Abstract
This study explored the anticipated time to seek medical advice for possible colorectal cancer (CRC) signs/symptoms and its association with CRC symptom awareness. In addition, it examined perceived barriers that may delay seeking medical advice. Palestinian adults were recruited from hospitals, primary healthcare centers, and public spaces in 11 governorates. A modified, translated-into-Arabic version of the validated Bowel Cancer Awareness Measure was used. The questionnaire comprised three sections: sociodemographics, assessment of CRC symptom awareness and time to seek medical advice, and barriers to early presentation. A total of 4623 participants were included. The proportion that reported seeking immediate medical advice for possible CRC signs/symptoms with blood or mass ranged from 47.1% for ‘blood in stools’ to 59.5% for ‘bleeding from back passage’. Less than half of the participants reported immediate seeking of medical advice for non-specific symptoms (ranging from 5.4% for ‘loss of appetite’ to 42.0% for ‘anemia’) and other gastrointestinal symptoms (ranging from 7.7% for ‘feeling persistently full’ to 35.7% for ‘change in bowel habits’). Good CRC symptom awareness was associated with higher likelihood of seeking medical advice within a week from recognizing a CRC symptom. About 13.0% reported a delay to visit their doctor after recognizing a CRC symptom. The most reported barriers were practical with ‘would try some herbs first’ (50.9%) as the leading barrier. CRC symptoms with blood or mass prompted earlier help seeking. Participants with good CRC awareness were more likely to seek medical advice within a week.
Similar content being viewed by others
Introduction
Globally, colorectal cancer (CRC) is the third most common cancer accounting for 10.0% of the total cancer cases and the second most common cause of cancer-related mortality; accounting for 9.4% of total cancer deaths1. In Western Asia, a total of 41,569 cases of CRC were registered in 20202. In Palestine, CRC is the most common cancer among males and the second most common cancer among females after breast cancer3. CRC accounted for 13.7% of the total cancer cases in the West Bank and Jerusalem (WBJ) in 2021 with an incidence rate of 16.4 per 100,000 general population, and 12.8% of the total cancer cases in the Gaza Strip with an incidence rate of 11.5 per 100,000 general population3,4.
Previous studies have shown an association between the nature of CRC signs/symptoms and the time needed to seek medical advice5,6. Esteva and colleagues from Spain found that patients, who presented with abdominal pain or vomiting, had a shorter time to seek medical advice than those with other signs/symptoms. The authors also found that a patient’s perception of the seriousness of a sign/symptom led to shorter intervals to seeking medical advice and early diagnosis5.
Early diagnosis plays an important role in improving the prognosis and survival rates of CRC7. Immediate seeking of medical advice is a key to early diagnosis, but there are several factors that can delay seeking medical advice. These include the ability to recognize CRC signs/symptoms and the existence of barriers to early presentation, which could be emotional, practical or service-related barriers8. A recent national study from Palestine has demonstrated that only 40% of the participants displayed good awareness of CRC signs/symptoms9. Another study conducted in the Gaza Strip found that the most common emotional barrier encountered by participants was ‘feeling worried about what the doctor might find’8. However, the interplay between recognition of CRC signs/symptoms with the time to seek medical advice as well as having barriers to early presentation warrants further investigation.
Therefore, this national study aimed to: (i) explore the anticipated time to seek medical advice for a possible CRC sign/symptom, (ii) examine the association between CRC signs/symptom awareness and the time to seek medical advice, and (iii) examine the barriers that may delay help-seeking and their association with the awareness levels of CRC signs/symptoms.
Materials and methods
Study design and population
This was a national cross-sectional study, where data were collected between the 1st of July 2019 and the 31st of March 2020. The target population was adult (≥ 18 years) Palestinians, who make up 62.2% of about five million living in the Gaza Strip and the WBJ10. Palestine has 16 governorates: five in the Gaza Strip and 11 in the WBJ10. Participants were recruited from 11 governorates: four in the Gaza Strip and seven in the WBJ.
Settings and sampling methods
In Palestine, healthcare is provided by governmental facilities, non-governmental organizations (NGOs), private healthcare organizations, and the United Nations Relief and Works Agency (UNRWA) facilities. The majority of patients utilize health services provided by governmental hospitals or primary healthcare centers at no cost or little co-payments3. To maximize the representativeness of the study cohort, potential participants were invited to participate from governmental hospitals, primary healthcare centers, and public spaces, such as mosques, churches, downtown areas, parks, trade streets, malls and public transportation stations using convenience sampling.
Inclusion and exclusion criteria
Inclusion criteria for this study were being an adult (≥ 18 years) Palestinian and being a visitor to one of the data collection sites. Exclusion criteria included working or studying in a health-related field, holding a nationality other than Palestinian, being unable to complete the questionnaire, and being a visitor to an oncology department at the time of data collection.
Data collection and measurement tool
A modified version of the validated tool Bowel Cancer Awareness Measure (BoCAM) was used for data collection11. BoCAM was translated into Arabic and then back translated into English by four bilingual healthcare professionals (two at each stage) who had experience in clinical research and survey design. To ensure content validity, the translated questionnaire was reviewed by five independent experts specialized in the fields of coloproctology, gastroenterology, and public health. This was then followed by conducting a pilot study (n = 25) to assess the clarity of the questions of the Arabic version. The data collected in the pilot study were not included in the final data analysis. Internal consistency was assessed using Cronbach’s Alpha, which reached an acceptable value (α = 0.887).
The questionnaire comprised three sections. The first section described participants’ socio-demographic factors including age, gender, marital status, level of education, employment status, monthly income, place of residence, having a chronic health condition, following a vegetarian diet, and knowing someone with cancer. The second section evaluated the participants’ awareness of 12 CRC signs and symptoms based on a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = not sure, 4 = agree, and 5 = strongly agree). Out of the 12 CRC signs/symptoms, nine were adapted from the original BoCAM, where they had yes/no/unknown responses but were then converted into a 5-point Likert scale questions to minimize the possibility of answering randomly8,9,12,13,14,15,16,17,18,19,20. The signs/symptoms of ‘feeling persistently full’, ‘unexplained loss of appetite’, and ‘unexplained generalized fatigue’ were added to the questionnaire since they were used in other forms of the Cancer Awareness Measure21,22,23. The second section also assessed the anticipated time to seek medical advice for each possible CRC sign/symptom when recognized using an open-ended question. The third section evaluated perceived barriers to early presentation based on the aforementioned 5-point Likert scale. A total of 10 barriers were adopted from the original BoCAM22, whereas the remaining were deemed important to include based on previous similar studies24,25,26.
Participants were invited to complete the questionnaire in a face-to-face interview with the presence of a data collector. The data were collected using ‘Kobo Toolbox’, a secure, user-friendly data collection tool that can be easily accessed via smartphones27.
Statistical analysis
The American Cancer Society recommends starting CRC screening for people at average risk at the age of 4528. Therefore, the continuous variable of age was categorized into two categories using this cutoff: 18–44 years and ≥ 45 years. The minimum wage in Palestine is 1450 NIS (about $450) 29. Therefore, monthly income was categorized using this cutoff into two categories: < 1450 NIS and ≥ 1450 NIS.
Median and interquartile ranges (IQR) were used to describe non-normally distributed, continuous variables, whereas frequencies and percentages were used to describe categorical variables. Comparisons between baseline characteristics of participants recruited from the Gaza Strip and those recruited from the WBJ were performed using the Kruskal–Wallis test if the characteristic was continuous or the Pearson’s Chi-square test if it was categorical.
CRC signs/symptoms were categorized into three categories: (i) signs/symptoms with a mass or blood, (ii) signs/symptoms of a non-specific nature, and (iii) other gastrointestinal signs/symptoms. The anticipated time to seek medical advice for a possible CRC sign/symptom was categorized into four categories: immediately (less than 24 h), 2–7 days, > 7 days, and never. Frequencies and percentages were used to describe the anticipated time and comparisons between participants recruited from the Gaza Strip and those recruited from the WBJ were performed using the Pearson’s Chi-Square test. The awareness level of CRC signs and symptoms was evaluated as previously described9,12,13,14,15,16,17. Answers provided by participants who responded with agree or strongly agree were considered correct, and other answers were considered incorrect. One point was given for each correctly recognized CRC sign/symptom. The total score was calculated (ranging from 0 to 12) and categorized, based on the number of CRC signs/symptoms recognized, into three categories: poor (0–4), fair (5–8), and good awareness (9–12). Multivariable logistic regression was utilized to examine the association between awareness level of CRC signs/symptoms and the anticipated time to seek medical advice for a possible CRC sign or symptom. The multivariable analysis adjusted for age group, gender, education, employment status, monthly income, place of residency, marital status, having a chronic disease, following a vegetarian diet, knowing someone with cancer, and site of data collection. This model was determined a priori based on previous studies6,8,9,12,24,25,26.
Consistent with the original BoCAM22, barriers to early presentation were categorized into three categories: emotional, service, and practical barriers. Frequencies and percentages were used to describe the displayed barriers and comparisons between participants recruited from the Gaza Strip and those recruited from the WBJ were performed using Pearson’s Chi-Square test. The median number of barriers in each category (overall, emotional, service, and practical) was utilized as a cutoff to dichotomize the number of displayed barriers. This was followed by running a multivariable logistic regression to examine the association between CRC signs/symptom awareness level and displaying at least the median number of barriers in each category. The same aforementioned multivariable model was used in all those analyses.
Missing data were hypothesized to occur completely at random and were handled using a complete case analysis. Data were analyzed using Stata software version 16.0 (StataCorp, College Station, Texas, United States).
Ethical approval and consent to participate
Prior to data collection, ethical approval had been sought and obtained from the Research Ethics Committee at the Islamic University of Gaza, the Human Resources Development department at the Palestinian Ministry of Health, and the Helsinki Committee in the Gaza Strip. The study along with its purpose and objectives were thoroughly explained to the participants and they were well informed that their participation is completely voluntary. A written informed consent was obtained from each participant prior to filling out the questionnaire, and data were collected and reported anonymously. All methods were performed in accordance with the relevant guidelines and regulations.
Results
Participant characteristics
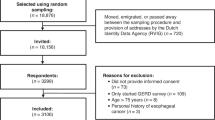
Of the 5254 participants approached, 4877 participants agreed and completed the questionnaire (response rate = 92.3%). A total of 4623 questionnaires were included in the final analysis (254 were excluded: 210 had missing data and 44 did not meet the inclusion criteria); 2700 were from the WBJ and 1923 from the Gaza Strip. The median age [IQR] among all study participants was 31.0 [24.0, 43.0] years and 1879 (40.6%) were males (Table 1). Participants from the Gaza Strip were younger, had lower monthly income, and suffered from a fewer number of chronic diseases than participants from the WBJ. The majority of participants displayed fair (42%) to good (40%) levels of awareness about CRC signs/symptoms. Participants from the WBJ were more likely than participants from the Gaza Strip to display good awareness of CRC signs/symptoms (42.1% vs. 37.0%).
Immediate seeking of medical advice for a possible CRC sign/symptom
The proportion of study participants who reported that they would immediately seek medical advice for possible CRC signs/symptoms with blood or a mass was 59.5% (n = 2752) for ‘bleeding from back passage’, 52.9% (n = 2445) for ‘lump in the abdomen’, and 47.1% (n = 2176) for ‘blood in stools’ (Table 2). Participants from the WBJ were more likely than participants from the Gaza Strip to immediately visit a doctor if they had “blood in the stool,” but were less likely to immediately seek medical advice if they experienced a “lump in the abdomen”.
The proportion of study participants who reported that they would immediately seek medical advice for a possible non-specific CRC sign/symptom was 42.0% (n = 1943) for ‘anemia’, 21.1% (n = 974) for ‘unexplained weight loss’, 6.8% (n = 313) for ‘unexplained generalized fatigue’, and 5.4% (n = 249) for ‘unexplained loss of appetite’. Participants from the WBJ were more likely than participants from the Gaza Strip to immediately seek medical advice when asked about all non-specific CRC signs/symptoms.
The proportion of study participants who reported that they would immediately seek medical advice for other gastrointestinal signs/symptoms was 35.7% (n = 1650) for ‘change in bowel habits’, 23.5% (n = 1086) for ‘persistent pain in the abdomen, 21.1% (n = 977) for ‘pain in the back passage’, 9.4% (n = 436) for ‘bowel not emptying completely’, and 7.7% (n = 357) for ‘feeling persistently full’. Participants from the WBJ were more likely than participants from the Gaza Strip to immediately seek medical advice when asked about all other gastrointestinal signs/symptoms.
Association between awareness level of CRC signs/symptoms and no seeking of medical advice
There was an associated decrease in the likelihood of reporting no seeking of medical advice for each of the CRC signs/symptoms among participants who displayed fair levels of awareness of CRC signs/symptoms compared to those who displayed poor levels (Table 3). Additionally, there was a further associated decrease in the likelihood of not seeking medical advice for all CRC signs/symptoms among participants who displayed good awareness of CRC signs/symptoms (Table 3).
Association between awareness level of CRC signs/symptoms and seeking medical advice within a week
Compared to participants who displayed poor awareness of CRC signs/symptoms, participants with a fair level of awareness had an associated increase in the likelihood of seeking medical advice within a week for each of the CRC signs/symptoms except for ‘change in bowel habits’, where no associated difference was found (Table 4). Additionally, there was a further associated increase in the likelihood of seeking medical advice within a week for all CRC signs/symptoms among participants who displayed good awareness of CRC signs/symptoms.
Barriers to early presentation and association with CRC symptom awareness
When participants were asked if they would delay seeking medical advice after recognizing a sign/symptom of CRC, 609 (12.5%) answered with ‘yes’ and reported at least one barrier to early presentation. Overall, the most commonly reported barriers were practical and those included ‘would try some herbs first’ (n = 310, 50.9%), ‘would think that symptom is not something important to see the doctor for’ (n = 305, 50.1%), and ‘too busy to go to the doctor’ (n = 304, 49.9%) (Table 5). The most commonly reported service-related barrier was ‘the thought that there is a small number of qualified doctors in the Palestinian Ministry of Health facilities’ (n = 260, 42.7%). The most commonly reported emotional barriers were ‘disliking the visit to healthcare facilities’ (n = 284, 46.6%) and ‘feeling worried about what a doctor might find’ (n = 258, 42.4%). All these findings were consistent in both the Gaza Strip and the WBJ.
On the multivariable analysis, displaying fair or good awareness of CRC symptoms was associated with a higher likelihood of reporting at least three emotional barriers to early presentation (OR = 1.71, 95% CI: 1.06–2.77 and OR = 1.67, 95% CI: 1.02–2.73, respectively) (Table 6). However, there was no association between CRC symptom awareness level and reporting practical or service-related barriers.
Discussion
In this study, participants reported that it would take them less time to present with possible CRC signs/symptoms that are related to blood or a mass than other CRC signs/symptoms. Seeking immediate medical advice was most likely to be associated with bleeding from the back passage, and least likely with anemia. Other symptoms displayed a wide variation in reporting immediate help-seeking. Practical barriers were the most frequently reported barriers by study participants. Displaying good awareness of CRC signs/symptoms was associated with a higher likelihood of seeking medical advice within a week from recognizing the sign/symptom and a greater likelihood of reporting emotional barriers.
Immediate seeking of medical advice for a possible CRC sign/symptom
Bleeding from the back passage was the most commonly reported symptom to seek immediate medical advice (59.5%), which could be explained by a possible tendency of the Palestinian population to associate bleeding with ominous diagnoses. This is supported by findings from a study by Koo and colleagues, who demonstrated that the nature of the presenting signs/symptoms could be a critical influencing factor in the interval of seeking medical advice30. In addition, Courtney and colleagues surveyed 1592 participants, aged between 56 and 88 years, and found that 18% of them had experienced rectal bleeding but had never sought medical advice. The reason for this delay was the perception of the respective signs/symptoms as being mild and not serious or as being benign31. This could also explain the lower proportions of study participants who reported immediate help-seeking for non-specific CRC signs/symptoms or with gastrointestinal manifestations in this study; as these might also have been perceived as benign symptoms based on the findings and observations from this study. Another possibility could be that some participants may have expected their symptoms to subside over time without the need to visit a doctor, which is consistent with findings of a national study in the United States showing that perception of symptom self-resolution contributed to delay in seeking medical care32. Moreover, participants could delay help-seeking due to the hard economic situation in Palestine, especially in the Gaza Strip where about 65% of the population suffer from poverty and 60% are unemployed33.
Association between awareness level of CRC signs/symptoms and seeking medical advice
Mhaidat and colleagues conducted a cross-sectional study in Jordan and reported that 60.6% of participants would seek medical advice within one week of experiencing CRC symptoms. The authors suggested that promoting early help-seeking can be achieved by raising the awareness of CRC signs and symptoms34. This study supports their findings, where it demonstrated that good awareness levels of CRC signs/symptoms were associated with a greater likelihood to seek medical advice for any or all of the CRC signs/symptoms within one week. In addition, Niksic and colleagues showed that higher awareness of CRC signs/symptoms led to an increase in the cancer survival index35. Moreover, a previous study conducted in Malaysia demonstrated how using mass media campaigns helped to significantly improve the recognition of CRC signs and symptoms36. These findings collectively reflect the importance of integrating educational interventions in healthcare and educational systems, which may have a significant impact on patients’ ability to recognize possible CRC signs/symptoms, and thus, increase the likelihood of early help-seeking, which may potentially reduce morbidity and mortality related to CRC37,38.
Barriers to early presentation and association with CRC symptom awareness
A previous study conducted in the Gaza Strip in 2021 reported that emotional barriers to seeking medical advice, in case of having cancer signs/symptoms, were the most commonly reported barriers, where ‘feeling worried about what the doctor might find’ was the most commonly reported barrier to early presentation8. The authors also reported the barrier ‘too busy to go to the doctor’ as the most common practical barrier and ‘difficulty making an appointment with the doctor’ as the most common service-related barrier8. A previous study from Oman found that lacking time to visit the physician was the most common overall barrier hindering early presentation, followed by emotional barriers39. In our study, the most reported barriers to seeking medical advice for possible CRC signs/symptoms were practical, followed by emotional and service-related barriers. This is concordant with findings of a study conducted in New Zealand, showing that patients’ appraisal and normalization of symptoms led to delays in seeking medical advice and therefore, delays in prompt diagnosis of CRC40. Furthermore, a study conducted in Jordan showed that 3.1% of participants reported not wanting to visit physicians for their symptoms due to a combination of service, practical, and emotional barriers41. This study found that the thought of ‘small number of qualified doctors in the Palestinian Ministry of Health facilities’ was the most common service-related barrier. This is also demonstrated in a study done in New Zealand, which showed that poor perception of physicians led to deterioration in the physician–patient relationship that subsequently acted as a barrier to early presentation and diagnosis of CRC40. These findings demonstrate the vital role of patients’ perception of physicians’ technical and interpersonal communication competence in their decision making to seek medical advice, and follow-up appropriately thereafter.
Another important practical barrier reported in this study was thinking that the sign/symptom is not important for the doctor to check. This is consistent with findings by Al-Azri and colleagues who surveyed 999 participants in Oman and found that 21.2% were worried about wasting the physician’s time39. Interestingly, another study conducted in Jordan showed that some participants did not want to visit the physician for their possible symptoms without displaying any specific reason explaining such behavior41. Moreover, a study from Spain demonstrated that non-specific signs/symptoms (e.g., change in bowel movement) would significantly delay presentation of CRC42. This might be due to a lack of awareness and/or faulty perception especially in regards to signs/symptoms recognized as “non-alarming”.
Noticeably, good awareness of CRC signs/symptoms was associated with a higher likelihood of reporting emotional barriers. This could possibly be due to the amplifying effect of fears and concerns after recognizing CRC signs/symptoms, which is consistent with findings reported in a previous study conducted in Lebanon43. Educational interventions should help participants to gain insight about the availability of diagnostic and screening modalities, and treatment options, which could potentially have a positive impact on early help-seeking44,45. This may mitigate the influence of emotional, practical, and service barriers on individuals’ behavior by helping them understand that early detection of CRC could lead to a significant reduction of the disease burden.
Future directions
This study explored the anticipated time to seek medical advice and the various barriers that could hinder early presentation of CRC. Using educational interventions that focus on overcoming these barriers and changing the attitudes of the public could possibly shape help-seeking behaviors and lead to earlier seeking of medical advice and, thus, a better overall prognosis. A multidisciplinary and culturally adapted approach should be used to enlighten healthy individuals about CRC, and help them rationalize the fears and false presumptions regarding the disease. Efforts are also needed to address the concerns the public has about the small number of qualified doctors who are working in the facilities of the Palestinian Ministry of Health. Furthermore, qualitative studies are needed to further explore reasons for the delay in help-seeking to understand why these barriers exist.
Limitations of the study
This study has some limitations that should be considered while interpreting the results. Convenience sampling was utilized to recruit the study participants, which may limit the generalizability of the study findings. However, the large sample size and data collection from various geographical locations in Palestine might have mitigated this limitation. Patients or visitors to oncology departments and those with medical backgrounds were excluded from the study, which might have reduced the number of participants with presumably good CRC symptom awareness. Their exclusion, however, was meant to make this study more pertinent as a measure of the public awareness and perception of CRC. Furthermore, this study sampled participants who did not experience actual CRC symptoms and looked at their perceived knowledge and barriers to early presentation. This may differ from experiencing CRC symptoms and future studies are needed to estimate the time taken by CRC patients to seek medical advice and to examine the interplay between CRC symptom awareness and barriers to early presentation.
Conclusion
In this study, CRC signs and symptoms with blood or a mass were perceived as the most alarming and prompted earlier help-seeking behavior. Good awareness of CRC signs/symptoms was associated with a higher likelihood of seeking medical advice within a week from recognizing the sign/symptom, but also with a greater likelihood of reporting emotional barriers. The most frequently reported barriers to early presentation were practical barriers. Establishing educational interventions to raise CRC awareness may help in promoting earlier help-seeking and, thus, facilitate earlier diagnosis and improved prognosis.
Data availability
The dataset used during the current study is available from the corresponding author on reasonable request.
References
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
The Global Cancer Observatory -World Health Organization. https://bit.ly/3GxH5bk (2020).
Palestinian Ministry of Health. Palestine Annual Health Report. https://bit.ly/3Vpiqdl (2021).
Palestinian Ministry of Health. Palestine Annual Health Report. https://bit.ly/3AHZYD2 (2020).
Esteva, M. et al. Factors related with symptom duration until diagnosis and treatment of symptomatic colorectal cancer. BMC Cancer 13, 87 (2013).
Walter, F. M. et al. Symptoms and patient factors associated with longer time to diagnosis for colorectal cancer: Results from a prospective cohort study. Br. J. Cancer 115, 533–541 (2016).
Faivre-Finn, C. et al. Colon cancer in France: Evidence for improvement in management and survival. Gut 51, 60–64 (2002).
Elshami, M. et al. Public awareness and barriers to seeking medical advice for colorectal cancer in the Gaza strip: A cross-sectional study. J. Glob. Oncol. 5, Jgo1800252 (2019).
Elshami, M. et al. Awareness of colorectal cancer signs and symptoms: A national cross-sectional study from Palestine. BMC Public Health 22, 866 (2022).
Palestinian Central Bureau of Statistics. Palestine in Figures. https://bit.ly/3i6G54C (2021).
Power, E., Simon, A., Juszczyk, D., Im, S. & Wardle, J. Assessing awareness of colorectal cancer symptoms: Measure development and results from a population survey in the UK. BMC Cancer 11, 366 (2011).
Elshami, M. et al. Awareness of colorectal cancer risk factors in palestine: Where do we stand?. JCO Glob. Oncol. 8, e2200070 (2022).
Elshami, M. et al. Women’s awareness of breast cancer symptoms: A national cross-sectional study from Palestine. BMC Public Health 22, 801 (2022).
Elshami, M. et al. Awareness of Palestinians about lung cancer symptoms: A national cross-sectional study. BMC Pulm. Med. 22, 135 (2022).
Elshami, M. et al. Awareness of ovarian cancer risk and protective factors: A national cross-sectional study from Palestine. PLoS ONE 17, e0265452 (2022).
Elshami, M. et al. Knowledge of Palestinian women about cervical cancer warning signs: A national cross- sectional study. BMC Public Health 21, 1779 (2021).
Elshami, M. et al. Awareness of human papillomavirus and acceptability of the vaccine among women in Palestine: Is it time for policy adjustment?. BMC Womens Health 22, 352 (2022).
Elshami, M. et al. Knowledge level of cancer symptoms and risk factors in the Gaza Strip: A cross-sectional study. BMC Public Health 20, 414 (2020).
Elshami, M. et al. Perceived barriers to seeking cancer care in the Gaza Strip: A cross-sectional study. BMC Health Serv. Res. 21, 28 (2021).
Elshami, M. et al. Breast cancer awareness and barriers to early presentation in the Gaza-strip: A cross-sectional study. J. Glob. Oncol. 4, 1–13 (2018).
Simon, A. E. et al. Knowledge of lung cancer symptoms and risk factors in the U.K.: Development of a measure and results from a population-based survey. Thorax 67, 426–432 (2012).
Stubbings, S. et al. Development of a measurement tool to assess public awareness of cancer. Br. J. Cancer 101(Suppl 2), S13-17 (2009).
Simon, A. E. et al. Ovarian and cervical cancer awareness: Development of two validated measurement tools. J. Fam. Plann. Reprod. Health Care 38, 167–174 (2012).
Alatise, O. I. et al. Health-seeking behavior and barriers to care in patients with rectal bleeding in Nigeria. J. Glob. Oncol. 3, 749–756 (2017).
Siminoff, L., Thomson, M. & Dumenci, L. Factors associated with delayed patient appraisal of colorectal cancer symptoms. Psychooncology 23, 981–988 (2014).
Simon, A. E., Waller, J., Robb, K. & Wardle, J. Patient delay in presentation of possible cancer symptoms: The contribution of knowledge and attitudes in a population sample from the United Kingdom. Cancer Epidemiol. Biomark. Prev. 19, 2272–2277 (2010).
Harvard Humanitarian Initiative. KoBoToolbox. https://bit.ly/3jWdUmi (2009).
American Cancer Society. Colorectal Cancer Screening Guidelines 2018. https://bit.ly/3WBg9gi (2018).
Palestinian Central Bureau of Statistics. The current Status of the Palestinian Labor Force. https://bit.ly/3ZfkDv9 (2020).
Koo, M. M., Hamilton, W., Walter, F. M., Rubin, G. P. & Lyratzopoulos, G. Symptom signatures and diagnostic timeliness in cancer patients: A review of current evidence. Neoplasia 20, 165–174 (2018).
Courtney, R. J. et al. Current state of medical-advice-seeking behaviour for symptoms of colorectal cancer: Determinants of failure and delay in medical consultation. Colorectal Dis. 14, e222-229 (2012).
Taber, J. M., Leyva, B. & Persoskie, A. Why do people avoid medical care? A qualitative study using national data. J. Gen. Intern. Med. 30, 290–297 (2015).
United Nations. One third of Gaza Strip population in need of psychological and social support. https://bit.ly/3WobrlU) 2020).
Mhaidat, N. M. et al. Knowledge and awareness of colorectal cancer early warning signs and risk factors among university students in Jordan. J. Cancer Educ. 33, 448–456 (2018).
Niksic, M. et al. Is cancer survival associated with cancer symptom awareness and barriers to seeking medical help in England? An ecological study. Br. J. Cancer 115, 876–886 (2016).
Schliemann, D. et al. Change in public awareness of colorectal cancer symptoms following the Be Cancer Alert Campaign in the multi-ethnic population of Malaysia. BMC Cancer 20, 252 (2020).
Kyle, R. G., Forbat, L., Rauchhaus, P. & Hubbard, G. Increased cancer awareness among British adolescents after a school-based educational intervention: A controlled before-and-after study with 6-month follow-up. BMC Public Health 13, 190 (2013).
Tatari, C. R. et al. Perceptions about cancer and barriers towards cancer screening among ethnic minority women in a deprived area in Denmark—a qualitative study. BMC Public Health 20, 921 (2020).
Al-Azri, M. et al. Awareness of cancer symptoms and barriers to seeking medical help among adult people attending primary care settings in Oman. Health Serv. Res. Manag. Epidemiol. 3, 2333392816673290 (2016).
Blackmore, T. et al. Barriers and facilitators to colorectal cancer diagnosis in New Zealand: A qualitative study. BMC Fam. Pract. 21, 206 (2020).
Abu-Helalah, M. A. et al. Delay in presentation, diagnosis and treatment for colorectal cancer patients in Jordan. J. Gastrointest. Cancer 47, 36–46 (2016).
Zarcos-Pedrinac, I. et al. Factors associated with prolonged patient-attributable delay in the diagnosis of colorectal Cancer. Cancer Res. Treat. 50, 1270–1280 (2018).
Tfaily, M. A., et al. Awareness of colorectal cancer and attitudes towards its screening guidelines in Lebanon. Ann. Glob. Health. 85, https://doi.org/10.5334/aogh.2437 (2019).
Tong, S., Hughes, K., Oldenburg, B. B. & Mar, C. D. Colorectal cancer screening with faecal occult blood testing: Community intention, knowledge, beliefs and behaviour. Asia Pac. J. Public Health 18, 16–23 (2006).
Brandt, H. M., Dolinger, H. R., Sharpe, P. A., Hardin, J. W. & Berger, F. G. Relationship of colorectal cancer awareness and knowledge with colorectal cancer screening. Colorectal Cancer 1, 383–396 (2012).
Author information
Authors and Affiliations
Contributions
M.E., M.M.A., and F.K.H. contributed to design of the study, data analysis, data interpretation, and drafting of the manuscript. M.A., I.A., S.A.N., B.M.M., W.S.I., A.S., B.Y., Y.A.Q., M.F.D., R.R.S., R.T.J., K.A.A., M.E.A., M.M.H., I.I.A., B.K.A., M.N.A., A.S.A., M.S.A., O.A.A., R.A., C.T.G., A.Y.A., R.M.A.N., N.M.A., and S.M.S. contributed to design of the study, data collection, data entry, and data interpretation. N.A.E. and B.B. contributed to design of the study, data interpretation, drafting of the manuscript, and supervision of the work. All authors have read and approved the final manuscript. Each author has participated sufficiently in the work to take public responsibility for the content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elshami, M., Ayyad, M., Hamdan, F.K. et al. Perceived barriers to early presentation and symptom-specific time to seek medical advice for possible colorectal cancer symptoms among Palestinians. Sci Rep 13, 6871 (2023). https://doi.org/10.1038/s41598-023-34136-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34136-5
This article is cited by
-
Anticipated time to seek medical advice for possible lung cancer symptoms and barriers to timely presentation in Palestine: a national cross-sectional study
BMC Cancer (2024)
-
Anticipated time to seek medical advice for possible ovarian cancer symptoms and perceived barriers to early presentation among Palestinian women: a national cross-sectional study
BMC Cancer (2023)
-
Common myths and misconceptions about breast cancer causation among Palestinian women: a national cross-sectional study
BMC Public Health (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.