Abstract
Clinical scoring systems such as the HEART score can predict major adverse cardiovascular events, but they cannot be used to demonstrate the degree and severity of coronary artery disease. We investigated the potential of HEART Score in detecting the existence and severity of coronary artery disease based on SYNTAX score. This multi-centric cross-sectional study investigated patients referred to the cardiac emergency departments of three hospitals between January 2018 and January 2020. Data including age, gender, risk factors, comorbidities, 12-lead ECG, blood pressure and echocardiogram were recorded for all the participants. Serum troponin I level was measured on admission and 6 h later. Coronary angiography was done via the femoral or radial route. HEART and SYNTAX scores were calculated for all patients and their association was assessed. 300 patients (65% female) with mean age of 58.42 ± 12.42 years were included. mean HEART Score was 5.76 ± 1.56 (min = 3, max = 9), and mean SYNTAX score was 14.82 ± 11.42 (min = 0, max = 44.5). Pearson correlation coefficient was 0.493 between HEART Score and SYNTAX score which was statistically significant (P < 0.001). We found that HEART Score of more than 6 is 52% sensitive and 74.7% specific to detect extensive coronary artery involvement (SNTAX score ≥ 23). The present study showed that the HEART score has a moderate and positive correlation with the SYNTAX score and HEART score with a cut-off value of 6 is a predictor for SYNTAX score of ≥ 23.
Similar content being viewed by others
Introduction
While chest pain (CP) is a major cause of referral to the emergency departments (ED), only less than 25% of these patients actually have acute coronary syndrome (ACS). Patients with CP are usually hospitalized and undergo further testing and even invasive procedures like coronary angiography which leads to unnecessary hospitalization and cost1,2. On the other hand, normal levels of troponin or normal electrocardiograms (ECGs) do not necessarily exclude the presence of ACS3. Therefore, the ability to reduce hospital costs and its burden on the public health system relies on the ability to correctly risk stratify patients which will also directly influence management plan4.
Scoring systems such as SYNTAX and Gensini scores are basically scoring systems used to determine the extent and the severity of coronary artery disease and to determine treatment choice based on angiographic data5 and these scoring systems have been used in some studies to determine the prognosis of patients and have been observed to have successful results. Scoring systems such as Heart score and Grace score are scoring systems that try to show the prognosis of patients according to their clinical status6,7 and the main expectation from these scoring systems is to be an indicator of coronary plaque burden and extent rather than determining the severity of coronary artery disease.
HEART score (HS) is valuable in risk stratification of patients presenting with chest pain8. It is based on five elements including history, ECG, age, coronary risk factors, and troponin level9. Patients with a risk score of three or less are considered low-risk while a score more than seven is considered high risk and those between these two values are regarded as moderate risk for major adverse cardiac events (MACE)10.
On the other hand, the SYNTAX score (SS) has been developed to measure the complexity of coronary artery disease (CAD) and so determine the best revascularization strategy for patients with CAD. High SS indicates that patients are more prone to major MACE and need early intervention. Although SS is a well-validated method but requires coronary angiogram which is an invasive diagnostic intervention11,12,13,14,15. Therefore, an alternative non-invasive clinical scoring system such as the HS to determine the extent of the underlying CAD would be clinically relevant. However, previous studies on HS mainly sought to find the incidence of MACE, and the correlation of HS with angiographic findings have never been investigated16,17,18,19.
In this study, we aim to assess the ability of the HS to predict the extension of coronary artery disease according to SS in patients with CP.
Materials and methods
Study design and participant selection
This multi-centric cross-sectional study was conducted for a period of 2 years from January 2018 to January 2020. This research was approved by the ethics committee of Shiraz University of Medical Sciences. Written informed consent was obtained from all patients after explaining the purpose of the study. We made sure that the participation of patients did not influence diagnostic or therapeutic approaches.
All patients who were referred to the cardiac EDs of the three main hospitals affiliated with Shiraz University of Medical Sciences were included.
Patients with non-coronary chest pain including aortic syndrome, pulmonary embolism, pneumothorax, and pneumonia, and those who were not candidates for coronary angiography were excluded. Furthermore, patients who had ST-segment elevation on electrocardiogram (ECG) were immediately transferred to the catheterization unit and consequently omitted from the study.
Data acquisition, HEART score, and SYNTAX score
A pre-defined questionnaire was filled out to obtain the patients' demographic data including age, gender, and risk factors such as smoking, hypertension (HTN), diabetes mellitus (DM) and hyperlipidemia as well as clinical data including blood pressure.
A 12-lead ECG was obtained from all the participants upon entry to the ED. An experienced cardiologist who was blinded to the study interpreted ECGs20. A copy of the admission ECG was recorded in each patient’s data file.
Echocardiography was performed by an expert cardiologist with the USA GE HEALTHCARE VIVID7 DIMENSION device.
Serum troponin I level was measured in all the participants on admission and 6 h later via troponin assay ELISA kit. The Troponin value of the first blood sample was used for the HS calculation.
HS and SS were calculated by an independent cardiologist, blinded to the study and patient's characteristics. HS was calculated for each patient using initial admission data21,22. Furthermore, patients were divided into three groups; low risk (HS ≤ 3), moderate risk (3 ≤ HS > 7), and high risk (HS ≥ 7) based on HS.
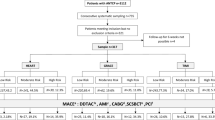
Coronary angiography was done via the femoral or radial route by an experienced cardiologist. SS was calculated according to the software available online at (The Syntax Score website. https://syntaxscore.org/. Accessed 29 Aug 2022). SS of ≥ 23 was considered as high-risk for occlusive coronary artery disease. The patients were included in the study consecutively (Fig. 1).
Statistical analysis
Statistical analysis was done using SPSS software, version 23. Categorical and continuous variables were presented as number (%) and mean ± SD, respectively. Statistical significance of scores’ differences within the groups of patients was evaluated by independent samples T-test and One-way ANOVA test. The association of quantitative parameters and scores were examined via Pearson correlation test and presented by r-coefficient and p-value. The relationship between the SS and its potential predictors was analysed by univariate and multivariate logistic regression models and illustrated by odds ratio, 95% confidence interval (CI), and corresponding statistical significance. Receiver operating characteristic (ROC) curves were used to determine the accuracy, sensitivity, and specificity of significant parameters (the result of multi-variate analysis) to predict the SS. P-values less than 0.05 were considered statistically significant.
Ethics approval
All procedures involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Approval was granted by the ethical committee of Shiraz University of Medical Sciences.
Informed consent
Written Informed consent was obtained from all individual participants included in the study. The purpose of this research was entirely explained to the patients. They were assured that their information would be kept confidential by the researcher.
Results
As illustrated by the flowchart in Fig. 1, during the investigation period, 2460 patients were referred to the emergency department with complaint of CP, and cardiac-related pain was confirmed in 414 of them. After application of the exclusion criteria, 114 patients were omitted and the remaining 300 patients were included in the study.
The patients’ baseline demographics are described in Table 1. The mean age was 58.42 ± 12.42 years (range 20–87) of which 65% were male and 35% were female. HTN was the main risk factor (60%) in our study’s population; other risk factors were DM (40%), hyperlipidemia (35%), and smoking (25%). According to our analysis, the HS and SS scores were associated with age, the presence of DM and HTN, angiography outcomes and management group of the patients (P-value < 0.05). Even though P. value of < 0.001 has been calculated between all group (SVD, 2VD, 3VD, SF or MB), it was not significant between just the two group of 2VD (6.59 ± 1.50) and 3VD (6.27 ± 1.28) statistically significant (P = 0.1380). For the management group also the P. value of < 0.001 has been calculated between all of them (Medical, PCI-SV, PCI-MV, CABG). It was not significant just between two group of MV PCI and CABG (P = 0.2981) even though the mean of PCI-MV was higher. However, we could not demonstrate a significant association between HS and SS with gender, smoking status and the presence of hyperlipidemia. Moreover, no statistically significant association was found between HS and SS with blood pressure on presentation and ejection fraction on echocardiograms.
In Table 2 all the aspects of the association between the HS and SS are demonstrated. First, we examined quantity values of SS and HS by Pearson correlation and the result was significant (r-coefficient 0.493). Categorization of the SS into low and intermediate/high risk groups and comparison of these sub-groups against HS showed statistically significant differences. One-way ANOVA test confirmed the statistically significant difference in SS between the different HS tertiles as well.
The predictive accuracy of the variables derived from different demographic and clinical data was investigated using initially univariate and then multivariate analysis with regard to the SS (Table 3). Age (OR 1.063, 95% CI 1.031–1.096, P < 0.001) and HS (OR 1.282, 95% CI 1.032–1.591, P = 0.025) were independently associated with higher SS. Based on this analysis, for each 1 year increase in age and for each 1 unit increase in HS, the chance of SS being more than 23 will increase by 6% and 28%, respectively. These predictors were analysed by Receiver operating characteristic (ROC) curves to determine their accuracy, sensitivity, and specificity (Table 4).
Discussion
Application of HS, a risk stratification scoring system originally designed for patients presenting with CP22, is a non-invasive and practical way of timely approach for these patients at the ED. In the present study, the association between HS and SS, an otherwise invasive risk assessment tool, was assessed. This would help us elucidate the potential of HS for predicting the extension of CAD in CP patients based on SS.
The result of different analyses of the association of HS and SS in the present study revealed that they are indeed positively and significantly related (r = 0.493). This positive relation is further backed up by the result of comparing sub-groups of SS and HS. Furthermore, HS with a cut-off value of 6 is 52% sensitive and 74.67% specific for predicting high SS (≥ 23).
Although studies have already assessed the relation of GRACE and TIMI with SS23,24, data regarding our research query is undeniably scarce. Vianna Cedro et al.25 in a recent and novel study have demonstrated the association of HEART, GRACE, and TIMI risk scores with angiographic complexity, using SYNTAX, in 138 ACS patients without STE. For the utilization of the ROC curve, they divided patients into two groups of low vs moderate-high SS (≥ 23) and low-moderate versus high SS (> 32). Their results are as follows; a positive and significant correlation was observed between HEART and GRACE score and SS (r = 0.29, P < 0.01 and r = 0.18, P < 0.01 respectively). They found that elevated clinical scores (HEART, GRACE, and TIMI) are predictive of high SS (> 32). Moreover, HS with cut-off points of 5 and 4 were shown to be 64% sensitive and 70% specific and 100% sensitive, and 50% specific for high SS (> 32) respectively. Although their results are in line with ours, some points should be noted. First, their study is conducted on those diagnosed with non-ST ACS whereas we aimed to target a more general population of patients, i.e., CP patients, because HS was primarily developed for risk stratification in CP patients. Second, as discussed earlier, the authors have provided a different cut-off for SS compared to ours and although the presented ROC curve in their study indicates that HS is also predictive of moderate SS, values other than AUC are not presented for SS ≥ 23 in their paper. Nonetheless, the AUC of the HS for moderate SS (≥ 23) is 0.72 (95% CI 0.62–0.83) with P-value < 0.001, which is comparable to our study results.
Additionally, it was shown in our study that HS as well as SS correlated significantly with angiographic results and management, in the sense that lower HS, consequently led to less complex angiographic findings and less aggressive management. Nevertheless, angiographic outcome and management weren't assessed in relation to HS in the above-mentioned study.
As for the remaining results, the aforementioned study by Vianna Cedro et al.25 has similarly established a significant relationship between age and SS. Although some conflicts may exist23, this relation between age and SS is recognized in other studies as well24,26 and our results confirm the same finding. The predictive value of age for SS is considerable to the extent that it is considered as one of the clinical predictors in SYNTAX score II.
In our study, 65% of patients were male and HTN was the main risk factor (60%) followed by DM (40%) and hyperlipidemia (35%). DM was substantially associated with HS, and HTN had a significant association with SS. Vianna-Cedro et al. have also reported that male patients accounted for 68.1% of their population and HTN (83.3%), DM (36.2%), and dyslipidemia (52.2%) were the most common risk factors among them. However, aside from age, they found no significant association between patients’ characteristics and SS. Existing data concerning the association of gender and SS is somewhat contradictory23,26,27,28 and a strong relationship hasn't been established yet. In the same manner, our results have revealed no significant relationship between gender and either of HS and SS. Likewise, even though heart failure and ejection fraction were substantially different in high and low SS in some studies23,26, in the present study, no significant association was observed between ejection fraction and either of HS or SS.
Even so, regardless of these discrepancies, demographic and clinical data of patients are so valuable that randomized clinical trials have already developed to incorporate such data into SS. SYNTAX score II, a modified version of SYNTAX based on both anatomical and clinical predictors aiding in more precise and individualized decision making along with the prediction of longer-term mortality in CAD has already been completed29,30.
Although our study is multi-centric with a larger sample size compared to previous ones, other clinical scores were not evaluated. Nevertheless, the results of the present study not only emphasize the efficacy of HS, as suggested in previous studies, but also highlight HS as a tool to predict the presence and extension of CAD in CP patients. Despite finding a acceptable association with SS, whether HS can be solely relied on or used along with other risk assessment tools should be investigated in future studies. Moreover, this study was retrospective and the number of participants was relatively low.
Conclusion
The present study demonstrated that the HEART score has a moderate and positive correlation with the SYNTAX score, highlighting that HEART is potentially a powerful tool for early detection of the extension of CAD in CP patients presenting to the ED. It was revealed that a HEART score of 6 is a predictor for SYNTAX score of ≥ 23.
Data availability
The data that support the findings of this study are available from Hamed Bazrafshan Drissi (corresponding author) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Hamed Bazrafshan Drissi.
Abbreviations
- SS:
-
SYNTAX score
- HS:
-
HEART score
- CP:
-
Chest pain
- ACS:
-
Acute coronary syndrome
- MACE:
-
Major adverse cardiac events
- CAD:
-
Coronary artery disease
- ECG:
-
Electrocardiogram
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- PCI:
-
Percutaneous coronary intervention
- HTN:
-
Hypertension
- DM:
-
Diabetes mellitus
References
Bassand, J.-P. et al. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: The task force for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes of the European Society of Cardiology. Eur. Heart J. 28(13), 1598–1660 (2007).
Kis, M. & Guzel, T. Relationship between hemoglobin A1c and fractional flow reserve lesion severity in non-diabetic patients. Age 58, 51–66 (2022).
Buntine, P. G., Sze, S. & Aldridge, E. S. High-sensitivity troponin T use in non-chest pain presentations in the emergency department. Emerg. Med. Australas. 32(5), 864–866 (2020).
Poldervaart, J. M. et al. Effect of using the HEART score in patients with chest pain in the emergency department: A stepped-wedge, cluster randomized trial. Ann. Intern. Med. 166(10), 689–697 (2017).
Boyraz, B. & Peker, T. Comparison of SYNTAX and gensini scores in the decision of surgery or percutaneous revascularization in patients with multivessel coronary artery disease. Cureus 14(2), 22482 (2022).
Sofidis, G. et al. Association of GRACE risk score with coronary artery disease complexity in patients with acute coronary syndrome. J. Clin. Med. 10(10), 2210 (2021).
Boyraz, B., Ibisoglu, E. & Aslan, B. The prognostic value of the nutritional prognostic index (NPI) and controlling nutritional status (CONUT) scoring systems in non-ST elevated myocardial infarction patients over 65 years of age. Aging Clin. Exp. Res. 1, 1–8 (2022).
Backus, B. E. et al. A prospective validation of the HEART score for chest pain patients at the emergency department. Int. J. Cardiol. 168(3), 2153–2158 (2013).
Poldervaart, J. M. et al. The impact of the HEART risk score in the early assessment of patients with acute chest pain: Design of a stepped wedge, cluster randomised trial. BMC Cardiovasc. Disord. 13(1), 1–8 (2013).
Poldervaart, J. M. et al. Comparison of the GRACE, HEART and TIMI score to predict major adverse cardiac events in chest pain patients at the emergency department. Int. J. Cardiol. 227, 656–661 (2017).
Altun, B. et al. The relationship between high-sensitive troponin T, neutrophil lymphocyte ratio and SYNTAX Score. Scand. J. Clin. Lab. Invest. 74(2), 108–115 (2014).
Ikeda, N., Kogame, N., Iijima, R., Nakamura, M. & Sugi, K. Carotid artery intima-media thickness and plaque score can predict the SYNTAX score. Eur. Heart J. 33(1), 113–119 (2012).
Karadeniz, M. et al. High sensitive CRP level is associated with intermediate and high syntax score in patients with acute coronary syndrome. Int. Heart J. 1, 14–299 (2015).
Zhang, L., Wu, W.-C., Ma, H. & Wang, H. Usefulness of layer-specific strain for identifying complex CAD and predicting the severity of coronary lesions in patients with non-ST-segment elevation acute coronary syndrome: Compared with Syntax score. Int. J. Cardiol. 223, 1045–1052 (2016).
Hatamnejad, M. R. et al. The utility of SYNTAX score predictability by electrocardiogram parameters in patients with unstable angina. BMC Cardiovasc. Disord. 22(1), 1–11 (2022).
Fernando, S. M. et al. Prognostic accuracy of the HEART score for prediction of major adverse cardiac events in patients presenting with chest pain: A systematic review and meta-analysis. Acad. Emerg. Med. 26(2), 140–151 (2019).
Sakamoto, J. T. et al. Comparing HEART, TIMI, and GRACE scores for prediction of 30-day major adverse cardiac events in high acuity chest pain patients in the emergency department. Int. J. Cardiol. 221, 759–764 (2016).
Six, A. J. et al. The HEART score for the assessment of patients with chest pain in the emergency department: A multinational validation study. Crit. Pathw. Cardiol. 12(3), 121–126 (2013).
Rostambeigi, S. et al. The correlation between the severity of coronary artery disease and coronary collateral circulation and atrial fibrillation after coronary artery bypass surgery: A cross-sectional study. Int. Cardiovasc. Res. J. 15(4), 1–10 (2021).
Blackburn, H., Keys, A., Simonson, E., Rautaharju, P. & Punsar, S. The electrocardiogram in population studies: A classification system. Circulation 21(6), 1160–1175 (1960).
Backus, B. E. et al. Chest pain in the emergency room: A multicenter validation of the HEART Score. Crit. Pathw. Cardiol. 9(3), 164–169 (2010).
Six, A. J., Backus, B. E. & Kelder, J. C. Chest pain in the emergency room: Value of the HEART score. Neth Heart J. 16(6), 191–196 (2008).
Hammami, R. et al. Accuracy of the TIMI and GRACE scores in predicting coronary disease in patients with non-ST-elevation acute coronary syndrome. Rev. Port. Cardiol. 37(1), 41–49 (2018).
Rahmani, R., Majidi, B., Ariannejad, H. & Shafiee, A. The value of the GRACE score for predicting the SYNTAX score in patients with unstable angina/non-ST elevation myocardial infarction. Cardiovasc. Revasc. Med. 21(4), 514–517 (2020).
Cedro, A. V. et al. Association between clinical risk score (heart, grace and TIMI) and angiographic complexity in acute coronary syndrome without ST segment elevation. Arq. Bras. Cardiol. 117(2), 281–287 (2021).
Brzozowski, P. et al. Utility of the SYNTAX score in the risk stratification of patients undergoing rotational atherectomy. Arch. Med. Sci. Atheroscler. Dis. 5, e313–e319 (2020).
Eickhoff, M. et al. Age-dependent impact of the SYNTAX-score on longer-term mortality after percutaneous coronary intervention in an all-comer population. J. Geriatr. Cardiol. 15(9), 559–566 (2018).
Huang, Z. et al. The predictive value of the HEART and GRACE scores for major adverse cardiac events in patients with acute chest pain. Intern. Emerg. Med. 16(1), 193–200 (2021).
Farooq, V. et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: Development and validation of SYNTAX score II. Lancet 381(9867), 639–650 (2013).
Takahashi, K. et al. Redevelopment and validation of the SYNTAX score II to individualise decision making between percutaneous and surgical revascularisation in patients with complex coronary artery disease: Secondary analysis of the multicentre randomised controlled SYNTAXES trial with external cohort validation. Lancet 396(10260), 1399–1412 (2020).
Author information
Authors and Affiliations
Contributions
A.Z. and H.B.D. conceived the idea for the study and in cooperation with F.D. interpreted the patient data and carried out the treatment. S.J., A.A., and M.B. drafted the manuscript. M.H. analyzed the data. M.S., A.S., and P.Y. revised the manuscript and A.Z. acts as the guarantor of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salimi, A., Zolghadrasli, A., Jahangiri, S. et al. The potential of HEART score to detect the severity of coronary artery disease according to SYNTAX score. Sci Rep 13, 7228 (2023). https://doi.org/10.1038/s41598-023-34213-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34213-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.