Abstract
Burning mouth syndrome (BMS) is frequently accompanied by dysgeusia and xerostomia. Clonazepam has been widely prescribed and is effective, but it is unclear whether clonazepam also affects the symptoms that accompany BMS, or whether such symptoms affect treatment outcomes. Here, we investigated the therapeutic outcomes in BMS patients with various symptoms or comorbidities. We retrospectively reviewed 41 patients diagnosed with BMS between June 2010 and June 2021 at a single institution. Patients were instructed to take clonazepam for 6 weeks. Before the first dose, burning pain intensity was measured using a visual analog scale (VAS); the unstimulated salivary flow rate (USFR), psychologic characteristics, site(s) of pain, and any taste disturbance were evaluated. Burning pain intensity was measured again after 6 weeks. Thirty-one of the 41 patents (75.7%) exhibited a depressed mood, whereas more than 67.8% of the patients exhibited anxiety. Subjective xerostomia was reported by ten patients (24.3%). The mean salivary flow rate was 0.69 mL/min and hyposalivation (an unstimulated salivary flow rate ≤ 0.5 mL/min) was apparent in ten patients (24.3%). Dysgeusia was present in 20 patients (48.7%); a bitter taste (n = 15, 75%) was reported by the largest proportion of patients. Patients who reported a bitter taste responded best in terms of burning pain reduction after 6 weeks (n = 4, 26.6%). Overall, 32 patients (78%) reported decreased oral burning pain after clonazepam (mean VAS score changed from 6.56 to 5.34) use. Patients who reported taste disturbances exhibited a significantly greater decrease in burning pain, compared with other patients (mean VAS score changed from 6.41 to 4.58) (p = 0.02). Clonazepam significantly improved burning pain in BMS patients who had taste disturbances.
Similar content being viewed by others
Introduction
Burning mouth syndrome (BMS) is a complex disorder, usually present in older women (1.5–5.5% of older women), and is characterized by pain and a burning sensation in the mouth but no visible mucosal abnormality1. The principal symptom is pain, often accompanied by oral dryness (xerostomia) and dysgeusia. Further, BMS is often associated with psychological issues (depression or anxiety)2,3, hormonal changes, local effects (lichen planus or candidiasis), and systemic dysfunctions. Although many authors have studied BMS pathogenesis, the etiology remains unclear but is probably multifactorial, involving complex interactions between local, systemic, and/or psychogenic factors. BMS has been divided into two types: spontaneous (or primary) BMS, and Secondary BMS may be caused by complex interactions between local factors (e.g., hyposalivation) or systemic/psychogenic factors, but a clear definition of secondary BMS remains elusive4,5,6. Based on recent findings, primary BMS is now believed to be a form of neuropathic pain7,8. With respect to secondary BMS, there are findings for local or systemic factors1,9,10,11. Among them, many studies have focused on psychologic issues, hyposalivation, and disturbance of the taste sensory pathway as causes of BMS1,12,13. Depressive mood (in up to 35% of patients) or anxiety trait (in up to 50% of patients) have been reported frequently in BMS patients1,13,14. In addition, approximately 25% of BMS patients exhibit xerostomia, and two-thirds of patients report taste disturbances1,11. However, the exact cause has not been proven to date1,6. Thus, diagnosis and management remain challenging, and the responses to various treatments have been inconsistent and limited. In the meantime, several studies have been conducted on the treatment of BMS; representative examples include clonazepam therapy, which has demonstrated relatively consistent therapeutic effects15,16,17,18. However, compared to the frequent accompaniment of xerostomia and taste change or psychogenic factors in BMS patients, studies on the therapeutic effect of clonazepam in the presence of these medical conditions or comorbidities have not been well studied. Here, we investigated the effects of clonazepam on xerostomia, taste disturbances, dysgeusia, and psychogenic conditions.
Methods
Patients and study design
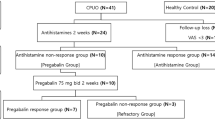
From June 2020 to June 2021, we retrospectively enrolled consecutive patients with BMS. This study included 41 patients who visited our otorhinolaryngology outpatient department for treatment of intraoral burning or dysesthesia and were then diagnosed with BMS. The inclusion criteria were established in accordance with the 2013 International Classification of Headache: intraoral burning or dysesthesia daily for > 2 h/day for > 3 months, without any clinically evident causative lesion. Pain has both of the following characteristics: (1) burning quality, (2) felt superficially in the oral mucosa19. The exclusion criteria were: current usage of benzodiazepines; allergy to benzodiazepines; and any serious disease of the central nervous system. At the first visit, an oral examination, Beck Depression Inventory (BDI), State-Trait Anxiety Inventory (STAI) questionnaire, and the comprehensive questionnaire were provided to the patients. Patients were then interviewed by one doctor and received an explanation regarding the possible etiology and management strategies for BMS. At the second visit, scheduled in the morning, the salivary flow rate was measured, the BDI and STAI was recollected, and the comprehensive questionnaire was checked by the staff to ensure the completion of any omitted sections. Then, patients were instructed to take 0.75 mg clonazepam (one half tablet) three times daily for the first 2 weeks (2.25 mg daily). If no severe drowsiness and/or dizziness developed, the dose was increased to 1.5 mg (one full tablet) three times daily for the remaining 4 weeks (4.5 mg daily). Patients were instructed to place clonazepam tablets sublingually, allow them to dissolve, and then swallow. Questionnaires were completed before treatment and after 6 weeks of treatment. All patients completed treatment without side effects.
This study was carried out in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All study procedures were approved by the Institutional Review Board of the Inje university (IRB No. 2022-08-005-001). All the participants gave their informed written consent and all methods were performed in accordance with the relevant guidelines and regulations.
Questionnaire
The questionnaire used to evaluate subjective symptoms included questions about duration of suffering, area of symptoms, type of discomfort. Burning sensation was assessed using a visual analog scale (VAS) that ranged from 0 to 10, with 0 indicating no pain and 10 indicating the worst possible pain. Additionally, the following items were explored in the questionnaire. Before treatment items were pain location; time of day when pain was most severe; pain duration; factors affecting pain (eating, type of food, talking, any drug); any change in taste (and the extent of such a change); dry mouth intensity; time since onset of burning; and whether dry mouth was worst before or after burning symptom onset. After treatment (6 weeks) items were burning sensation improvement (VAS score); region of improvement; and any change in taste.
Salivary flow rate
Saliva was collected by a standardized method as described elsewhere20,21. We measured unstimulated salivary flow rates (uSFRs) in patients at rest in a quiet room. Samples from the subjects were collected between 9:00 and 11:00 a.m., to minimize diurnal variability. All subjects abstained from smoking, eating, and drinking for 2 h prior to the measurement of salivary flow rate. The collection of unstimulated saliva started with the instruction to void the mouth of saliva by swallowing. Subsequently, saliva was allowed to ac cumulate in the floor of the mouth, without stimulation of saliva secretion by means of orofacial movements. After 5 min, participants were told to expectorate residual saliva into the container and unstimulated saliva flow rates were read. Then, patients were asked to collect saliva and spit it into a test tube for 5 min. The flow rate of whole saliva was expressed as mL/min. Hyposalivation was defined as a uSFR ≤ 0.1 mL/min22.
Psychologic status
We used the Beck Depression Inventory (BDI) and State-Trait Anxiety Inventory (STAI). Beck Depression Inventory (BDI) is a self-reported instrument that measures attitudes and symptoms characteristic of depression23. The 21-item BDI measures the extent of depression (0–9, no depression; 10–18, mild-to-moderate depression; 19–29, moderate-to-severe depression; and 30–63, severe depression). State-Trait Anxiety Inventory (STAI) actually classifies patients who have anxiety as a trait, i.e. personality characteristic while anxiety as a state reflects current anxious state of the person. STAI questionnaire is used to diagnose and measure state and trait anxiety and also to distinguish it from depressive syndromes24. The STAI includes two 20-item subscales: the State Anxiety Scale (S-Anxiety) evaluates state anxiety (i.e., how a respondent feels “right now”), whereas the Trait Anxiety Scale (T-Anxiety) evaluates longer-term “anxiety proneness”. A score of 20–37 indicates no or low anxiety, while scores of 38–44 and 45–80 indicate moderate anxiety and high anxiety, respectively.
Statistical analysis
Data were compared using the chi-square, Fisher’s exact, paired-t, or Wilcoxon-signed rank test, as appropriate. In comparing demographic and clinical data, the authors used Student’s t-test for continuous data and Chi-square tests or Fisher’s exact tests for discrete data. All calculations were performed using IBM SPSS Statistics for Windows ver. 25 (IBM Corporation, Armonk, NY, USA). The level of statistical significance was set to P < 0.05.
Results
Patient characteristics
Forty-one patients (four men and 37 women) were included. Table 1 lists the descriptive and demographic characteristics of the patients. The mean age was 66.5 ± 7.92 years; two patients (4.8%) had a history of diabetes, 23 patients (56%) had a history of hypertension, and seven patients (17%) had a history of psychologic treatment. Subjective burning severity was high (VAS score of 6–10) in 65.8% of patients; the mean VAS score was 6.56 ± 1.92. Pain was most commonly worst in the afternoon (58.5%), followed by the night (53.6%), immediately after waking (36.5%), and the morning (36.5%). All patients reported burning pain in the tongue (n = 41, 100%) followed by the buccal mucosa (n = 12, 29.2%) and palate (n = 12, 29.2%); 24 patients (58.5%) reported pain in > 2 sub-sites. The mean dry mouth VAS score was 5.48 ± 3.0 and the mean USFR was 3.45 ± 4.43 mL/min. Hyposalivation was observed in ten patients (24.3%); all also reported xerostomia. Twenty patients reported dysgeusia (24.3%) (Table 1).
Psychological status
The BDI showed that 19 patients (46.3%) had mild-to-moderate depression, six patients (14.6%) had moderate-to-severe depression, and six patients (14.6%) had severe depression. The STAI-S showed that 12 patients (29.2%) exhibited moderate state anxiety and 18 patients (43.9%) exhibited severe anxiety. The STAI-T showed that 12 patients (29.2%) exhibited moderate trait anxiety and 18 patients (43.9%) exhibited severe anxiety (Table 2).
Burning pain improvement according to sub-site
Of the 41 patients, 32 (78%) reported that clonazepam was effective (mean VAS score changed from 6.56 to 5.34). The changes in pain severity in the tongue, palate, lip, buccal area, gingiva, mouth floor, and teeth are listed in Table 3. The summed incidences exceed 100% because of duplications. Clonazepam efficacy did not significantly differ according to the number of affected sites. The most effective response was observed in the tongue (n = 32, 78%), followed by the lips (n = 4, 44.4%) and palate (n = 5, 41.6%) (Fig. 1).
Effect of therapy according to psychological status
Patients were divided into subgroups according to the BDI, STAI-T, and STAI-S scores (Table 4). Nine patients (90%) responded (mean VAS score changed from 6.32 to 5.25) in the no-depression group (n = 10), whereas 23 patients (74.2%) responded in the depressive mood group (mean VAS score changed from 7.3 to 5.6). According to STAI status, 11 of 14 patients (78.5%) with no or mild anxiety responded (mean VAS score changed from 6.33 to 5.44), whereas 21 of 27 patients (77.7%) with moderate or severe anxiety responded (mean VAS score changed from 7 to 5.14) (Fig. 3). However, the differences were not statistically significant.
Effect of therapy according to salivary flow rate
Patients were divided into subgroups according to the USFR (Table 5). In the hyposalivation group (n = 10), seven patients (70%) responded (mean VAS score changed from 7.6 to 5.9). In the normal salivation group (n = 31), 25 patients (80.6%) responded (mean VAS score changed from 6.2 to 5.16). The difference was not statistically significant.
Effects of therapy according to dysgeusia status
The effects of clonazepam on taste are listed in Table 6. Twenty patients (48.7%) reported taste disturbances, whereas five patients (25%) reported improvement after treatment (mean VAS score changed from 7.33 to 4.33) (Figs. 2, 3). The summed incidences of taste types exceed 100% because of duplication. Patients who reported bitter taste responded best (in terms of burning pain reduction) (n = 4, 26.6%), followed by patients who reported salty taste (n = 3, 21.4%) (Fig. 2). The difference was not statistically significant.
Burning pain improvement according to combinations of accompanying symptoms
We analyzed three subgroups: burning pain only (n = 9), burning pain with taste disturbance (n = 17), and burning pain with xerostomia (n = 10). Patients who reported concurrent burning pain, taste disturbance, and xerostomia (n = 5) were excluded. After treatment, all three subgroups responded, but only the second subgroup reported significant improvement in burning pain (mean VAS score changed from 6.41 to 4.58, p = 0.02) (Table 7).
Discussion
Due to its complex nature, the definition of BMS has been changed over time. A recent international study using the Delphi method found that experts are of the view that the ICD-11 term, disease description, and diagnostic criteria for BMS should be revised and the condition termed burning mouth disorder (BMD)25. BMS has been divided into two types, thus primary (there is no other disease) and secondary (possibly attributable to a local or systemic disorder)11. Primary BMS is idiopathic, in that the organic local/systemic causes cannot be identified; however, peripheral and central neuropathological pathways are potentially involved9. Secondary BMS may feature a local or systemic condition such as a mucosal disease (i.e., lichen planus or candidiasis); a hormonal disturbance; a psychosocial stressor; a vitamin or nutritional deficiency; diabetes; dry mouth; a contact allergy; a parafunctional habit; a cranial nerve injury; or a side-effect of medication, but this remains unclear1,11,26. Primary BMS treatments seek to alleviate symptoms; secondary BMS requires diagnosis and treatment of the underlying condition11. There were substantial differences in burning symptom cessation with treatment; the patients who had secondary BMS improved if the underlying clinical abnormality was treated, whereas the primary BMS group rarely reported such positive results11. Meanwhile, the main accompanying medical conditions or comorbidities of BMS are xerostomia, dysgeusia, or psychological issues such as depression and anxiety2,3. Thus, clinicians have attempted to manage BMS along with xerostomia, taste disturbance, and psychogenic issues. In general, clonazepam has been recognized as the most effective standard treatment, regardless of the accompanying symptoms or type of BMS15,16,17,18; its therapeutic effect is mediated by the inhibition of pain signaling16. Clonazepam is known as an agent for the inhibitory neurotransmitter gamma-amino butyric acid (GABA), and GABA receptors are distributed in the oral pain and taste signaling pathways12,27. Therefore, clonazepam may have the effect of reducing burning pain in the oral cavity.
Optimal administration route for clonazepam in BMS patients has been explored by many studies. A few studies on topical clonazepam demonstrated both significantly decreased pain scores and improvement of pain/burning symptoms in BMS patients28,29,30. Rodriguez et al. gave detailed data and analysis of all 66 patients, including a gradual increase in number of pills used in the placebo group compared to that of the treatment group, and affirmed the benefit of the medication29. Some other studies investigated the systemic effect of clonazepam18,31. Heckmann et al. demonstrated ingested clonazepam showed a significant decrease in pain scores, but reanalysis of the data failed to show a significant change between the initial and final stages of the therapy18. On the other hand, Grushka’s study presented a consistent pain reduction in systemic clonazepam treatment31. To see topical as well as systemic effects, Amos et al. explored combined administration methods32. This study found that intraoral clonazepam was superior to oral ingestion; pain was much more rapidly alleviated but the duration of action was reduced32. As such, there have been several studies on the effect of clonazepam according to the route of administration, but there is no consensus as to which is the optimal method, with a large-scale study yet to take place. Under this circumstance, clonazepam tablets were placed sublingually to see both local and systemic effects in this study.
BMS is often accompanied by complaints of xerostomia, as reported by 25–40% of BMS patients in recent studies1,11,33. Scala et al. reported that 46–67% of BMS patients claim to be experiencing xerostomia, regardless of whether the salivary flow rate is decreased; notably, dry mouth is often subjective, as opposed to any real decrease in salivary gland function9,26. However, the response to clonazepam treatment for BMS in those with xerostomia is not clear, as only a few studies have examined this. In one of them, Silva reported that the therapeutic response of topical urea treatment (10% of concentration, applied to the oral cavity three to four times per day for 3 months) was 60% in patients with xerostomia, which was similar to the results obtained with the control group34. In our present work, ten patients (24.3%) out of 41 reported subjective xerostomia, and all ten of these patients exhibited objective hyposalivation. Among the hyposalivation patients, seven out of ten (17%) responded to clonazepam in terms of a reduced BMS visual analogue score (VAS) score (mean VAS changed from 7.6 to 5.9); however, the response rate was lower than that (80%) of the normal group, which was not statistically significant. Previous studies have presented evidence suggesting that changes in the salivary flow rate may be associated with mucosal atrophy and/or subclinical inflammation, which may be accompanied by oral neuropathy in BMS patients34,35,36. Lauria et al. also demonstrated oral neuropathy by examining the tongue epithelium of BMS patients and found fewer small-diameter nerve fibers, which may explain the thermal hypoesthesia symptoms and change in the pain thresholds. Considering the above, it is thought that dry mouth is closely related to BMS onset. In addition, it can be hypothesized that the effect of clonazepam may be reduced as chronic neural degeneration occurs extensively as the duration of dry mouth is extended. Therefore, we think that this study can provide some insight into predicting the treatment effects of BMS patients with xerostomia.
From the aspect of psychogenic factors, several studies have suggested that psychological factors cause BMS1,11,13,14,37,38,39. Depressive mood, anxiety, somatization, and aberrant personality traits have frequently been reported in BMS patients, and much of the research has been devoted to the role of psychological factors in BMS1,13,14,38, in which psychosocial disorders with a principal focus on anxiety and/or depression were examined. Several studies reported that up to 35% of BMS patients showed depressive mood and up to 50% of patients complained of anxiety1,14,38. On the other hand, some controversy remains as to whether psychogenic pathological conditions occur primarily or are secondary to BMS. In general, psychological disorders may be associated with the modulation of pain perception, increasing nerve transmission by peripheral pain receptors, and altering of an individual’s perception of pain. Based on this, with the belief that the treatment effect for each BMS patient may differ depending on the accompanying psychogenic problem, some studies have shown that psychological problems are associated with worse prognoses9,26,40. According to Ko's study, the reduction in burning pain caused by clonazepam was smaller in the psychologic disease group than the control group (29% vs. 45%, respectively)26. Among our patients, depressive mood and anxiety trait were reported by 75.7% and 65.9%, respectively. Like other studies, our study found that the response rate with clonazepam therapy on burning pain was less in patients with psychologic problems than in those without (in depressive mood: 74.2% vs. 90%; in anxiety trait: 77.7% vs. 78.5%, respectively). However, there was no significant improvement in the BMS VAS score, regardless of the Beck Depression Inventory or State Trait Anxiety Inventory (T/S) score. The small degree of pain reduction in patients with psychogenic problems may be explained by emotional and cognitive factors for chronic pain. Forssell et al. demonstrated that BMS patients with more intensive and interfering pain report more depressive and pain-related anxiety symptoms, compared to patients with less severe pain intensity41; he explained this using a biopsychosocial model of chronic pain, showing that emotional and cognitive factors play a role in pain experience. Forssell also claimed that BMS patients with more intensive pain reported more depressive- and pain-related anxiety symptoms, and more hypervigilance to pain, compared to patients with less severe pain intensity41. Excessive attention to pain or pain hypervigilance has been reported in association with a higher pain intensity, disability, and emotional distress in different pain patient populations42. Such patients usually exaggerate their pain, thus they are likely to express a poor response to clonazepam26. Also, patients with psychogenic symptoms are likely to take psychologic medications. According to Ko's study, 23% of BMS patients had been taking psychologic medications; these patients showed significantly reduced salivary flow rates because psychologic medications may decrease salivary gland function and may result in a reduction of saliva’s protective capacity in the mouth26. As described above, the treatment effect of clonazepam may be influenced by a change in salivary components and xerostomia induced by psychologic medication.
Especially, menopause has been suggested to be a major cause of BMS. Earlier reports found that BMS affected primarily postmenopausal women9,13, and suggested that changes in the female sex hormone levels may predispose women to BMS. As both BMS and vulvodynia are far more common in postmenopausal than menstruating women, estrogen deficiency may be a shared etiological mechanism; estrogen receptors have been identified in the tongue, salivary gland, and vaginal mucosae43. Some reports stated that hormone replacement therapy in postmenopausal patients with oral discomfort was useful44; however, more research is needed.
A loss of taste inhibition by central structures that mediate oral pain has been proposed to explain BMS development13. Repetitive nociceptive inputs against a background of peripheral neuropathy eventually elicit central sensitization and other changes. Grushka proposed that BMS reflects the persistent breakdown of an intrinsic equilibrium caused by a reduction in corda tympani function; subsequently, lingual nerve inhibition and central sensitization tend to occur1. Multiple studies have revealed damage to the innervation areas of the corda tympani and glossopharyngeal nerves in BMS patients; these areas control bitter taste. Such selective inhibition may reflect the loss of central pain inhibition1,27,45. Among our patients with taste disturbances, most of them showed changes in bitter taste; these patients responded best to treatment, supporting the selective inhibition hypothesis described above. Although the role of taste in terms of oral burning syndrome is complex, clonazepam is an agonist of the inhibitory neurotransmitter GABA, which is active in the oral mucosa, mandible, palate, and salivary gland. Above all, it can be noted that it also acts on the taste pathway12. If burning causes taste disturbances that result in the loss of normal inhibition of a central structure that mediates oral pain, GABA-specific agents may relieve such pain. We found that the pain VAS scores improved significantly after treatment in patients with taste disturbances. Based on the contents described above, we assume that when taste change accompanies the treatment response, there is a better effect on pain improvement.
There have been many studies reporting the prevalence of psychogenic conditions, and taste disturbance in patients with BMS26,29. However, studies on the therapeutic effect of clonazepam in the presence of these concomitant symptoms or comorbidities have been insufficient. Thus, we assessed the therapeutic effects according to psychological, dysgeusia, and hyposalivation status. We found no correlation of psychological or hyposalivation status with the therapeutic effect of clonazepam; however, taste disturbance was associated with a higher response rate and greater improvement in relieving the burning pain. Our work had several limitations. First, it was questionnaire-based and retrospective. Second, the sample size was small. Third, it was a single-center study. Finally, we could not confirm that clonazepam had been appropriately taken; nevertheless, we found that clonazepam significantly improved the burning sensations of BMS patients with taste disturbances. Such information can be employed during patient counseling and to predict therapeutic outcomes.
Conclusion
A large proportion of BMS patients also experience xerostomia, psychogenic symptoms, and taste change. Clonazepam significantly reduced burning pain in BMS patients with taste disturbances, but no significant reduction in burning pain was found in BMS patients with xerostomia or psychogenic traits only. Such information can be used in BMS patient counseling and the prediction of therapeutic outcomes with clonazepam treatment.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Grushka, M., Epstein, J. B. & Gorsky, M. Burning mouth syndrome. Am. Fam. Phys. 65, 615–620 (2002).
Riley, J. L. 3rd., Gilbert, G. H. & Heft, M. W. Orofacial pain symptom prevalence: Selective sex differences in the elderly?. Pain 76, 97–104. https://doi.org/10.1016/s0304-3959(98)00030-x (1998).
Bergdahl, M. & Bergdahl, J. Burning mouth syndrome: Prevalence and associated factors. J. Oral Pathol. Med. 28, 350–354. https://doi.org/10.1111/j.1600-0714.1999.tb02052.x (1999).
Lamey, P. J., Freeman, R., Eddie, S. A., Pankhurst, C. & Rees, T. Vulnerability and presenting symptoms in burning mouth syndrome. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 99, 48–54. https://doi.org/10.1016/j.tripleo.2004.01.021 (2005).
Svensson, P., Bjerring, P., Arendt-Nielsen, L. & Kaaber, S. Sensory and pain thresholds to orofacial argon laser stimulation in patients with chronic burning mouth syndrome. Clin. J. Pain 9, 207–215. https://doi.org/10.1097/00002508-199309000-00009 (1993).
Yilmaz, Z. et al. Burning mouth syndrome as a trigeminal small fibre neuropathy: Increased heat and capsaicin receptor TRPV1 in nerve fibres correlates with pain score. J. Clin. Neurosci. 14, 864–871. https://doi.org/10.1016/j.jocn.2006.09.002 (2007).
Forssell, H., Jääskeläinen, S., Tenovuo, O. & Hinkka, S. Sensory dysfunction in burning mouth syndrome. Pain 99, 41–47. https://doi.org/10.1016/s0304-3959(02)00052-0 (2002).
Lauria, G. et al. Trigeminal small-fiber sensory neuropathy causes burning mouth syndrome. Pain 115, 332–337 (2005).
Scala, A., Checchi, L., Montevecchi, M., Marini, I. & Giamberardino, M. A. Update on burning mouth syndrome: Overview and patient management. Crit. Rev. Oral Biol. Med. 14, 275–291. https://doi.org/10.1177/154411130301400405 (2003).
Paterson, A. J., Lamb, A. B., Clifford, T. J. & Lamey, P. J. Burning mouth syndrome: The relationship between the HAD scale and parafunctional habits. J. Oral Pathol. Med. 24, 289–292. https://doi.org/10.1111/j.1600-0714.1995.tb01186.x (1995).
Klasser, G. D., Fischer, D. J. & Epstein, J. B. Burning mouth syndrome: Recognition, understanding, and management. Oral Maxillofac. Surg. Clin N. Am. 20, 255–271. https://doi.org/10.1016/j.coms.2007.12.012 (2008).
Bartoshuk, L. M. et al. Taste damage: Previously unsuspected consequences. Chem. Senses 30(Suppl 1), i218-219. https://doi.org/10.1093/chemse/bjh192 (2005).
Grushka, M. Clinical features of burning mouth syndrome. Oral. Surg. Oral Med. Oral Pathol. 63, 30–36. https://doi.org/10.1016/0030-4220(87)90336-7 (1987).
Galli, F., Lodi, G., Sardella, A. & Vegni, E. Role of psychological factors in burning mouth syndrome: A systematic review and meta-analysis. Cephalalgia 37, 265–277. https://doi.org/10.1177/0333102416646769 (2017).
Liu, Y. F., Kim, Y., Yoo, T., Han, P. & Inman, J. C. Burning mouth syndrome: A systematic review of treatments. Oral Dis. 24, 325–334. https://doi.org/10.1111/odi.12660 (2018).
Tan, H. L., Smith, J. G., Hoffmann, J. & Renton, T. A systematic review of treatment for patients with burning mouth syndrome. Cephalalgia 42, 128–161 (2022).
Çinar, S., Kartal, D., Pergel, T. & Borlu, M. Effectiveness and safety of clonazepam, pregabalin, and alpha lipoic acid for the treatment of burning mouth syndrome. Erciyes Med. J. 40, 35–38 (2018).
Heckmann, S. M., Kirchner, E., Grushka, M., Wichmann, M. G. & Hummel, T. A double-blind study on clonazepam in patients with burning mouth syndrome. Laryngoscope 122, 813–816. https://doi.org/10.1002/lary.22490 (2012).
The International Classification of Headache Disorders. 3rd edition (beta version). Cephalalgia 33, 629–808. https://doi.org/10.1177/0333102413485658 (2013).
Birkhed, D. & Heintze, U. Salivary secretion rate, buffer capacity, and pH. in Human Saliva: Clinical Chemistry and Microbiology. 25–74 (CRC Press, 2021).
Navasesh, M. & Christensen, C. A comparison of whole mouth resting and stimulated salivary measurements. J. Dent. Res. 61, 1158–1162 (1982).
Sreebny, L. M. Saliva in health and disease: An appraisal and update. Int. Dent. J. 50, 140–161. https://doi.org/10.1111/j.1875-595x.2000.tb00554.x (2000).
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J. & Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 4, 561–571 (1961).
Spielberger, C. D., Gonzalez-Reigosa, F., Martinez-Urrutia, A., Natalicio, L. F. & Natalicio, D. S. The state-trait anxiety inventory. Rev. Interam. Psicol./Interam. J. Psychol. 5, 133 (1971).
Chmieliauskaite, M. et al. Consensus agreement to rename burning mouth syndrome and improve International Classification of Diseases-11 disease criteria: An international Delphi study. Pain 162, 2548–2557 (2021).
Ko, J. Y., Kim, M. J., Lee, S. G. & Kho, H. S. Outcome predictors affecting the efficacy of clonazepam therapy for the management of burning mouth syndrome (BMS). Arch. Gerontol. Geriatr. 55, 755–761. https://doi.org/10.1016/j.archger.2011.10.001 (2012).
Bartoshuk, L. et al. Do taste-trigeminal interactions play a role in oral pain. Chem. Senses 21, 578 (1996).
Woda, A., Navez, M. L., Picard, P., Gremeau, C. & Pichard-Leandri, E. A possible therapeutic solution for stomatodynia (burning mouth syndrome). J. Orofac. Pain 12, 272–278 (1998).
Rodríguez de Rivera Campillo, M. E., López López, J. & ChimenosKüstner, E. Response to topical clonazepam in patients with burning mouth syndrome: A clinical study. Bull. GIRSO 49(1), 19–29 (2010).
Grémeau-Richard, C., Dubray, C., Aublet-Cuvelier, B., Ughetto, S. & Woda, A. Effect of lingual nerve block on burning mouth syndrome (stomatodynia): A randomized crossover trial. Pain® 149, 27–32 (2010).
Grushka, M., Epstein, J. & Mott, A. An open-label, dose escalation pilot study of the effect of clonazepam in burning mouth syndrome. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 86, 557–561 (1998).
Amos, K., Yeoh, S.-C. & Farah, C. S. Combined topical and systemic clonazepam therapy for the management of burning mouth syndrome: A retrospective pilot study. J. Orofac. Pain 25, 125–130 (2011).
Gorsky, M., Silverman, S. Jr. & Chinn, H. Clinical characteristics and management outcome in the burning mouth syndrome: An open study of 130 patients. Oral Surg. Oral Med. Oral Pathol. 72, 192–195 (1991).
Silva, L.A.D., Siqueira, J.T.T.D., Teixeira, M.J. & Siqueira, S.R.D.T.D. The role of xerostomia in burning mouth syndrome: A case–control study. Arq. Neuro-psiquiatr. 72, 91–98 (2014).
De Souza, F. T. et al. Burning mouth syndrome: A therapeutic approach involving mechanical salivary stimulation. Headache J. Head Face Pain 52, 1026–1034 (2012).
Spadari, F. et al. Low basal salivary flow and burning mouth syndrome: New evidence in this enigmatic pathology. J. Oral Pathol. Med. 44, 229–233 (2015).
Shibata, M. et al. Alexithymia is associated with greater risk of chronic pain and negative affect and with lower life satisfaction in a general population: The Hisayama Study. PLoS ONE 9, e90984. https://doi.org/10.1371/journal.pone.0090984 (2014).
Rojo, L., Silvestre, F. J., Bagan, J. V. & De Vicente, T. Psychiatric morbidity in burning mouth syndrome. Psychiatric interview versus depression and anxiety scales. Oral. Surg. Oral. Med. Oral Pathol. 75, 308–311. https://doi.org/10.1016/0030-4220(93)90142-q (1993).
Takenoshita, M. et al. Psychiatric diagnoses in patients with burning mouth syndrome and atypical odontalgia referred from psychiatric to dental facilities. Neuropsychiatr. Dis. Treat. 6, 699–705. https://doi.org/10.2147/ndt.S12605 (2010).
Komiyama, O. et al. Pain intensity and psychosocial characteristics of patients with burning mouth syndrome and trigeminal neuralgia. J. Oral Sci. 54, 321–327. https://doi.org/10.2334/josnusd.54.321 (2012).
Forssell, H., Teerijoki-Oksa, T., Puukka, P. & Estlander, A. M. Symptom severity in burning mouth syndrome associates with psychological factors. J. Oral Rehabil. 47, 713–719 (2020).
McCracken, L. M. “Attention” to pain in persons with chronic pain: A behavioral approach. Behav. Ther. 28, 271–284 (1997).
Leimola-Virtanen, R., Salo, T., Toikkanen, S., Pulkkinen, J. & Syrjänen, S. Expression of estrogen receptor (ER) in oral mucosa and salivary glands. Maturitas 36, 131–137 (2000).
Forabosco, A. et al. Efficacy of hormone replacement therapy in postmenopausal women with oral discomfort. Oral Surg. Oral Med. Oral Pathol. 73, 570–574 (1992).
Bartoshuk, L., Kveton, J., Yanagisawa, K. & Catalanotto, F. Taste loss and taste phantoms: A role of inhibition in the taste system. Olfaction Taste (Springer) XI, 557–560 (1994).
Acknowledgements
The author wish to acknowledge the financial support of the Catholic Medical Center Research Foundation made in the program year of 2022.
Author information
Authors and Affiliations
Contributions
S.-Y.K. designed the study. M.-R.K. collected data, H.-I.S. analyzed data and wrote the main manuscript. J.-I.B. and G.-J.K. inspected the figures and tables. D.-I.S. and S.-Y.K. reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shin, HI., Bang, JI., Kim, GJ. et al. Therapeutic effects of clonazepam in patients with burning mouth syndrome and various symptoms or psychological conditions. Sci Rep 13, 7257 (2023). https://doi.org/10.1038/s41598-023-33983-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-33983-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.