Abstract
Opisthorchis viverrini infection is an emerging disease in Cambodia, especially in central and southeastern areas. However, its status in northern areas bordering Lao PDR has been relatively unknown. The present study was performed to investigate the status of O. viverrini infection among people in Preah Vihear and Stung Treng provinces through fecal examination to detect eggs and recovery of adult flukes from some of the egg-positive cases. Fecal examinations were performed on a total of 1101 people from 10 villages in the 2 provinces using the Kato-Katz thick smear technique. For recovery of adult flukes and other helminth parasites 10 volunteers positive for eggs of Opisthorchis viverrini and/or minute intestinal flukes (Ov/MIF), in Kampong Sangkae village, Preah Vihear province, were administered a single oral dose of 40 mg/kg praziquantel plus 5–10 mg/kg of pyrantel pamoate and purged with 40–50 g magnesium salts. Adult trematodes, together with nematodes and cestodes expelled in diarrheic stools were collected under a stereomicroscope or with the naked eye. The proportion of egg-positive cases for overall liver and intestinal helminths was high but not notably different between the 2 provinces, 65.5% in Preah Vihear versus 64.7% in Stung Treng. The average proportion of Ov/MIF egg-positive cases was 59.8%. A total of 315 adult specimens of O. viverrini were recovered from the 10 volunteers (4–98 specimens per individual; mean, 32). A smaller number of Haplorchis taichui adults, an intestinal fluke, were found mixed-infected in 7 (103 specimens in total; 1–31 per individual; mean, 15) of the 10 volunteers. Adult specimens of hookworms, Enterobius vermicularis, Trichostrongylus sp., and a Taenia tapeworm strobila were recovered in some cases. Based on the results, it has been confirmed that the surveyed areas in Preah Vihear and Stung Treng provinces, Cambodia, are highly endemic areas of O. viverrini infection with a low-grade mixed infection with H. taichui.
Similar content being viewed by others
World Health Organization (WHO) has recognized foodborne trematodiases, including liver, lung, and intestinal fluke infections, as an essential group of neglected tropical diseases1. Among the liver flukes, Opisthorchis viverrini, Opisthorchis felineus, and Clonorchis sinensis are the 3 major species causing liver diseases in humans and animals. For completion of their life cycles, they need freshwater snail species, for example, Bithynia spp. for O. viverrini and O. felineus, and Parafossarulus spp. for C. sinensis, to develop into cercariae, freshwater fish species, including cyprinoid fish, to develop into metacercariae, and mammalian hosts, including humans and domestic animals, to develop into adult flukes in the bile duct2. Consumption of raw or undercooked freshwater fish is the principal mode of infection2. The infection is characterized by cholangitis in acute stages and liver cirrhosis and cholangiocarcinoma (more commonly in O. viverrini and C. sinensis) in chronic stages2. Common clinical manifestations include fever, jaundice, anorexia, weight loss, fatigue, yellow sclera, and decreased liver functions2,3,4. O. viverrini is the responsible species in the Greater Mekong Subregion, especially in Thailand, Lao PDR, and southern parts of Vietnam3. O. felineus is distributed mainly in Eastern Europe, and C. sinensis is distributed in far East Asia (China and Korea) and northern parts of Vietnam2.
In Cambodia, information on the status of O. viverrini infection has historically been scarce. Recently, however, O. viverrini infection became acknowledged as an emerging disease based on published as well as unpublished observations4. In 2006, an O. viverrini initiative was launched as the National Helminth Control Program4. However, this program was mostly focused on the detection of endemic areas of O. viverrini through nationwide fecal examinations using the Kato-Katz fecal smear technique4. The results revealed that the geographical distribution of O. viverrini in Cambodia seemed to be almost countrywide, i.e., in 22 of the total 24 provinces surveyed; the prevalence in egg positive rate of O. viverrini and/or minute intestinal flukes (Ov/MIF) ranged from 0.1 to 47.5% depending on different localities4,5. The highest prevalence was found in central and southeastern provinces, including Takeo (23.8–47.5%), Kampong Thom (34.8%), Kampong Cham (24.0%), and Kandal (20.2%)4,5,6,7.
Regarding the two northernmost provinces bordering Lao PDR, Preah Vihear and Stung Treng, the prevalence was reported to be relatively low, 2.7 and 2.5%, respectively, based on a nationwide survey5. However, according to other reports, the prevalence in these areas was variable; for example, 1.4% in 20 villages (2010)4, 5.1% in 1 village (2014)8, and 45.7% in 1 village (2010)4 in Preah Vihear, and 0% in 11 villages (2000 and 2007)4 and 2.3% in 4 villages (1998)9 in Stung Treng. Thus, it is considered that the endemicity of O. viverrini and/or MIF in Preah Vihear and Stung Treng provinces varies depending on the locality (riversides or remote from the river) and target population (children or adults) and should be further investigated in different areas, particularly among people living along the rivers and streams.
In addition, O. viverrini and MIF produce visually similar eggs10, although they are biologically dissimilar organisms and parasitize different organs in the definitive host. Hence, parasitological diagnostic tests have imperfect specificity when there are co-infections with O. viverrini and MIF, and thus these eggs are expressed as Ov/MIF eggs. It is needed to confirm whether the Ov/MIF eggs detected in the present study are really those of O. viverrini or of MIF, or mixed-infected. For this, adult worm recovery from egg-positive individuals after chemotherapy is one of the procedures that can be applied11,12. Sequencing of relevant genes, for example, 18S and 28S rDNA, from the eggs can be an alternative method showing high sensitivity and high specificity13.
In the present study, we surveyed the infection status of liver and intestinal helminths among riparian people in 10 villages of Preah Vihear and Stung Treng provinces (Fig. 1) bordering Lao PDR using the Kato-Katz technique to detect fecal eggs. In addition, 10 volunteers from Preah Vihear province positive for Ov/MIF eggs were prescribed praziquantel and pyrantel pamoate followed by purging with magnesium salts, and the adult flukes, nematodes, and cestodes expelled in diarrheic stools were collected and morphologically identified.
Results
Overall prevalence and intensity of infection of Ov/MIF and other helminthes
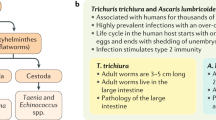
The proportion of overall helminth egg-positive cases was very high, 64.9%, with a 95% confidence interval (CI) of 62.1–67.7%, among the people surveyed in 5 villages each of Preah Vihear and Stung Treng provinces (Table 1). The eggs of Ov/MIF were the most commonly identified species with an average prevalence of 59.8% (56.8–62.6%), which slightly varied among different villages and between the two provinces, 58.3% (52.7–63.7%) in Preah Vihear and 60.3% (56.9–63.7%) in Stung Treng (Table 1). The arithmetic mean EPG (number of eggs per gram of feces) of Ov/MIF was 862 per egg-positive person (n = 658). The highest prevalence was found in Kampong Sangkae village (80.9%) in Preah Vihear province. The second highly prevalent helminth was hookworms (12.2%; 10.1–13.9%; mean EPG 413), followed by Taenia spp. (2.4%), Trichuris trichiura (1.5%; 0.9–2.4%; mean EPG 67), Schistosoma mekongi (1.0%), Enterobius vermicularis (0.8%), echinostomes (0.6%), Trichostrongylus sp. (0.4%), and others (0.5%). Others included dicrocoeliid eggs and Hymenolepis diminuta eggs. The species of echinostomes was difficult to determine by the eggs, although it was highly suggested to be Echinostoma mekongi. However, the eggs of Ascaris lumbricoides were not detected in both surveyed provinces.
Age- and sex-specific prevalence and EPG of Ov/MIF eggs
The prevalence and intensity of infection in EPG of Ov/MIF eggs showed a trend by age (Fig. 2A, B). The average prevalence and EPG (both males and females) were the lowest in the age group 0–9 years, 33.8% (27.9–39.9%) and 408 (300–572), followed by the age groups 10–19 years, 57.5% (52.8–62.2%) and 717 (602–863), 20–29 years, 72.6% (64.7–79.6%) and 730 (570–956), and 30–39 years, 77.8% (68.9–85.2%) and 1034 (770–1433), respectively. Then, the prevalence became steadily high showing a plateau, 78.9–80.0%, in the age groups between 40 and 49 and ≥ 60 years (Fig. 2A). Meanwhile, the mean EPG showed the highest value at 40–49 years, 2273 (1505–3664), followed by a reduction in the ages 50–59 and ≥ 60 years groups (Fig. 2B). The age-prevalence and intensity of infection patterns were almost similar in males and females (Fig. 2A, B) and in Preah Vihear and Stung Treng provinces (data not shown). The average prevalence and EPG were not significantly different between males (59.0%; 54.3–63.6% and 747; 629–896, respectively) and females (60.2%; 56.5–63.9% and 934; 811–1082, respectively). The overall total prevalence and EPG were 59.8% (56.8–62.6%) and 862 (773–965), respectively.
Age- and sex-specific prevalence (mean and 95% confidence interval) (A) and EPG (B) of Ov/MIF eggs among the riverside people (n = 1101) in Preah Vihear and Stung Treng provinces, Cambodia in 2018. A prominent age tendency is recognizable, but no significant difference is seen between males (n = 432) and females (n = 669).
Adult flukes and other helminths recovered from volunteers in Preah Vihear province
The adult worm recovery was successfully performed in 10 volunteers (5 men and 5 women; aged 21 to 45 years) who were positive for Ov/MIF eggs (Fig. 3), with EPG higher than 240. Eight kinds of helminths, including 2 trematode species, 5 nematode species, and 1 cestode species, were recovered from their diarrheic stools (Table 2). A total of 315 (4–98 per individual) adult specimens of O. viverrini were collected from 10 volunteers (Table 2; Fig. 4A), and a total of 103 adult specimens (1–31 per individual) of H. taichui (Fig. 4B) were collected from 7 of the 10 volunteers (Table 2). The number of adult worms of O. viverinii and H. taichui recovered in each case showed a strong positive correlation (r = 0.85; P = 0.0019) with the EPG (eggs per gram of feces) (Ov/MIF eggs) of each case in the fecal examination (Table 2). EPG was measured by counting the total number of eggs on each Kato-Katz fecal smear, which was multiplied by 24, assuming that the volume of feces on each Kato-Kato smear was 41.7 mg14. In addition, 70 adult specimens of hookworms (64 Necator americanus and 6 Ancylostoma ceylanicum) were collected from 7 volunteers (reported separately by Chang et al.15), 57 Enterobius vermicularis were from 6 volunteers, 9 Trichostrongylus sp. from 3 volunteers, 1 strobila of Taenia saginata from 1 volunteer (reported separately by Chang et al.16), and 1 unknown nematode from 1 volunteer (Table 2).
Differential morphological features of O. viverrini and H. taichui
For the speciation of two adult trematode species, their brief morphological features are described here. Adult flukes of O. viverrini (Fig. 4A) were elongated and lanceolate, 8.0–10.9 (av. 8.9) mm long and 1.5–2.5 (av. 1.7) mm wide (n = 9). The oral sucker was slightly smaller than the ventral sucker (sucker ratio, 0.9: 1.0). They had 2 obliquely tandem testes, which were 4- (anterior testis) to 5-lobulated (posterior testis) (different from markedly branched testes in Clonorchis sinensis), near the posterior end of the body. The vitellaria were distributed laterally from the level of the seminal receptacle or anterior end of the anterior testis up to the 1/3–1/4 length level of the uterus. The vitelline follicles were dense and compact and aggregated into 7–8 groups on each side. The ovary was 5- to 10-lobulated (less lobulated and almost oval in Opisthorchis felineus).
Adult flukes of H. taichui (Fig. 4B) were small, ovoid to elliptical, 0.73–1.08 (av. 0.88) mm long and 0.38–0.49 (av. 0.42) mm wide (n = 10). They were characterized by the presence of only 1 testis but lacked an expulsor of the seminal vesicle, thus were assigned to the genus Haplorchis. They had a small inconspicuous ventral sucker, embedded in the parenchyma, forming a ventrogenital sac with its dorsal and ventral lobes, armed with 12–16 long crescentic and hollow minute spines of 19–30 μm in length. These characters, especially the number and size of minute spines, are differential points from the related species, Haplorchis pumilio and Haplorchis yokogawai.
Discussion
The prevalence of Ov/MIF (confirmed to be mostly O. viverrini) infection observed in this study appeared to be the highest ever reported in Cambodia. In a nationwide survey performed previously by our group5, high prevalences of Ov/MIF were found in Kampong Cham (24.0%) and Takeo province (23.8%), and a relatively lower prevalence was detected in Preah Vihear (2.7%), Stung Treng (2.5%), Kratie (3.4%), and Ratanakiri province (2.8%). In another study by our group6, a riparian population in Prey Kabas District in Takeo province revealed a much higher prevalence (47.5%) of Ov/MIF infection. A study by another group7 undertaken in 5 provinces of Cambodia reported high prevalences of Ov/MIF infection in Kampong Thom (34.8%) followed by Kampong Cham (33.1%), Takeo (21.4%), and Kandal (18.7%), with no infection in Prey Veng province (0%). Taken together, a total of 6 provinces, including Preah Vihear, Stung Treng, Kampong Cham, Kampong Thom, Takeo, and Kandal, are currently recognized as the major endemic areas of opisthorchiasis in Cambodia. Interestingly, however, in Kratie province, which is located along the mainstream of the Mekong River, and neighbored by the highest endemic areas (Stung Treng, Kampong Thom, and Kampong Cham provinces), the prevalence of Ov/MIF infection was relatively low, 4.6%, among people in 7 riverside villages17. Further investigations are needed to properly estimate the prevalence of Ov/MIF infection in Kratie province and other localities of Cambodia along the Great Mekong Subregion.
The high prevalence of O. viverrini in the surveyed areas of Preah Vihear and Stung Treng province is comparable with those reported in Lao PDR, the most highly endemic country ever known18,19,20,21,22. The reported prevalence of Ov/MIF infection in Lao PDR was 43.8% around Pakse city (Champasak province)18, 67.1% in Savannakhet province19, 52.0–60.7%20 or 81.1%21 in Khammouane province, and 53.3% in Vientiane Municipality22. Thailand, formerly known as the most highly endemic country for O. viverrini infection, became a lower-grade endemic country owing to the active and sustained national control activities over 40 years since the 1980s3. The national prevalence in Thailand was 14.7% in 1980–1981, with the highest level of 34.6% in the northeast areas, but the national prevalence decreased to 11.8% in 1996 and 9.6% in 20013. In northeast areas, the prevalence remained at 60.8% in Nakhon Phanom, 38.6% in Sisaket, and 32.6% in Amnat Charoen province by 2009; however, the prevalence in these areas also decreased substantially in 2014 with Nakhon Phanom remained the only province showing the prevalence over 20%3. After 2014, however, there were several publications reporting a considerably high prevalence (16.9–28.7%) in northeastern and central Thailand23,24,25,26. In Vietnam, Phu Yen province and some other mid- to southern provinces have been notified as endemic areas of O. viverrini, with the prevalence ranging from 0.3 to 36.9%3. A low-grade endemicity was recently reported in lower Myanmar with a 0.7% egg-positive rate27. Thus, the present survey areas in Cambodia appeared to be one of the most highly endemic areas of O. viverrini infection ever reported.
There seem to be potential risk factors for the surveyed areas to appear as highly endemic areas of opisthorchiasis. One is the locality of the surveyed villages. These villages are located along the main stem or tributaries of the Mekong River. The 5 villages of Preah Vihear province locate just along the border between Cambodia and Lao PDR. In Lao PDR, O. viverrini infection has been known to be highly endemic, especially in Vientiane Municipality, Khammouane, Savannakhet, and Champasak provinces18,19,20,21,22. The 5 villages of Stung Treng province are located along the river and streams not far from the border area. Other risk factors include that most villagers are engaged in fisheries and are traditionally accustomed to eating raw or undercooked freshwater fish.
This study showed a significant age tendency in the prevalence of Ov/MIF infection. The prevalence was the lowest among children under 9 years, followed by the age groups 10–19 years and 20–29 years. It approached a peak at ages 30–39 years and then maintained the peak up to the age groups 40–49, 50–59, and ≥ 60 years. This tendency was like those reported previously for liver fluke infections in other countries; O. viverrini in Lao PDR and Thailand28,29,30, O. felineus in Russia31, and C. sinensis in South Korea32. Also, in Cambodia (Takeo province), almost the same age-prevalence pattern of O. viverrini infection was observed among the riverside people4,6.
Sex difference in the incidence of liver fluke infections is known to be variable according to locality and human behavior31,32, although helminth infections are generally known to be heavier in males than in females in mammalian hosts33. In South Korea, males revealed a higher incidence of C. sinensis infection than females, related to some social customs in males, i.e., frequent consumption of raw or undercooked freshwater fish with liquor in social gatherings32. Similar trends were observed in China, where C. sinensis is endemic32. Reversely, in O. felineus infection, the greatest incidence was noted among housewives, i.e., females, in Russia31. However, in Thailand, where O. viverrini is prevalent, male preponderance or no significant sex difference has been reported20,31,34. In Cambodia, a male preponderance was reported in Takeo province6. However, in the present study, no significant sex difference was noted. One of the reasons may be that the major source of infection in the surveyed areas is traditional fish dishes popularly consumed by the people regardless of gender, such as ‘plea tre’ (fish salad), ‘plea tre chou’ (sour fish salad), and ‘ma’am’ (fermented fish, kept for 2–5 days).
There was a positive correlation between the number of adult O. viverrini and/or H. taichui specimens recovered and the number of EPGs in 10 volunteers, as presented in Table 2. Our results agreed with a previous report from Thailand where 231 residents of a northeast community positive for O. viverrini eggs were treated with praziquantel, and adult flukes were collected35. The pre-treatment egg counts (EPG) showed a strong linear relationship with the number of worms recovered after the treatment. It was also of note that the fecundity of O. viverrini appeared to be related to the degree of parasite aggregation within the host body and negatively associated with the total worm burden in each host individual35,36. In the present study, the number of cases in whom worm recovery was performed was small (only 10), and the density-dependent reduction in worm fecundity was difficult to analyze.
It is noteworthy that H. taichui was found mix-infected with O. viverrini among the volunteers in Preah Vihear province. To the best of our knowledge, this is the first report of human H. taichui infection in Cambodia. This combination of mixed infections was previously found in other countries, including Lao PDR19,21,22,37,38 and Thailand39,40. One of the points that should be considered is the relative predominance of these fluke species. For example, in Saravane province, Lao PDR, only 68.4% (13/19) of the volunteers positive for Ov/MIF eggs in fecal examination expelled O. viverrini specimens after chemotherapy and purging, whereas 100% (19/19) of the volunteers did H. taichui flukes41. In addition, the total number of fluke specimens recovered was notably different; only 796 (n = 13) specimens of O. viverrini versus 409,738 (n = 19) specimens of H. taichui41. This41 and another study in Lao PDR22 support the finding that Saravane province is a highly endemic area of H. taichui infection with a low-grade infection with O. viverrini. Reversely, Vientiane Municipality was confirmed to be a highly endemic area of O. viverrini infection with a low-grade mixed infection with H. taichui22. On the other hand, Savannakhet province was an area with almost equal endemicity (prevalence and worm load) of O. viverrini and H. taichui19, whereas Khammouane province was an area with a slightly higher endemicity of H. taichui than O. viverrini21. Thus, the surveyed areas in our study, Preah Vihear and Stung Treng provinces, are regarded as an O. viverrini dominant area with a low-grade (low prevalence and low intensity) H. taichui infection.
In areas of mixed infections with O. viverrini and MIF (H. taichui, for example), molecular testing of the fecal eggs would be advantageous. Buathong et al. (2020)42 reported the usefulness of PCR and PCR-restriction fragment length polymorphism (PCR–RFLP) analysis targeting internal transcribed spacer 2 (ITS2) gene in differentially diagnosing O. viverrini and H. taichui infections in northern Thailand.
The average prevalence of S. mekongi appeared to be quite low, 0.8% in 10 villages surveyed, with a prevalence of 1.6% in Preah Vihear and 0.5% in Stung Treng province. These two provinces have been well known as the endemic areas of schistosomiasis mekongi, and long-time surveillance (1995–2010), as well as control efforts, have been implemented by the government4. The present findings seem to be the results of the governmental control activities against this trematode infection.
The eggs of A. lumbricoides were not detected in this study. This finding denotes that the national control program against soil-transmitted helminthiases in Cambodia by the mass drug administration (MDA) using mebendazole and/or albendazole twice a year for over 20 years4 has been highly successful. The prevalence of other soil-transmitted helminths appeared to be 12.2% for hookworms and 1.5% for T. trichiura; however, the prevalence of these parasites is also expected to decrease further so far as the national control program is continued. We regret that the prevalence of S. stercoralis, another soil-transmitted helminth species, could not be determined in this study because the Kato-Katz fecal examination method alone was applied. There were 6 people from whom female E. vermicularis adult nematodes were collected; among them, 5 people were egg-negative in Kato-Katz fecal examinations.
In conclusion, it has been confirmed for the first time in this study that the northernmost areas of Preah Vihear and Stung Treng provinces, Cambodia, bordering Lao PDR are highly endemic areas of O. viverrini infection, with a prevalence of 58.3 and 60.3% (59.8% in average), respectively. The adult flukes recovered from 10 volunteers in Kampong Sangkae village, Preah Vihear, were, in their majority, identified as O. viverrini. A substantial number of H. taichui adult specimens were also recovered from 7 of the 10 volunteers, together with a few or quite many specimens of adult nematodes (5 species) and cestodes (1 species). Further epidemiological studies of O. viverrini and H. taichui infections in humans should be performed in various localities along the Mekong River in Cambodia.
Methods
Ethical consideration and data processing
The National Ethics Committee for Health Research, Ministry of Health, Cambodia approved this study (approval no.: 099NECHR), and all the methods used were performed in accordance with the relevant guidelines and regulations. The CNM staff were informed of and oriented on the proposed project, explained about this project to the participants, and then the informed consent form was obtained from each participant for fecal examination and from each volunteer for adult worm recovery. The collected data were analyzed in Excel 2016 (Microsoft, Redmond, WA, USA) and were statistically evaluated using the chi-square test. The level of statistical significance was set at P < 0.05.
Survey areas and participants
To determine the endemicity of O. viverrini and/or MIF among riparian people in the northernmost parts of Cambodia, a cross-sectional community-based survey was performed in April–May 2018 in 10 villages of Preah Vihear and Stung Treng province bordering Lao PDR (Fig. 1). These villages are located along the Mekong River; 5 villages in Preah Vihear are located along the mainstream, and the other 5 villages in Stung Treng are along a small tributary. These villages were selected in consideration of the previous results of fecal examinations in which small trematode eggs of about 28–30 μm in length (possibly the eggs of O. viverrini and/or MIF) were detected in a high proportion of the people examined (unpublished observations). The number of recruited people in this study was 432 males and 669 females, with an age range of 5–95 years. There were no special exclusion criteria for recruiting people for fecal examinations. Most residents in these villages were agricultural workers or fishermen along the Mekong River and popularly consumed traditional foods made of raw or undercooked freshwater fish.
Fecal examinations
A total of 1101 fecal samples were collected from the people, one sample for each person, in the 10 selected villages of 2 provinces which were transported to the laboratory of the National Center for Parasitology and Malaria Control (CNM) in Phnom Penh in April–May 2018 within 24 h after collection. Fecal examinations were performed using the Kato-Katz thick smear method, which is useful for large-scale monitoring of helminthic infections, except for Strongyloides stercoralis larvae. One smear slide was prepared per person and examined under a light microscope in the CNM.
Adult worm recovery and identification
Adult trematodes were recovered from 10 volunteers in Kampong Sangkae village, Preah Vihear Province, in December 2018. The reason for selecting this village was in consideration of the highest Ov/MIF prevalence among the 10 villages surveyed (see the “Results” Section). The inclusion criteria for volunteers were those showing > 240 EPG of Ov/MIF eggs, and the exclusion criteria included pregnant women, children younger than 15 years, and elderly people over 61 years. The adult worm recovery was performed in a regional health center within the village. The volunteers were provided with informed consent and were given orally 40 mg/kg single dose of praziquantel (Shinpoong Pharmaceutical Co., Seoul, Korea) plus 5–10 mg/kg pyrantel pamoate (Hangzhou Minsheng Pharm. Co., Hangzhou, China) followed by 40–50 g of magnesium sulfate for purging. The whole consecutive diarrheic stool passed 4–5 times after the medication was collected and washed several times with > 10 volumes of water and re-suspended in water. After 10 min, the clean upper layer was discarded, and the dark lower layer was examined under the naked eye or placed under a stereomicroscope (Olympus, Japan) and explored for worm parasites. The number of worms collected was counted for each helminth species. Some of the adult fluke specimens were fixed in 10% formalin under a coverslip pressure, stained with Semichon’s acetocarmine, dehydrated in a graded series of ethanol, cleared in xylene, and morphologically identified using a light microscope.
Statistical tests
Statistical tests were performed using the R Statistical Software (v 4.1.2; R Core Team 2021, Vienna, Austria).
Ethics approval
The study protocols were approved by the National Ethics Committee for Health Research, Ministry of Health, Cambodia (approval no.: 099NECHR). Informed consent was obtained from all the participants for fecal examinations and adult worm collection following chemotherapy.
Data availability
The datasets used and/or analyzed during the present study are available from the corresponding author.
References
World Health Organization. Ending the Neglect to Attain the Sustainable Development Goals: A Road Map for Neglected Tropical Diseases 2021–2030. Geneva, Switzerland: WHO (2020). http://www.who.int/publications/i/item/9789240010352.
Chai, J. Y. & Jung, B. K. General overview of the current status of human foodborne trematodiasis. Parasitology 149, 1262–1285. https://doi.org/10.1017/S0031182022000725 (2022).
Suwannatrai, A., Saichua, P. & Haswell, M. Epidemiology of Opisthorchis viverrini infection. Adv. Parasitol. 101, 41–67. https://doi.org/10.1016/bs.apar.2018.05.002 (2018).
Khieu, V. et al. Is Opisthorchis viverrini emerging in Cambodia?. Adv. Parasitol. 103, 31–73. https://doi.org/10.1016/bs.apar.2019.02.002 (2019).
Yong, T. S. et al. Prevalence of intestinal helminths among inhabitants of Cambodia (2006–2011). Korean J. Parasitol. 52, 661–666. https://doi.org/10.3347/kjp.2014.52.6.661 (2014).
Yong, T. S. et al. High prevalence of Opisthorchis viverrini infection in a riparian population in Takeo Province, Cambodia. Korean J. Parasitol. 50, 173–176. https://doi.org/10.3347/kjp.2012.50.2.173 (2012).
Miyamoto, K. et al. Field survey focused on Opisthorchis viverrini infection in five provinces of Cambodia. Parasitol. Int. 63, 366–373. https://doi.org/10.1016/j.parint.2013.12.003 (2014).
Schär, F. et al. The prevalence and diversity of intestinal parasite infections in humans and domestic animals in a rural Cambodian village. Parasitol. Int. 63, 597–603. https://doi.org/10.1016/j.parint.2014.03.007 (2014).
Sinuon, M., Ananthaphruti, M. T. & Socheat, D. Intestinal helminthic infections in schoolchildren in Cambodia. Southeast Asian J. Trop. Med. Public Health 34, 254–258 (2003).
Ditrich, O., Giboda, M., Scholz, T. & Beer, S. A. Comparative morphology of eggs of the haplorchiinae (Trematoda: Heterophyidae) and some other medically important heterophyid and opisthorchiid flukes. Folia Parasitol. 39, 123–132 (1992).
Chai, J. Y. et al. Echinostoma aegyptica (Trematoda: Echinostomatidae) infection in five riparian people in Savannakhet Province, Lao PDR. Korean J. Parasitol. 58, 67–72. https://doi.org/10.3347/kjp.2020.58.1.67 (2020).
Cho, J. et al. Echinostoma mekongi n. sp. (Digenea: Echinostomatidae) from riparian people along the Mekong River in Cambodia. Korean J Parasitol. 58, 431–443. https://doi.org/10.3347/kjp.2020.58.4.431 (2020).
Shin, H. et al. Molecular detection of Haplorchis pumilio eggs in schoolchildren, Kome Island, Lake Victoria, Tanzania. Emerg. Infect. Dis. 28, 2298–2301. https://doi.org/10.3201/eid2811.220653 (2022).
Chang, T. et al. Morphological and molecular diagnosis of Necator americanus and Ancylostoma ceylanicum recovered from villagers in northern Cambodia. Korean J. Parasitol. 58, 619–625. https://doi.org/10.3347/kjp.2020.58.6.619 (2020).
Chang, T. et al. Molecular diagnosis of Taenia saginata tapeworms from two residents of northern Cambodia. Korean J. Parasitol. 58, 201–204. https://doi.org/10.3347/kjp.2020.58.2.201 (2020).
Chai, J. Y. et al. Prevalence of Heterophyes nocens and Pygidiopsis summa infections among residents of the western and southern coastal islands of the Republic of Korea. Am. J. Trop. Med. Hyg. 71, 617–622 (2004).
Sohn, W. M. et al. Prevalence of Opisthorchis viverrini infection in humans and fish in Kratie Province, Cambodia. Acta Trop. 124, 215–220. https://doi.org/10.1016/j.actatropica.2012.08.011 (2012).
Chai, J. Y. & Hongvanthong, B. A small-scale survey of intestinal helminthic infections among the residents near Pakse, Laos. Korean J. Parasitol. 36, 55–58. https://doi.org/10.3347/kjp.1998.36.1.55 (1998).
Chai, J. Y. et al. High prevalence of liver and intestinal fluke infections among residents of Savannakhet Province in Laos. Korean J. Parasitol. 45, 213–218. https://doi.org/10.3347/kjp.2007.45.3.213 (2007).
Kobayashi, J. et al. An epidemiological study on Opisthorchis viverrini infection in Lao villages. Southeast Asian J. Trop. Med. Public Health 31, 128–132 (2000).
Chai, J. Y. et al. High prevalence of Haplorchis taichui, Prosthodendrium molenkampi, and other helminth infections among people in Khammouane Province in Lao PDR. Korean J. Parasitol. 47, 243–247. https://doi.org/10.3347/kjp.2009.47.3.243 (2009).
Chai, J. Y. et al. Mixed infections with Opisthorchis viverrini and intestinal flukes in residents of Vientiane Municipality and Saravane Province in Laos. J. Helminthol. 79, 283–289. https://doi.org/10.1079/JOH2005302 (2005).
Buathong, S. et al. Molecular discrimination of Opisthorchis-like eggs from residents in a rural community of central Thailand. PLoS Negl. Trop. Dis. 11, e0006030. https://doi.org/10.1371/journal.pntd.0006030 (2017).
Pumidonming, W. et al. Potential risk of a liver fluke Opisthorchis viverrini infection brought by immigrants from prevalent areas: A case study in the lower Northern Thailand. Acta Trop. 178, 213–218. https://doi.org/10.1016/j.actatropica.2017.11.023 (2018).
Laoraksawong, P. et al. Current high prevalences of Strongyloides stercoralis and Opisthorchis viverrini infections in rural communities in northeast Thailand and associated risk factors. BMC Public Health 18, 940. https://doi.org/10.1186/s12889-018-5871-1 (2018).
Mairiang, E. et al. Hepatobiliary morbidities detected by ultrasonography in Opisthorchis viverrini-infected patients before and after praziquantel treatment: A five-year follow up study. Acta Trop. 217, 105853. https://doi.org/10.1016/j.actatropica.2021.105853 (2021).
Sohn, W. M. et al. Low-grade endemicity of opisthorchiasis, Yangon, Myanmar. Emerg. Infect. Dis. 25, 1435–1437. https://doi.org/10.3201/eid2507.190495 (2019).
Forrer, A. et al. Spatial distribution of, and risk factors for, Opisthorchis viverrini infection in Southern Lao PDR. PLoS Negl. Trop. Dis. 6, e1481. https://doi.org/10.1371/journal.pntd.0001481 (2012).
Suwannahitatorn, P., Webster, J., Riley, S., Mungthin, M. & Donnelly, C. A. Uncooked fish consumption among those at risk of Opisthorchis viverrini infection in central Thailand. PLoS ONE 14, e0211540. https://doi.org/10.1371/journal.pone.0211540 (2019).
Pengput, A. & Schwartz, D. G. Risk factors for Opisthorchis viverrini infection: a systematic review. J. Infect. Public Health 13, 1265–1273. https://doi.org/10.1016/j.jiph.2020.05.028 (2020).
Rim, H. J. Opisthorchiasis. In CRC Handbook Series in Zoonoses, Section C. Parasitic Zoonoses. Vol. III (Trematode Zoonoses) 109–121 (CRC Press, Inc., Boca Raton, 1982).
Rim, H. J. Clonorchiasis. In CRC Handbook Series in Zoonoses, Section C. Parasitic Zoonoses. Vol. III (Trematode Zoonoses) 17–32 (CRC Press, Inc., Boca Raton, 1982).
Wilson, W. et al. Heterogeneities in microparasite infections: Patterns and processes. Ecol. Wildl. Dis. 44, 6–44 (2022).
Wattanawong, O. et al. Current status of helminthiases in Thailand: A cross-sectional, nationwide survey, 2019. Acta Trop. 223, 106082. https://doi.org/10.1016/j.actatrropica.2021.106082 (2021).
Elkins, D. B. et al. Opisthorchis viverrini: relationships between egg counts, worms recovered and antibody levels within an endemic community in Northeast Thailand. Parasitology 102, 283–288. https://doi.org/10.1017/S0031182000062600 (1991).
Crellen, T. et al. Diagnosis of helminths depends on worm fecundity and the distribution of parasites within hosts. Proc. R. Soc. B. 290, 20222204. https://doi.org/10.1098/rspb.2022.2204 (2023).
Lovis, L. et al. PCR diagnosis of Opisthorchis viverrini and Haplorchis taichui infection in a Lao community in an area of endemicity and comparison of diagnostic methods for parasitological field surveys. J. Clin. Microbiol. 47, 1517–1523. https://doi.org/10.1128/JCM.02011-08 (2009).
Sato, M. et al. Patterns of trematode infections of Opisthorchis viverrini (Opisthorchiidae) and Haplorchis taichui (Heterophyidae) in human populations from two villages in Savannakhet Province, Lao PDR. J. Helminthol. 89, 439–445. https://doi.org/10.1017/S0022149X14000261 (2015).
Sato, M., Thaenkham, U., Dekumyoy, P. & Waikagul, J. Discrimination of O. viverrini, C. sinensis, H. pumilio, and H. taichui using nuclear DNA-based PCR targeting ribosomal DNA ITS region. Acta Trop. 109, 81–83. https://doi.org/10.1016/j.actatropica.2008.09.015 (2009).
Wongsawad, C., Phalee, A., Noikong, W., Chuboon, S. & Nithikathkul, C. Co-infection with Opisthorchis viverrini and Haplorchis taichui detected by human fecal examination in Chomtong district, Chiang Mai Province, Thailand. Parasitol. Int. 61, 56–59. https://doi.org/10.1016/j.parint.2011.10.003 (2012).
Chai, J. Y. et al. Hyperendemicity of Haplorchis taichui infection among riparian people in Saravane and Champasak Province, Lao PDR. Korean J. Parasitol. 51, 305–311. https://doi.org/10.3347/kjp.2013.51.3.305 (2013).
Buathong, S. et al. Genetic differentiation of Opisthorchis-like eggs in northern Thailand using stool specimens under national strategic plan to control liver fluke infection and cholangiocarcinoma. Am. J. Trop. Med. Hyg. 103, 1118–1124. https://doi.org/10.4269/ajtmh20-0231 (2020).
Acknowledgements
We would like to thank the staff of the National Center for Parasitology and Malaria Control (CNM), Cambodia, for their kind assistance in this project. Special thanks should be given to all participants in this epidemiological study, including village people for fecal examinations and volunteers for adult worm recovery. We also appreciate the Korea Association of Health Promotion (KAHP), Seoul, South Korea for the support for this project.
Author information
Authors and Affiliations
Contributions
B.K.J. contributed to field studies, resources, data collection, data analysis, interpretation, visualization, and writing the manuscript. S.H. performed field studies, data collection, data analysis, and visualization. T.C. performed field studies, data collection, data analysis, interpretation, and visualization. J.C. performed field studies and data collection. S.R. performed field studies, data collection, data analysis, interpretation, and visualization. K.H.L. contributed to administrative support, finance, resources, and field studies. J.L. contributed to administrative support, finance, and resources. W.M.S. performed field studies, data collection, data analysis, and supervision. S.J.H. performed field studies, data collection, data analysis, and supervision. V.K. and R.H. contributed to conceptualization, administrative support, field studies, resources, and supervision. J.Y.C. performed conceptualization, field studies, resources, data collection, data analysis, interpretation, visualization, writing manuscript, and supervision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jung, BK., Hong, S., Chang, T. et al. High endemicity of Opisthorchis viverrini infection among people in northern Cambodia confirmed by adult worm expulsion. Sci Rep 13, 9654 (2023). https://doi.org/10.1038/s41598-023-36544-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-36544-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.