Abstract
This study aimed to (1) set a reference value for anterior center edge angle (ACEA) for preoperative planning of periacetabular osteotomy (PAO), (2) investigate the effects of pelvic rotation and inclination from false profile (FP) radiographs on the measured ACEA, and (3) determine the “appropriate range of positioning” for FP radiograph. This single-centered, retrospective study analyzed 61 patients (61 hips) who underwent PAO from April 2018 and May 2021. ACEA was measured in each digitally reconstructed radiography (DRR) image of the FP radiograph reconstructed in different degrees of pelvic rotation. Detailed simulations were performed to determine the “appropriate range of positioning” (0.67 < ratio of the distance between the femoral heads to the diameter of the femoral head < 1.0). The vertical-center-anterior (VCA) angle was measured on the CT sagittal plane considering the patient-specific standing positions, and its correlation with the ACEA was investigated. The reference value of ACEA was determined by receiver operating characteristic (ROC) curve analysis. The ACEA measurement increased by 0.35° for every 1° pelvic rotation approaching the true lateral view. The pelvic rotation with the “appropriate range of positioning” was found at 5.0° (63.3–68.3°). The ACEA on the FP radiographs showed a good correlation with the VCA angle. The ROC curve revealed that an ACEA < 13.6° was associated with inadequate anterior coverage (VCA < 32°). Our findings suggest that during preoperative PAO planning, an ACEA < 13.6° on FP radiographs indicates insufficient anterior acetabular coverage. Images with the “appropriate positioning” can also have a measurement error of 1.7° due to the pelvic rotation.
Similar content being viewed by others
Introduction
Periacetabular osteotomy (PAO) is a valid surgical option for treating symptomatic developmental dysplasia of the hip (DDH)1,2,3,4,5,6,7. This procedure can be used to correct acetabular coverage three-dimensionally and prevent or delay osteoarthritis progression2,3. Many studies have shown that correcting the lateral acetabular coverage can affect the longevity of the native hip following PAO6,7. However, recent studies have shown that postoperative anterior acetabular coverage has a greater impact on postoperative hip longevity4,5. Furthermore, weight-bearing radiographs are more appropriate for evaluating hip deformity because DDH causes abnormal mechanical loading in the weight-bearing position rather than in the supine position8,9,10. Additionally, patient-specific pelvic inclination should be considered because radiographic measurements are significantly affected by changes in pelvic inclination between the standing and supine positions8,11.
Kitamura et al. performed virtual PAO and reported that anterior acetabular rotation should be considered in addition to lateral rotation in PAO with a preoperative anterior acetabular coverage angle of < 32° in the CT sagittal plane in the patient-specific standing position12. CT is a useful tool to study pelvic morphology in detail, but routine imaging is not performed in all institutions because of the high radiation dose and cost13. In addition, understanding the three-dimensional anatomic features from the two-dimensional radiographs is essential for correcting the acetabular coverage three-dimensionally.
The anterior center edge angle (ACEA) is a commonly used radiographic parameter for evaluating anterior acetabular coverage14,15. The ACEA is the projected angle from the anterolateral margin of the acetabulum as measured using a false profile (FP) radiograph. However, the ACEA has not been used as a valuable parameter for preoperative planning, and there is no clear reference value. The reason is that radiographic measurements are affected by the pelvic position16,17,18. As originally reported by Lequesne and de Size15, the following criterion for “appropriate range of positioning” has been used widely: the horizontal distance between the medial aspects of the femoral heads was between 67 and 100% of the femoral head (Fig. 1). However, few studies have examined the validity of this criterion in detail17. Moreover, there is a need to understand the extent of the measurement error that will occur within the range of rotation that is judged to be appropriate.
FP radiographs of different pelvic rotations are shown in (a–c). ACEA is measured in a FP radiograph at 65°of rotation (b). Investigated the “appropriate range of positioning” where the distance-to-diameter ratio is between 0.67 (a: 68.1°of rotation) and 1.0 (c: 63.2°of rotation). The arrows indicate the distance between the femoral heads and the femoral head diameter. ACEA Anterior center edge angle, FP False profile.
Therefore, this present study had the following objectives: to use three-dimensional (3D) computer simulations to (1) set a valid reference value for the preoperative planning of PAO, (2) investigate the effects of pelvic rotation and inclination from FP radiographs on the measured ACEA, and (3) determine the “appropriate range of positioning”.
Methods
Patient selection and data acquisition
This is a case series with a level of evidence of 4. Eighty-four consecutive patients (91 hips) who underwent PAO for symptomatic DDH between April 2018 and May 2021 were included in this study. All of the patients were Japanese. The indications for PAO included both clinical symptoms (hip pain that interfered with daily activities) and radiological evidence of DDH (a lateral center–edge angle [LCEA] of < 20°, a Tönnis angle of > 10°, and a sharp angle of > 45°19,20,21,22) or borderline dysplasia (defined by an LCEA between 20° and 25°21,22). In seven patients with bilateral PAO during this period, only the first operated side was included. Twenty-one patients were excluded because they had a history of hip surgery on the contralateral side. Two patients with images of insufficient quality for analysis were also excluded. After eligibility assessment, 61 patients (61 hips) were enrolled in this study (Fig. 2).
Supine and standing anteroposterior (AP) pelvic radiographs and CT images were obtained during preoperative planning of PAO. Preoperative transverse CT scans (Aquilion ONE; Canon Medical Systems Corporation, Tochigi, Japan) of the whole pelvis and femur (from the top of the iliac crest to the distal femur) were obtained in all patients with a 512 × 512 image matrix, a 0.35 × 0.35 pixel dim, and a 1-mm thickness. The patients were placed supine on a scanning table and instructed to naturally extend their affected hip and knee joints. The CT images were acquired using digital imaging and communications in medicine (DICOM) format data from the CT system server. The supine and standing radiographs were investigated using Fujifilm OP-A software (Fujifilm, Co., Ltd, Tokyo, Japan).
Definition of the pelvic 3D coordinate system in the standing position
The DICOM datasets were imported into 3D planning software (3D template; Kyocera, Osaka, Japan). First, the pelvic 3D coordinate system was defined based on the anterior pelvic plane (APP)11,23. The pubic tuberosity was defined as the origin, and the APP, including the pubic tuberosity and bilateral anterior superior iliac spines, was defined as the coronal plane. Next, the pelvis was realigned in the sagittal plane to simulate patient-specific pelvic inclination in the standing position. Digitally reconstructed coronal radiographs considering the patient-specific standing positions were created so that the vertical-to-horizontal ratio of the pelvic foramen matched the standing radiograph by incrementally adjusting the projection angle11,23,24 (Fig. 3a, b). Changes in sagittal pelvic inclination in the standing position relative to the APP were measured, and a positive value indicated anterior pelvic inclination (Fig. 3c).
DRR image (a) and standing radiograph (b). Adjust the pelvic inclination (c) so that the vertical-to-horizontal ratio of the pelvic foramen is the same between (a) and (b). The arrows indicate the vertical distance between the bilateral sacroiliac joints and pubic symphysis and the maximum horizontal diameter of the pelvic foramen. The pelvic inclination was defined as the angle between the solid line (z-axis) and the dotted line (APP). (d) VCA angle was measured as the angle between the vertical line and a line connecting the femoral head center and the anterior end of the acetabulum after adjustment to the standing position. The dotted line indicates APP. (e) DRR image of the FP radiograph (rotating AP image 65° in the axial plane), ± 5° and ± 10°relative to the FP radiograph (rotating AP image 55°, 60°, 70°, 75°in the axial plane). Indicates a change of sourcil edge with pelvic rotation. The ACEA was measured for each DRR image. DRR Digitally reconstructed radiography, APP Anterior pelvic plane, VCA Vertical-center-anterior, FP False profile, AP Anterior–posterior, ACEA Anterior center edge angle.
Evaluation of anterior acetabular coverage in the CT sagittal plane
After adjustment to the patient-specific standing position, the anterior acetabular coverage in the CT sagittal plane was measured as the angle between (1) the line connecting the center of the femoral head and the anterior end of the acetabular roof and (2) the line from the center of the femoral head vertically25. This angle was defined as the vertical-center-anterior (VCA) angle in the sagittal CT plane (Fig. 3d). According to a previous study12, a VCA angle < 32° in the sagittal CT plane after adjustment to the standing position is defined as inadequate anterior coverage.
DRR image reconstruction and measurement of the center–edge angle
Consequently, the DRR image of the FP radiograph was reconstructed by rotating the AP image in the standing position to 65° in the axial plane. This DRR image was defined as an FP radiograph with neutral rotation (NR). Then, DRR images rotated by ± 5° and ± 10° in the axial plane relative to the neutral FP radiographs (at 55°, 60°, 70°, and 75° from the AP view; Fig. 3e) were reconstructed. The positive value of pelvic rotation was defined as rotation toward the affected side, approaching a true lateral view. Finally, various pelvic inclination was simulated. DRR images of each pelvic inclination were reconstructed by tilting the pelvis ± 5° and ± 10° from the patient-specific standing position and then rotating the pelvis 65° in the axial plane. The positive value of pelvic inclination was defined as an anterior pelvic inclination. The ACEA was measured for each DRR image. The ACEA is defined as the angle between (1) the line from the center of the femoral head, perpendicular to the transverse axis of the pelvis, and (2) the line from the center of the femoral head to the most anterior edge of the acetabular sourcil2,17,26.
Examination of the “appropriate range of positioning”
Detailed validation of the “appropriate range of positioning” criteria17 was performed. In each DRR image, the diameter of the femoral head and the horizontal distance between the medial aspects of the femoral heads were measured. The distance-to-diameter ratio, which is the ratio of the horizontal distance to the femoral head diameter, was calculated according to a previous study17. Pelvic rotation was simulated in increments to determine the axial rotation angle corresponding to distance-to-diameter ratios of 0.67 and 1.0.
Statistical analysis
Data analysis of the ACEA measurement for each DRR image in different pelvic rotations was conducted using repeated-measures analysis of variance. Correlations between the VCA angle in the CT sagittal plane (after adjustment to the standing position) and ACEA with NR were investigated using Pearson’s correlation coefficient analysis, and the reference value of ACEA with inadequate anterior coverage (VCA angle < 32°) was investigated by receiver operating characteristic (ROC) analysis. Statistical analyses were performed using JMP statistical analysis software (version 15.0; SAS Institute, Cary, NC, USA), and statistical significance was set at p < 0.05. To evaluate intra-observer and interobserver reproducibility, measurements were performed twice by one examiner (Y.K.) and once by another examiner (S.K.) in the study group. The intraclass correlation coefficient and the interclass correlation coefficient were good 0.89 to 0.97 and 0.84 to 0.94, respectively) for all measurements.
Ethics approval and consent to participate
This retrospective study was approved by Kyushu University institutional review board for clinical research (No. 30-137) and was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients prior to the study.
Results
Patient demographics and radiographic data are shown in Table 1. The standing pelvic inclination was -0.24°. After adjustment to the standing position, the VCA angle in the sagittal CT plane was 32.8° on average, of which 26 hips (43%) had a VCA angle < 32°. The ACEA on the FP radiographs with NR was 16.8° on average, which showed a good correlation (r = 0.71, p < 0.001) with the VCA angle in the CT sagittal plane after adjustment to the standing position (Fig. 4a). Receiver operating characteristic (ROC) curves indicated that an ACEA with NR < 13.6° was associated with inadequate anterior coverage (sensitivity 69%, specificity 89%, area under the curve 0.85) (Fig. 4b).
(a) Correlations among the VCA angle in the CT sagittal plane and the ACEA on the FP radiograph with neutral rotation. (b) The receiver operating characteristic curve for inadequate anterior coverage with the ACEA in FP radiograph. The cut-off value of the ACEA was 13.6° (sensitivity 69%, specificity 89%, area under the curve 0.85). VCA Vertical-center-anterior, ACEA Anterior center edge angle, FP False profile.
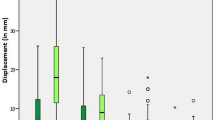
In the simulation of pelvic rotation, the ACEA measurement increased by 0.35° for every 1° increment approaching the true lateral view (Fig. 5a). In the simulation of pelvic inclination, the ACEA measurement increased by 0.68° for every 1° increment of anterior inclination (Fig. 5b). The rotational pelvic positions that met the “appropriate range of positioning” (0.67 < distance-to-diameter ratio < 1.0) were found in the range of 5.0° between 63.3° and 68.3°. Pelvic rotation for all patients meeting the "appropriate range of positioning" criteria were shown in Fig. 6. Fifty-five hips (90.2%) met the “appropriate range of positioning” criteria for the FP radiographs with NR.
(a) The line plots show the values of ACEA (mean and standard deviation) for each pelvic rotation. (b) The line plots show the values of ACEA (mean and standard deviation) for each pelvic inclination. The positive value of pelvic inclination was defined as an anterior pelvic inclination. ACEA Anterior center edge angle.
Discussion
The present study showed a good correlation (r = 0.71) between the ACEA on the FP radiographs and the VCA angle in the CT sagittal plane after adjustment to the patient-specific standing position. In contrast, a previous study reported no significant correlation between ACEA on the FP radiograph and anterior acetabular coverage in the CT sagittal plane25. This inconsistency can be explained by the fact that the previous studies did not consider patients-specific pelvic inclination in the standing position and that the pelvic rotation was not strictly adjusted during radiography. In the present study, a good correlation was found by precisely matching the pelvic rotation and inclination. Although the FP radiographs are useful for diagnosing dysplasia and detecting the joint space15, studies reporting valid reference values of ACEA for preoperative planning for PAO have been scarce. Preoperative planning requires evaluation of the anterior acetabular coverage. Kitamura et al. performed virtual PAO and developed finite-element models to simulate joint contact pressure12. Although normal joint contact pressure was achieved in 63% of patients by lateral acetabular rotation in that study, the anterior rotation should be additionally considered in patients with a VCA < 32° in the CT sagittal plane after adjustment to the standing position. In the present study, ROC curve analysis showed that patients with an ACEA < 13.6° on FP radiographs had low anterior coverage corresponding to < 32° on sagittal CT, with a good area under the curve, sensitivity, and specificity. This reference value can evaluate anterior acetabular coverage on standing radiographs. Moreover, CT is not routinely performed for preoperative planning in all institutions because of the high radiation dose and cost. For patients with ACEA less than 13.6° on FP radiographs, detailed preoperative planning using CT images is recommended for three-dimensional acetabular correction. To the best of our knowledge, this is the first study to set a reference value for ACEA in FP radiographs for preoperative planning of PAO taking the standing condition into account.
As pelvic rotation increased (approaching a true lateral view), the more anterior part of the acetabular rim is projected as the sourcil edge27 (Fig. 3e), and the ACEA increased by 0.35° for every degree of increased rotation. This effect was also observed in previous studies. Ryan et al. conducted a study on the effect of pelvic rotation and reported an approximately 0.3° change in ACEA with every degree of rotation in 11 cadaver pelvises17. Putnam et al. reported changes in ACEA of 0.18° with every degree of rotation on eight hips of four cadaveric pelvises18. Previous studies included cadavers without dysplasia, whereas the current study is the first to investigate pelvic dysplasia. Compared to the current study, the slight difference in values in the previous studies may be due to the type of study subjects enrolled. However, as pelvic inclination increased (anterior inclination), the ACEA measurement increased by 0.68° for every 1° of anterior inclination. Putnam et al. also reported changes in ACEA of 0.65° for 1° inclination and that the FP radiograph is a standing radiograph, wherein patients were instructed not to assume a forced posture during the radiographic examination18. The radiographs also ensure that the patient's anatomy is functionally represented and minimize the influence of inclination on the ACEA measurements. The patient should be positioned in a natural standing position so that the radiograph accurately represents the patient's anatomy.
The “appropriate range of positioning” criterion from Lequesne and de Seze has been conventionally used to exclude inappropriate images. Putnam first examined this criterion using eight cadaver hips18. The position was rotated by 5°, and the measurements were repeated to validate the criterion. They reported that all cases met the criteria with an obliquity between 60° and 70°. The criterion was fulfilled in 55 hips (90.2%) of the 61 hips of FP radiographs taken at the 65° oblique position. The criteria reported by Lequesne and de Seze may be useful for selecting inappropriate images. Whereas previous reports used a small number of cadavers for validation, in the present study, we performed further simulations using a large number of CT images to determine the rotation range that met the criteria in each case. The results showed that the average optimal range was 5.0° (63.3–68.3°). Therefore, when evaluating an image with the “appropriate range of positioning” it is necessary to assume a variation of 1.7° (0.35 × 5) due to pelvic rotation.
This study had limitations. First, this study population was limited to Japanese patients. Second, most patients in the study population were females. Female patients are reported to have more acetabular dysplasia than male patients28. However, Japanese patients with hip osteoarthritis have been reported to differ from Caucasians in terms of sex distribution and frequency of acetabular dysplasia as an etiology29. The results may therefore not be generalizable to different races. Third, in patients with severe acetabular dysplasia, when LCEA < 0°, the VCA angle cannot be measured because the acetabulum cannot contact the femoral head in the CT sagittal plane through the center of the femoral head. Previous reports have treated these cases by assuming anterior hip coverage of 0°30 or excluded these cases31. Although none of the patients in this study had such severe acetabular dysplasia (LCEA < 0°), our results may not apply to patients with such severe acetabular dysplasia.
In conclusion, during preoperative planning of PAO, an ACEA < 13.6° on FP radiographs indicates insufficient anterior acetabular coverage. Images with the “appropriate range of positioning” can also have a measurement error of 1.7° due to pelvic rotation. Therefore, when evaluating radiographs, it is important to note these measurement errors.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Ibrahim, M. M., Smit, K., Poitras, S., Grammatopoulos, G. & Beaulé, P. E. Correlation of patient-reported outcomes after periacetabular osteotomy with femoral head coverage and acetabular orientation: A single-center cohort study. Am. J. Sports Med. 49, 1209–1219 (2021).
Hasegawa, Y., Iwase, T., Kitamura, S., Kawasaki, M. & Yamaguchi, J. Eccentric rotational acetabular osteotomy for acetabular dysplasia and osteoarthritis: Follow-up at a mean duration of twenty years. J. Bone Joint Surg. Am. 96, 1975–1982 (2014).
Fujii, M. et al. Effect of intra-articular lesions on the outcome of periacetabular osteotomy in patients with symptomatic hip dysplasia. J. Bone Joint Surg. Br. 93, 1449–1456 (2011).
Wyles, C. C. et al. Hitting the target: Natural history of the hip based on achieving an acetabular safe zone following periacetabular osteotomy. J. Bone Joint Surg. Am. 102, 1734–1740 (2020).
Stetzelberger, V. M. et al. The acetabular wall index is associated with long-term conversion to THA after PAO. Clin. Orthop. Relat. Res. 479, 1052–1065 (2021).
Albers, C. E., Steppacher, S. D., Ganz, R., Tannast, M. & Siebenrock, K. A. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin. Orthop. Relat. Res. 471, 1602–1614 (2013).
Hartig-Andreasen, C., Troelsen, A., Thillemann, T. M. & Søballe, K. What factors predict failure 4 to 12 years after periacetabular osteotomy?. Clin. Orthop. Relat. Res. 470, 2978–2987 (2012).
Henebry, A. & Gaskill, T. The effect of pelvic tilt on radiographic markers of acetabular coverage. Am. J. Sports Med. 41, 2599–2603 (2013).
Pullen, W. M., Henebry, A. & Gaskill, T. Variability of acetabular coverage between supine and weightbearing pelvic radiographs. Am. J. Sports Med. 42, 2643–2648 (2014).
Troelsen, A., Jacobsen, S., Rømer, L. & Søballe, K. Weightbearing anteroposterior pelvic radiographs are recommended in DDH assessment. Clin. Orthop. Relat. Res. 466, 813–819 (2008).
Tachibana, T., Fujii, M., Kitamura, K., Nakamura, T. & Nakashima, Y. Does acetabular coverage vary between the supine and standing positions in patients with hip dysplasia?. Clin. Orthop. Relat. Res. 477, 2455–2466 (2019).
Kitamura, K. et al. Is anterior rotation of the acetabulum necessary to normalize joint contact pressure in periacetabular osteotomy? A finite-element analysis study. Clin. Orthop. Relat. Res. 480, 67–78 (2022).
Furlow, B. Radiation dose in computed tomography. Radiol. Technol. 81, 437–450 (2010).
Lequesne, M. False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies. Rev. Rhum. Mal. Osteoartic. 28, 643–652 (1961).
Lequesne, M. G. & Laredo, J. D. The faux profil (oblique view) of the hip in the standing position. Contribution to the evaluation of osteoarthritis of the adult hip. Ann. Rheum. Dis. 57, 676–681 (1998).
Li, P. L. S. & Ganz, R. Morphologic features of congenital acetabular dysplasia: One in six is retroverted. Clin. Orthop. Relat. Res. 416, 245–253 (2003).
Li, R. T. et al. Does pelvic rotation alter radiologic measurement of anterior and lateral acetabular coverage?. Arthroscopy 35, 1111-1116.e1 (2019).
Putnam, S. M., Clohisy, J. C. & Nepple, J. J. Do changes in pelvic rotation and tilt affect measurement of the anterior center edge angle on false profile radiographs? A cadaveric study. Clin. Orthop. Relat. Res. 477, 1066–1072 (2019).
Clohisy, J. C. et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J. Bone Joint Surg. Am. 90(Suppl 4), 47–66 (2008).
Welton, K. L., Jesse, M. K., Kraeutler, M. J., Garabekyan, T. & Mei-Dan, O. The anteroposterior pelvic radiograph: Acetabular and femoral measurements and relation to hip pathologies. J. Bone Joint Surg. Am. 100, 76–85 (2018).
Freiman, S. M., Schwabe, M. T., Fowler, L., Clohisy, J. C. & Nepple, J. J. Prevalence of borderline acetabular dysplasia in symptomatic and asymptomatic populations: A systematic review and meta-analysis. Orthop. J. Sports Med. 10, 23259671211040456 (2022).
Kraeutler, M. J. et al. A contemporary look at the evaluation and treatment of adult borderline and frank hip dysplasia. Am. J. Sports Med. 48, 2314–2323 (2020).
Nishihara, S., Sugano, N., Nishii, T., Ohzono, K. & Yoshikawa, H. Measurements of pelvic flexion angle using three-dimensional computed tomography. Clin. Orthop. Relat. Res. 411, 140–151 (2003).
Kitamura, K. et al. Does patient-specific functional pelvic tilt affect joint contact pressure in hip dysplasia? A finite-element analysis study. Clin. Orthop. Relat. Res. 479, 1712–1724 (2021).
Zingg, P. O. et al. The anterior center edge angle in Lequesne’s false profile view: Interrater correlation, dependence on pelvic tilt and correlation to anterior acetabular coverage in the sagital plane. A cadaver study. Arch. Orthop. Trauma. Surg. 129, 787–791 (2009).
Hanson, J. A. et al. Discrepancies in measuring acetabular coverage: Revisiting the anterior and lateral center edge angles. J. Hip Preserv. Surg. 2, 280–286 (2015).
Mozingo, J. D., Schuring, L. L., Mortensen, A. J., Anderson, A. E. & Aoki, S. K. Effect of patient positioning on measurement of the anterior center-edge angle on false-profile radiographs and its 3-dimensional mapping to the acetabular rim. Orthop. J. Sports Med. 10, 23259671211073830 (2022).
Iidaka, T. et al. Prevalence of radiographic hip osteoarthritis and its association with hip pain in Japanese men and women: the ROAD study. Osteoarthr. Cartil. 24, 117–123 (2016).
Jingushi, S. et al. Multiinstitutional epidemiological study regarding osteoarthritis of the hip in Japan. J. Orthop. Sci. 15, 626–631 (2010).
Kamenaga, T. et al. Pelvic morphology medial to the femoral head center predicts anterior coverage and range of motion after curved periacetabular osteotomy. J. Orthop. Res. 38, 2031–2039 (2020).
Cheng, H., Zhang, L., Luo, D. & Ren, N. Determining anterior hip coverage in patients with hip dysplasia using the anterior center-edge angle on Lequesne’s false-profile radiograph and on computed tomography. J. Hip Preserv. Surg. 00, 1–6 (2023).
Acknowledgements
The authors would like to thank Editage (www.editage.jp) for the English language review.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Y.K. and S.K. performed the literature review and drafted the manuscript. Y.N. supervised writing of the manuscript. K.K., S.H., G.M., S.I., T.S., R.Y., D.H., and M.F. contributed to the data collection. Y.K. and S.K. analyzed the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kokubu, Y., Kawahara, S., Kitamura, K. et al. Evaluation of the anterior acetabular coverage with a false profile radiograph considering appropriate range of positioning. Sci Rep 13, 8288 (2023). https://doi.org/10.1038/s41598-023-35514-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-35514-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.