Abstract
In medical trials, ‘blinding’ ensures the equal distribution of expectancy effects between treatment arms in theory; however, blinding often fails in practice. We use computational modelling to show how weak blinding, combined with positive treatment expectancy, can lead to an uneven distribution of expectancy effects. We call this ‘activated expectancy bias’ (AEB) and show that AEB can inflate estimates of treatment effects and create false positive findings. To counteract AEB, we introduce the Correct Guess Rate Curve (CGRC), a statistical tool that can estimate the outcome of a perfectly blinded trial based on data from an imperfectly blinded trial. To demonstrate the impact of AEB and the utility of the CGRC on empirical data, we re-analyzed the ‘self-blinding psychedelic microdose trial’ dataset. Results suggest that observed placebo-microdose differences are susceptible to AEB and are at risk of being false positive findings, hence, we argue that microdosing can be understood as active placebo. These results highlight the important difference between ‘trials with a placebo-control group’, i.e., when a placebo control group is formally present, and ‘placebo-controlled trials’, where patients are genuinely blind. We also present a new blinding integrity assessment tool that is compatible with CGRC and recommend its adoption.
Similar content being viewed by others
Introduction
In medical research the gold standard experimental design is the blinded randomized controlled trial1, where ‘blinding’ refers to the concealment of the intervention2. The purpose of blinding is to equally distribute expectancy effects between treatment arms3, thus, to eliminate biases associated with expectancy. ‘Blinding integrity’ refers to how successfully blinding is maintained. Blinding integrity can be assessed by asking blinded parties, e.g., patients and/or doctors, to guess treatment allocation. If the correct guess rate (CGR) is higher than chance, then, blinding is ineffective. Assessing blinding integrity could be especially important when outcomes are subjective, for example in pain and psychiatric research, where there is a high susceptibility to expectation biases4. In these domains, only 2–7% of trials report blinding integrity and when blinding is assessed, it is found to be ineffective for about 50% of the trials5,6,7,8,9.
Poor reporting of blinding integrity may be explained by at least three factors. First, there is no accepted standard for how to assess blinding integrity. Most commonly, patients are asked to guess their treatment after the trial has concluded, but such data may be subject to recall and other biases10,11,12. Secondly, there is no accepted standard for how to incorporate blinding integrity into data analysis. Even if blinding integrity is assessed, most scientific reports do not attempt to incorporate blinding integrity data into the interpretation of the results. Finally, others have speculated that a reluctance to assess blinding stems from a fear that weak blinding could cast doubt on positive trial outcomes5. Supporting this reasoning, lesser blinding integrity reporting has been associated with industry sponsorship6,9.
There is a resurgent interest in the medicinal potential of psychedelic drugs, such as LSD and psilocybin13. Recently, ‘microdosing’ has emerged as a new paradigm for psychedelic use. Microdosing does not have a universally accepted definition, but most microdosers take oral doses of 10–20 μg LSD or 0.1–0.3 g of dried psilocybin containing mushrooms, 1–4 times a week14. Anecdotal claims have been made that microdosing improves well-being and cognition15,16. Observational studies have generally confirmed the positive anecdotal claims17,18,19,20, but so far placebo-controlled studies have failed to find robust evidence for larger than placebo efficacy in healthy samples21,22,23,24,25.
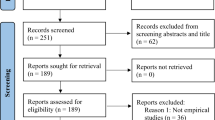
We recently conducted a ‘self-blinding citizen science trial’ on microdosing, where participants implemented their own placebo control based on online setup instructions without clinical supervision24. The strength of this design is twofold: it tested the effects of microdosing in a real-life context, increasing the trial’s external validity26, and it allowed us to obtain a large sample size while implementing placebo control at minimal logistic and economic costs. The study was completed by 191 participants, making it the largest placebo-controlled trial on psychedelic microdosing for a fraction of the cost of even a small traditional clinical trial.
Methods
Activated expectancy bias (AEB) model
We introduce a theoretically motivated computational model of AEB, the model’s structure and equations are shown on Fig. 1, the key model features are:
-
The presence or lack of side effects allow patients to infer their treatment at a higher than chance rate. The correct guess probability, \({p}_{CG}\), in the model is 0.7, which is consistent with both microdosing21,24 and antidepressants27,28,29 trials.
-
AEB model parameters are calibrated such that the treatment effect is 3 points, corresponding to a small-moderate effect size of 0.4 standardized mean difference, which is consistent with microdosing21,22,24 and antidepressant trials30, numeric parameters can be found in Supplementary Table 1.
-
Patients have higher efficacy expectations for the active treatment than for placebo treatment, this positive expectancy bias is represented by the \({N}_{AEB}\) term in the model, see Fig. 1.
The activated expectancy bias (AEB) model, consisting of 3 binary nodes (TRT, PT and TE) and a continuous value node, the outcome (OUT). In the equations, \({B}_{X} / {N}_{X}\) stand for a random Bernoulli/normal variable, respectively. The binary nodes (TRT, PT and TE) represent Bernoulli variables (BTRT, BPT, BTE), where the values of 0/1 correspond to placebo/active. To generate AEB model data, first Treatment (TRT) is determined by Eq. 1 and then the Perceived treatment (PT) by Eq. 2, where \({p}_{CG}\) is the probability of correct guess, i.e. the correct guess rate, and then Treatment expectancy is fixed according to Eq. 3. Finally, the outcome score is calculated by Eq. 4 which has components of natural history (\({N}_{NH}\)), direct treatment effect (\({N}_{DTE}\)) and activated expectancy bias (\({N}_{AEB}\)), see Supplementary table 1 for the numeric value of all parameters.
The AEB model was used to generate pseudo-experimental data with 2*2 = 4 parameter configurations, corresponding to direct treatment effect and activated expectancy bias being either active or not, see Fig. 1. In our analysis the direct treatment effect (blue)/activated expectancy bias (red) pathways are turned off by setting the mean \({N}_{DTE}\)/\({N}_{AEB}\) equal to 0. For each configuration, 500 trials were simulated, each with 230 patients, mimicking the sample size of the microdose trial analyzed.
Self-blinding microdose trial
The self-blinding microdose trial used an 'self-blinding' citizen science approach, where participants implemented their own placebo control based on online setup instructions without clinical supervision24. Self-blinding involved enclosing the microdoses inside non-transparent gel capsules and using empty capsules as placebos. Then, these capsules were labeled with QR codes that allowed investigators to track when placebo/microdose was taken without sharing this information with participants. Participants were followed throughout a 4-week dosing period, taking 2 microdoses/week in the active group. For each capsule taken, participants made a binary guess whether their capsule was placebo or microdose, see Supplementary materials for details.
Here, the trial’s acute and post-acute outcomes are re-analyzed. Acute measures were completed 2–6 h after ingestion of the capsule, while post-acute measures were taken the day after a capsule was taken. Acute outcomes were: positive and negative affect schedule (PANAS)31, cognitive performance score (CPS) and visual analogue scale items for mood, energy, creativity, focus, and temper. The CPS is an aggregated quantification of cognitive performance based on 6 computerized tasks (spatial span, odd one out, mental rotations, spatial planning, feature match, paired associates). Post-acute outcomes were: Warwick–Edinburgh mental well-being scale (WEMWB)32, quick inventory of depressive symptomatology (QIDS)33, state-trait anxiety inventory (STAIT)34 and social connectedness scale (SCS)35. To simplify the current analysis, we only used data from the first week of the experiment, thus, each datapoint is independent and not confounded by order effects. This approach reduced the overall sample, but yielded almost identical qualitative conclusion as the full dataset. In the current analysis n = 233 datapoints were included.
The trial only engaged people who planned to microdose through their own initiative, but who consented to incorporate placebo control to their self-experimentation. The trial team did not endorse microdosing or psychedelic use and no financial compensation was offered to participants. The study was approved by Imperial College Research Ethics Committee and the Joint Research Compliance Office at Imperial College London (reference number 18IC4518). Informed consent was obtained from all subjects, the trial was carried out in accordance with relevant guidelines and regulations.
Estimate of treatment effects
Throughout this work treatment effects are estimated by an outcome ~ treatment linear model, where outcome is a numeric, treatment is a binary variable (placebo or active treatment). In this manuscript ‘non-CGR adjusted analysis’ means that this model is fitted to empirical data, while ‘CGR adjusted analysis’ means that this model is fitted to the CGR adjusted pseudo-experimental data, see Correct guess rate curve section for details. Therefore, the CGR-adjusted treatment estimate/p-value is to the estimate/p-value associated with the treatment term in the model above, applied to data adjusted by the CGRC method. All linear models were implemented using the lme package (version 3.1–155) in R (v4.0.2).
Correct guess rate curve
We developed CGR adjustment, a novel statistical technique that can estimate the outcome of a perfectly blinded trial, based on data from an imperfectly blinded trial. Briefly, first the scores are separated into four strata corresponding to all four possible combinations of treatment and guess. Next, statistical models of these four strata are built using kernel density estimation (KDE). KDE estimates were implemented by the scikit-learn package (v1.0.2) in python (v3.7), all parameters were left at default value. Then, random samples are drawn from each strata, such that the combined sample has CGR = 0.5, mimicking a perfectly blinded trial, see Fig. 2 for a detailed explanation. Treatment estimates for other CGR values can be obtained in a similar manner by changing the number of samples drawn from each KDE. For example, a trial with CGR = 0.6 can be approximated by drawing 0.6*n random samples from the correct guess KDEs and 0.4*n random samples from the incorrect guess KDEs, etc.
Correct guess rate (CGR) adjustment to estimate the outcome of a perfectly blinded trial based on data from an imperfectly blinded trial. First, scores (purple histogram at top) are separated into four strata corresponding to all possible combinations of treatment and guess. Both treatment and guess are binary with potential values of placebo/active, thus, the four strata are (using the treatment/guess notation): PL/PL, AC/PL, PL/AC and AC/AC. Next, statistical models of these strata are built using kernel density estimation (KDE). Note that two strata correspond to correct guesses (PL/PL and AC/AC; red) and two to incorrect guesses (AC/PL, PL/AC; blue). Next, n/2 random samples are drawn from the correct guess KDEs, such that the relative sample sizes of the correct guess strata are preserved, i.e. the ratio nPL/PL/nAC/AC is same as in the original data, see Supplementary materials for a numeric example. Similarly, n/2 random samples are drawn from the incorrect guess KDEs, such that the ratio nAC/PL/nPL/AC is same as in the original data. These random samples are then combined, resulting in a pseudo-experimental dataset with CGR = 0.5 (purple distribution at bottom), corresponding to effective blinding. The random sampling from KDEs is repeated 100 times, for each CGR-adjusted pseudo-experimental dataset is analyzed to estimate the direct treatment effect, see Estimate of treatment effects. The ‘CGR adjusted treatment effect/p-value’ is the mean treatment estimate / p-value across these 100 samples. Estimates at other CGR values can be obtained similarly, e.g. a trial with CGR = 0.6 can be approximated by drawing 0.6*n random samples from the correct guess KDEs and 0.4*n random samples from the incorrect guess KDEs, etc.
Results
Correct guess rate (CGR) adjustment of the activated expectancy bias (AEB) model
We analyze pseudo-experimental data generated by the 2*2 = 4 configurations of the AEB model (corresponding to direct treatment effect and activated expectancy bias either being active or not, see Fig. 1) with both traditional, i.e. non-CGR adjusted, and CGR-adjusted analysis. To demonstrate that the qualitative conclusions presented here do not require fine tuning of parameters, we present a robustness analysis in the Supplementary Materials.
First, the case was analyzed where neither direct treatment effect nor the activated expectancy bias pathways are activated (top row in Table 1). In this case, the outcome is a normal random variable. The treatment p-value was significant for 5%/6% of the simulated trials using the traditional/CGR adjusted models, which is expected based on the 0.05 significance level.
Correct guess rate (CGR) curves of the activated expectancy bias (AEB) model. Each panel shows the estimated treatment p-value (blue; scale shown on left y-axis) and effect size (red; scale shown on right y-axis), with their corresponding confidence interval, as a function of CGR. Horizontal purple dashed line represents the p = .05 significance threshold, vertical green dashed line corresponds to the simulated trial’s original CGR, while the black dashed line corresponds to a perfectly blinded trial (CGR = 0.5). The model was analyzed with 2*2 = 4 configurations of parameters, corresponding to the possibilities of the direct treatment effect (DTE) and activated expectancy bias (AEB) either being active or inactive, see Fig. 1. For the DTE off; AEB on case (bottom left) generates a false positive finding when CGR is not considered during analysis (green dashed line intersects p-value estimate below 0.05), but CGR adjustment recovers the lack of treatment effect (black dashed line intersects p-value estimate above 0.05). For the DTE on; AEB on case (bottom right), both analyses correctly identify that there is a treatment effect; however, non-CGR adjusted analysis overestimates the effect size by ~ 40%, see Table 1 for numeric results.
Next, the case was analyzed where a direct treatment effect was active, but activated expectancy bias was not active (second row from top in Table 1). Non-CGR adjusted and CGR adjusted analysis identifies a significant treatment effect in 86/84% of the simulations with an average p-value of 0.032/0.036, respectively. We note that this 14%/16% false negative rate is due to the small effect used in simulations (~0.4 Hedges’ g), larger effects decrease the false negative rate of both analyses, see robustness analysis in Supplementary materials. In both analysis the treatment estimate is within 5% of the true effect.
Next, the case was analyzed where a direct treatment effect was inactive, but activated expectancy bias was active (third row from top in Table 1), i.e. a scenario where there is no true treatment effect and activated expectancy is a complete mediator of the treatment. For the traditional models, 78% of the simulated trials resulted in a false positive treatment effect. For the CGR-adjusted models, only 3% of the simulated trials produced a false positive treatment effect.
Finally, the case was analyzed where both a direct treatment effect and activated expectancy bias were active (bottom row in Table 1), i.e., a case where AEB is a partial mediator of treatment. The average treatment p-value was 0.001/0.041 with 99%/82% of the trials resulting a significant treatment effect for the traditional/CGR adjusted analysis, respectively. Note that the CGR adjusted analysis can only be as good to detect a treatment effect as the unadjusted analysis when only DTE is active (as the adjustment aims to remove the effect of AEB). Thus, CGR adjusted analysis detects an effect in just 4% less of the simulations (86% vs. 82%) than this best-case scenario, i.e. CGR adjustment only adds 4% to the false negative rate. Furthermore, the traditional analysis estimated the effect to be 5.69 points, while the CGR adjusted estimate was 3.04 points (the true treatment effect was 3), so traditional analysis significantly overestimated the effect due to the influence of AEB. In summary, the CGR adjusted analysis’ false negative rate is ~2-4% higher than the traditional analysis’ (rows 2&4 in Table 2), but the false positive rate is ~75% lower when AEB is present (row1&3 in Table 2). Furthermore, when a true effect is present, CGR provides a more reliable estimate of the effect size (row 4 in Table 2) as it subtracts the influence of AEB.
Correct guess rate (CGR) adjusted analysis of the self-blinding microdose trial
Next, we advance from analyzing pseudo-experimental data to scrutinizing empirical data from the self-blinding microdose trial24. Using traditional, i.e. non-CGR adjusted, data analysis, statistically significant placebo-microdose differences were observed on the following scales: acute emotional state (PANAS; mean difference ± SE = 3.2 ± 1.3; p = 0.01**), energy visual analogue scale VAS (11.5 ± 2.7; p < 0.001***), mood VAS (6.4 ± 2.7; p = 0.02*), creativity VAS (6.4 ± 2.5; p = 0.01*) and post-acute depression (QIDS; − 1.2 ± 0.06; p = 0.04*).
After CGR adjustment, none of these outcomes remained significant with the exception of the energy VAS that remained significant (p ~ 0.04), but with a ~ 40% reduced effect size.
This finding suggests that microdosing increases self-perceived energy beyond what is explainable by expectancy effects, although the magnitude of the remaining effect is small (Hedges’ g = 0.34). Equivalence testing for all outcomes where significance changed after CGR adjustment (i.e. PANAS, QIDS, mood and creativity VASs) with an equivalence bound equal to the average within-subject variability were significant, arguing that outcomes were equivalent in the placebo and microdose groups after the CGR adjustment, see Supplementary materials for details. See Table 2 for numeric results and Fig. 4 for the CGR curves of selected outcomes.
Correct guess rate (CGR) curves for self-blinding microdose trial outcomes. Each panel shows the estimated treatment p-value (blue; scale shown on left y-axis) and effect size (red; scale shown on right y-axis), with their corresponding confidence interval, as a function of CGR. Horizontal purple dashed line represents the p = .05 threshold, vertical green dashed line corresponds to the trial’s original CGR (= 0.72), while the black dashed line corresponds to a perfectly blinded trial (CGR = 0.5). Outcomes in the top row (Positive and Negative Affection Scale (PANAS) and Mood visual analogue scale) are significant according to unadjusted analysis (green dashed line intersects p-value estimate below 0.05), but become insignificant after CGR adjustment (black dashed line intersects p-value estimate above 0.05), arguing that these findings could be false positives driven by AEB. Energy VAS remains significant even after CGR adjustment, although the effect size is reduced by ~ 40%. This finding suggests that microdosing increases self-perceived energy beyond what is explainable by expectancy effects, although the remaining effect is small (Hedges’ g = .34). Finally, CGR adjustment has little impact on the cognitive performance score as both the p-value and the effect estimate remain close to a constant. This finding suggests that this measure is not affected by AEB, possibly because cognitive performance was not self-rated, rather measured by objective computerized tests, see Table 2 for numerical results.
Treatment guess questionnaire
In the supplementary materials we included a brief, 5-items questionnaire developed to collect treatment guess and source of unblinding data. The resulting data is compatible with the current and planned future versions of the CGR curve.
Discussion
Effective blinding distributes expectancy effects equally between treatment arms3. However, if blinding is ineffective, i.e. patients can deduce their treatment allocation, and if patients have a positive expectancy bias for the active arm, then expectancy effects will be no longer equally distributed and trial outcomes will be biased towards the active arm. We call this bias ‘activated expectancy bias’ (AEB), which can be viewed as a residual expectancy bias potentially present even in ‘blinded’ trials. A key consequence is that the research community needs to distinguish between trials with a placebo-control group, i.e., when a placebo control group is formally present in the trial, and placebo-controlled trials, where patients are genuinely blinded and thus AEB is not present. In other words, a placebo control group is necessary, but in-itself insufficient to control for expectancy effects. For example, a recent trial on LSD therapy includes ‘double-blind, placebo-controlled’ in its title, but as the manuscript describes "only one patient in the LSD-first group mistook LSD as placebo” (out of 18 patients), highlighting that the trial was formally blinded, but not in practice36. The implication is that ‘placebo-controlled’ studies are more fallible than conventionally assumed with consequences for evidence-based medicine.
Current FDA drug approval only requires two trials with statistically significant drug-placebo difference37, thus, the self-blinding microdose trial yielded evidence consistent with FDA approval, despite that the findings were likely false positives, driven by AEB. In our view, placebo-controlled trials should only be considered ‘gold standard’ if blinding integrity is demonstrated with empirical data. This requirement would create a new, more rigorous standard for what is ‘placebo control’. Given the high costs and low success rate of psychiatric trials38, there may be little appetite from industry and regulators to create such new standard, but it should be embraced by the scientific community.
We note that it is difficult to estimate how prevalent AEB is in medical trials, because blinding integrity has only been reported in 2–7% of trials5,6,9. To understand the prevalence of AEB, more trials need to capture blinding integrity data39. To aid this practice, in the supplementary materials we suggest a brief 5-items questionnaire that is compatible with the method presented here and recommend its adoption.
When the self-blinding microdose trial was analyzed traditionally, small, but significant microdose-placebo differences were observed on emotional state, depression, mood, energy and creativity, favoring microdosing24. After CGR adjustment, only energy VAS remained significant (p ~ 0.04) with a ~ 40% reduced effect size—we note that another recent trial similarly found significant increases in self-perceived energy beyond what is explainable by the placebo and expectancy effects40. One could argue that these negative results are false negatives; however, the consistency of the negative results across measures argues against this possibility. Furthermore, the trial had the necessary features for AEB, i.e. weak blinding and a positively biased24, implying that the trial is susceptible to AEB. AEB is likely to be present in other psychedelic microdose trials as well, results should be interpreted with caution, especially if evidence for effective blinding is not presented.
We hypothesize that the reported benefits psychedelic microdosing on mood and creativity can be understood as an ‘active placebo’, i.e., an intervention without medical benefits, but with perceivable effects36,39,40, emphasizing the difference between effects and benefits. A recent comprehensive review of microdosing concluded that: “These findings together provide clear evidence of psychopharmacological effects. That is, microdosing is doing something. A key question for researchers is whether the effects of microdosing have clinical or optimization benefits beyond what might be explained by placebo or expectation.”41. In short, microdosing leads to perceivable effects, for example by the heightened energy levels, explaining why CGR is universally high across trials21,24,40, but at this point none of these effects seem to be related improved mental health. If our hypothesis is correct, then, either improved blinding or a sample without positive expectancy would nullify the observed benefits of microdosing by nullifying AEB. An alternative possibility is that microdosing is only effective at doses where blinding integrity cannot be maintained due to conspicuous subjective effects, such as in the case of psychedelic macrodosing42. In this scenario the possibility of effective placebo control is abandoned and efficacy beyond expectancy needs to be established outside of blinded trials. Arguments for the merit of alternative trial designs to assess the efficacy of psychedelics have been made before43, for example mechanistic studies could also help to establish the causal effect of treatment. Recently, arguments against the value of placebo control have been raised in psychedelic trials44. This article remains neutral on this issue, it merely insists that if a trial is called ‘placebo controlled', then it should really control for the placebo effect and not just have a ‘placebo group'.
Our arguments above assume that the high CGR is explained by malicious unblinding, i.e. positive treatment expectancy drives the positive outcomes, rather than benign unblinding, i.e. patients correctly guess their treatment due to noticeable health improvements45. If unblinding is benign, then CGR adjustment could lead to false negative findings due to collider bias46 (currently Fig. 1 represents malicious unblinding, for benign unblinding PT → TE → OUT would need to be replaced with OUT → PT). Accordingly, investigators need to carefully assess the source of unblinding prior to using our method. To facilitate this assessment, our questionnaire in the supplementary materials captures this source of unblinding information.
What was the source of unblinding in the self-blinding psychedelic microdose trial? Two lines of evidence point towards that it was the perceptual/side effects rather than efficacy, corresponding to malicious unblinding. First, 55% reported that the primary cue to formulate their treatment guess was ‘body/perceptual sensations’, such as muscle tension (58%) and stomach discomfort (27%), in contrast only 23% reported ‘mental/psychological benefits’. Secondly, among participants who were assessed under both placebo and microdose conditions, the mean placebo-microdose difference on the positive / negative affect subdomains of the PANAS was 2.1/0.8. In a recent study without any intervention, the mean temporal intra-individual difference, i.e. the within-subject day-to-day variability, of the same subdomains was ~ 10/~ 647. Thus, the natural within-subject variability is ~ 500–750% larger than the mean placebo-microdose difference, arguing that the effect is too small to be noticeable.
Limitations
CGR adjustment relies on binary treatment guess data from patients, however, treatment belief is a complex construct that cannot be reduced to a single binary variable. We focused on binary guess data due to its availability and note that even this imperfect data is rare to find. Treatment guess could be better characterized if guess confidence was also rated. Such confidence data would allow to distinguish between those who truly identified their drug condition (high confidence guess) versus those who guess correctly by chance (low confidence guess).
In our analysis, we treat the source of unblinding as a binary variable, either being only benign or malicious. A more realistic scenario is that for some patients, both efficacy and non-specific effects contribute to their guesses. Relatedly, our assessment on the source of unblinding is based on retrospective self-reports, that cannot provide conclusive evidence on causation.
Our AEB model assumes linear addition of the direct treatment and the activated expectancy effects to estimate the total effect, however, these effects may not be additive for all circumstances48.
The CGR curve relies on resampling the observed data, thus, the resulting data cannot be considered experimentally randomized, and as a consequence confounding variables may not be equally distributed. Despite the KDE approximation of each strata, practically some datapoints may appear multiple times in the pseudo-experimental samples, potentially increasing the error rate due to dependent observations. The error rate of our methodology is a function of the sample characteristics, generally, the smaller the sample, the more extreme the CGR and the smaller the effects are, the less reliable the results will be. In a range of these parameters that mimics microdosing and antidepressant trials (n ~ 200, CGR ~ 0.7, treatment effect ~ 0.4 Hedges’ g), our method has comparable false negative rate as traditional, non-CGR adjusted analysis. However, when AEB is present CGR adjusted analysis has a much lower false positive rate and a more reliable estimate of the true effect size compared to non-CGR adjusted analysis. The error rate of our methodology can be higher in other contexts, in particular if the sample is small. Researchers wishing to use CGR adjustment should first run simulations to determine whether CGR produces acceptable error rates for the parameters of their data and the application in mind. For the limitations listed above, our CGR adjustment is inferior to results from a truly blind RCT, its value lies that it can provide an approximate answer when achieving ideal blinding is difficult or impossible.
CGR adjustment can be viewed as an example of a resampling method to overcome the challenges of imbalanced data. Here we present only a particular solution to this problem and not a systematic exploration of how rebalancing of the data can be achieved.
Finally, our data on microdosing was obtained from a self-selected healthy sample. Microdosing may be effective for certain conditions in a clinical population, in domains we did not assess, if used at higher doses or longer time periods or when it is co-administered with a behavioral therapy, such as cognitive training.
Data availability
The data and software used here is available for scientific and research purposes at https://github.com/szb37/CorrectGuessRateCurve. The repository contains a conda computational environment, the data analyzed and scripts to reproduce all figures and major statistical findings described here.
References
von Similon, M. et al. Expert consensus recommendations on the use of randomized clinical trials for drug approval in psychiatry-comparing trial designs. Eur. Neuropsychopharmacol. 60, 91–99. https://doi.org/10.1016/j.euroneuro.2022.05.002 (2022).
Karanicolas, P. J., Farrokhyar, F. & Bhandari, M. Blinding: Who, what, when, why, how?. Can. J. Surg. 53(5), 345–348 (2010).
Colagiuri, B. Participant expectancies in double-blind randomized placebo-controlled trials: Potential limitations to trial validity. Clin. Trials 7(3), 246–255. https://doi.org/10.1177/1740774510367916 (2010).
Bausell, R. B. Snake oil Science: The Truth About Complementary and Alternative Medicine (Oxford University Press, 2009).
Baethge, C., Assall, O. P. & Baldessarini, R. J. Systematic review of blinding assessment in randomized controlled trials in schizophrenia and affective disorders 2000–2010. Psychother. Psychosom. 82(3), 152–160. https://doi.org/10.1159/000346144 (2013).
Colagiuri, B., Sharpe, L. & Scott, A. The blind leading the not-so-blind: A meta-analysis of blinding in pharmacological trials for chronic pain. J. Pain 20(5), 489–500. https://doi.org/10.1016/j.jpain.2018.09.002 (2019).
Fergusson, D., Glass, K. C., Waring, D. & Shapiro, S. Turning a blind eye: The success of blinding reported in a random sample of randomised, placebo controlled trials. BMJ 328(7437), 432. https://doi.org/10.1136/bmj.37952.631667.EE (2004).
Hróbjartsson, A., Forfang, E., Haahr, M. T., Als-Nielsen, B. & Brorson, S. Blinded trials taken to the test: An analysis of randomized clinical trials that report tests for the success of blinding. Int. J. Epidemiol. 36(3), 654–663. https://doi.org/10.1093/ije/dym020 (2007).
Scott, A. J., Sharpe, L. & Colagiuri, B. A systematic review and meta-analysis of the success of blinding in antidepressant RCTs. Psychiatry Res. 307, 114297. https://doi.org/10.1016/j.psychres.2021.114297 (2022).
Hemilä, H. Assessment of blinding may be inappropriate after the trial. Contemp. Clin. Trials 26(4), 512–514. https://doi.org/10.1016/j.cct.2005.04.002 (2005).
Sackett, D. L. Commentary: Measuring the success of blinding in RCTs: Don’t, must, can’t or needn’t?. Int. J. Epidemiol. 36(3), 664–665. https://doi.org/10.1093/ije/dym088 (2007).
Schulz, K. F., Altman, D. G., Moher, D. & Fergusson, D. CONSORT 2010 changes and testing blindness in RCTs. The Lancet 375(9721), 1144–1146. https://doi.org/10.1016/S0140-6736(10)60413-8 (2010).
Tupper, K. W., Wood, E., Yensen, R. & Johnson, M. W. Psychedelic medicine: A re-emerging therapeutic paradigm. CMAJ 187(14), 1054–1059. https://doi.org/10.1503/cmaj.141124 (2015).
Kuypers, K. P. et al. Microdosing psychedelics: More questions than answers? An overview and suggestions for future research. J. Psychopharmacol. 33(9), 1039–1057. https://doi.org/10.1177/0269881119857204 (2019).
Fadiman, J. & Korb, S. Might microdosing psychedelics be safe and beneficial? An initial exploration. J. Psychoact. Drugs 51(2), 118–122. https://doi.org/10.1080/02791072.2019.1593561 (2019).
Winkelman, M. J. & Sessa, B. Advances in Psychedelic Medicine: State-of-the-Art Therapeutic Applications (ABC-CLIO, 2019).
Anderson, T. et al. Microdosing psychedelics: Personality, mental health, and creativity differences in microdosers. Psychopharmacology 236(2), 731–740. https://doi.org/10.1007/s00213-018-5106-2 (2019).
Kaertner, L. S. et al. Positive expectations predict improved mental-health outcomes linked to psychedelic microdosing. Sci. Rep. 11(1), 1941. https://doi.org/10.1038/s41598-021-81446-7 (2021).
Polito, V. & Stevenson, R. J. A systematic study of microdosing psychedelics. PLoS ONE 14(2), e0211023. https://doi.org/10.1371/journal.pone.0211023 (2019).
Rootman, J. M. et al. Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers. Sci. Rep. 11(1), 22479. https://doi.org/10.1038/s41598-021-01811-4 (2021).
Cavanna, F. et al. Microdosing with psilocybin mushrooms: A double-blind placebo-controlled study. Transl. Psychiatry 12(1), 307. https://doi.org/10.1038/s41398-022-02039-0 (2022).
de Wit, H., Molla, H. M., Bershad, A., Bremmer, M. & Lee, R. Repeated low doses of LSD in healthy adults: A placebo-controlled, dose-response study. Addict. Biol. https://doi.org/10.1111/adb.13143 (2022).
Hutten, N. R. P. W. et al. Mood and cognition after administration of low LSD doses in healthy volunteers: A placebo controlled dose-effect finding study. Eur. Neuropsychopharmacol. 41, 81–91. https://doi.org/10.1016/j.euroneuro.2020.10.002 (2020).
Szigeti, B. et al. Self-blinding citizen science to explore psychedelic microdosing. Elife 10, e62878. https://doi.org/10.7554/eLife.62878 (2021).
Yanakieva, S. et al. The effects of microdose LSD on time perception: A randomised, double-blind, placebo-controlled trial. Psychopharmacology 236(4), 1159–1170. https://doi.org/10.1007/s00213-018-5119-x (2019).
Patino, C. M. & Ferreira, J. C. Internal and external validity: Can you apply research study results to your patients?. J. Bras. Pneumol. 44, 183–183. https://doi.org/10.1590/S1806-37562018000000164 (2018).
Margraf, J. et al. How ‘blind’ are double-blind studies. J. Consult Clin. Psychol. 59(1), 184–187. https://doi.org/10.1037//0022-006x.59.1.184 (1991).
Rabkin, J. G. et al. How blind is blind? Assessment of patient and doctor medication guesses in a placebo-controlled trial of imipramine and phenelzine. Psychiatry Res. 19(1), 75–86. https://doi.org/10.1016/0165-1781(86)90094-6 (1986).
Riddle, M. & Greenhill, L. Research unit on pediatric psychopharmacology anxiety treatment study. clinicaltrials.gov, Clinical trial registration NCT00000389, 2007. Accessed: Aug. 31, 2021. [Online]. Available: https://clinicaltrials.gov/ct2/show/NCT00000389
Cipriani, A. et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. FOC 16(4), 420–429. https://doi.org/10.1176/appi.focus.16407 (2018).
Watson, D., Clark, L. A. & Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Pers. Soc. Psychol. 54(6), 1063–1070. https://doi.org/10.1037/0022-3514.54.6.1063 (1988).
Tennant, R. et al. The Warwick–Edinburgh mental well-being scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 5(1), 63. https://doi.org/10.1186/1477-7525-5-63 (2007).
Rush, A. J. et al. The 16-Item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biol. Psychiat. 54(5), 573–583. https://doi.org/10.1016/S0006-3223(02)01866-8 (2003).
Spielberger, C. D. State-trait anxiety inventory for adults (1983).
Lee, R. M. & Robbins, S. B. Measuring belongingness: The social connectedness and the social assurance scales. J. Couns. Psychol. 42(2), 232–241. https://doi.org/10.1037/0022-0167.42.2.232 (1995).
Holze, F., Gasser, P., Müller, F., Dolder, P. C. & Liechti, M. E. Lysergic acid diethylamide-assisted therapy in patients with anxiety with and without a life-threatening illness A randomized, double-blind, placebo-controlled Phase II study. Biol. Psychiatry https://doi.org/10.1016/j.biopsych.2022.08.025 (2022).
Kirsch, I. The emperor’s new drugs: Medication and placebo in the treatment of depression. In Placebo, 291–303 (Springer, 2014).
Kola, I. & Landis, J. Can the pharmaceutical industry reduce attrition rates?. Nat. Rev. Drug Discov. 3(8), 711–715. https://doi.org/10.1038/nrd1470 (2004).
Webster, R. K. et al. Measuring the success of blinding in placebo-controlled trials: Should we be so quick to dismiss it?. J. Clin. Epidemiol. 135, 176–181. https://doi.org/10.1016/j.jclinepi.2021.02.022 (2021).
Murphy, R. J. et al. Acute mood-elevating properties of microdosed LSD in healthy volunteers: A home-administered randomised controlled trial. Biol. Psychiatry https://doi.org/10.1016/j.biopsych.2023.03.013 (2023).
Polito, V. & Liknaitzky, P. The emerging science of microdosing: A systematic review of research on low dose psychedelics (1955–2021) and recommendations for the field. Neurosci. Biobehav. Rev. 139, 104706. https://doi.org/10.1016/j.neubiorev.2022.104706 (2022).
Muthukumaraswamy, S., Forsyth, A. & Lumley, T. Blinding and expectancy confounds in psychedelic randomised controlled trials. PsyArXiv, preprint (2021). https://doi.org/10.31234/osf.io/q2hzm.
Carhart-Harris, R. L. et al. Can pragmatic research, real-world data and digital technologies aid the development of psychedelic medicine?. J. Psychopharmacol. 36(1), 6–11. https://doi.org/10.1177/02698811211008567 (2022).
Schenberg, E. Who is blind in psychedelic research? Letter to the editor regarding: Blinding and expectancy confounds in psychedelic randomized controlled trials. Expert Rev Clin Pharmacol. 14(10), 1317–1319 (2017).
Howick, J. H. The Philosophy of Evidence-Based Medicine (Wiley, 2011).
Cole, S. R. et al. Illustrating bias due to conditioning on a collider. Int. J. Epidemiol. 39(2), 417–420. https://doi.org/10.1093/ije/dyp334 (2010).
von Stumm, S. Is day-to-day variability in cognitive function coupled with day-to-day variability in affect?. Intelligence 55, 1–6. https://doi.org/10.1016/j.intell.2015.12.006 (2016).
Kube, T. & Rief, W. Are placebo and drug-specific effects additive? Questioning basic assumptions of double-blinded randomized clinical trials and presenting novel study designs. Drug Discov. Today 22(4), 729–735. https://doi.org/10.1016/j.drudis.2016.11.022 (2017).
Acknowledgements
We would like to acknowledge Allan Blemings, Fernando Rosas and Laura Kartner for the stimulating discussions that inspired this work.
Author information
Authors and Affiliations
Contributions
B.S. did the conceptualization, investigation, formal analysis, software, visualization, wrote original draft and reviewed/edited the manuscript. D.N., R.C.H. and D.E. supervised the work and reviewed/edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
B.S. declares no conflict. D.N. is an advisory to COMPASS Pathways, Neural Therapeutics, and Algernon Pharmaceuticals; received consulting fees from Algernon, H. Lundbeck and Beckley Psytech; received lecture fees from Takeda and Otsuka and Janssen plus owns stock in Alcarelle, Awakn and Psyched Wellness. D.E. received consulting fees from Aya, Mindstate, Field Trip, Clerkenwell Health. R.C.H. is an advisor to Beckley Psytech, Mindstate, TRYP Therapeutics, Mydecine, Usona Institute, Synthesis Institute, Osmind, Maya Health, and Journey Collab.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Szigeti, B., Nutt, D., Carhart-Harris, R. et al. The difference between ‘placebo group’ and ‘placebo control’: a case study in psychedelic microdosing. Sci Rep 13, 12107 (2023). https://doi.org/10.1038/s41598-023-34938-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34938-7
This article is cited by
-
Unique Psychological Mechanisms Underlying Psilocybin Therapy Versus Escitalopram Treatment in the Treatment of Major Depressive Disorder
International Journal of Mental Health and Addiction (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.