Abstract
Bilateral subthalamic nucleus deep brain stimulation (STN-DBS) is an effective treatment in advanced Parkinson’s Disease (PD). However, the effects of STN-DBS on speech are still debated, particularly in the long-term follow-up. The objective of this study was to evaluate the long-term effects of bilateral STN-DBS on speech in a cohort of advanced PD patients treated with bilateral STN-DBS. Each patient was assessed before surgery through a neurological evaluation and a perceptual-acoustic analysis of speech and re-assessed in the long-term in different stimulation and drug conditions. The primary outcome was the percentage change of speech intelligibility obtained by comparing the postoperative on-stimulation/off-medication condition with the preoperative off-medication condition. Twenty-five PD patients treated with bilateral STN-DBS with a 5-year follow-up were included. In the long-term, speech intelligibility stayed at the same level as preoperative values when compared with preoperative values. STN-DBS induced a significant acute improvement of speech intelligibility (p < 0.005) in the postoperative assessment when compared to the on-stimulation/off-medication and off-stimulation/off-medication conditions. These results highlight that STN-DBS may handle speech intelligibility even in the long-term.
Similar content being viewed by others
Introduction
Bilateral subthalamic nucleus deep brain stimulation (STN-DBS) represents a short and long-term effective treatment in advanced Parkinson’s Disease (PD)1,2. However, the long-term effects of bilateral STN-DBS on axial features3,4 and different speech variables are still debated. After surgery, PD patients may develop heterogeneous profiles of dysarthria related to the possible spreading of current to cerebellothalamic, cortico-bulbar, cortico-spinal and pallido-fugal levels5,6. Moreover, it has been previously reported that speech intelligibility may worsen 1 year after surgery when compared with those under a control group under optimal medical treatment7. The majority of the studies regarding the effects of STN-DBS on speech focused on short-term follow-up7,8,9,10,11 while few studies have assessed the long-term effects2,12,13,14. In particular, a previous study reported a worsening of speech intelligibility at five and eight years after surgery in the off-medication condition12, while another acoustic study reported variation of the long-term averaged spectrum (LTAS) descriptors for reading and monologue in different stimulation conditions in the long-term after surgery14. The objective of this study was to evaluate the long-term (five years) effects of bilateral STN-DBS on speech in advanced PD patients using a standardized perceptual-acoustic analysis of speech. In the following paragraphs we will report the results of the study, followed by the discussion of these findings before finally describing the methodology of the study.
Results
Patient population
From 2012 to 2017, 40 PD patients underwent STN-DBS. Of these, fifteen subjects were excluded from the study because of missing data (eight patients), lack of consent to participate (four patients), and non-native Italian speakers (three patients). The remaining 25 PD patients with a median follow-up of five years after surgery (range 3–7 years) were included (males: 18; disease duration at surgery: 10.44 [± 4.62] years; age at surgery: 58.40 [± 5.73] years; age at PD onset 47.76 [± 5.63] years). Nineteen patients were included in the PIGD subtype, five in the indeterminate, and one in the TD subtype. Genetic assessment revealed heterozygous mutation in the GBA gene in three patients (12%). Preoperative brain-MRI revealed the presence of white matter hyperintensities of vascular origin in four patients (16%). The mean preoperative levodopa responsiveness was 62.24% (± 16.38%). A detailed description of stimulation parameters and settings is reported in Table 1, while the changes of the different speech and clinical variables in the different conditions tested are shown in Table 2. Concerning the perceptual assessment of dysarthria severity, a significant reduction of the score was found in all the three postoperative conditions tested when compared with the preoperative ones. On the contrary, no significant differences were found by comparing the different postoperative conditions with each other.
Primary outcomes
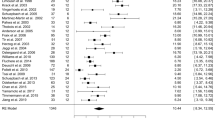
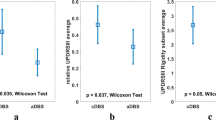
In the long-term and at the group level, speech intelligibility did not significantly worsen with respect to preoperative values when comparing the postoperative on-stimulation/off-medication condition with the preoperative off-medication condition (z = − 0.371, p = 0.710). The shutdown of the stimulation led to an acute significant worsening of speech intelligibility in the postoperative assessment (z = − 3.500, p < 0.001) when comparing the on-stimulation/off-medication and off-stimulation/off-medication conditions. Furthermore, the assessment of disease progression effects on speech intelligibility obtained when comparing the postoperative off-stimulation/off-medication condition with the preoperative off-medication condition showed a significant worsening with respect to preoperative values (z = − 2.92, p < 0.005). Analyzing the long-term postoperative changes of speech intelligibility at the individual level for each patient, sixteen patients were classified as “stable” while the remaining nine patients integrated a “worsened” subgroup (Fig. 1). Compared to a “stable” subgroup, “worsened” patients showed a greater preoperative and postoperative disease motor severity quantified by: (i) higher scores in the UPDRS part III total score, H&Y staging, and akinesia subscore in the off-medication condition; (ii) lower loudness of spontaneous speech and lower speech intelligibility in all three postoperative conditions; (iii) lower intensity of prolonged phonation in on-stimulation/off-medication and off-stimulation/off-medication conditions (Table 3). Furthermore, they showed a significantly worse performance in the preoperative Stroop test (errors) and postoperative Trail Making test B. In addition, all the GBA1-PD patients were included in the “worsened” subgroup with a trend toward significance (p = 0.06) at the chi-square independence test. Disease duration, age at surgery, follow-up duration and stimulation parameters were not significantly different between the two subgroups.
Secondary outcomes
Regarding the comparison between the different speech variables in the conditions tested, a statistically significant reduction of the duration of sustained phonation was found in the off-stimulation/off-medication condition when compared with the on-stimulation/off-medication condition (p < 0.005) and with the preoperative on-medication condition (p < 0.005). In addition, the mean intensity of sustained phonation was significantly reduced in the off-stimulation/off-medication condition if compared with the preoperative off-medication condition (p < 0.005) highlighting the negative effects of disease progression on this acoustic parameter.
A direct correlation between the variation of speech intelligibility and tremor (p = 0.026) and PIGD subscores (p = 0.040) by comparing the off-stimulation/off-medication with the on-stimulation/off-medication one was also found, highlighting that the rebound of tremor and axial symptoms can worsen speech in the acute testing situation. On the contrary, no correlations were found between the variation of speech intelligibility and the changes in the different motor scores and subscores when comparing the on-stimulation/off-medication and preoperative off-medication condition. Furthermore, a negative correlation was also found in the on-stimulation/off-medication condition between speech intelligibility and akinesia subscore (p = 0.025) meaning that patients with a more severely decreased movements amplitude and speed have less intelligibility. The negative correlation between speech intelligibility and akinesia subscore was also confirmed in the on-stimulation/on-medication condition (p = 0.013).
Discussion
Our results add to further observations regarding the long-term effects of bilateral STN-DBS on speech in PD patients7,12. Globally, the studied cohort showed a long-term maintenance of speech intelligibility after surgery, highlighting some possible beneficial long-term effects of STN-DBS when comparing off stimulation and on stimulation conditions. This is consistent with previous studies that showed no worsening of speech following STN-DBS when assessed either with the UPDRS speech item15 or dedicated perceptual assessments16, which was reduced with the introduction of L-DOPA17, in line with our findings. Nevertheless, when using a proper perceptual assessment of speech intelligibility, it is commonly accepted that a significant worsening of speech intelligibility should be expected one year after surgery, when comparing postoperative on-stimulation/off-medication condition with the preoperative off-medication condition9,18. This has also been reported in the long-term by Aviles-Olmos et al.12, who reported a significant worsening of speech intelligibility at five (− 43.7%) and eight years (− 21.4%) in the off-medication conditions if compared with preoperative values. The different results obtained in our cohort may be due to the different evaluation of speech intelligibility (i.e., sentence task of the Assessment of Intelligibility for Dysarthric Speech and single word intelligibility). However, by looking at the individual cases of our cohort in detail, two distinct subgroups could be identified based on the long-term changes of speech intelligibility, with different clinical characteristics. This is in line with similar approaches that tried to disentangle different possible speech outcomes following STN-DBS18,19. Patients in the “worsened” subgroup showed a worse preoperative and postoperative motor disease severity together with a worse cognitive function particularly regarding executive-frontal domain. These results are in line with a recent 2-year follow-up study that underlined the potential predictor role of preoperative cognitive function for speech deterioration after STN-DBS19. The trend toward the significance of PIGD subscores between the two “worsened” and “stable” subgroups suggests a possible link between speech deterioration and axial features, confirming the correlation between hypokinetic dysarthria and PD axial symptoms8. A similar tendency towards significance was also found for the over-distribution of GBA1-PD patients in the “worsened” group. GBA1-PD patients complain about higher axial and cognitive burden when compared with wild-type PD patients20 leading to the assumption that GBA1-PD patients may be at higher risk of developing post-operatively not only gait and cognitive worsening but also speech deterioration. Interestingly, disease duration, sex, duration of follow-up and the total electrical energy delivered by STN-DBS21 did not significantly differ between the two groups. This result is in line with a previous study that did not find any association between speech intelligibility deterioration and disease duration7 even if another study by Tripoliti et al.9 found that disease duration was a predictive factor for speech outcome. In addition, concerning preoperative speech variables we did not find differences between the two groups, while postoperatively, both speech intelligibility and mean intensity of spontaneous speech were significantly lower in the worsened group if compared with the stable one. With regards to the comparison between the different speech variables, a statistically significant reduction of the intensity of sustained phonation emerged in the off-stimulation/off-medication condition if compared with the on-stimulation/off-medication condition highlighting the possible positive effect of STN-DBS on voice intensity, as already confirmed in previous studies7,18. The improvement of speech intensity due to STN-DBS has been linked to its effects on hypokinesia and rigidity of language-related organs18,22 which represent one of the major pathophysiological bases of hypokinetic dysarthria, characterized by hypophonia, monotony, hypoarticulation of consonants and inappropriate silences23.
A further result that emerged in our sample was the significant reduction of the maximum phonation time (MPT) in the off-stimulation/off-medication condition when compared to the on-stimulation/off-medication condition. This result shows how stimulation, even 5 years after surgery, can positively influence MPT that is significantly reduced following the device’s shutdown. This finding is in line with previous studies that reported a beneficial effect of stimulation on MPT in the short-term after surgery24. Even in this case, the reduction of MPT can be traced back to the underlying laryngeal dysfunction and the reduced respiratory volume mainly related to the rigidity and hypo-bradykinesia of the laryngeal and diaphragmatic muscles23.
This study also allows for evaluation of the possible effects of dopaminergic therapy alone on speech parameters by comparing the preoperative off-medication and on-medication conditions. The results obtained did not show statistically significant differences between these two conditions, suggesting that dopaminergic therapy alone did not significantly improve or maintain speech postoperatively. These findings were consistent with previous studies that showed little or no effects of levodopa alone on acoustic speech parameters8,25,26,27. In particular, no significant changes following levodopa intake were found in phonatory, articulatory or prosodic parameters, as previously reported27 confirming the possible involvement of non-dopaminergic pathways in the pathophysiology of hypokinetic dysarthria in PD8.
We also found a direct correlation between the variation of speech intelligibility and tremor and PIGD subscores highlighting that the rebound of tremor and axial symptoms may worsen speech in the acute testing situation when stimulation is turned off. In addition, speech intelligibility also correlated with the UPDRS akinesia subscore in two out of the three postoperative conditions tested, highlighting a possible link between the decrease in limb movement speed and amplitude and speech. This is in line with other studies that have reported a correlation between speech variables and limb bradykinesia28,29. Our study has several limitations, including a lack of definition for the position of the electrodes, the small sample size, the lack of a control group and the lack of the assessment of speech intelligibility also at the sentence level. Nevertheless, our findings highlight the possibility of positive effects of STN-DBS on speech intelligibility after surgery in the long-term. Interestingly, it also gives a better understanding of PD characteristics associated with long-term speech worsening after STN-DBS. This information may allow clinicians to improve candidates’ selection for DBS and refine prognostic accuracy (e.g., GBA1 genetic status influence on speech) and that, if necessary, early speech interventions should be used after surgery in PD patients treated with STN-DBS at a higher risk of speech deterioration.
Methods
Participants
Patients treated with bilateral STN-DBS from 2012 to 2017 at the Neurological Unit of the OCB University Hospital were included. All patients fulfilled the diagnosis of PD according to the UK Brain Bank criteria30 and suffered from disabling motor complications. Data from non-native Italian speakers were excluded. This study was approved by the ethics committee of the Area Vasta Emilia Nord, Italy (protocol number: 2019/0,056,629), and written informed consent was obtained from participants. The study was performed in accordance with the Declaration of Helsinki.
Clinical assessment
The clinical evaluation was performed in accordance with the CAPSIT-PD protocol31. Levodopa responsiveness was evaluated through an acute levodopa challenge. Hoehn and Yahr scale (H&Y) and the Unified Parkinson’s Disease Rating Scale (UPDRS)32 were applied to quantify disease severity both in the “off-medication” condition (obtained after a 12-h antiparkinsonian medication withdrawal) and “on-medication” condition (obtained after 60 min and the administration of a 30% higher dose of the usual levodopa morning intake)31. Different subscores were extrapolated from the UPDRS including tremor, postural instability/gait disorders (PIGD), akinesia and UPDRS item 18 (speech) subscores. PD motor phenotype (tremor dominant [TD], indeterminate and PIGD)33 was also extrapolated and patients were screened for the presence of mutations in the glucocerebrosidase-1 (GBA-1), leucine-rich repeat kinase-2, α-synuclein and parkin genes34,35. The total amount of dopaminergic medications was calculated as levodopa equivalent daily dose (LEDD) milligrams36. All patients underwent 3-Tesla brain-MRI to evaluate the presence/absence of white matter hyperintensities of vascular origin. All subjects were re-evaluated with a median five-years follow-up (range 3–7 years) after surgery. Neurological evaluation (superimposable with the preoperative one) and the speech assessment were carried out on the same day and in the following conditions: on-stimulation/off-medication (washout of at least 12-h of dopaminergic medications); off-stimulation/off-medication (stimulation was temporarily turned off for at least 1-h); on-stimulation/on-medication (stimulation was turned on and dopaminergic therapy was administered [early morning LEDD plus 30%]). Each patient underwent a complete neuropsychological assessment before surgery and at long-term evaluation, including phonemic fluency, spatial perception (localization of numbers), Raven’s progressive matrices, Stroop test and Trail making test part B.
Speech evaluation
Speech evaluation was performed both preoperatively during the acute levodopa challenge and at postoperative assessment. Each evaluation was carried out in a silent environment with conversation voice intensity and was recorded with a digital voice recorder (model SONY ICDPX240) kept 20 cm from the patient’s lips25. The perceptual-acoustic analysis was performed using Praat software37 and blinded to the patient’s condition. The following tasks were included: word intelligibility (calculated as the percentage of words correctly transcribed by the examiner among a set of 25 recorded words)25; oral diadochokinesis task in which participants produced the syllables /pa/, /ta/, /ka/ and the pseudoword /pataka/, as fast as they could with habitual pitch and loudness (irregular rhythm [presence of absence], uncontrolled acceleration [presence of absence]); sustained production of the phoneme /a/ for as long as possible, performed three times (duration [sec], intensity [dB]); counting from 1 to 20 (speech rate [syllables/second]). Single words intelligibility was selected due to its advantage of eliminating a number of other variables that can affect intelligibility, such as sentence level syntactic and prosodic variables. Furthermore, the use of single words to assess intelligibility is a much less difficult task for dysarthric participants than sentence level productions. As such, if an intelligibility impairment is noted at the single word level, intelligibility deficits are more than likely at higher/more complicated levels of speech productions, such as the sentence level38. A calibration tone (80 SPL dB, 1 kHz) was included at the beginning of each recording to serve as a reference in the determination of speaking amplitude. According to recent guidelines39, these parameters have been selected because they represent acoustic characteristics previously reported as altered in hypokinetic dysarthria23,27. The presence and severity of hypokinetic dysarthria were perceptually determined by two speech language pathologists, both Italian native speakers. Speakers’ severity of dysarthria was categorized on a coarse scale ranging from none, mild, moderate to severe (1: severe, 2: moderate; 3: mild: 4: none)40,41.
Statistical analysis
Descriptive statistics were used for describing demographic and clinical data. The primary objective of the study was to evaluate the long-term effects of bilateral STN-DBS on speech intelligibility in advanced PD patients. As primary outcomes, we selected the change of speech intelligibility between postoperative on-stimulation/off-medication condition and preoperative off-medication condition; postoperative on-stimulation/off-medication and off-stimulation/off-medication condition. Positive changes represented improvement of speech intelligibility while negative changes represented speech worsening. The presence of significant differences in speech intelligibility in the different conditions tested was calculated using the Friedman test with subsequent post-hoc Wilcoxon signed rank test with Bonferroni correction for multiple comparisons because of the use of multiple tests (statistical adjusted significance was set at p-value < 0.005). Based on the presence/absence of long-term postoperative worsening of speech intelligibility, patients were divided into two groups (“stable/imp” [absent or positive variation] and “worsened” [negative variation]) that were compared to find significant differences in demographic, clinical and speech variables. With regards to continuous and ordinal variables, the Mann–Whitney test was used, while for categorical variables the chi-square independence test was applied (statistical significance was set at p-value < 0.05). Secondary outcomes included: the changes of the other speech variables in the different conditions tested; the correlation between the variation of speech intelligibility and the variation in the different motor scores and subscores in the on-stimulation/off-medication condition compared with the off-stimulation/off-medication condition and in the on-stimulation/off-medication compared with preoperative off-medication condition; the correlation between the different motor scores and subscores and speech intelligibility in the postoperative conditions tested. Correlation analyses were performed by using the Spearman Correlation analysis. Statistical analysis was performed using the IBM SPSS Statistics for Windows version 20.0 (IBM, Armonk, NY, USA).
Data availability
Anonymized data of this study may be available from the corresponding author upon request from any qualified researcher, following the EU General Data Protection Regulation.
Change history
17 August 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41598-023-39958-x
References
Cavallieri, F. et al. Predictors of long-term outcome of subthalamic stimulation in Parkinson disease. Ann. Neurol. 89, 587–597 (2021).
Bove, F. et al. Long-term outcomes (15 years) after subthalamic nucleus deep brain stimulation in patients with Parkinson disease. Neurology. https://doi.org/10.1212/WNL.0000000000012246 (2021).
Zampogna, A. et al. Axial impairment and falls in Parkinson’s disease: 15 years of subthalamic deep brain stimulation. NPJ Park Dis. 8, 121 (2022).
Di Rauso, G. et al. Freezing of gait in Parkinson’s disease patients treated with bilateral subthalamic nucleus deep brain stimulation: A long-term overview. Biomedicines 10, 2214 (2022).
Tommasi, G. et al. Pyramidal tract side effects induced by deep brain stimulation of the subthalamic nucleus. J. Neurol. Neurosurg. Psychiatry 79, 813–819 (2008).
Aldridge, D., Theodoros, D., Angwin, A. & Vogel, A. P. Speech outcomes in Parkinson’s disease after subthalamic nucleus deep brain stimulation: A systematic review. Parkinsonism Relat. Disord. 33, 3–11 (2016).
Tripoliti, E. et al. Effects of subthalamic stimulation on speech of consecutive patients with Parkinson disease. Neurology 76, 80–86 (2011).
Brabenec, L., Mekyska, J., Galaz, Z. & Rektorova, I. Speech disorders in Parkinson’s disease: Early diagnostics and effects of medication and brain stimulation. J. Neural Transm. Vienna Austria 2017(124), 303–334 (1996).
Tripoliti, E. et al. Predictive factors of speech intelligibility following subthalamic nucleus stimulation in consecutive patients with Parkinson’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 29, 532–538 (2014).
Pinto, S. et al. Changes induced by levodopa and subthalamic nucleus stimulation on parkinsonian speech. Mov. Disord. Off. J. Mov. Disord. Soc. 20, 1507–1515 (2005).
Pinto, S. et al. Results of a randomized clinical trial of speech after early neurostimulation in Parkinson’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 38, 212 (2022).
Aviles-Olmos, I. et al. Long-term outcome of subthalamic nucleus deep brain stimulation for Parkinson’s disease using an MRI-guided and MRI-verified approach. J. Neurol. Neurosurg. Psychiatry. 85, 1419–1425 (2014).
Fasano, A. et al. Motor and cognitive outcome in patients with Parkinson’s disease 8 years after subthalamic implants. Brain J. Neurol. 133, 2664–2676 (2010).
Svihlik, J. et al. Long-term averaged spectrum descriptors of dysarthria in patients with Parkinson’s disease treated with subthalamic nucleus deep brain stimulation. J. Speech Lang. Hear. Res. 65, 4690–4699 (2022).
Pinto, S. et al. Subthalamic nucleus stimulation and dysarthria in Parkinson’s disease: A PET study. Brain J. Neurol. 127, 602–615 (2004).
Atkinson-Clement, C. et al. Subthalamic nucleus stimulation effects on single and combined task performance in Parkinson’s disease patients: A PET study. Brain Imaging Behav. 11, 1139–1153 (2017).
Pinto, S. et al. Stimulation of the pedunculopontine nucleus area in Parkinson’s disease: Effects on speech and intelligibility. Brain J. Neurol. 137, 2759–2772 (2014).
Tsuboi, T. et al. Distinct phenotypes of speech and voice disorders in Parkinson’s disease after subthalamic nucleus deep brain stimulation. J. Neurol. Neurosurg. Psychiatry. 86, 856–864 (2015).
Tanaka, Y. et al. Longitudinal speech change after subthalamic nucleus deep brain stimulation in Parkinson’s disease patients: A 2-year prospective study. J. Park Dis. 10, 131–140 (2020).
Petrucci, S. et al. GBA-related Parkinson’s disease: Dissection of genotype–phenotype correlates in a large Italian cohort. Mov. Disord. 35, 2106–2111 (2020).
Koss, A. M., Alterman, R. L., Tagliati, M. & Shils, J. L. Calculating total electrical energy delivered by deep brain stimulation systems. Ann. Neurol. 58, 168 (2005).
Skodda, S. et al. Effect of subthalamic stimulation on voice and speech in Parkinson’s disease: For the better or worse? Front. Neurol. 4, 218 (2014).
Rusz, J. et al. Speech disorders reflect differing pathophysiology in Parkinson’s disease, progressive supranuclear palsy and multiple system atrophy. J. Neurol. 262, 992–1001 (2015).
Sung, J. E. et al. Effects of subthalamic nucleus deep brain stimulation on the phonation and articulation of the patients with Parkinson’s disease. J. Korean Neurol. Assoc. 22, 472–477 (2004).
Cavallieri, F. et al. Dopaminergic treatment effects on dysarthric speech: Acoustic analysis in a cohort of patients with advanced Parkinson’s disease. Front. Neurol. 11, 616062 (2020).
Fabbri, M. et al. Speech and voice response to a levodopa challenge in late-stage Parkinson’s disease. Front. Neurol. 8, 432 (2017).
Skodda, S., Visser, W. & Schlegel, U. Short- and long-term dopaminergic effects on dysarthria in early Parkinson’s disease. J. Neural Transm. 117, 197–205 (2010).
Rusz, J. et al. Comparative analysis of speech impairment and upper limb motor dysfunction in Parkinson’s disease. J. Neural Transm. Vienna Austria 2017(124), 463–470 (1996).
Cavallieri, F. et al. A study on the correlations between acoustic speech variables and bradykinesia in advanced Parkinson’s disease. Front. Neurol. 14, 1213772 (2023).
Hughes, A. J., Daniel, S. E., Kilford, L. & Lees, A. J. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: A clinico-pathological study of 100 cases. J. Neurol. Neurosurg. Psychiatry 55, 181–184 (1992).
Defer, G. L., Widner, H., Marié, R. M., Rémy, P. & Levivier, M. Core assessment program for surgical interventional therapies in Parkinson’s disease (CAPSIT-PD). Mov. Disord. Off. J. Mov. Disord. Soc. 14, 572–584 (1999).
Fahn, S., Marsden, C., Calne, D. & Goldstein, M. Recent Developments in Parkinson’s Disease (Macmillan Health Care Information, 1987).
Stebbins, G. T. et al. How to identify tremor dominant and postural instability/gait difficulty groups with the movement disorder society unified Parkinson’s disease rating scale: Comparison with the unified Parkinson’s disease rating scale. Mov. Disord. Off. J. Mov. Disord. Soc. 28, 668–670 (2013).
Grisanti, S. et al. Increased stroke risk in patients with Parkinson’s disease with LRRK2 mutations. Mov. Disord. Off. J. Mov. Disord. Soc. 37, 1117–1118 (2022).
Skrahina, V. et al. The Rostock International Parkinson's Disease (ROPAD) Study: Protocol and Initial Findings. Mov Disord. 36(4), 1005–1010. https://doi.org/10.1002/mds.28416 (2021).
Tomlinson, C. L. et al. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 25, 2649–2653 (2010).
Boersma, P. & Weenink, D. Praat: Doing Phonetics by Computer [Computer Program]. Version 5.3.51. http://www.praat.org/ (Accessed 2 June 2013) (2013).
Schulz, G. et al. Single Word Intelligibility of individuals with Parkinson’s disease in noise: Pre-specified secondary outcome variables from a randomized control trial (RCT) comparing two intensive speech treatments (LSVT LOUD vs LSVT ARTIC). Brain Sci. 11, 857 (2021).
Rusz, J., Tykalova, T., Ramig, L. O. & Tripoliti, E. Guidelines for speech recording and acoustic analyses in dysarthrias of movement disorders. Mov. Disord. 36, 803–814 (2021).
Yorkston, K. M., Miller, R. M. & Strand, E. A. Management of Speech and Swallowing in Degenerative Diseases (Pro-Ed, 2004).
Hartelius, L., Elmberg, M., Holm, R., Lövberg, A.-S. & Nikolaidis, S. Living with dysarthria: Evaluation of a self-report questionnaire. Folia Phoniatr. Logop. 60, 11–19 (2008).
Acknowledgements
This study was partially supported by Italian Ministry of Health – Ricerca Corrente Annual Program 2023. Thanks are also due to Mr. Jovian Salak for the English revision of the manuscript.
Author information
Authors and Affiliations
Contributions
(1) Design of the study; (2) data collection and analysis; (3) Manuscript preparation: A. Writing of the first draft, B. Review and critique. A.G.: 1, 2, 3A; F.C.: 1, 2, 3A; I.C.: 1, 3, 3A; A.M.: 1, 3, 3A; V.Fi.: 1, 2, 3A; G.D.R.: 1, 2, 3A; B.D.: 1, 2, 3A; S.C.: 1, 2, 3A; E.B.: 1, 2, 3A; M.G.C.: 1, 2, 3A; F.A.: 1, 2, 3A; F.Ca.: 1, 2, 3A; M.A.M.: 1, 2, 3A; S.C.: 1, 2, 3A; E.M.: 1, 2, 3A; A.F.: 1, 2, 3A; A.V.: 1, 2, 3A; G.B.: 1, 2, 3B; V.Fr.: 2, 3B; S.P.: 3B; E.M.: 2, 3B; C.B.: 1, 2, 3A, 3B; F.V.: 1, 2, 3A, 3B. All authors. All authors approve the final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The Acknowledgements section in the original version of this Article was incomplete. It now reads: “This study was partially supported by Italian Ministry of Health – Ricerca Corrente Annual Program 2023. Thanks are also due to Mr. Jovian Salak for the English revision of the manuscript.”
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gessani, A., Cavallieri, F., Fioravanti, V. et al. Long-term effects of subthalamic nucleus deep brain stimulation on speech in Parkinson’s disease. Sci Rep 13, 11462 (2023). https://doi.org/10.1038/s41598-023-38555-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-38555-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.