Abstract
An important challenge relating to clinical diagnostics of the foodborne pathogen Shiga toxin-producing E. coli (STEC), is that PCR-detection of the shiga-toxin gene (stx) in DNA from stool samples can be accompanied by a failure to identify an STEC isolate in pure culture on agar. In this study, we have explored the use of MinION long-read sequencing of DNA from bacterial culture swipes to detect the presence of STEC, and bioinformatic tools to characterize the STEC virulence factors. The online workflow “What’s in my pot” (WIMP) in the Epi2me cloud service, rapidly identified STEC also when it was present in culture swipes together with multiple other E. coli serovars, given sufficient abundance. These preliminary results provide useful information about the sensitivity of the method, which has potential to be used in clinical diagnostic of STEC, particularly in cases where a pure culture of the STEC isolate is not obtained due to the ‘STEC lost Shiga toxin’ phenomenon.
Similar content being viewed by others
Introduction
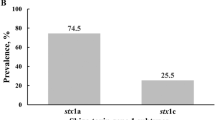
Shiga toxin-producing Escherichia coli (STEC) are foodborne pathogens capable of causing severe gastrointestinal and systemic disease1. STEC genomes are complex and contain many virulence genes on plasmids, bacteriophages and insertion sequences. Shiga toxin encoding genes (stx1/stx2) are located on different prophages that integrate into the E. coli genome, and their toxin products are essential for development of hemorrhagic colitis and hemolytic uremic syndrome2,3. Detection of stx1 and/or stx2 is, therefore, commonly used in clinical diagnostics as a marker of the pathotype of E. coli STEC. Primary diagnostic laboratories in Norway have switched from culture-based diagnostics to PCR-based detection of gastrointestinal pathogens directly in stool samples4,5. Detection of stx1/stx2 in stool DNA is usually followed up by selective culture plating, and a culture swipe is assessed for toxigenic potential by the same PCR assay. Finally, detection of stx1/stx2 in the culture swipe will typically lead to testing of multiple single colonies to identify the STEC isolate in pure culture6. However, failure to identify an STEC isolate in pure culture is not uncommon7,8. There are several possible reasons for failure to isolate STEC on agar from stx-positive swipes: for example, activation of stx expression and induction into the phage lytic cycle will result in cell lysis and low concentrations of intact STEC cells3. Furthermore, in the presence of a competitive microbiota (e.g., commensal E. coli), recovery of an STEC isolate on an agar plate may be technically challenging9. Additionally, stx may spontaneously excise from the genome without subsequent cell lysis, resulting in E. coli without integrated stx; a phenomenon which has been termed ‘STEC lost shiga toxin’—STEC-LST (10). A mix of STEC and STEC-LST colonies on agar renders the recovery of an stx-positive isolate difficult10,11,12,13. Finally, the absence of STEC growth on agar following a positive stx-PCR could be due to presence of free stx-phages, rather than STEC cells in the patient’s stool sample, suggesting that the patient is not in fact infected with STEC14.
As a guideline for choice of patient treatment and infection control measures, accurate diagnostics to identify whether a patient is infected with STEC, or simply a carrier of free stx-phages, is important. Furthermore, classification of STEC serotype and pathotype is paramount during an outbreak incident. Many public health agencies currently employ Next Generation Sequencing (NGS) to characterize isolates of foodborne pathogens such as STEC, in order to obtain specific information on serotype and virulence factors15,16. Short-read sequencing platforms like Illumina MiSeq or NextSeq are widely used, and the technology provides sequence data with high accuracy. Short read sequencing has, however, limitations with respect to the assembly of repetitive regions and regions showing high similarity in a genome that can range up to hundreds of kilobases17. Recently, Oxford Nanopore Technologies’ MinION small sequencing device was evaluated and found to be an accurate and economical option for whole genome sequencing of STEC isolates18. The technology is also well-suited for use by primary diagnostic laboratories, and the long reads obtained with MinION may be particularly useful in resolving cases with STEC-LST or samples with multiple strains. The long reads are likely to overlap and may facilitate a positive identification of the genome of interest as well as enable its characterization with respect to pathogenic potential. In this study, we have evaluated the use of long-read sequencing with MinION for the detection of STEC in culture swipes harboring different combinations of STEC and STEC-LST and other E. coli strains. The purpose of the investigation was to evaluate the usefulness of the method to identify the STEC serotype and pathotype present in cases where recovery of a pure STEC isolate by culture techniques is unsuccessful following a positive stx-PCR. This study provides a useful first set of experiments to obtain an indication of the sensitivity of the method, but is not a real substitute for data from clinical samples.
Material and methods
Bacterial strains
Escherichia coli representing four different serotypes and pathotypes were used in the experiments: Shiga toxin producing E. coli (STEC) O145:H28, Enteropathogenic E. coli (EPEC) O21, E. coli (EAEC) O104:H4 and an extraintestinal pathogenic E. coli (ExPEC) O6:H31. The O145:H28 isolate was also used as an STEC-LST variant that had lost the stx gene. STEC O145:H28 was previously characterized by our group13. Virulence genes of typical EPEC O21 and EAEC O104:H4 were determined by Clondiag GmbH using microarray technology (Clondiag GmbH, Jema, Germany).
Preparation of bacterial inoculums and DNA extraction
All strains were cultured on lactose agar. To mimic the diagnostic procedure under evaluation, DNA was extracted from mixed bacterial growth on agar in three different combinations as follows. In experiment 1, one loopful of bacterial colonies from STEC-LST O145:H28 and a pinpoint amount of colony material from STEC O145:H28 were suspended in PureLink® lysisbuffer (Thermo Fisher Scientific, Waltham, MA, USA) for DNA extraction. In experiment 2, one loopful of bacterial colonies from each of the following strains was suspended in lysis buffer: STEC O145:H28, STEC-LST O145:H28, EAEC O104:H4, EPEC O21 and ExPEC O6:H31. Experiment 3 was similar to experiment 2 except for that STEC O145:H28 (with stx) was added in a smaller amount (pinpoint of colony material). Figure 1 illustrates the experimental setup. PureLink® Genomic DNA extraction kit (Thermo Fisher Scientific) was used for DNA extraction, and DNA concentrations were measured using Qubit 4 Fluorometric quantification (ThermoFisher Scientific) employing the dsDNA Broad Range Assay according to the manufacturer’s instructions. Nanodrop™ 2000 (Thermo Fisher Scientific) was used to control for impurities (ratios 260/280 and 260/230).
Experimental setup and summary of main results from the study. Three experiments were performed with different relative abundances of E. coli strains. After sequencing with MinION, the online workflow WIMP was used to identify E. coli strains or serotypes. Sequence reads were then assembled to confirm stx integration in an E. coli genome.
qPCR quantification
To mimic the diagnostic procedure under evaluation, DNA extraction was performed from mixed bacterial growth on agar plates, and the relative abundance of each strain was subsequently quantified with specific qPCR assays. Shiga toxin (stx) qPCR was used to quantify STEC19, while a PCR assay targeting the virulence factor ehxA was used as a measure for total quantities of STEC O145:H28 and STEC-LST O145:H2820. PCR assays targeting O21, O104 and cnf1 were used to quantify EPEC O21, EAEC O104:H4 and ExPEC O6:H31, respectively21,22,23. TaqMan PCR-assays were performed using BrilliantIII UltraFast qPCR mix (Agilent Technologies Inc, Santa Clara, CA, USA) with the following cycling parameters: Initiation 3 min 95 °C, 40 cycles with 15 s 95 °C and 30 s 60 °C. SYBR Green PCR assays were performed using Quantifast SYBR Green PCR kit (Qiagen, Hilden, Germany) with the following cycling parameters: initiation 5 min 95 °C, 40 cycles with 10 s 95 °C, 30 s 56 °C and 30 s 72 °C. Primer and probe concentrations were 200 nM and 400 nM, respectively. Primer/probe sequences, PCR efficiencies and amplicon size for all PCR assays used in this study are listed in Table 1.
Analytical sensitivity and PCR efficiency tests were performed for each PCR assay, using tenfold serial dilutions of DNA from pure bacterial cultures containing from 4 ng/µl to 0.04 pg/µl. Standard curves were constructed and used for PCR efficiency calculations and to quantify the different E. coli in the samples. Specificity tests were carried out by cross-testing the different E. coli isolates in each of the strain-specific PCR assays.
MinION whole genome sequencing
Whole genome sequencing of DNA from the different E. coli combinations was performed using a minION MK1b device and the Rapid Barcoding Sequencing Kit (SQK-RBK004) (Oxford Nanopore Technologies, Oxford, GB), according to the manufacturer’s protocol. For each of the three experiments, approximately 400 ng DNA was loaded onto a R9.4 MinION Flow Cell (FLO-MIN107). The sequencing run was performed through the minKNOW platform using the MIN107 SQK-RBK004 protocol. The run time was 24 h.
Processing of sequence data
Basecalling of minION sequencing data was performed using Albacore version 1.2.4 (https://github.com/Albacore/albacore). FASTQ sequences were uploaded to the Epi2me cloud service and analyzed with the workflow “What’s in my pot” (WIMP) (Epi2me, Oxford nanopore technologies) which uses the RefSeq sequence database at NCBI (https://www.ncbi.nlm.nih.gov/refseq/) for identification24. PoreChop version 0.2.3 (https://github.com/rrwick/Porechop) was used for adapter trimming of the sequence reads. De novo assembly was performed with Canu version 1.625 and quality reports for assembled contigs were generated using QUAST26.
In silico detection of virulence genes, phages, pathogenic potential, and serotyping
FASTA-files with assembled contigs from each sequencing run were submitted to the Centre for Genomic Epidemiology (CGE) (http://www.genomicepidemiology.org). The web-based tools VirulenceFinder 1.527 and PathogenFinder28 were used to identify virulence genes and assess the pathogenic potential of strains. Sequences were also submitted to the typing services SerotypeFinder29 and MLSTFinder30. The threshold used for ID was 90%, and minimum length of overlap was set to 60%.
Results
Relative abundances of E. coli strains in different experiments
Three experiments with different combinations of each E. coli strain were performed; these are summarized in Fig. 1. After DNA extraction, quantification of each E. coli strain was performed using strain-specific qPCR assays. In experiment 2, each E. coli was present in similar quantities, while in experiments 1 and 3, the relative quantities of STEC O145:H28 were respectively 10 and 50 times lower than that of the other E. coli strains (Fig. 1). No cross-reactions were observed for any of the qPCR assays and PCR efficiencies were between 89 and 108% (Tables S1 and S2).
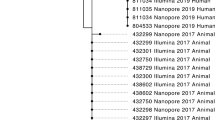
MinION sequencing and Epi2me real-time data analysis
The MinION sequencing platform provided between 2.3 and 2.5 Gbp data output and sequence reads with average read lengths of 10 kB in all three experiments. The average quality score for the sequencing reads was 10. The WIMP workflow in the Epi2me cloud service correctly identified E. coli O145:H28 in experiment 1. E. coli O145:H28 was the only serotype present in this experiment as a combination of STEC and STEC-LST (ie, with and without the stx gene). In experiments 2 and 3, with four different E. coli serotypes, WIMP identified two of them, namely E. coli O104:H4 and E. coli O45:H28. Neither E. coli O6:H31 nor E. coli serotype O21 were identified by WIMP in any of these two experiments. Results are presented in Table 2.
De novo sequence assembly
In experiment 1, Canu25 assembled the sequencing reads into one single large contig similar in size to an E. coli genome (5.4 Mbp), accompanied by two smaller contigs of 141,573 and 142,342 nucleotides. In experiments 2 and 3, with several different E. coli strains, the sequencing reads were assembled into 135 and 160 contigs, respectively. QUAST26 showed that the largest contig in experiment 2 was 573,742 nucleotides and that 128 contigs were larger than 50,000 nucleotides. In experiment 3, the largest contig was 535,013 nucleotides and 125 contigs were larger than 50,000 (Table 2). All sequence data have been made available through Figshare https://doi.org/10.6084/m9.figshare.21342453.
Detection of virulence genes and pathogenic potential
The sequence assemblies from Canu25 were used to assess the pathogenic potential of the strains. PathogenFinder28 predicted that the input organism(s) were human pathogens in all the experiments. VirulenceFinder29 detected important STEC virulence genes in experiment 1, for example Shiga-toxin encoding gene (stx), Enterohaemolysin gene (ehxA), Adherence-conferring molecule gene (iha) and Tir-cytoskeleton coupling protein gene (tccP) (Table 2). For the two experiments with several different E. coli, the program detected multiple virulence genes associated with STEC, EAEC, EPEC and ExPEC (Table 2). However, in experiment 3 stx was not identified in any of the contigs after de novo assembly. Unassembled FASTQ files from experiment 3 were also submitted to VirulenceFinder, but the stx gene was not identified in any of the reads. Results from VirulenceFinder and PathogenFinder are summarized in Table 2.
In silico serotyping and MLST analysis
The assembled contigs were also analysed with SerotypeFinder28 and MLSTFinder30. These are programs designed to determine the O-and H serotype and MLST-types of single strains. The SerotypeFinder only identified one O-gene in each experiment but indicated several H-genes. MLSTFinder correctly identified the MLST type of STEC in experiment 1. Results from SerotypeFinder, MLSTFinder and PlasmidFinder are summarized in Table 2.
A protocol to identify STEC in culture swipes
Based on the results, a protocol was suggested to improve diagnostics of STEC in samples which are stx PCR-postive and culture negative (Fig. 2).
Suggested protocol for clinical diagnostics of STEC with minION sequencing of DNA extracted from culture swipes. Real-time integrated basecalling allows for direct upload of sequence reads to the Epi2me cloud service and WIMP workflow. The suggested procedure results in identification of STEC serotype in less than 24 h. For further characterization of the STEC genome, FASTQ files can be assembled and online tools such as VirulenceFinder will identify virulence factors. If a near complete genome can be assembled and stx is detected in it, the presence of STEC is confirmed. If de novo assembly results in multiple smaller contigs, indicative of multiple E. coli, stx may still be identified as described. However, sequence typing and detailed characterization of the STEC isolate will be difficult.
Discussion
Several studies have reported challenges associated with the confirmation of stx PCR-positive stool samples. Subsequent culture of the stx-positive strain is advised for verification of the PCR-result and for strain characterization and infection control measures. When an STEC isolate cannot be cultured, the situation is described as the ‘STEC PCR-positive/culture-negative phenomenon’6,7. To identify the STEC isolate, several rounds of selective plating may be necessary. The repeated plating passages may lead to induction of the phage lytic cycle, or to spontaneous excision of the prophage from the STEC genome without subsequent cell lysis, resulting in STEC-LST. Consequently, the number of STEC with intact prophages will be limited, and, therefore, difficult to detect by culture and stx PCR-testing of single colonies. Loss of stx during laboratory work is a well-known phenomenon10,11,12,13.
This study investigated the use of MinION sequencing technology and the proposed protocol to identify STEC in bacterial culture swipes, in cases where recovery of a pure STEC isolate is unsuccessful. When DNA from a swipe of STEC and STEC-LST was sequenced, the Epi2me workflow WIMP rapidly identified the well-known STEC serotype O145:H28. De novo assembly resulted in one large genome-sized contig, in which all STEC virulence factors were identified by user-friendly online tools from CGE, even though only 10% of the E. coli in the sample were STEC with intact stx. Additionally, SerotypeFinder identified the correct serotype and MLSTFinder identified the correct multi-locus sequence type, thus illustrating the usefulness of the proposed protocol in samples with STEC and STEC-LST.
The protocol was further evaluated with culture swipes with different E. coli serotypes. In these experiments, WIMP rapidly identified the two E. coli that may cause severe gastrointestinal disease: STEC serotype O145:H28 and EAEC serotype O104:H4. E. coli serotype O6:H31 and EPEC O2 were not identified by WIMP, most likely because no O6:H31 genomes and only three O2 genomes are defined at assembly level as “complete” in the NCBI RefSeq database, which is used by WIMP24,31. De novo sequence assembly resulted in more than 100 sequence contigs, indicating the presence of more than one E. coli strain. In experiment 2, with similar abundances of four different E. coli strains, several STEC virulence genes (stx and others) were identified by VirulenceFinder27, confirming STEC in the sample. Due to the presence of more than one E. coli strain in the sample, no result from MLSTFinder was obtained, and, therefore, genotyping of the STEC could not be achieved. Nevertheless, the approach can be used to confirm the presence of STEC in mixed E. coli populations. In experiment 3, where STEC was present as approximately 2% of total E. coli, the stx gene was not detected by VirulenceFinder. Based on the MinION sequencing output (2.5 Gb) for this sample, which contained four different E. coli genomes (estimated total genome size > 20 Mb), a theoretical sequencing coverage of approximately 100 should be expected. The stx gene was present in significantly lower quantities (2%) than that of the other DNA-sequences, and it is, therefore, likely that the stx sequence reads could have been omitted in the de novo assembly process, or simply not sequenced at all. This suggests that when the abundance of STEC is significantly lower than that of non-STEC E. coli, the proposed procedure will not positively confirm STEC. Nevertheless, with detection of a well-known STEC serotype, the presence of STEC-LST should be considered.
In this study, we have evaluated the usefulness of MinION whole genome sequencing of E. coli from culture swipes for the purpose of confirming STEC. The results provide information about the sensitivity of the method, which potentially could be useful in cases where a STEC-isolate is not obtained following a positive stx-PCR. The protocol could potentially also be applicable to resolve other diagnostic challenges. For example, to differentiate the gastrointestinal pathogens Shigella spp. and enteroinvasive E. coli (EIEC). The invasion plasmid antigen H gene (ipaH), present in both these pathogens, is often used as a qPCR target. Culture and identification of single colonies is, therefore, necessary for identification, but is not always possible32. When neither Shigella nor EIEC can be retrieved after culture of an ipaH PCR-positive stool sample, the proposed protocol using MinION sequencing could be considered.
A concern with the MinION nanopore sequencing technology is its higher error rate when compared to short-read sequencing technologies. This problem was highlighted by Gonzales-Escalona et al.18, who compared E. coli sequencing results using three different technologies and found that data from MinION contained several artificial indels. Still, the authors successfully characterized the STEC isolates with respect to virulence genes, plasmids, and antibiotic resistance genes, results also supported by Taylor et al.33. Different programs and algorithms have been presented to improve the quality of MinION data and to enable detailed SNP phylogenetic analyses34. Additional bioinformatic analysis could be considered if the purpose is beyond presence/absence analysis of specific genes. This was not the purpose of the present study and was therefore not performed. Recently, Maguire et al.35 demonstrated that complete STEC genomes could be identified in spiked water samples using a metagenomic approach and the MinION technology. Results from the present study support previous reports of the usefulness of MinION sequencing and illustrate that the technology may also be useful for STEC identification in culture swipes with multiple strains. A limitation of the present work is that the protocol described has been developed and validated using only a limited number of strains and serovars. The workflow should in later work be tested against a larger panel of especially clinical isolates and starting with fecal material naturally containing or spiked with STEC.
Conclusion
In conclusion, the results from this study provide preliminary data about the use of MinION sequencing technology supported by user-friendly online web-tools to identify STEC in mixed samples. The protocol could be particularly useful in cases of PCR-positive/culture-negative samples caused by loss of stx, and it is possible that detailed characterization of the STEC genome can be obtained in samples containing both STEC and STEC-LST. The procedure is easy to implement in routine diagnostic laboratories and the instrumentation and consumables are affordable. However, more comprehensive analyses with different STEC serotypes are required to confirm the results from this study. Furthermore, the data presented are not a real substitute for data from clinical samples, and the protocol requires further testing using clinical samples to evaluate its true potential in clinical diagnostics.
Data availability
All sequence data have been made available through Figshare. https://doi.org/10.6084/m9.figshare.21342453 or https://figshare.com/articles/dataset/Genome_assembly_of_E_coli_strain_mixes/21342453.
References
Tarr, P. I., Gordon, C. A. & Chandler, W. L. Shiga toxin-producing Escherichia coli and haemolytic uremic syndrome. Lancet 365, 1073–1086 (2006).
Koudelka, G. B., Arnold, J. W. & Chkraborty, D. Evolution of STEC virulence: Insights from the antipredator activities of shiga toxing-producing E. coli. Int. J. Med. Microbiol. 308, 956–961 (2018).
Waldor, M. K. & Friedman, D. I. Phage regulatory circuits and virulence gene expression. Curr. Opin. Microbiol. 8(4), 459–465 (2005).
Jenssen, G. R. et al. Implementation of multiplex PCR diagnostics for gastrointestinal pathogens linked to increase of notified Shiga toxin-producing Escherichia coli cases in Norway. Eur. J. Clin. Microbiol. Infect. Dis. 38, 801–809 (2019).
Tunsjø, H. S. et al. Suitability of stx-PCR directly from fecal samples in clinical diagnostics of STEC. APMIS 123(10), 872–878 (2015).
Lassen, J., Hovig, B. & Sandven, P. Bacteriological Stool Analyses. Report from Strategy Meeting No. 10 (Norwegian Institute of Public Health, 1996). Revised 2007 and 2011. https://www.fhi.no/globalassets/dokumenterfiler/rapporter/strategirapporter/strategirapport-nr-10-1996-bakteriologiske-faecesundersokelser-med-revisjoner-fra-2007-og-2011-.pdf
Macori, G., McCarthy, S., Burgess, C. M., Fanning, S. & Duffy, G. Investigation of the causes of shigatoxigenic Escherichia coli PCR positive and culture negative samples. Microorganisms 8(4), 587 (2020).
Noll, L. W. et al. Comparison of culture and PCR-based methods to detect six major non-O157 serogroups of shiga toxin-producing Escherichia coli in cattle feces. PLoS ONE 10(8), e0135446 (2015).
Duffy, G., Whiting, R. & Sheridan, J. The effect of a competitive microflora, pH and temperature on the growth kinetics of Escherichia coli O157:H7. Food Microbiol. 16, 299–307 (1999).
Bielaszewska, M. et al. Shiga toxin gene loss and transfer in vitro and in vivo during enterohemorrhagic Escherichia coli O26 infection in humans. Appl. Environ. Microbiol. 73(10), 3144–3150 (2007).
Mellmann, A. et al. Recycling of Shiga toxin 2 genes in sorbitol fermenting enterohemorrhagic Escherichia coli O157:NM. Appl. Environ. Microbiol. 74(1), 67–72 (2008).
Karch, H., Meyer, T. & Rüssmann, J. Frequent loss of Shiga-like toxin genes in clinical isolates of Escherichia coli upon subcultivation. Infect. Immun. 60, 3464–3467 (1992).
Senthakumaran, T. et al. Implications of stx loss for clinical diagnostics of Shiga toxin-producing Escherichia coli. Eur. J. Clin. Microbiol. Infect. Dis. 37, 2361–2370 (2018).
Martinez-Castillo, A., Quirós, P., Navarro, F., Miró, E. & Muniesa, M. Shiga toxin 2-encoding bacteriophages in human fecal samples from healthy individuals. Appl. Environ. Microbiol. 79, 4862–4868 (2018).
Allard, M. W. et al. Genomics of foodborne pathogens for microbial food safety. Curr. Opin. Biotechnol. 49, 224–229 (2018).
Dallman, T. J. et al. The utility and public health implications of PCR and whole genome sequencing for the detection and investigation of an outbreak of Shiga toxin-producing Escherichia coli serogroup O26:H11. Epidemiol. Infect. 143, 1672–1680 (2015).
Bertrand, D. et al. Hybrid metagenomic assembly enables high-resolution analysis of resistance determinants and mobile elements in human microbiomes. Nat. Biotechnol. 37, 937–944 (2019).
González-Escalona, N., Allard, M. A., Brown, E. W., Sharma, S. & Hoffmann, M. Nanopore sequencing for fast determination of plasmids, phages, virulence markers, and antimicrobial resistance genes in Shiga toxin-producing Escherichia coli. PLoS ONE 14(7), e0220494 (2019).
Nielsen, E. M. & Andersen, M. T. Detection and characterization of verotoxin-producing Escherichia coli by automated 5’nuclease PCR-assay. J. Clin. Microbiol. 41, 2884–2893 (2003).
Bugarel, M., Beutin, L. & Fach, P. Low-density macroarray targeting non-locus of enterocyte effacement effectors (nle Genes) and major virulence factors of Shiga toxin-producing Escherichia coli (STEC): A new approach for molecular risk assessment of STEC isolates. Appl. Environ. Microbiol. 76(1), 203–211 (2010).
Li, D. et al. A multiplex PCR method to detect 14 Escherichia coli serogroups associated with urinary tract infections. J. Microbiol. Met. 82(1), 71–77 (2010).
Delannoy, S., Beutin, L., Burgos, Y. & Facha, P. Specific detection of enteroaggregative hemorrhagic Escherichia coli O104:H4 strains by use of the CRISPR locus as a target for a diagnostic real-time PCR. J. Clin. Microbiol. 50(11), 3485–3492 (2012).
Gómez-Moreno, R., Robledo, I. E. & Baerga-Oritiz, A. Direct detection and quantification of bacterial genes associated with inflammation in DNA isolated from stool. Adv. Microbiol. 4(15), 1065–1075 (2014).
Juul, S. et al. What’s in my pot? Real-time species identification on the MinION™. BioRxiv 2015, 030742 (2015).
Koren, S. et al. Canu: scalable and accurate long-read assembly via adaptive k-mer weighting and repeat separation. Genome Res. 27, 722–736 (2017).
Gurevich, A., Saveliev, V., Vyahhi, N. & Tesler, G. QUAST: quality assessment tool for genome assemblies. Bioinformatics 29(8), 1072–1075 (2013).
Joensen, K. G. et al. Real-time whole-genome sequencing for routine typing, surveillance, and outbreak detection of verotoxigenic Escherichia coli. J. Clin. Microbiol. 52, 1501–1510 (2014).
Cosentino, S., Larsen, M. V., Aarestrup, F. M. & Lund, O. PathogenFinder: Distinguishing friend from foe using bacterial whole genome sequence data. PLoS ONE 8(10), e77302 (2013).
Joensen, K. G., Tetzschner, A. M. M., Iguchi, A., Aarestrup, F. M. & Scheutz, F. Rapid and easy in silico serotyping of Escherichia coli isolates by use of whole-genome sequencing data. J. Clin. Microbiol. 53(8), 2410–2426 (2015).
Larsen, M. et al. Multilocus sequence typing of total genome sequenced bacteria. J. Clin. Microbiol. 50(4), 1355–1361 (2012).
Imai, K. et al. Rapid and accurate species identification of mitis group streptococci using the MinION nanopore sequencer. Front. Cell Infect. Microbiol. 10, 11 (2020).
Okeke, I. N., Aboderin, A. O. & Opintan, J. A. Enteroinvasive Escherichia coli may account for uncultured Shigella. Am. J. Trop. Med. Hyg. 94, 480–481 (2016).
Taylor, T. et al. Rapid, multiplexed, whole genome and plasmid sequencing of foodborne pathogens using long-read nanopore technology. Sci. Rep. 9(1), 1–11 (2019).
Jain, M. et al. Improved data analysis for the MinION nanopore sequencer. Nat. Methods 12(4), 351–356 (2015).
Maguire, M. et al. Precision long-read metagenomics sequencing for food safety by detection and assembly of Shiga toxin-producing Escherichia coli in irrigation water. PLoS ONE 16(1), e0245172 (2021).
Funding
This study was financed by Oslo Metropolitan University.
Author information
Authors and Affiliations
Contributions
Conceptualization H.S.T., I.F.U., C.C. Methodology: H.S.T., I.F.U. Interpretation of data: H.S.T., I.F.U., C.C. Writing—original draft preparation: H.S.T, I.F.U., C.C. Funding acquisition: H.S.T, C.C. All authors agree to the publication of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tunsjø, H.S., Ullmann, I.F. & Charnock, C. A preliminary study of the use of MinION sequencing to specifically detect Shiga toxin-producing Escherichia coli in culture swipes containing multiple serovars of this species. Sci Rep 13, 8239 (2023). https://doi.org/10.1038/s41598-023-35279-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-35279-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.