Abstract
High blood pressure is a major risk factor for premature death. Leisure-time physical activities have been recommended to control hypertension. Studies examining how leisure-time physical activity affects blood pressure have found mixed results. We aimed to conduct a systematic review examining the effect of leisure-time physical activity (LTPA) on lowering blood pressure among adults living with hypertension. We searched studies in Embase, Medline/PubMed, Web of Science, Physical Education Index, Scopus and CENTRAL (the Cochrane Library). The primary outcome variables were systolic blood pressure (SBP) and diastolic blood pressure (DBP). This systematic review is registered on PROSPERO (CRD42021260751). We included 17 studies out of 12,046 screened articles in this review. Moderate-intensity LTPA (all types) reduced SBP compared to the non-intervention control group (MD −5.35 mm Hg, 95% CI −8.06 to −2.65, nine trials, n = 531, low certainty of the evidence). Mean DBP was reduced by −4.76 mm Hg (95% CI −8.35 to −1.17, nine trials, n = 531, low certainty of the evidence) in all types of LTPA (moderate intensity) group compared to the non-intervention control group. Leisure-time walking reduced mean SBP by −8.36 mmHg, 95% CI −13.39 to −3.32, three trials, n = 128, low certainty of the evidence). Walking during leisure time reduced −5.03 mmHg mean DBP, 95% CI −8.23 to −1.84, three trials, n = 128, low certainty of the evidence). Performing physical activity during free time probably reduces SBP and DBP (low certainty of the evidence) among adults with hypertension.
Similar content being viewed by others
Introduction
Hypertension is a leading risk factor for premature death worldwide1,2. Thresholds of hypertension differed between American and European guidelines. The threshold value of hypertension according to American guidelines is 130/80 mmHg3, whereas European guidelines defined hypertension when blood pressure is greater than 140/90 mmHg4. High systolic blood pressure (according to American guidelines) was responsible for 10.8 million deaths which was 19% of total deaths globally in 20192. Globally, 1.3 billion people aged 30–79 years old lived with hypertension in 2019 (according to European guidelines). More than 1 billion people worldwide (82% of those with hypertension) live in low and middle-income countries5. Hypertension will affect 1.60 billion people worldwide by 20256. Hypertension has imposed a substantial economic burden, including direct healthcare expenses ($370 billion/year)7 as well as indirect costs associated with lost productivity, premature death, and morbidity8,9.
The reduction of every 10 mm Hg in systolic blood pressure (SBP) and 5 mm Hg in diastolic blood pressure (DBP) could reduce cardiovascular events by a quarter, stroke by a third, and all-cause mortality by 13%10,11,12. Even, a 2 mm SBP drop can have clinically significant impacts on mortality10,11,12,13. People with lower heart rates (70 to < 72 beats/min) show a 50% reduced cardiovascular-related heart mortality and heart failure compared to those with higher heart rates (≥ 87 beats/min)14. Pharmacological treatment is proven to significantly improve the primary prevention of cardiovascular disease mortality and morbidity12,15,16. However, in a pooled analysis of 104 million participants, only 40% of people with hypertension received pharmacological treatment, and 23% of women and 18% of men of the total participants had controlled blood pressure5. Also, poor drug adherence is a major issue to manage hypertension17. Given the above drawbacks to drug adherence, exercise, low salt intake, quitting smoking, and controlling overweight are non-pharmaceutical therapies that can play a substantial role cost-effectively in managing hypertension18,19,20,21,22.
World Health Organization defines physical activity as “any movement of the body involving the skeletal muscles that need energy expenditure”23. Physical activity reduces blood pressure by decreasing sympathetic nerve activity and expanding artery lumen widths, thus lowering peripheral vascular resistance24. Moreover, physical activity can reduce the left ventricular mass index which can reduce blood pressure among people with hypertension24,25. Recent evidence from interventional research has found a strong link between regular physical activity and hypertension control26,27,28,29,30,31. However, some studies found no positive effect32,33. These contradictory findings could be due to interventional differences in the type of physical activity, intensity, adherence to physical activity, and study population. Similarly, meta-analyses that investigated the effect of physical activity in controlling hypertension have shown inconsistent results34,35,36,37. Meta-analyses were performed on studies that included either both normotensive and hypertensive people or limited to a specific age group34; limited to a certain form of physical activity such as walking, low-intensity aerobic exercise35,36; or overall exercise37.
Leisure-time physical activity (LTPA) is defined as “all behaviour related to physical activity that people take in their free time”38. The effects of LTPA in reducing cardiometabolic risk are higher than that of work-related physical activity39. LTPA such as walking, running, bicycling, and soccer are the top most popular physical activities among adults40, and many people can fit them into their daily routine. Findings from randomised controlled trials show that specific types of LTPA, such as walking41, soccer42, and swimming43, can reduce blood pressure. LTPA may be well positioned to promote cardiovascular health, particularly for those with hypertension, as they are popular behaviours that can be easily incorporated into public health messages. However, synthesised findings of the effect of all types of LTPA on blood pressure in only hypertensive people are lacking. Our objective in this study is to investigate the effect of LTPA on blood pressure control in people with hypertension.
Methods
We followed the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) to perform this systematic review44. This study is registered on PROSPERO (CRD42021260751). The protocol of this study has been published in a peer-reviewed journal45.
Search methods
Our expert (KMSUR) on search strategy carried out comprehensive searches in Medline/PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), Embase, Scopus, Web of Science, and Physical Education Index (ProQuest) on September 8, 2021, using the keywords and subject heading terms linked to study inclusion criteria (Suppl Appendix p. 1). We updated the search in all databases on February 14, 2023. We present the search method for databases in Suppl Appendix p. 1. We performed additional searches to identify more relevant articles by checking the reference list of included studies and reviews or systematic review articles we found during searching in databases. If required data was not supplied or full articles were not available, we contacted the corresponding author.
Study selection criteria
We included both interventional and observational studies published since January 1, 2000. We followed the PICOS approach to select studies. We selected studies with only hypertensive people aged 18 and over. Any interventions on LTPA were included. The comparison was non-exercise performing controls (usual activities). The primary outcomes were SBP and DBP as continuous data. The secondary outcome was heart rate (beat per min). Interventions conducted to prevent hypertension were excluded. Details of the study selection criteria are in Appendix p. 6 and our published protocol45.
Study selection
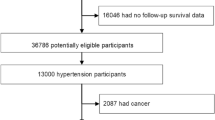
All identified articles were imported into Rayyan (an open-source software)46. Duplicate articles were removed. Two reviewers (AF and MGR) screened all the titles and abstracts independently, and discrepancies were resolved by discussion with a third reviewer (KMSUR). For the final selection of articles, an additional set of team members (MSI and MIS) independently examined the full text. Non-English papers were removed at the full-text assessment stage. The interrater reliability was 94.9% (kappa statistics 0.79) in full-text assessment. We used the prioritisation and sequential exclusion method during the screening of full-text articles47. We have illustrated the study selection process in the PRISMA flow chart (Fig. 1)48.
Process of systematic review (adopted from PRISMA 2020 statement48).
Data extraction
Data extraction forms were developed based on the study population, methods, interventions, and findings on outcome variables. Two separate forms were used for observational and interventional studies. Two reviewers independently retrieved data from the included articles using the forms. Reviewers critically checked data consistency after completing data extraction, and disagreements were resolved through discussion.
Assessment of risk of bias
Using the Joanna Briggs Institute (JBI) critical appraisal tools, two team members (RI and MSI) evaluated the methodological quality of the selected articles independently49. The interrater reliability was 90.9% (kappa statistics 0.75) in risk of bias assessments. The JBI tools for cross-sectional studies, cohort studies, and RCTs were used as appropriate. Any disagreements in this assessment were resolved by a third member (KMSUR).
Data synthesis
Primary analysis
We followed American guidelines (minimum SBP 130 and DBP 80 mm Hg) of hypertension to define a participant as a hypertensive respondent. For our primary comparison, we performed a meta-analysis of all the interventional studies (quasi-experimental studies, randomised controlled trials, crossover trials) that had any type of LTPA interventions with moderate intensity, around 150 min of physical activity weekly, and a non-intervention control group. Moderate-intensity LTPA was considered to perform a meta-analysis as we got sufficient data on that in the included studies. We performed a meta-analysis on the effect of LTPA on SBP, DBP and heart rates. A narrative synthesis was performed for the rest of the included studies. We performed a random-effects model meta-analysis considering the heterogeneity. We also performed subgroup analysis for leisure-time walking intervention studies. The mean difference with the standard error was used in the meta-analysis. We produced a funnel plot and Egger's test to examine publication bias. We used the metaphor package to perform the meta-analysis in R-studio.
Sensitivity analysis
We conducted sensitivity analyses for all outcomes (SBP, DBP, and HR) by removing trials that had unclear random sequence generation and allocation concealment to examine the possible impact of risk of bias on the primary pooled estimates. We also undertook sensitivity analyses by including the crossover trials in the meta-analyses.
Certainty assessment
We followed the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system to evaluate the evidence certainty for the intervention effect50. This integrates data from five main domains: risk of bias evaluation, heterogeneity, indirectness of evidence, the imprecision of findings (95% CI or small size of effect), and potential publication bias. Two reviewers graded the evidence independently as 'high quality', 'moderate', 'low', and 'very low quality'. We lowered the evidence from 'high certainty' by one level for serious constraints or by two levels for very serious study constraints. The overall certainty of the evidence is shown in Table 1.
Role of the funding source
There was no funding for this study.
Results
Results of searches
We identified 12,046 articles in our searches. After methodically screening all the articles, 17 articles were included in this review 41,42,43,51,52,53,54,55,56,57,58,59,60,61,62,63,64 (Fig. 1). Out of the 17 selected articles, 12 were randomised control trials, two were quasi-experimental42,55, and three were cross-sectional studies51,52,64. Details and characteristics of studies are described in Suppl Appendix p.19.
Characteristics of studies and participants
The included studies were conducted in 14 countries. Two studies were from the USA59,62, the UK41,43, and Brazil 42,61 each. Bangladesh64, China51, Hong Kong60, Indonesia55, Japan57, Korea53, Kuwait52, Iran56, Nepal58, New Zealand63, and Sweden54 had one study each. The age range of participants was 18 to 80. Out of 17 articles, 11 studies recruited both women and men respondents, while all participants were women in five studies43,53,56,57,59 and men in one study42.
Intervention details
The types of LTPA in the interventions were walking (five studies)41,42,59,62,63, yoga (two studies)54,58, and one studies each on progressive muscle relaxation exercise55, stair climbing53, circuit training and chair-based exercise57, Quinton treadmill56, beach tennis61, swimming43, and qigong60. We classified walking, yoga, muscle relaxation exercise, stair climbing, moderate-intensity swimming, stair climbing as moderate-intensity exercise, and running, soccer, beach tennis, and high-intensity swimming as high-intensity exercise. The duration of exercise interventions ranged from six days to 26 weeks.
Risk of bias in included studies
Details of the risk of bias have shown graphically in Suppl Appendix p. 16–18.
The total quality scores across all randomised controlled trials (RCT) ranged from 7 to 12 out of 13. The scores of the two selected quasi-experimental studies42,55 were 7 and 5 out of 9. The quality score in the three selected cross-sectional studies was 7 out of 8. The domains of quality assessed were inclusion criteria in the sample, details of study subjects and setting, reliability of exposure measurement, criteria of measurement, identification of confounders, strategies to deal with confounders, way of outcomes measurement, and appropriate statistical analyses. We assessed the reliability of exposure measurement as unclear in both studies. All other criteria were rated as yes in both studies.
Other potential sources of bias
The funnel plots with Egger’s test in both SBP and DBP showed no publication bias (p < 0.05) (Suppl. Appendix p. 15).
Effects of leisure-time physical activity
Primary outcomes
Finding from meta-analysis
Out of the 12 RCTs, we performed a meta-analysis of studies on moderate intensity had a duration of 150 min of physical activity weekly, were not crossover trials and had a non-exercise control group. Nine studies met the inclusion criteria41,43,53,54,56,57,58,59,62.
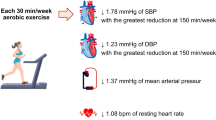
Moderate-intensity LTPA (all types) reduced systolic blood pressure (SBP) compared to the non-intervention control group [mean difference (MD) −5.35 mm Hg, 95% confidence interval (CI) −8.06 to −2.65, P = 0.0001, I2 = 87.9%, nine trials, and n = 531] (Fig. 2A). Sensitivity analysis revealed a little larger effect when we pooled cross-over trials (MD −5.66 mm Hg, 95% CI −7.95 to −3.36, P < 0.0001, I2 = 84.9%, 11 trials, and n = 617) (Suppl Appendix p. 28), while the finding from parallel trials was statistically not significant (Suppl Appendix p. 33). The effect was reduced when we excluded studies with unsure randomization and allocation (MD −4.00 mmHg, 95% CI −7.70 to −0.30, P < 0.034, I2 = 91.2%, 11 trials, and n = 617) (Suppl Appendix p. 31). Subgroup analysis by only leisure-time walking showed a mean SBP reduction of −8.36 mmHg (95% CI −13.39 to −3.32, P = 0.0012, I2 = 87.0%, three trials, and n = 128) (Fig. 2B).
Mean diastolic blood pressure (DBP) reduced by −4.76 mm Hg, (95% CI −8.35 to −1.17, P = 0.0094, I2 = 95.7%, nine trials, and n = 531) in all types of moderate-intensity LTPA group compared to the non-interventions control group, nine studies, n = 531 (Fig. 3A). Sensitivity analysis revealed little difference when we included cross-over trials (MD −4.52 mmHg, 95% CI −7.52 to −1.58, p = 0.002, I2 = 94.2%, 11 trials and n = 617) (Suppl Appendix p. 29) and excluded studies with unsure randomization and allocation (MD −3.49 mmHg, 95% CI −6.43 to −0.54, p = 0.0202, I2 = 90.8%, five trials, and n = 346) (Suppl Appendix p. 32), while the finding from parallel trials was statistically not significant (Suppl Appendix p. 34). Walking during leisure time reduced mean DBP by −5.03 mm Hg, 95% CI −8.23 to −1.84, P = 0.02, I2 = 77.2%, three trials, n = 128) (Fig. 3B).
Overall, the evidence synthesised from the selected shows that moderate-intensity LTPA can reduce both systolic and diastolic blood pressure among adult people living with hypertension, however, the evidence is of low certainty as the GRADE approach (Table 1).
Narrative synthesis
All interventional studies that were not included in the meta-analysis found that LTPA reduced both SBP and DBP significantly42,60,61,63. Cheung et al. (2005) compared the effect of conventional exercise with the effect of qigong in controlling hypertension and found a nonsignificant difference in SBP and DBP60. Nóbrega et al. (2013) compared the effect of walking with the effect of soccer in controlling hypertension and found a nonsignificant difference42. Three included cross-sectional studies also found that people who had a sedentary lifestyle had more likely higher blood pressure. Yang et al. (2019) found that 2 to 4 h of leisure-time daily walking was associated with lower DBP; however, the association was nonsignificant for SBP51. Alsairafi et al. (2010) found people who had to relax/do simple activities had more odds of uncontrolled hypertension than people who had moderate/vigorous activities52. Islam et al. (2023) found people who were involved in recreational sports had −3.9 mmHg lower SBP, however, the finding was not statistically significant64.
Secondary outcomes
Moderate intensity LTPA (all types,) reduced mean heart rate by −2.69 beats/min (95% CI −4.80 to −0.58, p = 0.012, I2 = 66.9%, six trials, n = 256) (Suppl Appendix p. 35). The effect differed little in the sensitivity analysis. When we included cross-over trials, mean heart rate reduction was −2.94 (95% CI −4.76 to −1.13, p = 0.0015, I2 = 62.9%, seven trials and n = 318). The reduction of health rate was −1.94 (95% CI −3.38 to −0.49, p = 0.0085, I2 = 0%, two trials and n = 71) when we excluded unsure randomization and allocation studies (Suppl Appendix p. 33).
Additional findings
Three studies examined the effect of LTPA in controlling mean atrial pressure43,55,56. Two studies reported that mean atrial pressure was reduced significantly55,56, while a study found that leisure-time swimming had an insignificant effect in controlling mean atrial pressure43.
Discussion
The results of this meta-analysis of nine randomised controlled trials (531 people with hypertension) showed that moderate-intensity leisure-time physical activity significantly reduced blood pressure (both systolic and diastolic blood pressure) compared with non-intervention control (usual activities). The effect of LTPA exists even after undertaking sensitivity analyses excluding studies with unclear randomisation and allocation bias. LTPA also reduced heart rate. Furthermore, we found that leisure-time walking also has blood pressure and heart rate-lowering effects. Overall high-intensity physical activity (high-intensity group56 and soccer group42) reduced higher SBP than lower/moderate intensity physical activity (lower intensity group56 and walking group42). We found the amount of blood pressure (in mmHg) reduction was not dependent on the length of intervention. A short-term (10 days) intervention, brisk walking reduced −11.2 mmHg SBP63, while a long-term (26 weeks) intervention, walking reduced −8.5 mmHg SBP62.
Physical activity has been shown to improve a variety of biological processes related to reducing cardiovascular risk. Physical activity lowers blood pressure by reducing sympathetic nerve activity among people with hypertension65. It reduces the release of norepinephrine mediating vasoconstriction66, which in turn reduces vascular resistance. Physical activity increases insulin sensitivity and can reduce insulin-medicated sympathetic activity65. Physical activity reduces vascular responsiveness to endothelin-1, another vasoconstrictor among people with hypertension67. Physical activity also increases endothelial-dependent medicated vasodilation by enhancing nitric oxide production, and acetylcholine infusion. Physical activity causes vascular remodelling68,69. Vascular remodelling includes new arteries, increase cross-sectional area and enhancement of the diameter of existing veins and arteries. All of this vascular re-structure reduce peripheral resistance70. LTPA reduces heart rate. Bahrainy et al. reported the mechanism of physical activity and exercise to reduce heart rate is unclear71. They found an increase in parasympathetic tone or a reduction in beta-adrenergic stimulation due to physical activity does not reduce heart rate72. Tyagi et al. reported that an increased parasympathetic output can reduce heart rate after yoga73.
Our findings show that leisure-time physical activity reduced both SBP and DBP. The GRADE assessment shows the evidence has low certainty due to high heterogeneity among the RCTs and imprecision. The possible reason for heterogeneity is the type of LTPA, geographic location and sex of the participants. Subgroup analyses on geographic location and sex showed no to minimum heterogeneity (data not shown). The latitude, ambient temperature and solar radiation vary in geographic location. The effect of those factors on blood pressure can produce a heterogeneous response to LTPA74. Gender differences in LTPA on blood pressure can be due to differences in the metaboreflex, in insular gyral response, and in hormones (e.g. estrogen)75,76. The cause of the heterogenous effect of LTPA types on blood pressure is needed to explore. The included articles for meta-analysis did not classify the effect of LTPA on blood pressure based on the common effect modifiers for hypertension and LTPA, such as age, sex, body mass index, and socio-economic status. However, included articles considered those factors as confounders during analysis41,54,57,58,59,62.
A previous study reported that lowering blood pressure is associated with decreased mortality from cardiovascular diseases. A reduction of 2 mm Hg in SBP is associated with a 10% reduction in stroke mortality and a 7% reduction in vascular risk mortality13. We reported that moderate-intensity LTPA could reduce SBP MD by −5.35 mm Hg (95% CI: −8.06 to −2.65), which is a considerably greater magnitude than the 2 mm Hg reduction13. The findings thus can be considered clinically significant. It indicates that LTPA could serve as an effective and beneficial complement to or alternative to pharmacological treatment for lowering blood pressure in people with hypertension. The effect of physical activity does not sustain for the long term77, indicating the importance of regular physical activity. It is recommended that 150 min of physical activity a week78. We performed this meta-analysis of the intervention which examined physical activity length of 150 min per week. The finding of this study can be used to make LTPA recommendations for people with hypertension.
To the best of our knowledge, this is the first study that examines the effect of LTPA in lowering blood pressure among people with hypertension. However, a large number of systematic reviews and meta-analyses have investigated the effect of physical activity in reducing blood pressure34,35,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95. Our review, like other systematic reviews, identifies a diverse group of physical activity interventions that differ in terms of participant willingness and intensity. For instance, aerobic exercise reduced both SBP (− 5.4 mm Hg) and DBP (− 3 mm Hg) among people with hypertension37. Another meta-analysis found moderate-intensity continuous training reduced SBP by 3.7 mm Hg and DBP by 2.41 mm Hg among people with hypertension91. Agreeing with another meta-analysis, this study suggests that LTPA reduces both SBP and DBP. We found walking also reduces SBP and DBP. The finding is coherent with the result of a Cochrane review36.
Policy and practice implications
The findings of this study could be used to improve strategies and guidelines to recommend LTPA to reduce hypertension. The number of people with hypertension increased due to a recent change of practice guidelines designed by the American Heart Association96,97. Our findings from up-to-date evidence support the findings of the previous studies to offer LTPA as a treatment option, aside from the fact that the studies included in this meta-analysis did not directly evaluate the effects of exercise vs medicines87,98,99. As the findings are based on recreational activities among people living with hypertension, this nonpharmacological treatment option could increase adherence to continuing treatment among people with hypertension. This finding can be used to drive evidence-based conversations between patients and their clinicians regarding the benefits of exercise in decreasing blood pressure. This nonpharmacological intervention will reduce the treatment cost of hypertension, especially in countries that have limited resources and a shortage of medical services.
Research implications
Studies conducted on a large number of people with hypertension are rare. Addressing this gap, the findings of this review will provide ethical justification to investigate the effectiveness of LTPA in reducing blood pressure among people living with hypertension. There is also a scope for future research to explore the barriers and facilitators of adherence to leisure-time physical activity among people with hypertension. In our included studies, Cheung et al. (2005)60 compared the effect of conventional exercise with the effect of qigong, and Nóbrega et al. (2013)42 compared the effect of walking with the effect of soccer in controlling hypertension. Both found LTPA reduced SBP and DBP; however, the mean difference was nonsignificant among the two comparison groups. It indicates the magnitude of the effectiveness of LTPA in controlling blood pressure varies little among the different types of LIPA. However, more evidence is needed to examine the effect difference by comparing different types of LTPA further.
Strength and limitation
This systematic review and meta-analysis have several strengths. First, we have followed the standard robust method of conducting a systematic review and meta-analysis. We have performed meta-analysis only on randomised controlled trials, the gold standard for answering research questions.
This systematic review and meta-analysis has several limitations. The first limitation is that a good number of studies did not mention about randomisation process. We assessed the impact of unclear randomisation by performing a sensitivity analysis excluding studies that had unclear randomisation. We found a significant reduction of both SBP and DBP in the sensitivity analysis. Another limitation of this systematic review is that our search terms regarding leisure time (terms used in #1) were narrow. However, we have added a comprehensive list of LTPA in search term #2. It offsets the narrower strategy regarding the search term leisure time. The included studies in this meta-analysis had high heterogeneity. We performed a random effect model to address this potential limitation. We considered all types of LTPA together in meta-analysis. However, we have conducted several subgroup analyses and sensitivity analyses to overcome this. We included only articles published in the English language and removed five non-English articles during the full-text assessment. Finally, the small sample size of the majority included studies reduced the accuracy of the effect estimate.
Conclusion
Moderate-intensity leisure-time physical activity may reduce both systolic and diastolic blood pressure (low certainty of the evidence) among people with hypertension. Moderate-intensity physical activity during recreational time can be promoted among people with high blood pressure to lower blood pressure. However, more studies are required to understand the effect difference among various types of LTPA in controlling blood pressure.
Data availability
We shared most of our data as an appendix. If further data is required, it is possible to share on request with the corresponding author, KM Saif-Ur-Rahman.
References
WHO. Hypertension. https://www.who.int/news-room/fact-sheets/detail/hypertension (2023).
Murray, C. J. L. et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1223–1249. https://doi.org/10.1016/S0140-6736(20)30752-2 (2020).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 71, e127–e248 (2018).
Williams, B. et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 39, 3021–3104. https://doi.org/10.1093/eurheartj/ehy339 (2018).
Zhou, B. et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 398, 957–980. https://doi.org/10.1016/S0140-6736(21)01330-1 (2021).
Kearney, P. M. et al. Global burden of hypertension: Analysis of worldwide data. Lancet 365, 217–223. https://doi.org/10.1016/S0140-6736(05)17741-1 (2005).
Frieden, T. R. & Jaffe, M. G. Saving 100 million lives by improving global treatment of hypertension and reducing cardiovascular disease risk factors. J. Clin. Hypertens. 20, 208–208. https://doi.org/10.1111/jch.13195 (2018).
Mills, K. T., Stefanescu, A. & He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 16, 223–237. https://doi.org/10.1038/s41581-019-0244-2 (2020).
Gaziano, T. A., Bitton, A., Anand, S., Weinstein, M. C., Hypertension, f. t. I. S. o. The global cost of nonoptimal blood pressure. J. Hypertens. https://doi.org/10.1097/HJH.0b013e32832a9ba3 (2009).
Rahimi, K. et al. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: An individual participant-level data meta-analysis. Lancet 397, 1625–1636. https://doi.org/10.1016/S0140-6736(21)00590-0 (2021).
Law, M. R., Morris, J. K. & Wald, N. J. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ https://doi.org/10.1136/bmj.b1665 (2009).
Ettehad, D. et al. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet 387, 957–967. https://doi.org/10.1016/S0140-6736(15)01225-8 (2016).
Collaboration Prospective Studies. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913. https://doi.org/10.1016/S0140-6736(02)11911-8 (2002).
Bohm, M. et al. Heart rate as a risk factor in chronic heart failure (SHIFT): The association between heart rate and outcomes in a randomised placebo-controlled trial. Lancet 376, 886–894. https://doi.org/10.1016/S0140-6736(10)61259-7 (2010).
Musini, V. M., Tejani, A. M., Bassett, K., Puil, L. & Wright, J. M. Pharmacotherapy for hypertension in adults 60 years or older. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD000028.pub3 (2019).
Li, Q. et al. Effect and safety of LCZ696 in the treatment of hypertension: A meta-analysis of 9 RCT studies. Medicine https://doi.org/10.1097/MD.0000000000016093 (2019).
Burnier, M. Drug adherence in hypertension. Pharmacol. Res. 125, 142–149. https://doi.org/10.1016/j.phrs.2017.08.015 (2017).
Fu, J. et al. Nonpharmacologic interventions for reducing blood pressure in adults with prehypertension to established hypertension. J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.120.016804 (2020).
Saif-Ur-Rahman, K. M. et al. Nonpharmacological interventions for the prevention of hypertension in low- and middle-income countries: A systematic review and meta-analysis. J. Hum. Hypertens. https://doi.org/10.1038/s41371-019-0223-x (2019).
Gupta, R. & Guptha, S. Strategies for initial management of hypertension. Indian J. Med. Res. 132, 531–542 (2010).
Akonobi, A. & Khan, J. A systematic review of randomized controlled trials about some non-pharmacological interventions for treatment of hypertension: Physical exercise, sodium restriction, weight and alcohol use reduction. J. Health Soc. Sci. https://doi.org/10.19204/2019/syst4 (2019).
Abolhosseini, H. et al. The effect of improving dietary habits derived from Persian medicine on blood pressure in adults with pre-hypertension: A randomized controlled clinical trial. J. Complement. Med. Res. 12, 91–91 (2021).
WHO. Physical Activity Fact Sheet. (2021).
Hamer, M. The anti-hypertensive effects of exercise. Sports Med. 36, 109–116. https://doi.org/10.2165/00007256-200636020-00002 (2006).
Pitsavos, C. et al. The impact of moderate aerobic physical training on left ventricular mass, exercise capacity and blood pressure response during treadmill testing in borderline and mildly hypertensive males. Hellenic J. Cardiol. 52, 6–14 (2011).
Arija, V. et al. Physical activity, cardiovascular health, quality of life and blood pressure control in hypertensive subjects: Randomized clinical trial. Health Qual. Life Outcomes 16, 184–184. https://doi.org/10.1186/s12955-018-1008-6 (2018).
Medina, C. et al. Occupational and leisure time physical inactivity and the risk of type II diabetes and hypertension among Mexican adults: A prospective cohort study. Sci. Rep. 8, 5399–5399. https://doi.org/10.1038/s41598-018-23553-6 (2018).
Lamina, S., Okoye, C. G. & Hanif, S. M. Randomised controlled trial: Effects of aerobic exercise training programme on indices of adiposity and metabolic markers in hypertension. JPMA J. Pak. Med. Assoc. 63, 680–687 (2013).
Byambasukh, O., Snieder, H. & Corpeleijn, E. Relation between leisure time, commuting, and occupational physical activity with blood pressure in 125 402 adults: The lifelines cohort. J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.119.014313 (2020).
Herrod, P. J. J., Lund, J. N. & Phillips, B. E. Time-efficient physical activity interventions to reduce blood pressure in older adults: A randomised controlled trial. Age Ageing 50, 980–984. https://doi.org/10.1093/ageing/afaa211 (2021).
Mattila, R., Malmivaara, A., Kastarinen, M., Kivelä, S. L. & Nissinen, A. Effectiveness of multidisciplinary lifestyle intervention for hypertension: A randomised controlled trial. J. Hum. Hypertens. 17, 199–205. https://doi.org/10.1038/sj.jhh.1001531 (2003).
Liira, H. et al. Exercise intervention and health checks for middle-aged men with elevated cardiovascular risk: A randomized controlled trial. Scand. J. Prim. Health Care 32, 156–162. https://doi.org/10.3109/02813432.2014.984967 (2014).
Lawton, B. A. et al. Exercise on prescription for women aged 40–74 recruited through primary care: Two year randomised controlled trial. BMJ https://doi.org/10.1136/bmj.a2509 (2008).
Sardeli, A. V., Griffth, G. J., Dos Santos, M. V. M. A., Ito, M. S. R. & Chacon-Mikahil, M. P. T. The effects of exercise training on hypertensive older adults: An umbrella meta-analysis. Hypertens. Res. 44, 1434–1443. https://doi.org/10.1038/s41440-021-00715-0 (2021).
Shao, B.-Y. et al. The effectiveness of Baduanjin exercise for hypertension: A systematic review and meta-analysis of randomized controlled trials. BMC Complement. Med. Ther. 20, 1–12. https://doi.org/10.1186/s12906-020-03098-w (2020).
Lee, L.-L. et al. Walking for hypertension. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD008823.pub2 (2021).
Saco-Ledo, G., Valenzuela, P. L., Ruiz-Hurtado, G., Ruilope, L. M. & Lucia, A. Exercise reduces ambulatory blood pressure in patients with hypertension: A systematic review and meta-analysis of randomized controlled trials. J. Am. Heart Assoc. 9, e018487–e018487. https://doi.org/10.1161/JAHA.120.018487 (2020).
Moore, S. C. et al. Leisure time physical activity of moderate to vigorous intensity and mortality: A large pooled cohort analysis. PLoS Med. 9, e1001335. https://doi.org/10.1371/journal.pmed.1001335 (2012).
Feig, E. H. et al. Association of work-related and leisure-time physical activity with workplace food purchases, dietary quality, and health of hospital employees. BMC Public Health 19, 1–10. https://doi.org/10.1186/s12889-019-7944-1 (2019).
Hulteen, R. M. et al. Global participation in sport and leisure-time physical activities: A systematic review and meta-analysis. Prev. Med. 95, 14–25 (2017).
Cooper, A. R., Moore, L. A. R., McKenna, J. & Riddoch, C. J. What is the magnitude of blood pressure response to a programme of moderate intensity exercise? Randomised controlled trial among sedentary adults with unmedicated hypertension. Br. J. Gen. Pract. 50, 958 (2000).
Da Nóbrega, T. K. S. et al. Walking/running or a recreative soccer game presents similar effectiveness in inducing post-exercise hypotension. Rev. Bras. Med. Esporte https://doi.org/10.1590/S1517-86922013000100006 (2013).
Mohr, M. et al. High-Intensity intermittent swimming improves cardiovascular health status for women with mild hypertension. BioMed Res. Int. https://doi.org/10.1155/2014/728289 (2014).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71–n71. https://doi.org/10.1136/bmj.n71 (2021).
Shariful Islam, M., Rabbani, M. G., Fardousi, A., Sizear, M. I. & Saif-Ur-Rahman, K. M. Effect of leisure-time physical activity in controlling hypertension: a systematic review and meta-analysis protocol. BMJ Open 11(12), e056270. https://doi.org/10.1136/bmjopen-2021-056270 (2022).
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4 (2016).
Saif-Ur-Rahman, K. M. et al. Prioritization and sequential exclusion of articles in systematic reviews. Campbell Syst. Rev. https://doi.org/10.1002/cl2.1229 (2022).
Rethlefsen, M. L. et al. PRISMA-S Group. PRISMA-S: An extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst Rev. 10(1), 39. https://doi.org/10.1186/s13643-020-01542-z (2021).
Porritt, K., Gomersall, J. & Lockwood, C. JBI’s systematic reviews: Study selection and critical appraisal. AJN Am. J. Nurs. 114, 47–52. https://doi.org/10.1097/01.NAJ.0000450430.97383.64 (2014).
Guyatt, G. et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 64, 383–394. https://doi.org/10.1016/j.jclinepi.2010.04.026 (2011).
Yang, R., Liu, Y., Wang, H. & Du, Y. Leisure-time daily walking and blood pressure among Chinese older adults: Evidence from the China health and retirement longitudinal study (CHARLS). Res. Gerontol. Nurs. https://doi.org/10.3928/19404921-20190702-01 (2019).
Alsairafi, M., Alshamali, K. & Al-Rashed, A. Effect of physical activity on controlling blood pressure among hypertensive patients from Mishref area of Kuwait. Eur. J. Gen. Med https://doi.org/10.29333/ejgm/82889 (2010).
Wong, A., Figueroa, A., Son, W. M., Chernykh, O. & Park, S. Y. The effects of stair climbing on arterial stiffness, blood pressure, and leg strength in postmenopausal women with stage 2 hypertension. Menopause https://doi.org/10.1097/GME.0000000000001072 (2018).
Wolff, M. et al. Impact of a short home-based yoga programme on blood pressure in patients with hypertension: A randomized controlled trial in primary care. J. Hum. Hypertens. https://doi.org/10.1038/jhh.2015.123 (2016).
Sulaeman, R., Purnamawati, D., Wijayanti, I. G. & Muhasidah, A. P. W. How progressive muscle relaxation exercise affects patient with hypertension?. Rawal Med. J. 45, 13 (2020).
Shakoor, E., Salesi, M., Daryanoosh, F. & Izadpanah, P. Effect of acute high-intensity interval training and isometric handgrip exercise on hemodynamic responses in hypertensive women. Women’s Health Bull. 7, 60 (2020).
Miura, H., Takahashi, Y., Maki, Y. & Sugino, M. Effects of exercise training on arterial stiffness in older hypertensive females. Eur. J. Appl. Physiol. https://doi.org/10.1007/s00421-015-3168-y (2015).
Khadka, R., Paudel, B. H., Sharma, V. P., Kumar, S. & Bhattacharya, N. Effect of yoga on cardiovascular autonomic reactivity in essential hypertensive patients. Health Renaissance https://doi.org/10.3126/hren.v8i2.4421 (2010).
Moreau, K. L. et al. Increasing daily walking lowers blood pressure in postmenopausal women. Med. Sci. Sports Exerc. https://doi.org/10.1097/00005768-200111000-00005 (2001).
Cheung, B. M. Y. et al. Randomised controlled trial of qigong in the treatment of mild essential hypertension. J. Hum. Hypertens. https://doi.org/10.1038/sj.jhh.1001884 (2005).
Carpes, L., Jacobsen, A., Domingues, L., Jung, N. & Ferrari, R. Recreational beach tennis reduces 24-h blood pressure in adults with hypertension: A randomized crossover trial. Eur. J. Appl. Physiol. https://doi.org/10.1007/s00421-021-04617-4 (2021).
Sohn, A. J., Hasnain, M. & Sinacore, J. M. Impact of exercise (walking) on blood pressure levels in African American adults with newly diagnosed hypertension. Ethnic. Dis. 17, 503 (2007).
Scott, A. R. et al. First national audit of the outcomes of care in young people with diabetes in New Zealand: High prevalence of nephropathy in Māori and Pacific Islanders. N. Z. Med. J. 119, U2015 (2006).
Islam, F. M. A. et al. Associations of physical activity levels, and attitudes towards physical activity with blood pressure among adults with high blood pressure in Bangladesh. PLoS ONE 18, e0280879. https://doi.org/10.1371/journal.pone.0280879 (2023).
Pescatello, L. S. et al. Exercise and hypertension. Med. Sci. Sports Exerc. 36, 533–553. https://doi.org/10.1249/01.Mss.0000115224.88514.3a (2004).
Brown, M. D., Dengel, D. R., Hogikyan, R. V. & Supiano, M. A. Sympathetic activity and the heterogenous blood pressure response to exercise training in hypertensives. J. Appl. Physiol. 1985(92), 1434–1442. https://doi.org/10.1152/japplphysiol.00477.2001 (2002).
Maeda, S. et al. Effects of exercise training of 8 weeks and detraining on plasma levels of endothelium-derived factors, endothelin-1 and nitric oxide, in healthy young humans. Life Sci. 69, 1005–1016. https://doi.org/10.1016/s0024-3205(01)01192-4 (2001).
Kingwell, B. A., Tran, B., Cameron, J. D., Jennings, G. L. & Dart, A. M. Enhanced vasodilation to acetylcholine in athletes is associated with lower plasma cholesterol. Am. J. Physiol. 270, H2008-2013. https://doi.org/10.1152/ajpheart.1996.270.6.H2008 (1996).
Higashi, Y. et al. Regular aerobic exercise augments endothelium-dependent vascular relaxation in normotensive as well as hypertensive subjects: Role of endothelium-derived nitric oxide. Circulation 100, 1194–1202. https://doi.org/10.1161/01.cir.100.11.1194 (1999).
Laughlin, M. H., Korthuis, R. J., Duncker, D. J. & Bache, R. J. Control of blood flow to cardiac and skeletal muscle during exercise. Comprehens. Physiol. 3, 705–769 (2010).
Bahrainy, S., Levy, W. C., Busey, J. M., Caldwell, J. H. & Stratton, J. R. Exercise training bradycardia is largely explained by reduced intrinsic heart rate. Int. J. Cardiol. 222, 213–216. https://doi.org/10.1016/j.ijcard.2016.07.203 (2016).
Reimers, A. K., Knapp, G. & Reimers, C.-D. Effects of exercise on the resting heart rate: A systematic review and meta-analysis of interventional studies. J. Clin. Med. 7, 503 (2018).
Tyagi, A. & Cohen, M. Yoga and heart rate variability: A comprehensive review of the literature. Int. J. Yoga 9, 97–113. https://doi.org/10.4103/0973-6131.183712 (2016).
Cabrera, S. E., Mindell, J. S., Toledo, M., Alvo, M. & Ferro, C. J. Associations of blood pressure with geographical latitude, solar radiation, and ambient temperature: Results from the Chilean Health Survey, 2009–2010. Am. J. Epidemiol. 183, 1071–1073. https://doi.org/10.1093/aje/kww037 (2016).
Ettinger, S. M. et al. Influences of gender on sympathetic nerve responses to static exercise. J. Appl. Physiol. 1985(80), 245–251. https://doi.org/10.1152/jappl.1996.80.1.245 (1996).
Bassareo, P. P. & Crisafulli, A. Gender differences in hemodynamic regulation and cardiovascular adaptations to dynamic exercise. Curr. Cardiol. Rev. 16, 65–72. https://doi.org/10.2174/1573403x15666190321141856 (2020).
Mayo Clinic Staff. Exercise: A Drug-Free Approach to Lowering High Blood Pressure. https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/high-blood-pressure/art-20045206 (2022).
CDC. How Much Physical Activity Do Adults Need? https://www.cdc.gov/physicalactivity/basics/adults/index.htm (2022).
Cornelissen, V. A. & Smart, N. A. Exercise training for blood pressure: A systematic review and meta-analysis. J. Am. Heart Assoc. 2, e004473–e004473. https://doi.org/10.1161/JAHA.112.004473 (2013).
Hanson, S. & Jones, A. Is there evidence that walking groups have health benefits? A systematic review and meta-analysis. Br. J. Sports Med. 49, 710–715. https://doi.org/10.1136/bjsports-2014-094157 (2015).
Inder, J. D. et al. Isometric exercise training for blood pressure management: A systematic review and meta-analysis to optimize benefit. Hypertens. Res. 39, 88–94. https://doi.org/10.1038/hr.2015.111 (2016).
Casonatto, J., Goessler, K. F., Cornelissen, V. A., Cardoso, J. R. & Polito, M. D. The blood pressure-lowering effect of a single bout of resistance exercise: A systematic review and meta-analysis of randomised controlled trials. Eur. J. Prev. Cardiol. 23, 1700–1714. https://doi.org/10.1177/2047487316664147 (2016).
Zhu, Z. et al. Association between exercise and blood pressure in hypertensive residents: A meta-analysis. Evid.-Based Complement. Altern. Med. https://doi.org/10.1155/2022/2453805 (2022).
Pescatello, L. S. et al. Physical activity to prevent and treat hypertension: A systematic review. Med. Sci. Sports Exerc. 51, 1314–1323. https://doi.org/10.1249/MSS.0000000000001943 (2019).
Semlitsch, T. et al. Increasing physical activity for the treatment of hypertension: A systematic review and meta-analysis. Sports Med. 43, 1009–1023. https://doi.org/10.1007/s40279-013-0065-6 (2013).
Liu, X. et al. Dose-response association between physical activity and incident hypertension: A systematic review and meta-analysis of cohort studies. Hypertension 69, 813–820. https://doi.org/10.1161/HYPERTENSIONAHA.116.08994 (2017).
Naci, H. et al. How does exercise treatment compare with antihypertensive medications? A network meta-analysis of 391 randomised controlled trials assessing exercise and medication effects on systolic blood pressure. Br. J. Sports Med. 53, 859–869. https://doi.org/10.1136/bjsports-2018-099921 (2019).
Igarashi, Y. & Nogami, Y. The effect of regular aquatic exercise on blood pressure: A meta-analysis of randomized controlled trials. Eur. J. Prev. Cardiol. 25, 190–199. https://doi.org/10.1177/2047487317731164 (2018).
Cao, L. et al. The effectiveness of aerobic exercise for hypertensive population: A systematic review and meta-analysis. J. Clin. Hypertens. 21, 868–876. https://doi.org/10.1111/jch.13583 (2019).
Zhong, D. et al. Tai chi for essential hypertension: A systematic review of randomized controlled trials. Curr. Hypertens. Rep. 22, 1–12. https://doi.org/10.1007/s11906-020-1031-y (2020).
Leal, J. M., Galliano, L. M. & Del Vecchio, F. B. Effectiveness of high-intensity interval training versus moderate-intensity continuous training in hypertensive patients: A systematic review and meta-analysis. Curr. Hypertens. Rep. 22, 1–13. https://doi.org/10.1007/s11906-020-1030-z (2020).
Igarashi, Y. & Nogami, Y. Running to lower resting blood pressure: A systematic review and meta-analysis. Sports Med. 50, 531–541. https://doi.org/10.1007/s40279-019-01209-3 (2020).
Williamson, W. et al. Will exercise advice be sufficient for treatment of young adults with prehypertension and hypertension? A systematic review and meta-analysis. Hypertension 68, 78–87 (2016).
Albanaqi, A. L., Rahimi, G. R. M. & Smart, N. A. Exercise training for pulmonary hypertension: A systematic review and meta-analysis of randomized controlled trials. Biol. Res. Nurs. 23, 442–454. https://doi.org/10.1016/j.ijcard.2014.10.161 (2021).
Börjesson, M., Onerup, A., Lundqvist, S. & Dahlöf, B. Physical activity and exercise lower blood pressure in individuals with hypertension: Narrative review of 27 RCTs. Br. J. Sports Med. 50, 356–361. https://doi.org/10.1136/bjsports-2015-095786 (2016).
Khera, R. et al. Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: Nationally representative cross sectional study. BMJ https://doi.org/10.1136/bmj.k2357 (2018).
Muntner, P. et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation 137, 109–118. https://doi.org/10.1161/CIRCULATIONAHA.117.032582 (2018).
Pedersen, B. K. & Saltin, B. Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 25, 1–72. https://doi.org/10.1111/sms.12581 (2015).
Pedersen, B. K. & Saltin, B. Evidence for prescribing exercise as therapy in chronic disease. Scand. J. Med. Sci. Sports 16, 3–63. https://doi.org/10.1111/j.1600-0838.2006.00520.x (2006).
Acknowledgements
We would like to thank the current funders, which include the governments of Bangladesh, Canada, Sweden, and the United Kingdom, for their unrestricted support to icddr,b. We are grateful to these funders for their generosity and dedication to icddr,b's endeavours. We also like to acknowledge Safwan Shihab, a research assistant at icddr,b who supported us during the meta-analysis, and James Fowler, a research assistant at The University of Queensland, Australia who proofread the manuscript.
Author information
Authors and Affiliations
Contributions
K.M.S.-U.-R. and M.S.I. conceptualised the study. K.M.S.-U.-R. and M.S.I. searched the studies. A.F. and M.G.R. performed title and abstract screening. M.S.I. and M.M.I.S. conducted the full-text assessment. M.S.I. and R.I. conducted a risk of bias assessment. A.F. and M.M.I.S. performed data extraction. M.S.I. performed the meta-analysis. M.S.I. drafted the manuscript. K.M.S.-U.-R. resolved the conflicted decision during screening and supervised the steps of systematic review and meta-analysis. All authors had access to study data. K.M.S.-U.-R. critically reviewed the manuscript. All authors revised and commented on the draft manuscript and approved the final version of the manuscript for publication. K.M.S.-U.-R. is the guarantor of the systematic review.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shariful Islam, M., Fardousi, A., Sizear, M.I. et al. Effect of leisure-time physical activity on blood pressure in people with hypertension: a systematic review and meta-analysis. Sci Rep 13, 10639 (2023). https://doi.org/10.1038/s41598-023-37149-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-37149-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.