Abstract
Study design
Retrospective multicenter study.
Objective
To compare the surgical outcomes and complications of posterior decompression between individuals with cervical spondylotic myelopathy (CSM) and those with ossification of the posterior longitudinal ligament (OPLL).
Setting
Seventeen medical institutions in Japan.
Methods
This study included 814 individuals with CSM (n = 636) and OPLL (n = 178) who underwent posterior decompression. Propensity score matching of the baseline characteristics was performed to compare surgical outcomes and perioperative complications between the CSM and OPLL groups.
Results
Before propensity score matching, the OPLL group had higher percentage of male individuals, body mass index, and number of stenosis levels and longer duration of symptoms (P < 0.01, P < 0.01, P < 0.01, and P < 0.01, respectively). After matching, the baseline characteristics were comparable between the CSM (n = 98) and OPLL (n = 98) groups. The postoperative Japanese Orthopaedic Association (JOA) scores, preoperative-to-postoperative changes in the JOA scores, and JOA score recovery rates were not significantly different between the groups (P = 0.42, P = 0.47, and P = 0.09, respectively). The postoperative visual analog scale (VAS) score for neck pain and preoperative-to-postoperative changes in the VAS score for neck pain were not significantly different between the groups (P = 0.25 and P = 0.50, respectively). The incidence of perioperative complications was comparable between groups.
Conclusion
Neurological improvement and complication rates after surgery were comparable between individuals with CSM and those with OPLL, suggesting similar effectiveness and safety of posterior decompression for both conditions.
Similar content being viewed by others
Introduction
Degenerative cervical myelopathy (DCM) causes spinal cord dysfunction in the elderly, and it covers a variety of spinal cord compressive diseases such as cervical spondylotic myelopathy (CSM), ossification of the posterior longitudinal ligament (OPLL), and disc herniation [1]. Individuals with minimal symptoms can be treated conservatively; however, those with progressive myelopathy require surgery. Surgical decompression with or without fixation is widely accepted as an effective treatment option for DCM, as it halts the progression of symptoms and improves neurological outcomes and quality of life [2].
CSM is a degenerative disease caused by spondylotic changes of the cervical spine, including disc degeneration, osteophytes, hyperostosis of the uncovertebral joint, facet hypertrophy, and ligamentum flavum buckling, resulting in circumferential stenosis of the spinal canal [3]. Meanwhile, OPLL is a multifactorial disorder most commonly observed in Asian countries and is caused by ectopic ossification and hyperostosis of the posterior longitudinal ligament [4,5,6]. Cervical stenosis in individuals with OPLL is mainly induced by anterior factors. Although CSM and OPLL have different underlying mechanisms of disease, posterior cervical decompression is commonly used as a surgical treatment for both diseases. A previous prospective study revealed comparable improvements in neurological function between OPLL and other forms of DCM after miscellaneous surgical techniques, including anterior and/or posterior approach with or without fusion [7]. In their study, Nakashima et al. reported other forms of DCM, such as heterogenous diseases including myelopathy secondary to spondylosis, disc herniation, subluxation, and hypertrophied ligamentum flavum [7]. However, the authors compared surgical outcomes between OPLL and other forms of DCM after miscellaneous surgical techniques [7], and thus, the neurological outcomes after a single surgical procedure may differ between OPLL and CSM. Although a few studies have compared the surgical outcomes between CSM and OPLL after posterior cervical decompression, their results vary [8,9,10]. Two studies reported comparable outcomes in both CSM and OPLL individuals [8, 9], but another study showed worse neurological recovery in individuals with OPLL [10]. These inconsistent surgical outcomes may be due to the small sample size of those previous studies. To the best of our knowledge, there are no big-data studies comparing the surgical outcomes between CSM and OPLL after posterior cervical decompression. The present multicenter large cohort study investigated if the difference in the underlying mechanisms of spinal cord compression between CSM and OPLL has an effect on their surgical outcomes. Therefore, propensity score matching was performed to adjust for baseline characteristics. Subsequently, neurological outcomes and perioperative complications after posterior cervical decompression were compared between individuals with CSM and those with OPLL.
Materials and methods
Subjects
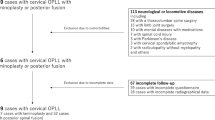
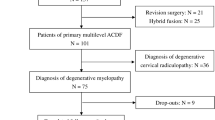
A total of 864 consecutive individuals with clinically and radiographically confirmed DCM who underwent posterior decompression in 17 medical institutes between January 2012 and December 2014 were included in our retrospective database. In the present study, 814 individuals with available data on the number of intervertebral levels of stenosis were included. The participant follow-up period was a minimum of 12 months after surgery. The inclusion criteria were DCM with at least 1 clinical sign of myelopathy, radiologic evidence of spinal cord compression on magnetic resonance imaging or cervical myelogram–computed tomography (CT), and no previous history of cervical spine surgery. The exclusion criteria were individuals with radiculopathy but without myelopathy and those who were diagnosed with infection, trauma, rheumatoid arthritis, ankylosing spondylitis, spinal tumors, or concomitant lumbar stenosis. The attending spine surgeon at each institute divided the individuals into two groups: individuals with radiographic evidence of OPLL (n = 178) and those with CSM (n = 636). We defined OPLL as ossification of the posterior longitudinal ligament with a thickness >2 mm on CT) according to previous studies [11, 12]. Osteophytes near the uncovertebral joint or at the corners of the vertebra were not diagnosed as OPLL.
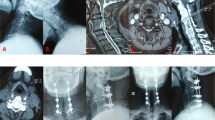
Indication and techniques of surgical decompression
Attending spine surgeons at each institute performed three different surgical techniques of posterior cervical decompression (expansive open-door laminoplasty [ELAP] [13], double-door laminoplasty [DD] [14], and muscle-preserving selective laminectomy [SL] [15, 16]). Surgical indication, technique, and number of intervertebral levels decompressed were decided by spine surgeons at each institute.
Data collection
The attending spine surgeons retrospectively collected the participants’ demographic data (age, sex, duration of symptoms, follow-up period, body mass index [BMI], smoking history, medical history, and the Charlson comorbidity index). Surgical details (ELAP, DD, or SL), operation time, blood loss, number of intervertebral levels of stenosis, number of intervertebral levels decompressed, and duration of symptoms were provided by the attending spine surgeon. Subjects were assessed at the preoperative stage and final follow-up using clinical outcome measures, including the Japanese Orthopaedic Association (JOA) score system for cervical myelopathy and the visual analog scale (VAS) score for neck pain. Hirabayashi’s method was used to calculate the recovery rate (RR) of the JOA score: (postoperative JOA scores − preoperative JOA scores)/(17 − preoperative JOA scores) × 100% [13]. The attending spine surgeon monitored perioperative complications within 30 days after surgery (i.e., C5 palsy, surgical site infection [SSI], hematoma, dural tear, delirium, and neurological deterioration). On a preoperative neutral lateral radiograph, the K-line was defined as the straight line joining the midpoint of the C2 spinal canal to the midpoint of the C7 spinal canal [17]. K-line was defined as (+) when the OPLL mass never crossed the K-line posteriorly, whereas K-line was defined as (−) when the OPLL mass crossed the K-line posteriorly. Using the midsagittal image of the cervical CT, we defined the OPLL occupancy ratio as the anterior-to-posterior ratio of the OPLL diameter on its thickest part to the diameter of the spinal canal [4].
Statistical analysis
Participants’ characteristics and perioperative and postoperative data were compared between the CSM and OPLL groups using unpaired t-test or Mann–Whitney U test for continuous variables and chi-square test for categorical variables, as appropriate for data distribution. Propensity score matching was performed to compare the surgical outcomes, perioperative complications, and radiological parameters between the groups. A logistic regression model was used to calculate the propensity scores. The moderator variables were age at surgery, sex, BMI, smoking history, diabetes mellitus, the Charlson comorbidity index, duration of symptoms, number of intervertebral levels of stenosis, preoperative JOA scores, and preoperative VAS score for neck pain. To adjust for individual characteristics, we performed 1-to-1 matching with fixed caliper widths (0.03) without replacement. Accordingly, a case in the CSM group was matched to a case in the OPLL group with the same propensity score. Pairs comprising 1 participant with CSM and 1 participant with OPLL were collected to form two groups (the CSM and OPLL groups). The standardized difference was used to measure the covariate balance. A standardized difference of <10% was regarded as an ignorable difference between the groups. A paired t-test was used to compare the JOA scores and VAS scores for neck pain between the preoperative and postoperative stages. All statistical analyses were performed with SPSS version 26.0 (IBM Corp., Armonk, NY). Continuous variables are presented as mean ± standard deviation or median (interquartile range). Statistical significance was set at P < 0.05.
Results
Individuals’ characteristics
The present study included 814 DCM individuals consisted of 562 men (69%) and 252 women (31%), with a mean age at surgery (±standard deviation) of 66 ± 12 years. Of the study cohort, 636 individuals (78%) were diagnosed with CSM, whereas 178 individuals (22%) displayed OPLL. The percentage of male in participants with OPLL was significantly higher than that of participants with CSM (P < 0.01). The BMI in the participants with OPLL was on average 1.7 (95% CI, 1.1–2.4) kg/m2 higher than that in the participants with CSM (P < 0.01). The number of intervertebral levels of stenosis in the OPLL group was on average 0.28 (95% CI, 0.10–0.46) higher than that in the CSM group (P < 0.01). The duration of symptoms was longer in participants with OPLL than in those with CSM (P < 0.01). Individuals with OPLL tended to have a high prevalence of diabetes and smoking history (P = 0.06 and P = 0.06, respectively). There was no significant difference in age at surgery, the Charlson comorbidity index, preoperative JOA scores, and preoperative VAS score for neck pain between the CSM and OPLL groups (Table 1). In the present study, 87% of individuals with OPLL were K-line (+), and the mean OPLL occupancy ratio was 37 ± 13%.
Individuals’ perioperative and postoperative data
The number of decompressed intervertebral levels in the OPLL group was on average 0.48 (95% CI, 0.34–0.62) higher than that in the CSM group (P < 0.01). The operation time in the OPLL group was on average 17 (95% CI, 8.0–26) minutes longer than that in the CSM group (P < 0.01). The blood loss was greater in the OPLL group than in the CSM group (P < 0.01). There was no significant difference between the groups in terms of the surgical technique, complication rates for C5 palsy, SSI, hematoma, dural tear, delirium, or neurological deterioration (Table 2). No significant differences were observed in the postoperative JOA scores, preoperative-to-postoperative changes in the JOA scores, or JOA score RR between the groups. Both the CSM and OPLL groups showed significant improvement in the JOA scores postoperatively (CSM group: 3.0 ± 2.1, 95% CI, 2.9–3.2, P < 0.01; OPLL group: 3.0 ± 2.3, 95% CI, 2.6–3.3, P < 0.01). The postoperative VAS scores for neck pain and preoperative-to-postoperative changes in the VAS score for neck pain were not significantly different between the groups. Both the CSM and OPLL groups showed a significant reduction in the VAS score for neck pain postoperatively (CSM group: −1.4 ± 2.7, 95% CI, −1.6 to −1.1, P < 0.01; OPLL group: −1.0 ± 2.7, 95% CI, −1.5 to −0.48, P < 0.01) (Table 2).
Individuals’ characteristics of the matched groups
After propensity score matching of the individuals’ characteristics, the CSM and OPLL groups had 98 individuals each. We observed no significant differences between the groups regarding age at surgery, sex ratio, BMI, smoking history, prevalence of diabetes, the Charlson comorbidity index, duration of symptoms, number of intervertebral levels of stenosis, preoperative JOA scores, and preoperative VAS score for neck pain. In the matched cohort, the standardized difference in covariates was <10% (Table 3). After propensity score matching, 87% of individuals with OPLL were K-line (+), and the OPLL occupancy ratio was 38 ± 13%.
Individuals’ perioperative and postoperative data of the matched groups
The number of decompressed intervertebral levels in the OPLL group was on average 0.35 (95% CI, 0.11–0.58) higher than that in the CSM group (P < 0.01) (Table 4). There was no significant difference in surgical technique, operation time, or blood loss between the CSM and OPLL groups. We observed no significant difference in the complication rates for C5 palsy, SSI, hematoma, delirium, or neurological deterioration between the groups. Dural tear was not observed in either group (Table 4). The postoperative JOA scores, preoperative-to-postoperative changes in the JOA scores, and JOA score RR between the groups were not significantly different. Both the CSM and OPLL groups demonstrated significant improvement in the JOA scores postoperatively (CSM group: 3.1 ± 2.2, 95% CI, 2.7–3.6, P < 0.01; OPLL group: 2.9 ± 2.5, 95% CI, 2.4–3.4, P < 0.01). The postoperative VAS score for neck pain and preoperative-to-postoperative changes in the VAS score for neck pain between the groups were not significantly different. Both the CSM and OPLL groups showed a significant reduction in the VAS score for neck pain postoperatively (CSM group: −1.3 ± 2.9, 95% CI, −1.9–0.7, P < 0.01; OPLL group: −1.0 ± 2.7, 95% CI, −1.5 to −0.50, P < 0.01) (Table 4).
Discussion
To the best of our knowledge, this is the first multicenter large cohort study to compare the surgical outcomes of posterior cervical decompression between CSM and OPLL using propensity score-matched analysis. The improvements after surgery assessed by the JOA score and VAS score for neck pain seen in participants with OPLL were comparable with those observed in participants with CSM. Moreover, perioperative complication rates were comparable between the groups. This study demonstrated no significant differences in effectiveness and safety of posterior cervical decompression for CSM and OPLL.
In general, cervical OPLL is more commonly observed in the Asian population [5, 18]. The incidence of OPLL in normal populations or asymptomatic individuals based on CT findings was 6.3% in Japan, 5.7% in South Korea, and 1.3–3.2% in the United States [11, 12, 19]. Meanwhile, the prevalence of OPLL in 7210 individuals with DCM was 18% in the Chinese population [20]. Consistently, the prevalence of OPLL was 22% in our Japanese cohort of DCM. We suggest that the incidence of OPLL in individuals with DCM is ~20% in the Asian population. Previous studies reported that the prevalence of DCM in male individuals was statistically higher than that in female individuals [12, 19, 20]. Consistently, 69% of the DCM participants in the present study were male. Moreover, the percentage of male individuals with OPLL (79%) was significantly higher than that in individuals with CSM (66%). Similar results were reported in a previous study in which the percentage of male individuals was higher in those with OPLL (68%) than in those with other forms of DCM (62%) [20]. Similarly, our results suggest that the percentage of male participants is higher in those with OPLL than in those with CSM.
Consistent with the findings of the present study, a previous study observed a higher BMI in individuals with OPLL than in individuals without OPLL [11]. A higher BMI was also reported as a risk factor for OPLL [21]. Another study demonstrated direct correlations of BMI with the extent of OPLL in the multiple regression analysis [22]. Liao et al. reported that the prevalence of OPLL in the overweight population was significantly higher than that in the normal-weight population, and the obesity population showed the highest prevalence [20]. Diabetes was reported as a risk factor of OPLL in previous studies [21,22,23]. Compared with participants with CSM, a tendency toward a high prevalence of diabetes was observed in participants with OPLL in the present study. Moreover, Akune et al. reported that the extent of OPLL was positively associated with the insulin secretory response [22]. The duration of symptoms was longer in participants with OPLL than in participants with CSM, suggesting that the slow progression of neurological symptoms due to slow growth of ossification influences the longer duration of symptoms before surgery. We observed a higher number of intervertebral levels of stenosis in participants with OPLL than in those with CSM. As the OPLL progresses, ossification extends to the upper and/or lower levels of the cervical spine, resulting in a higher number of stenosis levels in individuals with OPLL.
In the present study, we aimed to reveal the effect of different underlying mechanisms of spinal cord compression between CSM and OPLL on surgical outcomes. As we observed some differences in baseline characteristics, propensity score matching was used to reduce the influence of baseline differences on the comparison of surgical outcomes between individuals with CSM and those with OPLL. As the baseline factors were appropriately adjusted between the CSM and OPLL groups after propensity score matching, the possible confounding factors did not affect the results of this study. Our results showed that the improvements after surgery assessed by the JOA scores and VAS score for neck pain were not significantly different between the participants with CSM and those with OPLL. In general, spine surgeons tend to perform extensive decompression in individuals with OPLL because ossification progression was reported after posterior cervical decompression for OPLL individuals [24, 25]. Indeed, a higher number of intervertebral levels were surgically decompressed in the OPLL group than in the CSM group after matching the number of intervertebral levels of stenosis in the present study. Age and operation time were important predictors of surgical complications [26]. After propensity score matching, no significant difference was observed in age and operation time between participants with CSM and OPLL. We found that the incidence of complications after posterior cervical decompression was comparable between participants with CSM and those with OPLL. Therefore, posterior cervical decompression can be performed equally safely for OPLL and CSM.
The present study has several limitations. First, this was a retrospective study, which inevitably included selection bias. Second, a period of at least 1 year of follow-up after surgery was relatively short for a retrospective study, and long-term surgical outcomes were not assessed. Further studies with a longer follow-up period should be performed to confirm the results of the present study. Third, surgical outcomes, such as health-related quality of life outcomes, were not evaluated with objective individual-based outcome measures. Fourth, the indications for surgery and choice of surgical technique were left to the spine surgeon’s discretion at each institute. Fifth, although we accurately analyzed the effect of different underlying mechanisms of spinal cord compression between CSM and OPLL on their surgical outcomes, propensity score matching of disease specific difference in baseline characteristics may affect the results of the study. Finally, propensity score matching may cause some biases because data from unmatched individuals were not analyzed in the comparison of surgical outcomes between individuals with CSM and those with OPLL.
Conclusion
Propensity score-matched analysis revealed that neurological improvement and perioperative complication rates after posterior cervical decompression were not significantly different between individuals with CSM and those with OPLL in a short-term follow-up. Posterior cervical decompression is an equally effective and safe treatment option for CSM and OPLL; however, this finding requires further validation.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative Cervical Myelopathy: Epidemiology, Genetics, and Pathogenesis. Spine (Philos Pa 1976). 2015;40:E675–93.
Fehlings MG, Wilson JR, Kopjar B, Yoon ST, Arnold PM, Massicotte EM, et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: results of the AOSpine North America prospective multi-center study. J Bone Jt Surg Am. 2013;95:1651–8.
Parke WW. Correlative anatomy of cervical spondylotic myelopathy. Spine (Philos Pa 1976). 1988;13:831–7.
Abiola R, Rubery P, Mesfin A. Ossification of the Posterior Longitudinal Ligament: Etiology, Diagnosis, and Outcomes of Nonoperative and Operative Management. Glob Spine J. 2016;6:195–204.
Matsunaga S, Sakou T. Ossification of the posterior longitudinal ligament of the cervical spine: etiology and natural history. Spine (Philos Pa 1976). 2012;37:E309–14.
Nagoshi N, Tetreault LA, Nakashima H, Nouri A, Arnold P, Zileli M, et al. Do Caucasians and East Asians have Different Outcomes Following Surgery for the Treatment of Degenerative Cervical Myelopathy?: Results From the Prospective Multicenter AOSpine International Study. Spine (Philos Pa 1976). 2016;41:1428–35.
Nakashima H, Tetreault L, Nagoshi N, Nouri A, Arnold P, Yukawa Y, et al. Comparison of Outcomes of Surgical Treatment for Ossification of the Posterior Longitudinal Ligament Versus Other Forms of Degenerative Cervical Myelopathy: Results from the Prospective, Multicenter AOSpine CSM-International Study of 479 Patients. J Bone Jt Surg Am. 2016;98:370–8.
Yu D, Jeon I. Comparison of Radiological and Functional Changes After Multi-Level Laminoplasty Between Cervical Spondylotic Myelopathy and Ossification of the Posterior Longitudinal Ligament. Turk Neurosurg. 2021;31:432–40.
Meyer SA, Wu JC, Mummaneni PV. Laminoplasty outcomes: is there a difference between patients with degenerative stenosis and those with ossification of the posterior longitudinal ligament? Neurosurg Focus. 2011;30:E9.
Nori S, Aoyama R, Ninomiya K, Suzuki S, Anazawa U, Shiraishi T, et al. Ossified Posterior Longitudinal Ligament Existing at an Intervertebral Level Limits Compensatory Mechanism of Cervical Lordosis after Muscle-Preserving Selective Laminectomy. Spine Surg Relat Res. 2019;3:312–8.
Fujimori T, Le H, Hu SS, Chin C, Pekmezci M, Schairer W, et al. Ossification of the posterior longitudinal ligament of the cervical spine in 3161 patients: a CT-based study. Spine (Philos Pa 1976). 2015;40:E394–403.
Fujimori T, Watabe T, Iwamoto Y, Hamada S, Iwasaki M, Oda T, et al. Prevalence, Concomitance, and Distribution of Ossification of the Spinal Ligaments: Results of Whole Spine CT Scans in 1500 Japanese Patients. Spine (Philos Pa 1976). 2016;41:1668–76.
Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Philos Pa 1976). 1981;6:354–64.
Seichi A, Takeshita K, Ohishi I, Kawaguchi H, Akune T, Anamizu Y, et al. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine (Philos Pa 1976). 2001;26:479–87.
Nori S, Shiraishi T, Aoyama R, Ninomiya K, Yamane J, Kitamura K, et al. Muscle-Preserving Selective Laminectomy Maintained the Compensatory Mechanism of Cervical Lordosis After Surgery. Spine (Philos Pa 1976). 2018;43:542–9.
Shiraishi T, Kato M, Yato Y, Ueda S, Aoyama R, Yamane J, et al. New techniques for exposure of posterior cervical spine through intermuscular planes and their surgical application. Spine (Philos Pa 1976). 2012;37:E286–96.
Fujiyoshi T, Yamazaki M, Kawabe J, Endo T, Furuya T, Koda M, et al. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine (Philos Pa 1976). 2008;33:E990–3.
Inamasu J, Guiot BH, Sachs DC. Ossification of the posterior longitudinal ligament: an update on its biology, epidemiology, and natural history. Neurosurgery. 2006;58:1027–39.
Sohn S, Chung CK, Yun TJ, Sohn CH. Epidemiological survey of ossification of the posterior longitudinal ligament in an adult Korean population: three-dimensional computed tomographic observation of 3,240 cases. Calcif Tissue Int. 2014;94:613–20.
Liao X, Jin Z, Shi L, Zhao Y, Zhou S, Chen D, et al. Prevalence of Ossification of Posterior Longitudinal Ligament in Patients With Degenerative Cervical Myelopathy: Cervical Spine 3D CT Observations in 7210 Cases. Spine (Philos Pa 1976). 2020;45:1320–8.
Kobashi G, Washio M, Okamoto K, Sasaki S, Yokoyama T, Miyake Y, et al. High body mass index after age 20 and diabetes mellitus are independent risk factors for ossification of the posterior longitudinal ligament of the spine in Japanese subjects: a case-control study in multiple hospitals. Spine (Philos Pa 1976). 2004;29:1006–10.
Akune T, Ogata N, Seichi A, Ohnishi I, Nakamura K, Kawaguchi H. Insulin secretory response is positively associated with the extent of ossification of the posterior longitudinal ligament of the spine. J Bone Jt Surg Am. 2001;83:1537–44.
Tsuyama N. Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res. 1984;184:71–84.
Wang L, Jiang Y, Li M, Qi L. Postoperative Progression of Cervical Ossification of Posterior Longitudinal. Ligament: Syst Rev World Neurosurg. 2019;126:593–600.
Ogawa Y, Toyama Y, Chiba K, Matsumoto M, Nakamura M, Takaishi H, et al. Long-term results of expansive open-door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine. 2004;1:168–74.
Fehlings MG, Smith JS, Kopjar B, Arnold PM, Yoon ST, Vaccaro AR, et al. Perioperative and delayed complications associated with the surgical treatment of cervical spondylotic myelopathy based on 302 patients from the AOSpine North America Cervical Spondylotic Myelopathy Study. J Neurosurg Spine. 2012;16:425–32.
Acknowledgements
The authors thank Takahito Iga, MD, Ryoma Aoyama, MD, PhD, Norihiro Isogai, MD, PhD, Kazuki Takeda, MD, PhD, Morito Takano, MD, PhD, Masahiro Ozaki, MD, PhD, Takeshi Fujii, MD, PhD, Soraya Nishimura, MD, PhD and the members of the 17 participating institutions for their help with data collection.
Author information
Authors and Affiliations
Contributions
SN and NN designed the research. SN analyzed the data. SN and NN wrote the paper. SN, KD, TI, HF, KN, YT, and KF performed data collection. NN, SS, YT, OT, MY, MN, MM, KW, KI, and JY supervised the study. All authors reviewed and approved the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study received ethical approval from the institutional review boards of the participating institutions. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nori, S., Nagoshi, N., Daimon, K. et al. Comparison of surgical outcomes of posterior surgeries between cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament. Spinal Cord 60, 928–933 (2022). https://doi.org/10.1038/s41393-022-00848-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00848-0