Abstract
COVID-19 has had devastating effects on health systems but reports from sub-Saharan Africa are few. We compared inpatient admissions, diagnostic tests performed, clinical characteristics and inpatient mortality before and during the COVID-19 pandemic at an urban tertiary facility in Uganda. We conducted a retrospective chart review of patients admitted at Kiruddu National Referral Hospital in Uganda between January–July 2019 (before the pandemic) and January–July 2020 (during the pandemic). Of 3749 inpatients, 2014 (53.7%) were female, and 1582 (42.2%) had HIV. There was a 6.1% decline in admissions from 1932 in 2019 to 1817 in 2020. There were significantly fewer diagnostic tests performed in 2020 for malaria, tuberculosis, and diabetes. Overall, 649 (17.3%) patients died. Patients admitted during the COVID-19 pandemic (adjusted odds ratio [aOR] 1.2, 95% confidence interval [CI] 1.04–1.5, p = 0.018), patients aged ≥ 60 years (aOR 1.6, 95% CI 1.2–2.1, p = 0.001), HIV co-infected (aOR 1.5, 95% CI 1.2–1.9, p < 0.001), and those admitted as referrals (aOR 1.5, 95% CI 1.2–1.9, p < 0.001) had higher odds of dying. The COVID-19 pandemic disrupted inpatient service utilization and was associated with inpatient mortality. Policy makers need to build resilience in health systems in Africa to cope with future pandemics.
Similar content being viewed by others
Introduction
The corona virus of 2019 (COVID-19) has been the leading cause of death from an infectious agent since 2020. The lockdowns that were instituted also had a devastating impact on health care provision. As of 1st June 2022 there have been more than 527 million confirmed cases and 6.2 million deaths globally1. Nationwide and local social lockdowns, where persons are required to stay indoors to avoid inter-personal contact outside one’s family members, were instituted in several countries in a bid to prevent the spread of the disease2. During such lockdowns, public assembly was restricted and movement of the public was prohibited2. However, lockdown measures had the potential to affect access and utilisation of health services and result in a reduction child vaccination coverage3, an increase in maternal and child mortality4 and a rise malaria-related deaths5. Among people living with HIV (PLHIV), modelling showed that a 6-months interruption in antiretroviral therapy (ART) supply would result in a twofold rise in HIV-related deaths and maternal-to-child HIV transmission in sub-Saharan Africa6.
The overall utilisation of health services also suffered during the pandemic. A recent systematic review showed that the COVID-19 pandemic resulted in a 37% reduction in health service utilisation, including patient visits (42% reduction), admissions (28%), diagnostics (31%), and therapeutics (30%)7. However, there was no representation of studies from Africa in the systematic review. A study from Ethiopia reported an increase in childhood malnutrition and declines in detection of new HIV cases, cardiovascular disease diagnosis, cervical cancer screening and blood bank services8. Other studies from Africa suggest that the COVID-19 related lockdowns had negative effects on malaria, tuberculosis, HIV, reproductive health, and maternal-child health services and clinic appointments for chronic disease care9. There are few reports on the effect of the COVID-19 pandemic and its associated lockdowns on inpatient mortality in Africa.
In March 2020, Uganda instituted a nationwide lockdown that progressively banned private and public transport except for essential services and cargo10. Initial reports indicated a reduction in new HIV and malaria cases detected, fewer people were initiated on TB preventive therapy, there was a reduction in facility maternal deliveries and an increase in maternal mortality11. However, all-cause mortality at health facilities was reportedly level between 2019 (before the pandemic) and 2020 (early periods of the pandemic), although the data were drawn from health management information systems that had relatively low reporting rates12. In this study, the objective was to compare inpatient attendance, imaging and laboratory services accessed by inpatients, patient characteristics and inpatient mortality before and during the COVID -19 pandemic at an urban tertiary facility in Uganda.
Materials and methods
Study design, settings, and population
This was a retrospective longitudinal study conducted at Kiruddu National Referral Hospital (KNRH). KNRH has a 200-bed capacity and is one of four national referral hospitals in Uganda and located in Kampala, the capital city of Uganda. It is mandated to offer mainly specialized internal medicine and burns/reconstructive surgical services. The study population were patient files of adults admitted on the internal medicine units (cardiology, infectious diseases, pulmonology, nephrology, gastroenterology, hematology, and neurology) from January to July 2019 (before the pandemic) and from January to July 2020 (during the pandemic). We excluded patient files with > 20% missing data as this could cause misclassification bias. We conducted a census of all eligible files.
Data collection
We conducted a census of all files of patients admitted during the periods under consideration. Files were retrieved from the hospital records office and consecutively reviewed using a data abstraction form. Data on patient demographics, reasons for admission, presenting complaints, baseline vital signs, comorbidities, diagnostic tests performed, and treatment outcomes were collected. Treatment outcomes are documented in the file by the attending physician upon discharge (or death) of the patient. As such the physician indicated whether the patient was cured, improved, unimproved, transferred and died.
Data analysis
Data were exported to Microsoft Excel 2016 for cleaning and coding and imported to STATA 16.0 (Stata Corp LLC, College Station, Texas, USA) for formal analysis. First, numerical data was tested for normal distribution using Shapiro–Wilk test. Normally distributed numerical data were summarized as mean (standard deviation) whereas non-parametric numerical data as median (interquartile range). Categorical data were summarized as frequencies and percentages. At bivariate analysis, Chi-square test or Fisher’s exact test were used to assess the distribution of mortality across independent variables (sociodemographic and clinical characteristics). Simple logistic regression analysis was also used to assess the strength of these associations and presented as crude odds ratio at 95% confidence intervals. All independent variables with a p < 0.2 at bivariate analysis were used to construct multivariable logistic regression models in addition to variables that we deemed to have biological plausibility in influencing the risk of mortality. The goodness-of-fit was tested using Pearson goodness-of-fit test and the Hosmer–Lemeshow goodness-of-fit test and confusion matrix. The Hosmer–Lemeshow goodness-of-fit p-value was 0.748 and the confusion matrix showed, using the variables included in the multivariable logistic regression, the model correctly classified 82.54% of the mortality reported, both indicating that the model had a good fit. Results from the multivariable logistic regression model are presented as adjusted odds ratio at 95% confidence interval. At all levels of hypothesis testing, a p-value less than 0.05 were considered statistically significant.
Ethics declarations
The study was approved by the ethics committee of the School of Medicine, College of Health Sciences, Makerere University (REC approval number 2020-170) and Uganda National Council for Science and Technology (HS1030ES approval number). The School of Medicine, College of Health Sciences, Makerere University ethics committee waived the need of participant consent since we used retrospective data. Data were de-identified by using codes on data abstraction forms instead of patient names. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All methods and experimental protocols were carried out in accordance to the declaration of Helsinki.
Results
A total of 3804 files of patients who were admitted in the in-patient department between January–July 2019 and January–July 2020 was reviewed. Of these files, 55 (1.4%) were excluded due missing data. Figure 1 shows the participant accrual process.
Characteristics of patients
Table 1 shows the socio-demographic characteristics. Of 3749 patients, 2014 (53.7%) were female. More than half of the patients were aged more than 35 years old, with the elderly (60 + years) forming 21.3% of the patient population. Half of the patients were from the infectious disease unit (51.1%). The most frequent chronic diseases were HIV (42.2%), hypertension (18.0%) and diabetes mellitus (16.5%). About 20.6% and 9.6% of the patients had a history of alcohol use and smoking, respectively. The median duration of smoking and alcohol usage was 6.5 (IQR 3.5–20) years and 10 (5–20) years, respectively. About 7.3% (n = 275) had a history of both smoking and alcohol usage. More patients (51.6%) were admitted before the COVID-19 pandemic in 2019 (January–July 2019) than during the pandemic in 2020 (January–July 2020) indicating a 6.1% decline. By year of admission, patients differed by age category (p = 0.018), admission unit (p = 0.002), and region of origin in Uganda (p = 0.001). More patients with chronic obstructive pulmonary disease (COPD) were admitted in 2020 compared to 2019 (23 vs 11, p = 0.024).
Presenting symptoms and reason for admissions
A total of 491 patients (13.1%) were referrals from peripheral health facilities and some 22 (0.6%) patients needed oxygen on admission. Overall, the most frequent presenting symptoms were cough (43.2%), fever (36.7%), dyspnea (34.9%), general body weakness (27.5%) and headache (25.4%). About 12.4% and 5.1% presented with altered level of consciousness and convulsions, respectively. A lower proportion of patients were admitted with respiratory symptoms in 2020 compared to 2019 (45.5% vs 54.5%, p < 0.001). By year, patients presenting with cough (p < 0.001), sputum production (p = 0.001) and wheezing (p = 0.030) were significantly more in 2019 compared to 2020, whereas those presenting with fatigue (p = 0.018), altered level of consciousness (p = 0.001) and sore throat (p < 0.001) were significantly higher in 2020 than 2019. Table 2 summarizes the presenting complaints by year of admission.
Diagnostic tests performed
Table 3 summarizes the 20 most common laboratory tests and imaging that were performed. There were significantly fewer tests performed in 2020 than 2019 for the following tests: complete blood count, renal function tests, electrolytes, liver function tests, urinalysis, sputum GeneXpert, blood smears for malaria, blood sugar, glycated hemoglobin, and cerebral spinal fluid analysis (all p < 0.05). Only the CD4/viral load tests were performed more in 2020 than 2019. The decrease was 20.5% in blood slides for malaria, 21.5% in sputum GeneXpert, 30.1% in glycated hemoglobin and 29.4% in blood glucose. Similarly, the decline was 57.5% in serum electrolytes, 46.5% in cerebral spinal fluid analyses, 26.2% in liver function tests, 22.5% in urinalysis, 21.8% in renal function tests, 12.1% in complete blood counts.
Inpatient outcomes
A total of 649 patients (17.3%, 95% confidence interval: 16.1–18.5%) died during the period of review (Fig. 2). The majority of those who died, referred or did not improve were admitted in the year 2020, although there was more missing data on the outcomes in this same year (Fig. 2). Crude mortality rates were higher in 2020 when compared to 2019 (18% vs 16%, p = 0.151). Table 4 shows the distribution of mortality across independent variables. Mortality was significantly associated with admission unit (p < 0.001), region of origin in Uganda (p = 0.028) and purpose of visit (respiratory symptom: p = 0.018, non-respiratory symptom: p = 0.001, referral status: p < 0.001, and others: p = 0.043) at bivariate analysis. Having HIV (p < 0.001), hypertension (p < 0.001), diabetes (p = 0.003), tuberculosis (p = 0.002), and asthma (p = 0.010). were similarly significantly associated with mortality at bivariate analysis.
Factors associated with mortality
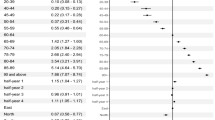
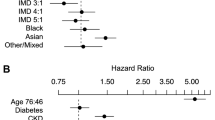
At simple logistic regression analysis (Table 5), patients admitted in the female infectious disease unit (IDF) (COR 1.8, 95% CI 1.3–2.5, p < 0.001) and male infectious disease unit (IDM) (COR 1.9, 95% CI 1.4–2.6, p < 0.001) wards were about twice more likely to die compared to those in the endocrine unit. Patients originating from the northern part of Uganda were also twice more likely to die (COR 2.3, 95% CI 1.1–4.5, p = 0.021 compared to those from central Uganda. Patients with HIV (COR 2.0, 95% CI 1.7–2.3, p < 0.001) and tuberculosis (COR 1.5, 95% CI 1.2–2.0, p = 0.002) were more likely to die, whereas those with hypertension (COR 0.4, 95% CI 0.3–0.6, p < 0.001), diabetes (COR 0.7, 95% CI 0.5–0.9, p = 0.003) and asthma (COR 0.4, 95% CI 0.2–0.8, p = 0.014) were less likely to die compared to those who did not have these comorbidities. Patients admitted due to non-respiratory symptoms were about thrice more likely to die compared to those with a respiratory complaint (COR 2.8, 95% CI 1.5–5.4, p = 0.019). Also, patients admitted as a referral were 1.6 times more likely to die than their non-referral counterparts (COR 1.6, 95% CI 1.2–2.0, p < 0.001).
In the final multivariable logistic regression model (Table 5), only age, period of admission, comorbidities (HIV and hypertension), and purpose of visits remained significantly associated with mortality. Age 60 years and above (AOR 1.6, 95% CI 1.2–2.1, p = 0.001), patients admitted during the COVID-19 pandemic (2020) (AOR 1.2, 95% CI 1.04–1.5, p = 018), those with HIV (AOR 1.5, 95% CI 1.2–1.9, p < 0.001), and those admitted as a referral from peripheral facilities (AOR 1.5, 95% CI 1.2–1.9, p < 0.001) were all significantly more likely to die. Conversely, hypertension remained significantly associated with less mortality compared to those without (AOR 0.5, 95% CI 0.4–0.7, p < 0.001).
Discussion
The COVID-19 pandemics has had a devastating impact on health care systems across the globe with significant reduction in overall service utilization (37% reduction), clinic visits (42%), admissions (28%), utilization of diagnostics (31%) and therapeutics (30%)7. In this study, we compared inpatient attendance, diagnostic tests performed on inpatients, patient characteristics and inpatient mortality between January–July 2019 (before the COVID-19 pandemic) and January–July 2020 (during the COVID- 19 pandemic) at an urban tertiary facility in Uganda. We found that inpatient admissions declined by 6.1% in 2020. People with respiratory conditions were less likely to be admitted during the pandemic at our study site although there were more COPD admissions. Additionally, there were fewer laboratory tests performed in 2020 and this was particularly concerning for sputum GeneXpert, blood smears for malaria, blood sugar, and glycated hemoglobin. While the difference in the crude mortality was not statistically significant (18% in 2020 vs. 16% in 2019, p = 0.15), being admitted during the pandemic was associated with 30% higher odds of mortality at multivariable analysis.
A decline in the number of inpatient admissions during the COVID-19 pandemic has been widely reported, although reports from Uganda a few. A decline in hospitalization among children with sickle cell disease was noted at an urban referral facility in Uganda during the pandemic13. A recent study found a decline in admission on adult medical wards in Kenya from April to June 2020 that coincided with national movement restrictions to curb the spread of COVID-1914. The decline in admissions was modest in our study compared to that reported in other studies in Croatia (21%)15, China (26%)16, Belgium (29–39%)17 and Spain (16.8%)18. Clearly, these countries had a larger scale of the pandemic and instituted more stringent lockdowns. Nonetheless, the reduction in admissions is likely due to lack of access to the hospital during the pandemic because of the transport restrictions that were instituted by government19, 20. This is supported by our data which shows fewer admission in 2020 for people from northern Uganda, the furthest region from the hospital. However, we cannot rule out that people stayed away from hospitals due to fear of infection or that referring clinicians had a higher threshold for referral to our facility during the pandemic period21.
Similar to our study, a large study in US hospitals reported a decline in admissions among patients with non-COVID related respiratory conditions22. A similar observation was made in South Africa23 and Spain18. While the reason for this is not apparent, we suppose that people with respiratory symptoms tended to shy away from hospitals to avoid stigma since many respiratory conditions have similar symptoms to COVID-19. Another possible explanation is that the lockdown resulted in lower pollution rates in Uganda and this coupled with use of face coverings could have led to a lower incidence of respiratory complaints24, 25. Additionally, Uganda had dedicated COVID treatment units in Kampala. Therefore, patients with respiratory symptoms could have been preferentially referred to those centers. Paradoxically, more people with COPD were admitted during the pandemic in our study. This could point to lack of access to the weekly respiratory outpatient clinic services that were closed during the pandemic. As such, the pandemic could have affected access and/or adherence to medicines for patients in chronic care. About 36% of people with chronic illnesses could not access medicines during the lock down s26.Conversely, one study in Spain reported that the rate of COPD exacerbations was lower during the pandemic than before although their sample size was small and they enrolled patients who were classified as frequent exacerbators27.
We observed a > 20% decline in the number of diagnostic tests performed including malaria (thick blood smears), tuberculosis (GeneXpert) and diabetes (blood sugar and glycated hemoglobin). This is worrisome and potentially affected TB and malaria detection, monitoring of diabetes mellitus treatment and overall treatment of patient who might have had these diseases. The decline in the number of tests performed is not proportionate to the decline in the number of inpatients in this study. Therefore, we cannot attribute the decline in the tests solely to the overall decline in inpatient numbers. Reported TB cases declined by 43% during the COVID lock down from pre-pandemic period in Uganda and this was estimated to increase TB-related mortality by 14%28. In rural Uganda, a recent study reported a decline in the number of malaria rapid diagnostic tests and the number of people initiating anti-malarial treatment before and during the pandemic29. Disruption of screening services for cardiovascular disease, such as diabetes mellitus, at health facilities has also been reported in Uganda during the pandemic30. Similar declines in laboratory test volumes (including the HbA1c) during the pandemic were noted elsewhere; and partial recovery to pre-pandemic levels might affect long term monitoring of people with chronic diseases31, 32. Taken together, the decline in these diagnostic tests due to the pandemic could have lasting effect on elimination of TB and malaria33, 34.
We found that being admitted during the pandemic was associated with higher odds of mortality. This is possibly because of delayed referrals or referral bias of critically ill individuals. This is supported by the higher likelihood of death we observed among referred patients. Additionally, clinical teams might have found difficulty in making diagnoses for life-threatening conditions such as sepsis, bacterial meningitis, acute kidney injury, acute liver injury and electrolyte abnormalities. From our study, there was a decline in the number of tests performed for these conditions; that is, fewer cerebral spinal fluid analyses, urinalysis, full blood count, serum electrolytes, serum creatinine and liver function tests. There is scanty data from medical wards in Uganda to compare our findings to. However, a study at a newborn unit in Uganda reported a 14% decline in admissions, an increase in inpatient mortality (16% vs. 11%) and patients referred from other facilities had a 55% higher mortality35. A large study of more than 32 million admissions in the US also showed a 30% increase in all-cause mortality among inpatients during the pandemic period36. A similar observation was made among non-COVID-19 admissions at 4626 US hospitals37. Conversely, a large study in Germany reported lower risk for all-cause mortality during the pandemic period when people with SARS-CoV-2 were excluded in the analysis38. However, their population had significantly low HIV infection rates compared to our study where 1 in 4 people had HIV infection. Moreover, HIV was independently associated with mortality in our study, and alongside advanced age, is consistently observed to increase the risk of mortality on medical wards in Uganda39.
Our study is limited in several ways. First, this was a single center study and this limits generalizability of findings. Moreover, the study site is a tertiary hospital, and this could introduce referral bias whereby critically ill individuals were referred during the pandemic. Thirdly, we did not evaluate system factors such as stock out of supplies and health worker absenteeism during the pandemic that could potentially affect the volume of diagnostic tests performed and the overall patient outcomes. For 26% of the participants included, the outcome was not documented in the files. We modelled these as non-fatal outcomes since death is meticulously documented in our hospital and admission units conduct mortality audits. Nonetheless, this might have introduced some misclassification bias. Our study included the months of January and February 2020 in the COVID pandemic period yet COVID-19 was declared a pandemic in March 2020. This could have affected the accuracy of our estimates. However, we believe that perceptions and health care utilization were already affected in the two months preceding March when cases and deaths started to be reported outside China and human-to-human transmission was confirmed40. Lastly, data on the COVID-19 vaccination status were not available in the files. Therefore, we were unable to determine if the COVID-19 vaccine affected the outcomes.
Conclusion
There was a modest decline in the number of admissions during the COVID-19 pandemic at a tertiary hospital in Uganda. There was a decline in the diagnostic tests during the pandemic and this could affect gains made in the control and elimination of TB and malaria. Being admitted during the pandemic was associated with 30% higher odds of mortality. Policy makers in Uganda need to build resilience in health systems to deal with future pandemics.
Data availability
Datasets used in this analysis are available from the corresponding author on reasonable request.
References
WHO. WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int.
Paital, B., Das, K. & Parida, S. K. Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. Sci. Total Environ. 728, 138914 (2020).
Santoli, J. M. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration: United States, 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 591–593 (2020).
Roberton, T. et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: A modelling study. Lancet Glob. Health 8, e901–e908 (2020).
World Health Organization. The Potential Impact of Health Service Disruptions on the Burden of Malaria: A Modelling Analysis for Countries in Sub-Saharan Africa (World Health Organization, 2020).
Jewell, B. L., Mudimu, E., Stover, J., Kelly, S. L. & Phillips, A. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models. Lancet HIV 7(9), e629–e640 (2020).
Moynihan, R. et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 11, e045343 (2021).
Desta, A. A. et al. Impacts of COVID-19 on essential health services in Tigray, Northern Ethiopia: A pre-post study. PLoS ONE 16, e0256330 (2021).
Tessema, G. A. et al. The COVID-19 pandemic and healthcare systems in Africa: A scoping review of preparedness, impact and response. BMJ Glob. Health 6, e007179 (2021).
Olum, R. & Bongomin, F. Uganda’s first 100 COVID-19 cases: Trends and lessons. Int. J. Infect. Dis. 96, 517–518 (2020).
Bell, D. et al. Predicting the impact of COVID-19 and the potential impact of the public health response on disease burden in Uganda. Am. J. Trop. Med. Hyg. 103, 1191–1197 (2020).
Tumwesigye, N. M., Denis, O., Kaakyo, M. & Biribawa, C. Effects of the COVID-19 Pandemic on Health Services and Mitigation Measures in Uganda (Center for Global Development Washington, 2021).
Namazzi, R. et al. Impact of a national lockdown for COVID-19 on morbidity and mortality among children with sickle cell anaemia at a tertiary care hospital in Uganda. Blood 136, 33–34 (2020).
Wambua, S. et al. The indirect impact of COVID-19 pandemic on inpatient admissions in 204 Kenyan hospitals: An interrupted time series analysis. PLOS Glob. Public Health 1, e0000029 (2021).
Kalanj, K., Marshall, R., Karol, K., Tiljak, M. K. & Orešković, S. The impact of COVID-19 on hospital admissions in Croatia. Front. Public Health 9, 948 (2021).
Yang, Y. et al. Changes in inpatient admissions before and during COVID-19 outbreak in a large tertiary hospital in Shanghai. Ann. Transl. Med. 10, 469–469 (2022).
Yombi, J. C., Yildiz, H., Beguin, C. & Habimana, L. Non-COVID-19 in-hospital admission in a large academic center in belgium during the first two waves of the COVID-19 pandemic. Int. J. Gen. Med. 14, 7895 (2021).
Domingo, L. et al. Impact of COVID-19 on hospital admissions and healthcare quality indicators in non-COVID patients: A retrospective study of the first COVID-19 year in a university hospital in Spain. J. Clin. Med. 11, 1752 (2022).
Peden, M. & Kobusingye, O. Transport and health during and after {COVID}-19:{An}{Insight}. Health 2019, 1–12 (2019).
Nuwematsiko, R. et al. Unintended socio-economic and health consequences of COVID-19 among slum dwellers in Kampala, Uganda. BMC Public Health 22, 88 (2022).
Banke-Thomas, A. et al. A mixed-methods study of maternal health care utilisation in six referral hospitals in four sub-Saharan African countries before and during the COVID-19 pandemic. BMJ Glob. Health 7, e008064 (2022).
Birkmeyer, J. D., Barnato, A., Birkmeyer, N., Bessler, R. & Skinner, J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff. Proj. Hope 39, 2010–2017 (2020).
McIntosh, A. et al. Effect of COVID-19 lockdown on hospital admissions and mortality in rural KwaZulu-Natal, South Africa: Interrupted time series analysis. BMJ Open 11, e047961 (2021).
Angom, J., Angiro, C. & Omara, T. Air quality improvement from COVID-19 lockdown in the East African community: Evidences from Kampala and Nairobi Cities. Open Access Libr. J. 8, 1–26 (2021).
Meji, M. A., Dennison, M. S. & Mobisha, M. Effect of COVID-19 induced lockdown on air quality in Kampala. Manag. J. Future Eng. Technol. 16, 43 (2020).
Katana, E. et al. Factors associated with access to food and essential medicines among Ugandans during the COVID-19 lockdown: A cross-sectional study. J. Interv. Epidemiol. Public Health 4, 1–4 (2021).
Baeza-Martínez, C., Zamora-Molina, L., Olea-Soto, J., Soler-Sempere, M. J. & García-Pachón, E. Reduction in hospital admissions for COPD Exacerbation during the covid-19 pandemic. Open Respir. Arch. 2, 201–202 (2020).
Kadota, J. et al. Impact of shelter-in-place on TB case notifications and mortality during the COVID-19 pandemic. Int. J. Tuberc. Lung Dis. 24, 1212 (2020).
Namuganga, J. F. et al. Impact of COVID-19 on routine malaria indicators in rural Uganda: An interrupted time series analysis. Malar. J. 20, 475 (2021).
Musinguzi, G. et al. The early impact of COVID-19 on a Cardiovascular disease prevention program in Mukono and Buikwe districts in Uganda: A qualitative study. Glob. Heart 16, 52 (2021).
Ahmed, S. & Ghani, F. Trend analysis of lab tests requisitions of COVID-19 prognostic biomarkers at a clinical chemistry reference laboratory-an observational study. Ann. Med. Surg. 60, 522–525 (2020).
Singh, I. R., Dowlin, M., Chong, T. H., Nakamoto, J. M. & Hilborne, L. H. Changes in test volumes during coronavirus disease 2019 (COVID-19): A laboratory stewardship opportunity. Arch. Pathol. Lab. Med. 145, 821–824 (2021).
Zawawi, A. et al. The impact of COVID-19 pandemic on malaria elimination. Parasite Epidemiol. Control 11, e00187 (2020).
Alene, K. A., Wangdi, K. & Clements, A. C. A. Impact of the COVID-19 pandemic on tuberculosis control: An overview. Trop. Med. Infect. Dis. 5, 123 (2020).
Hedstrom, A. et al. Impact of the early COVID-19 pandemic on outcomes in a rural Ugandan neonatal unit: A retrospective cohort study. PLoS ONE 16, e0260006 (2021).
Phillips, M. C. et al. Effect of mortality from COVID-19 on inpatient outcomes. J. Med. Virol. 94, 318–326 (2022).
Dang, A. et al. Hospitalizations and mortality from non–SARS-CoV-2 causes among medicare beneficiaries at US hospitals during the SARS-CoV-2 pandemic. JAMA Netw. Open 5, e221754 (2022).
König, S. et al. A comparative analysis of in-hospital mortality per disease groups in Germany before and during the COVID-19 pandemic from 2016 to 2020. JAMA Netw. Open 5, e2148649 (2022).
Kalyesubula, R. et al. Trends of admissions and case fatality rates among medical in-patients at a tertiary hospital in Uganda; A four-year retrospective study. PLoS ONE 14, e0216060 (2019).
CDC. CDC Museum COVID-19 Timeline. Centers for Disease Control and Prevention. https://www.cdc.gov/museum/timeline/covid19.html (2023).
Funding
This study was funded by Clockworks Research Company Limited.
Author information
Authors and Affiliations
Contributions
I.A.B.—Conceptualisation, funding acquisition, methodology, interpretation of data, manuscript revision, final approval. J.B.B.—methodology, formal analysis, interpretation of data, drafting manuscript, manuscript revision, final approval. R.O.—methodology, formal analysis, interpretation of data, manuscript revision, final approval. F.B.—methodology, interpretation of data, manuscript revision, final approval. A.P.K.—data accrual, interpretation of data, manuscript revision, final approval. S.N.—data accrual, interpretation of data, manuscript revision, final approval. P.S.—methodology, interpretation of data, manuscript revision, final approval. D.K.—methodology, interpretation of data, manuscript revision, final approval. S.B.—funding acquisition, methodology, interpretation of data, manuscript revision, final approval. E.S.—methodology, interpretation of data, manuscript revision, final approval. C.K.—methodology, interpretation of data, manuscript revision, final approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Andia-Biraro, I., Baluku, J.B., Olum, R. et al. Effect of COVID-19 pandemic on inpatient service utilization and patient outcomes in Uganda. Sci Rep 13, 9693 (2023). https://doi.org/10.1038/s41598-023-36877-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-36877-9
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.