Abstract
We aim to explore the classifications based on coronary computed tomography angiography (CTA) for predicting the risk of major adverse cardiovascular events (MACE) in patients with suspected non-obstructive coronary artery disease (CAD) and compare with traditional non-obstructive CAD (NOCAD) classification, Duke prognostic NOCAD index, Non-obstructive coronary artery disease reporting and data system (NOCAD-RADS). 4378 consecutive non-obstructive CAD patients were assessed by coronary CTA for traditional NOCAD classification, Duke prognostic NOCAD index, NOCAD-RADS and a new classification (stenosis proximal involvement, SPI) from two medical centrals. We defined proximal involvement as any plaque was present in the main or proximal segments of coronary artery (left main, left anterior descending artery, left circumflex artery, or right coronary artery). The main outcome was MACE. During a median follow-up of 3.7 years, a total of 310 patients experienced MACE event. Kaplan–Meier survival curves showed the cumulative events increased significantly associated with traditional NOCAD, Duke NOCAD index, NOCAD-RADS and SPI classifications (all P < 0.001). In multivariate Cox regressions, the risk for the events increased from HR 1.20 (95% CI 0.78–1.83, P = 0.408) for SPI 1 to 1.35 (95% CI 1.05–1.73, P = 0.019) for SPI 2, using SPI 0 as the reference group. Coronary CTA based SPI classification provided important prognostic information for all cause-mortality risk and MACE prediction in patients with non-obstructive CAD, which was non-inferior than traditional NOCAD, Duke NOCAD Index and NOCAD-RADS classifications. The plaque location information by coronary CTA may provide additional risk prediction in patients with non-obstructive CAD.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is a worldwide disease and the major contributor to reduced quality of life1. CVD is also the leading cause of both mortality and premature mortality in China, accounting for 40% of the death in the Chinese population2. Historically, coronary artery disease (CAD) is defined as the presence of obstructive coronary artery stenosis (≥ 50%) in one or more coronary vessels and most of current prevention and treatment protocols are in accordance with this paradigm: removing the obstruction for treating angina and preventing myocardial infarction3. However, a recent research has demonstrated that approximately two-thirds of the patients were belong to without obstructive CAD in the CONFIRM (Coronary CT angiography evaluation for clinical outcomes: an international multicenter) registry study4. Moreover, a large prospective trial recent reported that the majority of cardiovascular events occurred among patients with non-obstructive CAD5.
Coronary computed tomography angiography (CTA) is a non-invasive imaging technique that allows for accurate detection and assessment of non-obstructive CAD6. One important feature of coronary CTA is that it provides information on the presence, location, and quantity of coronary atherosclerotic lesions7,8. The prognostic significance of the presence and stenosis degree of coronary atherosclerotic lesions by coronary CTA has been well established9,10. Furthermore, plaque location of coronary atherosclerotic lesions was integrated into a comprehensive CTA score and showed a good prediction of future events8. Moreover, acute coronary events in proximal vessels are more likely to lead to a clinically significant event as proximal vessels supply more myocardium. Previous studies have demonstrated that the proximally located plaque is associated with poor prognosis in obstructive CAD patients detected by coronary CTA11. In addition, only a few studies assessed the prognostic value of proximal plaque location with major adverse cardiovascular events (MACE) in non-obstructive CAD patients12. However, the contribution of proximal plaque location to MACE in non-obstructive CAD patients has not been studied in Chinese population. Moreover, the prognostic performance of proximal plaque location to MACE in non-obstructive CAD patients has not been compared with the existed classifications of non-obstructive CAD. Thus, we aim to investigate the classifications based on coronary CTA for predicting the risk of MACE in patients with suspected non-obstructive CAD and then compare with traditional non-obstructive CAD (NOCAD) classification, Duke prognostic NOCAD index, Non-obstructive coronary artery disease reporting and data system (NOCAD-RADS).
Methods
This is a retrospective, observational, multicentre study. The trial protocol have been reviewed and approved by the ethics committee of the Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology and was conducted in compliance with the Health Insurance Portability and Accountability Act (HIPAA) of 1996. Written informed consent was waived because of its retrospective observational nature and waiver for informed consent is approved by ethics committee of the Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology.
Study population
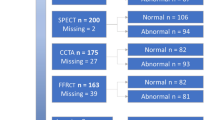
This study population consisted of 5991 consecutive patients with suspected CAD who were performed coronary CTA for clinical reasons between June 2017 and December 2019 at two hospitals in Wuhan, China. We have previous reported the details of the rational of the study and included parts of the patients13. We used the first coronary CTA examination to characterize CAD extent if multiple coronary CTAs were performed during the study period. In the current study, we excluded patients with no documentation of CAD severity (n = 26), prior history CAD or revascularization (defined as previous myocardial infarction, underwent percutaneous coronary intervention or coronary artery bypass grafting, n = 101), obstructive CAD (n = 1384), clinical data missing (n = 83) and loss of follow-up (n = 19) (Fig. 1). Finally, 4378 patients without obstructive CAD were included in the current analysis.
Coronary CTA protocol and coronary CTA based classifications
Coronary CTA was performed according to the Society of Cardiovascular Tomography (SCCT) guidelines7 using the following multi-detector CT scanners: Philips Brilliance 64, Philips Medical Systems, Best, the Netherlands; Somatom Definition AS, Siemens Healthineers, Germany. Lesions on coronary CTA were then categorized based on the severity of stenosis: 0% (no CAD) and 1–49% (non-obstructive CAD). Four classifications were defined according to coronary CTA: Traditional NOCAD classification: no CAD (0% stenosis) and NOCAD (1–49% stenosis). NOCAD-RADS classification was defined according to the highest degree of coronary stenosis: NOCAD-RADS 0 (0% stenosis), NOCAD-RADS 1 (1–24% stenosis) and NOCAD-RADS 2 (25–49% stenosis). Duke prognostic NOCAD index: Duke NOCAD 0 (0% stenosis in all vessels), Duke NOCAD 1 (1–24% stenosis, or at most 1 with 25–49% stenosis) and Duke NOCAD 2 (≥ 2 vessels of 25–49% stenosis). Stenosis proximal involvement (SPI) classification: SPI 0 (no CAD, 0% stenosis), SPI 1 (1–49% stenosis with no proximal lesion) and SPI 2 (1–49% stenosis with proximal lesion) (Fig. 2). We defined proximal involvement as any plaque was present (by visual estimation) in the main or proximal segments of coronary artery (left main, left anterior descending artery, left circumflex artery, or right coronary artery).
Follow-up and endpoint
Institutional review boards of all study centers have approved the follow-up procedures and MACE was the primary endpoint in this study. MACE was defined as all-cause death, non-fatal myocardial infarction and stroke. MACE status was determined by querying the local Community Health Service Centers. We then ascertained the event through medical records or telephone call if MACE is outside of the city. Loss of follow-up was defined as unable to obtain MACE status (without medical records or unable contacted patients by telephone outside of the city). The deadline date of follow-up was April 30, 2022.
Statistical analysis
Continuous variables were showed as mean (± SD) and categorical variables were expressed with frequencies and percentages. One-way ANOVA test was used to compare continuous variables between groups and chi-square test was used for the comparison of categorical variables. Cumulative event-free survival was estimated by Kaplan–Meier method and log-rank test was used for comparison between groups. Hazard ratio (HR) with 95% confidence intervals (95% CI) was calculated by univariate and multivariate Cox proportional hazard analyses. The discriminatory values of SPI classification, traditional NOCAD classification, NOCAD-RADS classification and Duke prognostic NOCAD index for the MACE were performed by time dependent receiver-operating characteristic (ROC) curves and C-index. Clinical characteristics including sex, age, smoke, history of hypertension and diabetes and dyslipidemia were included in the multivariate Cox regression, time dependent ROC and C-index analysis. P < 0.05 was considered as statistically significant. All statistical analyses were carried out using R statistical package (version 4.0, R foundation for Statistical Computing, Vienna, Austria), Stata (version 16, StataCorp LP, College Station, Texas, USA) and MedCalc Statistical Software (version16.8.4 Ostend, Belgium).
Results
Overall, the present study included 2281 (52.1%) and 2097 (47.9%) patients who had no CAD and non-obstructive CAD in the final analysis, respectively. Of the 4378 patients, 43.1% (1888 of 4378) were male and the average age was 59.3 ± 10.7 years. Table 1 presented the baseline and coronary CTA characteristics of the study population.
In total, 310 (7.1%) death or MACE occurred during the median 3.7 years (interquartile range 3.0–4.5) of study follow-up. The annualized MACE rate was 1.36 (95% CI 1.14–1.63) and 2.52 (95% CI 2.20–2.88) for the no CAD and non-obstructive CAD (SPI 1 and SPI 2) groups, respectively (Table 2). In addition, the annualized MACE was 2.32 (95% CI 1.62–3.31) and 2.55 (95% CI 2.21–2.94) for non-obstructive CAD without proximal involvement (SPI 1) and non-obstructive CAD with proximal involvement (SPI 2), respectively after stratifying by proximal involvement for non-obstructive CAD. Kaplan–Meier survival curves indicated that the Traditional NOCAD classification, NOCAD-RADS, Duke prognostic NOCAD index, and SPI classification is significantly associated with the increasing of the cumulative events (all P < 0.001) (Fig. 3).
In the univariate Cox regression analysis, SPI 1 and SPI 2 were significantly associated with MACE compared with SPI 0 (all P < 0.001). In multivariate Cox regressions, the risk for the MACE was increased from HR 1.20 (95% CI 0.78–1.83, P = 0.408) for SPI 1 to 1.35 (95% CI 1.05–1.73, P = 0.019) for SPI 2, using SPI 0 as the reference group (Table 3). The prognostic performance for predicting MACE of the classifications was using time dependent receiver-operating characteristic (ROC) curves at 1 year, 3 year and 5 year. The comparison of the prognostic performance between SPI and traditional NOCAD classification, NOCAD-RADS classification, or Duke prognostic NOCAD index was present in Fig. 4. The area under the time dependent ROC curve (AUC) for prediction of MACE was 0.684, 0.689, 0.695 for SPI classification in 1 year, 3 year, 5 year, respectively, which was similar with the results of Traditional NOCAD classification, NOCAD-RADS classification and Duke prognostic NOCAD index. In addition, adding SPI as a predictor to models (adjustment with clinical characteristics) did not improved their predictive value for MACE (Table 4).
Discussion
The current study demonstrated that the novel SPI classification had prognostic value for the prediction of MACE among patients with suspected no obstructive CAD in a retrospective, observational, multicentre study in the Chinese population, which was non-inferior to traditional NOCAD classification, NOCAD-RADS classification and Duke prognostic NOCAD index. Moreover, the presence of non-obstructive plaque in proximal coronary segments was associated with a 1.35-fold higher risk of MACE compared to patients with no CAD as assessed by coronary CTA. In addition, the mid or distal segments involvement in patients with non-obstructive CAD was not associated with the increasing of MACE risk compared to patients without CAD. These findings suggested that evaluating the location of coronary plaque in coronary CTA images may improve the practicability of coronary CTA in risk stratification of patients with non-obstructive CAD.
Previous studies have revealed that proximal coronary segments place higher weights on contribution to the total left ventricular blood flow and the volume affected of myocardium8,10,14. Moreover, plaque rupture and thrombus occlusion have been demonstrated to be more likely to occur in the proximal third of the coronary arteries in previous angiographic studies15,16. In addition, accumulating evidence has shown that the presence and severity of CAD in the proximal coronary segments are closely associated with poor prognosis10,11,17,18. However, these studies mainly focused on the prognostic significance of proximal plaque involvement in obstructive CAD. The contribution of proximal involvement to MACE in patients with non-obstructive is not well established.
Our previous study has showed that the prevalence of non-obstructive CAD is higher than that of obstructive CAD13, which is consistence with other multicenter studies4,5. Moreover, recent studies have suggested that the majority of cardiovascular events and all-cause mortality occurred among patients with non-obstructive CAD5,13. Thus, it is necessary to provide further risk stratification for the evaluation and management of non-obstructive CAD. Though traditional non-obstructive CAD classification presented a significant increased risk of MACE for non-obstructive CAD compared with no CAD, as shown in the present study. This classification lacks further risk stratification for patients with non-obstructive CAD, which may lead to overtreatment and management of this population. NOCAD-RADS and Duke prognostic NOCAD index classification provide more detailed risk stratification than that of traditional non-obstructive CAD classification10,13,19,20. This is in line with our findings. However, risk stratification in these studies was based on coronary stenosis rather than stenosis proximal involvement assessed by coronary CTA. Other study revealed that risk stratification improvement of non-obstructive CAD can be characterized by the extent of affected coronary segments evaluated by coronary CTA21. The few studies that do focus stenosis proximal involvement on risk stratification in patients with non-obstructive CAD. The recent CONFIRM registry study showed that proximal non-obstructive CAD had greater risk of MACE compared to patients with no CAD12. Our findings confirmed and expand these previous findings by demonstrating the proximal involvement was independently associated with increased MACE in of patients with non-obstructive CAD in Chinese population. Moreover, we compare the prognostic value of SPI with existed classifications and showed non-inferior to traditional NOCAD classification, NOCAD-RADS classification and Duke prognostic NOCAD index. Furthermore, considering both degree of stenosis and proximal involvement of CAD, the risk stratification of patients with non-obstructive CAD was improved.
Despite the import findings and clinical implications for SPI prognostic value in patients with suspected CAD in the present study, the study had several limitations. First, the study contains a relative larger sample size; however, the selection bias may be present with the retrospective nature of this study. Second, the numbers of classes are different according to the classifications that may lead inconsistent of the proportion between complex classifications and simple classifications. Specially, the relatively small sample size of patients in SPI 1 group may lead to inadequate detection of prognostic differences based on proximal involvement in non-obstructive CAD. Larger samples and multicenter researches are needed to reduce bias. Third, due to the unavailability of the data on specific causes of death, the clinical endpoint was MACE, defined as all-cause mortality, myocardial infraction or stroke. Cardiac mortality could not be separately assessed as an additional outcome which would be expected to have a stronger correlation with atherosclerotic burden. Finally, the present study had limited data on coronary artery calcium (CAC) which was recently shown to be a predictor of risk for death in non-obstructive CAD22.
In conclusion, Coronary CTA based SPI classification provided important prognostic information for MACE risk prediction in patients with non-obstructive CAD, which was non-inferior than traditional NOCAD, Duke NOCAD index and NOCAD-RADS classifications. The plaque location information by coronary CTA may provide additional risk prediction in patients with non-obstructive CAD.
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CVD:
-
Cardiovascular disease
- CAD:
-
Coronary artery disease
- CONFIRM:
-
Coronary CT angiography evaluation for clinical outcomes: an international multicenter
- CTA:
-
Computed tomography angiography
- MACE:
-
Major adverse cardiovascular events
- SCCT:
-
Society of cardiovascular tomography
- SPI:
-
Stenosis proximal involvement
- NOCAD:
-
Non-obstructive coronary artery disease
- NOCAD-RADS:
-
Non-obstructive coronary artery disease-reporting and data system
- HR:
-
Hazard ratios
- CI:
-
Confidence intervals
References
Collaborators, G. B. D. U. H. C. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1250–1284. https://doi.org/10.1016/S0140-6736(20)30750-9 (2020).
Zhao, D., Liu, J., Wang, M., Zhang, X. & Zhou, M. Epidemiology of cardiovascular disease in China: Current features and implications. Nat. Rev. Cardiol. 16, 203–212. https://doi.org/10.1038/s41569-018-0119-4 (2019).
Dweck, M. R. & Newby, D. E. Non-obstructive coronary artery disease can no longer be ignored. Eur. Heart J. Cardiovasc. Imaging 21, 489–490. https://doi.org/10.1093/ehjci/jeaa022 (2020).
Min, J. K. et al. Rationale and design of the CONFIRM (coronary CT angiography evaluation for clinical outcomes: An international multicenter) registry. J. Cardiovasc. Comput. Tomogr. 5, 84–92. https://doi.org/10.1016/j.jcct.2011.01.007 (2011).
Hoffmann, U. et al. Prognostic value of noninvasive cardiovascular testing in patients with stable chest pain: Insights from the PROMISE trial (prospective multicenter imaging study for evaluation of chest pain). Circulation 135, 2320–2332. https://doi.org/10.1161/CIRCULATIONAHA.116.024360 (2017).
Miller, J. M. et al. Diagnostic performance of coronary angiography by 64-row CT. N. Engl. J. Med. 359, 2324–2336. https://doi.org/10.1056/NEJMoa0806576 (2008).
Leipsic, J. et al. SCCT guidelines for the interpretation and reporting of coronary CT angiography: A report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J. Cardiovasc. Comput. Tomogr. 8, 342–358. https://doi.org/10.1016/j.jcct.2014.07.003 (2014).
van Rosendael, A. R. et al. Superior risk stratification with coronary computed tomography angiography using a comprehensive atherosclerotic risk score. JACC Cardiovasc. Imaging 12, 1987–1997. https://doi.org/10.1016/j.jcmg.2018.10.024 (2019).
Carrigan, T. P. et al. Prognostic utility of 64-slice computed tomography in patients with suspected but no documented coronary artery disease. Eur. Heart J. 30, 362–371. https://doi.org/10.1093/eurheartj/ehn605 (2009).
Hadamitzky, M. et al. Optimized prognostic score for coronary computed tomographic angiography: Results from the CONFIRM registry (Coronary CT angiography evaluation for clinical outcomes: An international multicenter registry). J. Am. Coll. Cardiol. 62, 468–476. https://doi.org/10.1016/j.jacc.2013.04.064 (2013).
Min, J. K. et al. Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J. Am. Coll. Cardiol. 50, 1161–1170. https://doi.org/10.1016/j.jacc.2007.03.067 (2007).
Han, D. et al. Prognostic significance of plaque location in non-obstructive coronary artery disease: From the CONFIRM registry. Eur. Heart J. Cardiovasc. Imaging https://doi.org/10.1093/ehjci/jeab223 (2021).
Huang, Z. et al. Prognostic value of CAD-RADS classification by coronary CTA in patients with suspected CAD. BMC Cardiovasc. Disord. 21, 476. https://doi.org/10.1186/s12872-021-02286-x (2021).
Leaman, D. M., Brower, R. W., Meester, G. T., Serruys, P. & van den Brand, M. Coronary artery atherosclerosis: Severity of the disease, severity of angina pectoris and compromised left ventricular function. Circulation 63, 285–299. https://doi.org/10.1161/01.cir.63.2.285 (1981).
Wang, J. C., Normand, S. L., Mauri, L. & Kuntz, R. E. Coronary artery spatial distribution of acute myocardial infarction occlusions. Circulation 110, 278–284. https://doi.org/10.1161/01.CIR.0000135468.67850.F4 (2004).
Valgimigli, M. et al. Distance from the ostium as an independent determinant of coronary plaque composition in vivo: An intravascular ultrasound study based radiofrequency data analysis in humans. Eur. Heart J. 27, 655–663. https://doi.org/10.1093/eurheartj/ehi716 (2006).
Farhan, S. et al. Association of culprit lesion location with outcomes of culprit-lesion-only vs immediate multivessel percutaneous coronary intervention in cardiogenic shock: A post hoc analysis of a randomized clinical trial. JAMA Cardiol. 5, 1329–1337. https://doi.org/10.1001/jamacardio.2020.3377 (2020).
Cho, I. et al. Prognostic value of coronary computed tomographic angiography findings in asymptomatic individuals: A 6-year follow-up from the prospective multicentre international CONFIRM study. Eur. Heart J. 39, 934–941. https://doi.org/10.1093/eurheartj/ehx774 (2018).
Bittner, D. O. et al. Prognostic value of coronary CTA in stable chest pain: CAD-RADS, CAC, and cardiovascular events in PROMISE. JACC Cardiovasc. Imaging 13, 1534–1545. https://doi.org/10.1016/j.jcmg.2019.09.012 (2020).
Xie, J. X. et al. The coronary artery disease-reporting and data system (CAD-RADS): Prognostic and clinical implications associated with standardized coronary computed tomography angiography reporting. JACC Cardiovasc. Imaging 11, 78–89. https://doi.org/10.1016/j.jcmg.2017.08.026 (2018).
Maddox, T. M. et al. Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA 312, 1754–1763. https://doi.org/10.1001/jama.2014.14681 (2014).
Cho, I. et al. Prognostic implications of coronary artery calcium in the absence of coronary artery luminal narrowing. Atherosclerosis 262, 185–190. https://doi.org/10.1016/j.atherosclerosis.2016.12.006 (2017).
Author information
Authors and Affiliations
Contributions
Study concepts: X.W., Z.F.H., J.H., Study design: X.W., Z.F.H., J.H., B.B.C., X.Y.D., M.L., Data acquisition and analysis: Z.Q.L., Z.F.H., J.W.X., Statistical analysis: Z.F.H., B.B.C., Manuscript preparation: X.W., Z.F.H., B.B.C., X.Y.D., M.L., Manuscript editing and review: X.W., Z.F.H.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, Z., Cao, B., Du, X. et al. Prognostic value of coronary CTA-based classifications for predicting major events without obstructive coronary artery disease. Sci Rep 13, 10635 (2023). https://doi.org/10.1038/s41598-023-37465-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-37465-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.