Abstract
The aim of this study was to forecast the risk factors of poor outcomes and postoperative loss of lordosis or recurrence of kyphosis. In this retrospective study, 101 patients with cervical spondylosis and preoperative kyphosis who underwent anterior cervical discectomy and fusion (ACDF) were enrolled, between June 2015 and June 2019. Patients were grouped according to the recovery rate of Japanese Orthopaedic Association (JOA) score whether more than 50%, and the change of postoperative cervical Cobb angle. There were 22 cases with less than 50% of recovery rate and 35 cases with the worsening of postoperative sagittal alignment (WPSA). Multivariate linear-regression analysis was conducted with the data. Advanced age (p = 0.019), longer duration of symptoms (p = 0.003) and loss of local Cobb angle (LCA) after surgery (p = 0.031) was significantly associated with a poor clinical outcome. A whole kyphosis (p = 0.009), aggravated neck pain after surgery (p = 0.012), preoperative lower thoracic 1 (T1) (p < 0.001), bigger change of C2-7 sagittal vertical axis (SVA) (p = 0.008) and adjacent segment degeneration (ASD) (p = 0.024) was significantly associated with the WPSA. Preoperative health education, nutritional support and early postoperative rehabilitation intervention, in perioperative period, were recommended for patients with advance age, longer duration of symptoms, whole cervical kyphosis and lower T1. Postoperative sagittal malalignment was related to neck pain and ASD after surgery.
Similar content being viewed by others
Introduction
Accompanied by the physiologic ageing process, the change of cervical sagittal alignment is a common result, which owes to degenerative changes in the discs and facet joints1,2. In addition, people’s professional and personal ways such as long hours of work or study with computers and mobile phones would lead to cervical sagittal malalignment. When a patient develops cervical kyphosis, the decreased cross-sectional area of the spinal canal, distortion of the spinal cord and neck pain may follow3,4. Although conservative treatment can alleviate progression of cervical kyphosis, surgery still play an important role in the correction of kyphosis5,6. However, it is also controversial whether the correction of kyphosis by an operation can improve the nerves and spinal cord to obtain a good postoperative outcome7,8,9. In addition, in previous studies of cervical anterior surgery, the postoperative less of lordosis and recurrence of kyphosis was rarely mentioned as a complication. Therefore, the purposes of this study were to investigate the predictors of poor outcome, while further to evaluate the risk factors of the worsening of postoperative sagittal alignment (WPSA).
Anterior and posterior decompression operations have been widely performed for patients with cervical spondylosis, which are effective procedures to improve the neurological outcome. However, the optimal surgical strategy in patients with cervical spondylosis particularly associated with kyphosis is debatable. Anterior procedure could adequately and directly remove isolated anterior pathologies, and posterior procedure was required for the treatment of the pathology over many vertebral segments10,11. Patients with sagittal kyphotic alignment might appear a poor outcome after posterior laminoplasty, due to insufficient posterior drift of the spinal cord and anterior impingement from kyphotic levels12,13. Hence, this investigation reviewed some cases that underwent an anterior cervical discectomy and fusion (ACDF). The object was to predict correlative factors of postoperative outcome and sagittal alignment, focusing especially on change of cervical curvature after surgery.
Material and methods
Study design
All procedures were approved by the Ethics Committee of the orthopedics hospital of XingTai, and were carried out in accordance with the relevant guidelines and regulations/ethical principles of the Declaration of Helsinki. We confirmed that informed consent was obtained from all participants. In addition, each patient was informed the risk factors and complications associated with treatment, treatment alternatives before surgery, and signed the written informed consents.
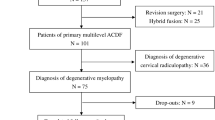
This retrospective study was based on medical records of patients who suffered from cervical spondylosis coexists with preoperative kyphosis. A total of 101 cases (47 males and 54 females) participated, all of whom underwent ACDF between June 2015 and June 2019. Inclusion criteria: patients with cervical kyphosis accompanied by cervical spondylotic radiculopathy (CSR) or cervical spondylotic myelopathy (CSM). The main reasons of cervical spondylosis included ossification of posterior longitudinal ligament, disc herniation and kyphotic alignment. Patients who underwent previous cervical surgery, combined posterior surgery, compression of spina cord or nerves resulting from tumors, fracture, infection, or congenital cervical deformity, missing imaging data and less than 12 months follow up were excluded.
Radiologic assessment
The standing lateral radiographs, computed tomography (CT) and magnetic resonance imaging (MRI) were performed for data collection at different stages of treatment. The lordosis and kyphosis were denoted by positive value and negative value, respectively. The C2–7 Cobb angle was defined as the angle of two lines of parallel to the inferior end plates of C2 and C7. Similarly, the local Cobb angle (LCA) was measured between the upper and lower vertebra of kyphotic segment. Hence, the cervical kyphosis was classified as whole type and local type. In addition, Park et al.14 reported that the T1 slope was correlated with the cervical sagittal alignment. The T1 slope was defined as the angle between the superior endplate of T1 and a horizontal line. The forward tilt and backward tilt of the superior endplate of T1 were denoted positive value and negative value, respectively. The C2–C7 SVA was defined as the distance between the plumb line of C2 centroid and posterior superior corner of C715. (Fig. 1) In this study, the loss of intervertebral height was measured on CT scan, and the change value more than 3 mm between pre-operation and last follow-up was defined as a noteworthy subsidence16,17. The above measurement methods were plotted on the figure. After surgery, less of lordotic alignment or recurrence of kyphosis was defined as the WPSA. The recurrence of kyphosis was defined as the absolute value of the C2–7 Cobb angle or LCA should be greater than 5° at the last follow-up. The diagnostic criteria of adjacent segment degeneration (ASD) included adjacent intervertebral height decreased by more than 3 mm, lower adjacent disc signal on T2-weighted MRI, vertebral posterior spur formation, more than 3 mm newly developed instability. To reduce the measurement errors of image data, the average value of three measurements was implemented. And all data was measured by one rater who was the first author: S.Q.L.
Clinical assessment
Each patient had a follow-up more than 12 months and was collected data at different times. The JOA score and Visual Analogue Score (VAS) were applied to evaluate the clinical outcome and neck pain degree. The (last follow-up JOA score -preoperative JOA score)/(17 − preoperative JOA score) × 100% was defined as the formula of evaluate clinal outcome. A score ≥ 75% was defined as excellent, ≥ 50% but < 75% as good, ≥ 25% but < 50% as fair, and < 25% as poor. In this study, the patients with recovery rates < 50% would be divided into the poor group. To avoid the interference of postoperative neck incision and muscle injury, the neck pain VAS score collected at 4–6 weeks after surgery.
Surgical procedure
In present study, the operative level was determined by patient’s physical condition, radiography, CT scan, MRI, and neurological examination. The main objective of the ACDF procedure was decompression of the spinal cord or nerves and corrected suitably the kyphosis of the cervical spine. We incised the skin on the right side of the neck and separated the muscle tissue by blunt dissection. After careful hemostasis, reaching the front of responsible vertebra through medial of the carotid sheath. We adequately resected diseased disc and released the uncovertebral joint on both sides. The kyphosis of cervical spinal was corrected by enlarging intervertebral space and changing intraoperative cervical curvature. After the decompression of spinal cord or nerves, an optimal polyether-ether-ketone (PEEK) cage with autogenous bone and anterior fixation of plate system were implant in an appropriate location. Finally, we sutured the incision and observed closely the oozing of blood and breathing state within 48 h after surgery (Fig. 2).
Case 25: a patients was 58 years, male, the walking unstable was main clinical symptom, the compression spinal cord due to herniation of intervertebral disc and cervical kyphosis, X-ray (a), CT (b,c) and MRI (e,f) before the ACDF. We performed single-level ACDF at C4/5, that decompressed spinal cord and corrected the cervical kyphosis (d,g,h). The walking unstable gradually improved during postoperative follow-up.
Statistical analyses
The means and standard deviations and frequencies were used to describe continuous variables and categorical variables, respectively. And the independent variables were analyzed by Mann–Whitney U-test, independent t-test and Chi-squared test. Multiple linear regression was applied to predict the correlation between the independent variables with a p-value less than 0.05 and dependent variable. The p < 0.05 represents a statistically significant difference. All analyses were performed using version SPSS software (version 22.0; SPSS Inc., Chicago, IL).
Results
A total of 101 cases were reviewed in this study, including 58 CSR patients and 43 CSM patients. There were 13 cases, 57 cases and 31 cases who underwent one segment, two segments and three segments ACDF procedure, respectively. By comparison of JOA score between pre-operation and last-follow, 22 cases were divided to the poor group with the recovery rates of JOA score greater less than 50%. Compared with the preoperative JOA score (10.96 ± 2.33), the JOA score at last follow-up (14.18 ± 1.95) had a statistically significant improvement (p < 0.001). There was no difference between the groups in terms of preoperative JOA score (p = 0.449), T1 slope (p = 0.189), and postoperative implant subsidence (p = 0.818) and ASD (p = 0.190). However, age (p = 0.002), duration of symptoms (p < 0.001), Disease classification (p = 0.024) and change of LCA after surgery (p = 0.011) was significantly difference between two groups (Table 1).
The multiple linear regression analyses predicted the risk factors of poor outcome, which showed a significant regression (p = 0.001) with an R2 of 0.168 and an adjusted R2 of 0.157. The model revealed that advance age (p = 0.019), longer duration of symptoms (p = 0.003) and loss of LCA after surgery (p = 0.031) was significant predictors of poor outcome (Table 2).
The less of lordosis and even recurrence of kyphosis occurred in some patients after surgery. Based on the change of sagittal alignment, the patients were divided to the maintained group and worsening group (Table 3). There was significant difference between the groups in terms of age (p = 0.031), classification of kyphosis (p = 0.002), recover rate of JOA score (p = 0.016), neck pain VAS score at last follow-up (p = 0.003), the change of neck pain VAS score (p = 0.007), preoperative T1 slope (p < 0.001), C2–7 SVA at last follow-up (p = 0.005), the change of C2–7 SVA after surgery (p = 0.001), and postoperative implant subsidence (p = 0.001) and ASD (p = 0.005). In addition, to determine the relationship between ASD and neck pain, change of neck pain VAS score between 4 and 6 weeks after surgery and last-follow was compared, which was 1.63 ± 1.21 and 1.46 ± 1.01 in patients with ASD or not, respectively (p = 0.183).
The multiple linear regression analyses predicted the risk factors of the WPSA, which showed a significant regression (p < 0.001) with an R2 of 0.302 and an adjusted R2 of 0.266. The model showed that patient with the whole kyphosis (p = 0.009), preoperative lower T1 slope (p < 0.001), aggravated neck pain (p = 0.012) and bigger C2–7 SVA (p = 0.008) after surgery, and ASD (p = 0.024) was significant predictors of the WPSA (Table 4).
Discussion
This part focuses on the risk factors of poor outcome, the relationship of T1 slope and the WPSA, influence of implant subsidence, the relationship of ASD and cervical kyphosis and the relationship of chronic pain and the WPSA. An optimal surgical approach and adequate decompression of spinal cord and nerves are the precondition of good postoperative outcome. The maintain of cervical lordosis have be considered an important factor for the long-term clinical outcome7. Moreover, Kim et al.3 showed that the less of lordosis after surgery would contribute to the reduction of relative cross-sectional area of spinal canal. However, Kaptain et al.8 deem clinical outcome was not association with the postoperative sagittal alignment. It remained controversial that the relationship between the correction of kyphosis and the improvement of neurological functions. In present study, the change of postoperative LCA was significantly related to the poor outcome, but the change of postoperative C2–7 Cobb was not associate with the poor outcome. Because of the effect of sigmoid alignment on the C2–7 Cobb, we thought that the LCA was more suitable for evaluation of the spinal cord compression. In addition, age and duration of symptoms were considered as predictors of poor outcome after surgery.
The T1 slope was supposed to be an important information of cervical curvature correction14. In previous study, T1 slope was frequently used as a risk factor to predict the less of lordosis after laminoplasty18,19. However, it was not usually evaluated in patient who underwent ACDF. In this research, the WPSA was significantly related to preoperative lower T1 slope, especially when the T1 slope was negative value before surgery. There were 17 patients with a negative value, and 14 of them happened the WPSA. By comparing the change of T1 slope angle before and after surgery, the T1 slope angle was relatively stable in this study. According to this conclusion, we considered that ACDF operation could correct the local kyphosis, but to ensure sagittal balance of the cervical spine, that a low T1 slope angle required a small lordosis of the lower cervical spine. Hence, the preoperative lower T1 slope might contributed to the WPSA.
There were eight patients occurred the implant subsidence in this study. Lee et al.20 thought that the lower T1 slope was a risk factor of implant subsidence. Suh et al.21 thought that cage morphology and material composition were related to the implant subsidence. However, we more likely to consider the early fusion was the determinant of implant subsidence. The results showed that the implant subsidence was not significantly related to the WPSA by multiple linear regression. The relatively small number of patients with cage subsidence might affect the result. In addition, there was a significant correlation between the whole type of cervical kyphosis and the WPSA. This reason might be a certain degree of limitation of anterior surgery on overall correction of the cervical kyphosis.
The intervertebral space narrowing was one of the important causes of postoperative ASD, while was an inevitable result of implant subsidence. In previous studies, Barsa et al.22 thought implant subsidence could accelerate cervical degenerative changes in adjacent segments. Lazic et al.23 showed that intervertebral spaces were positively correlated with cervical lordosis. Hence, we searched the relationship between the ASD and change of postoperative cervical curvature. The present result showed that the patients with ASD would contribute to the less of lordosis and even recurrence of kyphosis after surgery. This was related to the cause of ASD formation, such as instability and stress change in the adjacent motion segments. In addition, Risbud et al.24 found that degeneration of the intervertebral discs was a major contributor to neck pain, which physiologically based. However, the occurrence of ASD after surgery did not provide a powerful evidence for chronic neck pain in this study.
Chronic neck pain is a common symptom in patient with cervical vertebra degeneration24. Relieving neck pain could improve patient’s the quality of life and postoperative satisfaction. However, it remained controversial whether there was a connection between the neck pain and sagittal malalignment. Grob et al.25 thought cervical structural abnormalities was not necessarily indicative of the cause of pain. Whereas, Ferch et al.4 thought that neck pain could be alleviated by correcting and maintaining the physiological lordosis of cervical spine. In addition, some scholars found that there was a significant relationship between cervical muscular imbalance and the loss of physiological lordosis26. And the muscular imbalance was the one of important factors of choric pain. Based on the viewpoints of previous studies, we further investigated whether postoperative chronic pain was related to the WPSA. The results showed that the less of lordosis or recurrence of kyphosis after surgery would contribute to persistent neck pain.
In this study, several limitations should be presented. Firstly, this was a single-center retrospective study, and 12 months of follow-up was relatively short. However, a longer follow-up did not obtain a significant change of clinical and radiologic over 24 months after 6 months27. Secondly, the SF-36 scale and the HR-QOL scale were not applied to the evaluation of postoperative outcome. Thirdly, this study was not considered the correlation between the cervical sagittal alignment and thoracolumbar or spino-pelvic parameters. Fourthly, it is worthful to the orientation of study by investigating the relationship between postoperative outcome and clinical supports which including perioperative nutritional support and anti-osteoporosis therapy. Finally, all the imaging data were measured by one rater, and the intra-rater errors were inevitable. Although several limitations were included in this study, preoperative T1 slope and type of cervical kyphosis were meaningful preoperative parameters for predicting the change of postoperative cervical curvature. The results could helpful to improve the postoperative outcome and to determine whether anterior procedure was optimum selection.
Conclusion
Preoperative health education, nutritional support and early postoperative rehabilitation intervention, in perioperative period, were recommend for patients with advance age, longer duration of symptoms, whole cervical kyphosis and lower T1. In addition, postoperative sagittal malalignment was related to neck pain and ASD after surgery.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Rao, R. D. et al. Degenerative cervical spondylosis: Clinical syndromes, pathogenesis, and management. J. Bone Jt. Surg.-Am. 89A, 1360–1378 (2007).
Hardacker, J. W., Shuford, R. F., Capicotto, P. N. & Pryor, P. W. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine 22, 1472–1479. https://doi.org/10.1097/00007632-199707010-00009 (1997).
Kim, K. R., Lee, C. K., Park, J. Y. & Kim, I. S. Preoperative parameters for predicting the loss of lordosis after cervical laminoplasty. Spine 45, 1476–1484. https://doi.org/10.1097/brs.0000000000003604 (2020).
Ferch, R. D., Shad, A., Cadoux-Hudson, T. A. D. & Teddy, P. J. Anterior correction of cervical kyphotic deformity: Effects on myelopathy, neck pain, and sagittal alignment. J. Neurosurg. 100, 13–19. https://doi.org/10.3171/spi.2004.100.1.0013 (2004).
Guinn, J. M. V., Pennicooke, B., Rivera, J., Mummaneni, P. V. & Chou, D. Anterior cervical discectomy with fusion and plating for correction of degenerative cervical kyphosis: 2-dimensional operative video. Oper. Neurosurg. 20, E214–E214. https://doi.org/10.1093/ons/opaa339 (2021).
Han, K. et al. Surgical treatment of cervical kyphosis. Eur. Spine J. 20, 523–536. https://doi.org/10.1007/s00586-010-1602-8 (2011).
Wu, W. J., Jiang, L. S., Liang, Y. & Dai, L. Y. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur. Spine J. 21, 1374–1382. https://doi.org/10.1007/s00586-011-2131-9 (2012).
Kaptain, G. J., Simmons, N. E., Replogle, R. E. & Pobereskin, L. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J. Neurosurg. 93, 199–204. https://doi.org/10.3171/spi.2000.93.2.0199 (2000).
Uchida, K. et al. Cervical spondylotic myelopathy associated with kyphosis or sagittal sigmoid alignment: Outcome after anterior or posterior decompression. J. Neurosurg.-Spine 11, 521–528. https://doi.org/10.3171/2009.2.Spine08385 (2009).
Kawakami, M. et al. A comparative study of surgical approaches for cervical compressive myelopathy. Clin. Orthopaed. Relat. Res. 381, 129–136 (2000).
Cabraja, M., Abbushi, A., Koeppen, D., Kroppenstedt, S. & Woiciechowsky, C. Comparison between anterior and posterior decompression with instrumentation for cervical spondylotic myelopathy: Sagittal alignment and clinical outcome. Neurosurg. Focus. https://doi.org/10.3171/2010.1.Focus09253 (2010).
Taniyama, T. et al. Modified K-line in magnetic resonance imaging predicts clinical outcome in patients with nonlordotic alignment after laminoplasty for cervical spondylotic myelopathy. Spine 39, E1261–E1268. https://doi.org/10.1097/brs.0000000000000531 (2014).
Taniyama, T. et al. Modified K-line in magnetic resonance imaging predicts insufficient decompression of cervical laminoplasty. Spine 38, 496–501. https://doi.org/10.1097/BRS.0b013e318273a4f7 (2013).
Park, J. H. et al. T1 slope and cervical sagittal alignment on cervical CT radiographs of asymptomatic persons. J. Korean Neurosurg. Soc. 53, 356–359. https://doi.org/10.3340/jkns.2013.53.6.356 (2013).
Kim, B. et al. Relationship between T1 slope and loss of lordosis after laminoplasty in patients with cervical ossification of the posterior longitudinal ligament. Spine J. 16, 219–225. https://doi.org/10.1016/j.spinee.2015.10.042 (2016).
Maccormick, A. P. & Sharma, H. Analysis of the variables affecting the incidence, location, and severity of cage subsidence following anterior cervical discectomy and fusion operation. Int. J. Spine Surg. 14, 896–900. https://doi.org/10.14444/7137 (2020).
Noh, S. H. et al. Association of complete uncinate process removal on 2-year assessment of radiologic outcomes: Subsidence and sagittal balance in patients receiving one-level anterior cervical discectomy and fusion. BMC Musculoskelet. Disord. https://doi.org/10.1186/s12891-020-03443-7 (2020).
Hyun, S. J., Kim, K. J., Jahng, T. A. & Kim, H. J. Relationship between T1 slope and cervical alignment following multilevel posterior cervical fusion surgery impact of T1 slope minus cervical lordosis. Spine 41, E396–E402. https://doi.org/10.1097/brs.0000000000001264 (2016).
Kim, T. H., Lee, S. Y., Kim, Y. C., Park, M. S. & Kim, S. W. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine 38, E992–E997. https://doi.org/10.1097/BRS.0b013e3182972e1b (2013).
Lee, S. H. et al. A lower T1 slope as a predictor of subsidence in anterior cervical discectomy and fusion with stand-alone cages. J. Korean Neurosurg. Soc. 60, 567–576. https://doi.org/10.3340/jkns.2017.0404.001 (2017).
Suh, P. B., Puttlitz, C., Lewis, C., Bal, B. S. & McGilvray, K. The effect of cervical interbody cage morphology, material composition, and substrate density on cage subsidence. J. Am. Acad. Orthop. Surg. 25, 160–168. https://doi.org/10.5435/jaaos-d-16-00390 (2017).
Barsa, P. & Suchomel, P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur. Spine J. 16, 1395–1400. https://doi.org/10.1007/s00586-006-0284-8 (2007).
Lazic, E., Glisic, B., Stamenkovic, Z. & Nedeljkovic, N. Changes in cervical lordosis and cervicovertebral morphology in different ages with the possibility of estimating skeletal maturity. Srp. Arh. Celok. Lek. 143, 662–668. https://doi.org/10.2298/sarh1512662l (2015).
Risbud, M. V. & Shapiro, I. M. Role of cytokines in intervertebral disc degeneration: pain and disc content. Nat. Rev. Rheumatol. 10, 44–56. https://doi.org/10.1038/nrrheum.2013.160 (2014).
Grob, D., Frauenfelder, H. & Mannion, A. F. The association between cervical spine curvature and neck pain. Eur. Spine J. 16, 669–678. https://doi.org/10.1007/s00586-006-0254-1 (2007).
Yoon, S. Y., Moon, H. I., Lee, S. C., Eun, N. L. & Kim, Y. W. Association between cervical lordotic curvature and cervical muscle cross-sectional area in patients with loss of cervical lordosis. Clin. Anat. 31, 710–715. https://doi.org/10.1002/ca.23074 (2018).
Wang, B., Lu, G. H. & Kuang, L. Anterior cervical discectomy and fusion with stand-alone anchored cages versus posterior laminectomy and fusion for four-level cervical spondylotic myelopathy: A retrospective study with 2-year follow-up. BMC Musculoskelet. Disord. https://doi.org/10.1186/s12891-018-2136-1 (2018).
Acknowledgements
This work was supported by the Xingtai General Hospital of North China Medical Health Group, and thanks for every patient’s recognition. The project number: 2022ZC250.
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: S.Q.L. and X.P.P.; Collected data: S.Q.L., Q.L. and Q.Y.; Statistical analysis: B.Q.B.; Wrote the paper: S.Q.L.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, S., Bai, B., Li, Q. et al. Predicting surgical outcome and sagittal alignment change in patients with cervical spondylosis and degenerative kyphosis after anterior cervical discectomy and fusion. Sci Rep 13, 6704 (2023). https://doi.org/10.1038/s41598-023-34029-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34029-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.