ERBB2 status. Interestingly we found that RAD21 mRNA level increase significantly in patients with low-ERBB2 compared to patients with high-ERBB2. Furthermore, as Yu et al., indicated in their whole cohort RAD21 expression alone did not influence survival significantly on the OS28. In this study, we confirmed this in OS and DFS, also in both subgroups of ERBB2 cohorts. Interestingly we found high RAD21 mRNA was linked to poor survival in the ERBB2-low cohort in the main MIBC cohort and confirmed it in both high grade and MIBC validation cohorts. Furthermore, we also found this trend in both the low tumor grade subgroup and the early tumor stage (Ta) subgroup of the NMIBC validation cohort. In contrast, RAD21 low mRNA showed significant association with low tumor grade in ERBB2-high cohort. These findings suggest that additional data maybe required in the future to corroborate statistically the impact that RAD21 plays in specific types of bladder cancer.
RAD50 is one of the key players in homologous recombination repair and telomere maintenance29. Literature is reporting that RAD50 high expression associated with aggressive high grade cystadenocarcinomas and low RAD50 linked to better progression free survival72. The aggressive phenotype and poor survival associated with high RAD50 expression at protein and transcriptomic levels was also reported in bladder, gastric, colorectal, rectal and ovarian cancers73,74,75,76. Hence the RAD50 factor role is yet to be elucidated in different cancer types, in the current study we first assessed the total RAD50 mRNA expression level which was not altered in bladder cancer compared to normal tissues. Interestingly, following the subgrouping of cohort according to ERBB2 status, we found that RAD50 mRNA level increased significantly in patients with low-ERBB2 compared to patients with high-ERBB2. This increase was translated to poor DFS for patients with high RAD50 in the ERBB2-low cohort. This finding was confirmed in the MIBC and the high grade cohorts. Moreover, the same trend was seen in the low grade subgroup and the early tumor stage (Ta) subgroup of the NMIBC cohort. These findings further support our conclusion that RAD50 mRNA level may have a poor prognostic role in ERBB2-Low bladder cancer patients, regardless of the grade or stage distribution of the cohort. Further significant associations between clinicopathological variables and RAD50 at different ERBB2 levels were not seen.
BARD1 is another player in the homologous recombination pathway, it was suggested that this role in DNA repair pathway is through direct interact between BARD1 and BRCA140,41. Variants of BARD1 gene were associated with many solid tumors44,45,46,77. Hawsawi et al., recently illustrated that high BARD1 mRNA expression was associated with poor OS, relapse free survival and distant metastasis free survival in breast, ovarian and gastric cancer but not lung cancer43. In the current study, BARD1 mRNA did not show any alteration in expression level between bladder cancer tissues and normal. Though, significant upregulation was observed in BARD1 mRNA in patients with low-ERBB2 compared to patients with high-ERBB2 in all study cohorts. Interestingly this high BARD1 mRNA was translated to poorer DFS in the whole cohort and in the ERBB2-low cohort in compared to patients with low BARD1, though no significant was detected when ERBB2 expression was high. Based on our analysis, we have observed an association between high levels of BARD1 mRNA expression and poor survival in the main cohort, as well as the validation MIBC cohort. Additionally, we found a similar trend in the NMIBC subgroups, particularly in the low grade and early tumor stage (Ta–T1) patients. This implies that BARD1 mRNA may be a promising prognostic marker for bladder cancer patients, irrespective of the tumor grade or stage. In contrast, BARD1 low expression was significantly associated with low tumor grade and non-papillary tumor shape in ERBB2-high patients. We also showed that BARD1 mRNAs expression was independent prognostic factor for worse DFS in the ERBB2-low cohort, but not in ERBB2-high cohort. Our observations suggest the potential value of the expression pattern of BARD1 at specific subtypes of bladder cancer.
As we highlighted the role of each homologous recombination factors (RAD21, RAD50 or BARD1) to patients’ survival and cancer aggressiveness in bladder cancer, other groups studied these factors in different cancer types22,24,28,43,65,66. Here we also performed a co-expression analysis of these factors. Our data demonstrated that patients with low RAD21/low RAD50 tumors along with low ERBB2 expression had better survival outcome compared to those patients with high RAD21/high RAD50 tumors. Also, high RAD21/high BARD1 tumors had the worst survival in the whole cohort and ERBB2-low patients, but not in ERBB2-high patients. The high expression of either RAD21/RAD50 or RAD21/BARD1 in ERBB2-low cohort had a significant association with an increased chance of metastasis compared to the other combinations. Similarly, low RAD50/low BARD1 mRNA expression showed better outcome in compared to high RAD50/high BARD1 tumors in the whole cohort and ERBB2-low patients. High expression of RAD50/BARD1 associated significantly with papillary tumor shape in ERBB2-low patients. Multivariate analyses data showed that RAD50/BARD1 mRNA expression was independent prognostic factor for poor DFS in the ERBB2-low patients. Therefore, these homologous recombination potential biomarkers may play roles in predicting metastasis and survival in bladder cancer patients.
We next sought to investigate the interaction network between RAD21, RAD50, BARD1 and ERBB2 to provide deeper insight into the molecular mechanisms of these relations through identifying the most related genes network between our targets. Overlapping genes were identified with high physical interactions, co-expression, co-localization, genetic interactions, shared pathway and shared protein domains with RAD21, RAD50, BARD1 and ERBB2. These genes include: BRCA1, SMC3, H2AX, EGFR, SMC1A, PCNA, ATM, RPA2, TP53, RPA3, LMNB1, RPA1, BLM, TERF2, STAG1, MRE11, PRKDC, TERF2IP, STAG2, CDK4, TOPBP1, TERF1, POT1 and more. Centrality measure of this network indicates the importance of these intermediate genes to the interaction between our targets. This was followed with the functional and pathway enrichment analysis which showed majority of the overlapping genes with ERBB2, RAD21 and BARD1 involves in protein binding. ERBB2 and RAD50 factors appear in identical protein binding and ATP binding. Moncalian et al., showed how the motif signature is essential to ATP binding and biological function of RAD5078. Tarsounas et al., discussed how BARD1 and BRCA1 heterodimers through its E3 ubiquitin ligase activity, then the ability of this heterodimer to interact with other DNA damage response factors through the homologous repair pathway40. Our data suggested the involvement of both BARD1 and ERBB2 along with other overlapping genes in protein heterodimerization activity. We also found that many genes are enriched along with our four target genes in the nucleus, which agrees with other studies emphasizing our target genes functional role in localizing to the nucleus to participate in the DNA repair25,79,80. In addition, data illustrated that ERBB2 and RAD50 appear in the positive regulation of kinase activity. Similarly, the enriched results also identified ERBB2 and BARD1 are requires in the negative regulation of apoptotic process43,81. Altogether, a strong overlap of ERBB2-driven pathways was found with our homologous recombination factors, which may help define a signature to select bladder cancer patients who may benefit from targeted therapy and may use to evaluate drug response for patients.
Conclusions
To our knowledge, this is the first time where the relationship between RAD21, RAD50, BARD1 and ERBB2 was highlighted in bladder cancer. This study provided novel findings and potential prognostic markers in this type of cancer. Importantly, here we showed that high RAD21, RAD50 or BARD1 mRNA expression in bladder cancer patients with low-ERBB2 exhibit poor survival. In addition, gene expression of BARD1 alone or in combination with RAD50 acted as an independent prognostic factor for worst survival. We also identified several promising candidate genes between our targets which could be incorporated in tumor prognosis. The fact that this is a retrospective observational study is the main limitation of our work, therefore further analysis is needed. Additionally, we recognize that the median value method we used to divide the dataset into two groups based on expression levels may also have limitations due to the small sample size and limited clinical data available. In future studies, we plan to utilize more advanced methods that can accommodate larger sample sizes and more comprehensive clinical data. This is to better assess the clinical relevance of differentially expressed genes and identify potential biomarkers for bladder cancer prognosis. Also, the exact molecular mechanism between our homologous recombination targets and ERBB2 still need to be investigated to improve prognosis and treatment efficacy in bladder cancer. Using bioinformatical analysis tools to find potential overlapping gene is a good step, though validating these finding with experimental test is a must to understand the mechanism.
Data availability
All data analyzed during this study are from publicly available databases as indicated in the Materials and methods/Study cohorts and data analysis. TCGA data were downloaded from UALCAN portal (http://ualcan.path.uab.edu/index.html); [BLCA] and cBioPortal (https://www.cbioportal.org/); Bladder Cancer [TCGA, Cell 2017] and Bladder Cancer [MSK, J Clin Onco 2013]. From GEO database; Platform GPL570 [accession no. ‘GSE31684’] and Platform GPL6947 [accession no. ‘GSE48075’]. From ArrayExpress database (https://www.ebi.ac.uk/biostudies/arrayexpress) accession no. E-MTAB-4321 was used.
Abbreviations
- NMIBC:
-
Non-muscle invasive bladder cancer
- MIBC:
-
Muscle-invasive bladder cancer
- HER2/ERBB2:
-
Human epidermal growth factor receptor 2
- BRCA1:
-
Breast cancer 1 gene
- TCGA:
-
The Cancer Genome Atlas
- MSK:
-
Memorial Sloan Kettering
- GEO:
-
The Gene Expression Omnibus
- GO:
-
Gene Ontology
- KEGG:
-
Kyoto Encyclopedia of Gene and Genomes
- DAVID:
-
Database for Annotation, Visualization and Integrated Discovery tool
- OS:
-
Overall survival
- DFS:
-
Disease-free survival
References
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Witjes, J. A. et al. European association of urology guidelines on muscle-invasive and metastatic bladder cancer: Summary of the 2020 guidelines. Eur. Urol. 79(1), 82–104 (2021).
Planz, B. et al. The role of urinary cytology for detection of bladder cancer. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 31(3), 304–308 (2005).
Flaig, T. W. et al. NCCN guidelines® insights: Bladder cancer, version 22022: featured updates to the NCCN guidelines. J. Natl. Compr. Cancer Netw. 20(8), 866–878 (2022).
Batista, R. et al. Biomarkers for bladder cancer diagnosis and surveillance: A comprehensive review. Diagnostics (Basel, Switzerland). 10(1), 39 (2020).
Moasser, M. M. The oncogene HER2: Its signaling and transforming functions and its role in human cancer pathogenesis. Oncogene 26(45), 6469–6487 (2007).
Li, W. et al. HER2-targeted advanced metastatic gastric/gastroesophageal junction adenocarcinoma: Treatment landscape and future perspectives. Biomark. Res. 10(1), 71 (2022).
Koshkin, V. S., O’Donnell, P., Yu, E. Y. & Grivas, P. Systematic review: Targeting HER2 in bladder cancer. Bladder Cancer (Amsterdam, Netherlands). 5, 1–12 (2019).
Sanguedolce, F. et al. HER2 expression in bladder cancer: A focused view on its diagnostic, prognostic, and predictive role. Int. J. Mol. Sci. 24(4), 3720 (2023).
Gan, K., Gao, Y., Liu, K., Xu, B. & Qin, W. The clinical significance and prognostic value of HER2 expression in bladder cancer: A meta-analysis and a bioinformatic analysis. Front. Oncol. 11, 653491 (2021).
Sikic, D. et al. High expression of ERBB2 is an independent risk factor for reduced recurrence-free survival in patients with stage T1 non-muscle-invasive bladder cancer. Urol. Oncol. 40(2), 63e9-.e18 (2022).
Scholtes, M. et al. Targeted therapy in metastatic bladder cancer: Present status and future directions. Appl. Sci. 10(20), 7102 (2020).
De Carlo, C., Valeri, M., Corbitt, D. N., Cieri, M. & Colombo, P. Non-muscle invasive bladder cancer biomarkers beyond morphology. Front. Oncol. 12, 947446 (2022).
Sjödahl, G., Jackson, C. L., Bartlett, J. M., Siemens, D. R. & Berman, D. M. Molecular profiling in muscle-invasive bladder cancer: More than the sum of its parts. J. Pathol. 247(5), 563–573 (2019).
Chen, D., Ye, Y., Guo, S. & Yao, K. Progress in the research and targeted therapy of ErbB/HER receptors in urothelial bladder cancer. Front. Mol. Biosci. 8, 800945 (2021).
Peters, J. M., Tedeschi, A. & Schmitz, J. The cohesin complex and its roles in chromosome biology. Genes Dev. 22(22), 3089–3114 (2008).
Waldman, T. Emerging themes in cohesin cancer biology. Nat. Rev. Cancer. 20(9), 504–515 (2020).
Losada, A. Cohesin in cancer: Chromosome segregation and beyond. Nat. Rev. Cancer 14(6), 389–393 (2014).
Cheng, H., Zhang, N. & Pati, D. Cohesin subunit RAD21: From biology to disease. Gene 758, 144966 (2020).
Antony, J., Chin, C. V. & Horsfield, J. A. Cohesin mutations in cancer: Emerging therapeutic targets. Int. J. Mol. Sci. 22(13), 6788 (2021).
Sharaf, R. et al. A pan-cancer landscape of telomeric content shows that RAD21 and HGF alterations are associated with longer telomeres. Genome Med. 14(1), 25 (2022).
Deb, S. et al. RAD21 cohesin overexpression is a prognostic and predictive marker exacerbating poor prognosis in KRAS mutant colorectal carcinomas. Br. J. Cancer. 110(6), 1606–1613 (2014).
Zhu, T., Gao, Z., Yuan, K. & Wang, Y. High expression of RAD21 predicts poor survival in patients with operated non-small-cell lung cancer. Tumori 106, 300891620910805 (2020).
Xia, L. et al. The effect of aberrant expression and genetic polymorphisms of Rad21 on cervical cancer biology. Cancer Med. 7(7), 3393–3405 (2018).
Gou, R. et al. RAD21 confers poor prognosis and affects ovarian cancer sensitivity to poly(ADP-ribose)polymerase inhibitors through DNA damage repair. Front. Oncol. 12, 936550 (2022).
Deb, S., Xu, H., Clouston, D., Ramsay, R. & Fox, S. B. 20. RAD21 overexpression is frequently observed in prostate cancer. Pathology 44, S110–S1 (2012).
Xu, H. et al. Enhanced RAD21 cohesin expression confers poor prognosis and resistance to chemotherapy in high grade luminal, basal and HER2 breast cancers. Breast Cancer Res. 13(1), R9 (2011).
Yu, Z. et al. DNA topoisomerase IIα and RAD21 cohesin complex component are predicted as potential therapeutic targets in bladder cancer. Oncol. Lett. 18(1), 518–528 (2019).
Assenmacher, N. & Hopfner, K. P. MRE11/RAD50/NBS1: Complex activities. Chromosoma 113(4), 157–166 (2004).
Bian, L., Meng, Y., Zhang, M. & Li, D. MRE11-RAD50-NBS1 complex alterations and DNA damage response: implications for cancer treatment. Mol. Cancer 18(1), 169 (2019).
García-Sanz, P. et al. Chromatin remodelling and DNA repair genes are frequently mutated in endometrioid endometrial carcinoma. Int. J. Cancer 140(7), 1551–1563 (2017).
Fan, C. et al. RAD50 germline mutations are associated with poor survival in BRCA1/2-negative breast cancer patients. Int. J. Cancer 143(8), 1935–1942 (2018).
Wang, M. J. et al. Prognostic significance and molecular features of colorectal mucinous adenocarcinomas: A strobe-compliant study. Medicine (Baltimore) 94(51), e2350 (2015).
Ho, V. et al. Early postoperative low expression of RAD50 in rectal cancer patients associates with disease-free survival. Cancers 9(12), 163 (2017).
Söderlund, K. et al. Intact Mre11/Rad50/Nbs1 complex predicts good response to radiotherapy in early breast cancer. Int. J. Radiat. Oncol. Biol. Phys. 68(1), 50–58 (2007).
Wang, Y. et al. RAD50 expression is associated with poor clinical outcomes after radiotherapy for resected non-small cell lung cancer. Clin. Cancer Res. 24(2), 341–350 (2018).
Laurberg, J. R. et al. Expression of TIP60 (tat-interactive protein) and MRE11 (meiotic recombination 11 homolog) predict treatment-specific outcome of localised invasive bladder cancer. BJU Int. 110(11 Pt C), E1228–E1236 (2012).
Choudhury, A. et al. MRE11 expression is predictive of cause-specific survival following radical radiotherapy for muscle-invasive bladder cancer. Cancer Res. 70(18), 7017–7026 (2010).
Teo, M. T. W. et al. Next-generation sequencing identifies germline MRE11A variants as markers of radiotherapy outcomes in muscle-invasive bladder cancer. Ann. Oncol. 25(4), 877–883 (2014).
Tarsounas, M. & Sung, P. The antitumorigenic roles of BRCA1–BARD1 in DNA repair and replication. Nat. Rev. Mol. Cell Biol. 21(5), 284–299 (2020).
Westermark, U. K. et al. BARD1 participates with BRCA1 in homology-directed repair of chromosome breaks. Mol. Cell. Biol. 23(21), 7926–7936 (2003).
Alenezi, W. M., Fierheller, C. T., Recio, N. & Tonin, P. N. Literature review of BARD1 as a cancer predisposing gene with a focus on breast and ovarian cancers. Genes 11(8), 856 (2020).
Hawsawi, Y. M. et al. BARD1 mystery: Tumor suppressors are cancer susceptibility genes. BMC Cancer 22(1), 599 (2022).
Weber-Lassalle, N. et al. Germline loss-of-function variants in the BARD1 gene are associated with early-onset familial breast cancer but not ovarian cancer. Breast Cancer Res. 21(1), 55 (2019).
Lee, A. et al. Enhancing the BOADICEA cancer risk prediction model to incorporate new data on RAD51C, RAD51D, BARD1 updates to tumour pathology and cancer incidence. J. Med. Genet. 59(12), 1206–1218 (2022).
Suszynska, M. & Kozlowski, P. Summary of BARD1 mutations and precise estimation of breast and ovarian cancer risks associated with the mutations. Genes 11(7), 798 (2020).
Watters, A. K. et al. The effects of genetic and epigenetic alterations of BARD1 on the development of non-breast and non-gynecological cancers. Genes 11(7), 829 (2020).
Börcsök, J. et al. Detection of molecular signatures of homologous recombination deficiency in bladder cancer. Clin. Cancer Res. 27(13), 3734–3743 (2021).
Chandrashekar, D. S. et al. UALCAN: A portal for facilitating tumor subgroup gene expression and survival analyses. Neoplasia 19(8), 649–658 (2017).
Robertson, A. G. et al. Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell 171(3), 540–56.e25 (2017).
Cerami, E. et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2(5), 401–404 (2012).
Gao, J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 6(269), pl1 (2013).
Iyer, G. et al. Prevalence and co-occurrence of actionable genomic alterations in high-grade bladder cancer. J. Clin. Oncol. 31(25), 3133–3140 (2013).
Riester, M. et al. Combination of a novel gene expression signature with a clinical nomogram improves the prediction of survival in high-risk bladder cancer. Clin. Cancer Res. 18(5), 1323–1333 (2012).
Riester, M. et al. Integrative analysis of 1q23.3 copy-number gain in metastatic urothelial carcinoma. Clin. Cancer Res. 20(7), 1873–1883 (2014).
Choi, W. et al. Identification of distinct basal and luminal subtypes of muscle-invasive bladder cancer with different sensitivities to frontline chemotherapy. Cancer Cell 25(2), 152–165 (2014).
Guo, C. C. et al. Assessment of luminal and basal phenotypes in bladder cancer. Sci. Rep. 10(1), 9743 (2020).
Hedegaard, J. et al. Comprehensive transcriptional analysis of early-stage urothelial carcinoma. Cancer Cell 30(1), 27–42 (2016).
Mostafavi, S., Ray, D., Warde-Farley, D., Grouios, C. & Morris, Q. GeneMANIA: A real-time multiple association network integration algorithm for predicting gene function. Genome Biol. 9(Suppl 1), S4 (2008).
Warde-Farley, D. et al. The GeneMANIA prediction server: Biological network integration for gene prioritization and predicting gene function. Nucleic Acids Res. 38(Web Server issue), W214–W220 (2010).
Shannon, P. et al. Cytoscape: A software environment for integrated models of biomolecular interaction networks. Genome Res. 13(11), 2498–2504 (2003).
Assenov, Y., Ramírez, F., Schelhorn, S. E., Lengauer, T. & Albrecht, M. Computing topological parameters of biological networks. Bioinformatics (Oxford, England). 24(2), 282–284 (2008).
da Huang, W., Sherman, B. T. & Lempicki, R. A. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat. Protoc. 4(1), 44–57 (2009).
Albarakati, N. et al. Interaction between HER2 and ATM predicts poor survival in bladder cancer patients. J. Cell Mol. Med. 26(19), 4959–4973 (2022).
Li, Y. et al. Rad50 promotes ovarian cancer progression through NF-κB activation. J. Cell Mol. Med. 25(23), 10961–10972 (2021).
Heikkinen, K. et al. RAD50 and NBS1 are breast cancer susceptibility genes associated with genomic instability. Carcinogenesis 27(8), 1593–1599 (2006).
Subramanian, J., Katta, A., Masood, A., Vudem, D. R. & Kancha, R. K. Emergence of ERBB2 mutation as a biomarker and an actionable target in solid cancers. Oncologist 24(12), e1303–e1314 (2019).
Swain, S. M., Shastry, M. & Hamilton, E. Targeting HER2-positive breast cancer: Advances and future directions. Nat. Rev. Drug Discovery 22(2), 101–126 (2023).
Bartley, A. N. et al. Template for reporting results of HER2 (ERBB2) biomarker testing of specimens from patients with adenocarcinoma of the stomach or esophagogastric junction. Arch. Pathol. Lab. Med. 139(5), 618–620 (2015).
Wang, N. et al. Emerging role of ERBB2 in targeted therapy for metastatic colorectal cancer: Signaling pathways to therapeutic strategies. Cancers 14(20), 5160 (2022).
Kiss, B. et al. Her2 alterations in muscle-invasive bladder cancer: Patient selection beyond protein expression for targeted therapy. Sci. Rep. 7, 42713 (2017).
Alblihy, A. et al. RAD50 deficiency is a predictor of platinum sensitivity in sporadic epithelial ovarian cancers. Mol. Biomed. 1(1), 19 (2020).
Altan, B. et al. High expression of MRE11-RAD50-NBS1 is associated with poor prognosis and chemoresistance in gastric cancer. Anticancer Res. 36(10), 5237–5247 (2016).
Chen, C. et al. Targeting RAD50 increases sensitivity to radiotherapy in colorectal cancer cells. Neoplasma 65(1), 75–80 (2018).
Ho, V. et al. Overexpression of the MRE11-RAD50-NBS1 (MRN) complex in rectal cancer correlates with poor response to neoadjuvant radiotherapy and prognosis. BMC Cancer 18(1), 869 (2018).
Herrmann, J. et al. RNA expression of DNA damage response genes in muscle-invasive bladder cancer: Influence on outcome and response to adjuvant cisplatin-based chemotherapy. Int. J. Mol. Sci. 22(8), 4188 (2021).
Stempa, K. et al. Do BARD1 mutations confer an elevated risk of prostate cancer?. Cancers 13(21), 5464 (2021).
Moncalian, G. et al. The rad50 signature motif: Essential to ATP binding and biological function. J. Mol. Biol. 335(4), 937–951 (2004).
Zhu, Q. et al. RNF19A-mediated ubiquitination of BARD1 prevents BRCA1/BARD1-dependent homologous recombination. Nat. Commun. 12(1), 6653 (2021).
Friis, I. & Solov’yov, I. A. Activation of the DNA-repair mechanism through NBS1 and MRE11 diffusion. PLoS Comput. Biol. 14(7), e1006362 (2018).
Haenssen, K. K. et al. ErbB2 requires integrin alpha5 for anoikis resistance via Src regulation of receptor activity in human mammary epithelial cells. J. Cell Sci. 123(Pt 8), 1373–1382 (2010).
Funding
This work was supported by a grant from King Abdullah International Medical Research Center (Protocol No.: RJ17/072/J).
Author information
Authors and Affiliations
Contributions
N.A.: conception and design, data collection, analyzed, data interpretation and manuscript writing. H.A.: data collection and manuscript revision. B.A.: data interpretation, major contributor in writing, revising and editing the manuscript. A.A.: data interpretation, major contributor in writing, revising and editing the manuscript. All authors provided critical feedback. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Albarakati, N., Al-Ghamdi, H., Al-Sowayan, B. et al. Homologous recombination mRNAs (RAD21, RAD50 and BARD1) have a potentially poor prognostic role in ERBB2-low bladder cancer patients. Sci Rep 13, 11738 (2023). https://doi.org/10.1038/s41598-023-38923-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-38923-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.