Abstract
Streptococcus suis (S. suis) infection can cause clinically severe meningitis, arthritis, pneumonia and septicemia in pigs. To date, studies on the serotypes, genotypes and antimicrobial susceptibility of S. suis in affected pigs in Taiwan are rare. In this study, we comprehensively characterized 388 S. suis isolates from 355 diseased pigs in Taiwan. The most prevalent serotypes of S. suis were serotypes 3, 7 and 8. Multilocus sequence typing (MLST) revealed 22 novel sequence types (STs) including ST1831-1852 and one new clonal complex (CC), CC1832. The identified genotypes mainly belonged to ST27, ST94 and ST1831, and CC27 and CC1832 were the main clusters. These clinical isolates were highly susceptible to ceftiofur, cefazolin, trimethoprim/sulfamethoxazole and gentamicin. The bacteria were prone to be isolated from cerebrospinal fluid and synovial fluid in suckling pigs with the majority belonging to serotype 1 and ST1. In contrast, ST28 strains that corresponded to serotypes 2 and 1/2 were more likely to exist in the lungs of growing-finishing pigs, which posted a higher risk for food safety and public health. This study provided the genetic characterization, serotyping and the most current epidemiological features of S. suis in Taiwan, which should afford a better preventative and treatment strategy of S. suis infection in pigs of different production stages.
Similar content being viewed by others

Introduction
Streptococcus suis (S. suis), a gram-positive coccus with capsule, is one of the most important pathogens in the swine industry. As an opportunistic pathogen, S. suis colonizes the upper respiratory tract (tonsil and nasal cavity) of the pigs. The infected pigs commonly manifest meningitis, arthritis, pneumonia, septicemia, and may be accompanied by acute death1. The capsular polysaccharides (CPSs) antigen of the bacteria is used as the basis of classification and 29 serotypes have been identified by using polymerase chain reaction (PCR)2. Notably, S. suis is a zoonotic bacterial pathogen that endangers the people in close contact with the infected pigs or pork products. Among the identified serotypes, serotype 2 is considered the most prevalent and virulent serotype in pigs and humans1.
Different serotypes of S. suis can be isolated in the same herd, which suggests that similar clinical symptoms may not be caused by S. suis strains with identical serotypes. In addition, the importance of specific serotypes may vary geographically. Traditional typing methods only identify the strains that are single serotype or represent specific geographic locations, which renders the findings difficult to be compared across laboratories. Therefore, in comparison with the coagglutination test, genetic typing methods that can be used to rapidly screen the bacterial isolates with lower cost are favorable for the analysis of colonial structure and genetic diversity of S. suis. The knowledge is eminent to the understanding of the epidemiology of S. suis and to identify specific strains with high pathogenicity, which could ultimately contribute to the prevention of the disease progression2. Multilocus sequence typing (MLST) has been successfully used in many studies of molecular epidemiology in bacteria. It has been used for identifying the S. suis genotypes in order to confirm the differences between the sequence types (STs) and ST clonal complexes (CCs) of S. suis strains 3.
Among the identified S. suis serotypes, serotype 1 is related to the neurological symptoms accompanied by cerebral microlesion, while serotypes 2–8 tend to cause pulmonary lesions4. In comparison to the S. suis strains that only cause pneumonia, the strains causing meningitis, septicemia and arthritis are more likely to exhibit typical clinical symptoms, which may be attributed to the pathogenesis of different serotypes5. Different strains also exert significant differences in drug resistance. The S. suis strains isolated from clinical cases of pigs are less resistant to ampicillin, ceftiofur, enrofloxacin, florfenicol, penicillin, and sulfamethoxazole-trimethoprim, whereas a high proportion of the strains is resistant to tetracycline6. However, the strains isolated from the tonsils of healthy animals or the environment of the butcheries are usually multi-drug resistant7,8. In this study, we focus on the epidemiology and laboratory findings of clinical isolates of S. suis in diseased pigs in Taiwan, investigating the association among the distribution, serotypes, genotypes and the antimicrobial drug susceptibility.
Materials and methods
Ethical statement
All the diseased pigs were sent to Animal Disease Diagnostic Center in National Chiayi University by the farm owners for necropsy. Sacrifice of the diseased pigs, tissue collection and further bacterial isolation and identification were essential in the standard process for disease diagnosis and treatment. This study project collected the deposited samples for in-depth analysis. The Institutional Animal Care and Use Committee (IACUC) confirmed that this project did not involve animal experiments and approval of animal use protocol was not required.
Isolation and identification of isolates
From March 2017 to October 2021, a total of 388 isolates from 355 diseased pigs in 289 infected herds submitted to the Animal Disease Diagnostic Center (ADDC), Department of Veterinary Medicine of National Chiayi University (Taiwan) for necropsy were collected for analysis. All of the specimens, including liver, lung and bronchus, as well as the cerebrospinal fluid and synovial fluid, were aseptically sampled during necropsy. The specimens were cultured on a 5% defibrinated sheep blood agar plate (BBL™ Blood Agar Base, Infusion Agar, BD, USA) and incubated at 37 °C for 18–24 h. The S. suis isolates were suspected when α hemolytic colonies were observed. Bacterial DNA was extracted from the S. suis-suspected colony using the Taco™ DNA/RNA Extraction Kit (Taco, Taiwan). The primer pair designed for the gdh gene of S. suis were used for PCR9. The PCR products of positive samples were sequenced in both directions by Tri-I Biotech Inc (Taipei, Taiwan) and the sequences were analyzed and compared using the basic local alignment search tool (BLAST) database on the National Center for Biotechnology Information (NCBI) website. After identification, bacteria were stored in brain heart infusion broth (BHIB) containing 10% fetal calf serum (FCS) and 20% glycerol at − 80 °C.
Serotyping by multiplex PCR and restriction fragment length polymorphism
The primer pairs designed for cps genes for multiplex PCR10 were used to categorize the S. suis isolates into group 1 (serotypes 1/2, 1, 2, 3, 7, 9, 11, 14, and 16), group 2 (serotypes 4, 5, 8, 12, 18, 19, 24, and 25), group 3 (serotypes 6, 10, 13, 15, 17, 23, and 31) and group 4 (serotypes 21, 27, 28, 29, and 30). The PCR products were sequenced, analyzed and compared with NCBI BLAST database for the confirmation of S. suis serotypes. In addition, PCR-restriction fragment length polymorphysim (RFLP) was performed for the S. suis isolates that were temporarily identified as serotypes 1, 1/2, 2 and 14. The cpsK gene of these isolates were amplified by PCR and the PCR products were cleaved by restriction endonuclease BstNI (NEB®, USA) at 60 °C for 1 h. The PCR–RFLP products were analyzed by 2% agarose gel electrophoresis11,12.
Antimicrobial susceptibility testing
According to the guidelines of the Clinical and Laboratory Standards Institute (CLSI), the antimicrobial susceptibility testing was performed for the isolates by using the micro-broth dilution method with Mueller–Hinton II broth (BBL™ Mueller–Hinton II broth, MHB, BD, USA) containing 5% fetal bovine serum (FBS)13. Sixteen antimicrobials were selected, including amoxicillin, cefazolin, ceftiofur, doxycycline, enrofloxacin, erythromycin, florfenicol, gentamicin, lincomycin, lincospectin, oxytetracycline, penicillin G, tiamulin, trimethoprim-sulfamethoxazole, tylosin, and tylvalosin. The concentration of the antimicrobial agents ranged from 0.0625 to 1024 μg/mL, and the minimum inhibitory concentration (MIC) breakpoint values for Streptococcus spp. were provided by the CLSI veterinary breakpoints13, European Committee for Antimicrobial Susceptibility Testing (EUCAST)14, Food and Drug Administration (FDA)15, and reported data16. Escherichia coli (ATCC 25,922), Pseudomonas aeruginosa (ATCC 27,853), Enterococcus faecalis (ATCC 29,212), Staphylococcus aureus (ATCC 29,213) and Streptococcus pneumoniae (ATCC 49,619) were used as quality control strains following CLSI guidance.
MLST
Seven house-keeping genes, including aroA, cpn60, dpr, gki, mutS, recA and thrA, were amplified by PCR for the nucleic acid extracted from the purified S. suis isolates according to the MLST method established by King et al. and Rehm et al.3,17. The confirmed PCR products were then sent to Tri-I Biotech, Inc. (Taiwan) for 5' to 3' and 3' to 5' sequencing using an Applied Biosystems 3730 DNA Analyzer (Applied Biosystems, USA). Subsequently, the sequencing results were uploaded to BioNumerics® version7.6.3 (Applied Maths, USA), and the obtained alleles and STs were compared with the PubMLST database. New allele sequences and STs were uploaded to PubMLST to obtain the allele profile and define the genotypes18. By using the eBURST analysis of PubMLST, the S. suis isolates with respective allele profiles were clustered according to the association of STs. When 6 of 7 alleles among the S. suis isolates were identical, these isolates were identified as the same cluster. The isolates that did not belong to any cluster were singletons3. The minimum spanning tree (MST) was calculated using BioNumerics® version 7.6 according to the unweighted pairgroup method with an arithmetic mean algorithm (UPGMA). In order to understand the general distribution of the S. suis isolates, MST was set as distance ≤ 1 for partitioning, in which the involving nodes were clustered as CCs19.
Statistical analysis
Association of isolation sites, serotypes, and antimicrobial drug resistance were analyzed by Chi-square test and Fisher’s exact test, depending on the number of samples. SPSS was used for statistical analysis and p value < 0.05 was considered to be statistically significant. If p value < 0.01, there was an extremely significant association.
Results
Bacterial isolation, identification, and serotyping
This study identified serotypes of 388 isolates collected from 355 diseased pigs (Table 1). The major serotypes were serotypes 3 (79/388, 20.4%), 7 (12.9%), 8 (11.6%), 2 and 9 (8.2%), and 1 (7.2%), followed by serotypes 4, 5, 1/2 and 21. The serotypes of 73 isolates (18.8%) could not be identified by PCR. The main isolation sites were shown in Table 1. Among the 355 diseased pigs, single serotype was isolated from 348 pigs (348/355, 98.0%), while two serotypes were isolated from seven pigs (7/355, 2.0%). Among the seven pigs, five pigs had one strain with an unknown serotype; and for the other strain, there were 3 pigs with serotypes 4, 7, and 8 individually and 2 pigs with serotype 9. The remaining two of the seven pigs were serotypes 3 and 8, and serotypes 7 and 8, respectively.
Serotype 1 was frequently isolated from brains, cerebrospinal fluid or synovial fluid at the suckling stage (p < 0.01). Serotypes 3, 7, 8, and 9 were mostly isolated from lungs or bronchial lumina at the nursing stage. In addition, serotype 2 was most likely isolated from lungs at the growing-finishing stage (p < 0.05) (Table 1).
Antimicrobial susceptibility testing
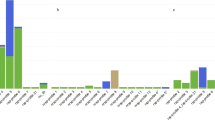
Antimicrobial susceptibility testing was performed on all 388 isolates by using the broth microdilution method according to the CLSI standards. The results showed that S. suis was highly susceptible to ceftiofur (96.4%), cefazolin (91.0%), trimethoprim /sulfamethoxazole (86.9%) and gentamicin (79.6%). The isolates showed moderate susceptibility (40–70%) to florfenicol (68.8%), amoxicillin (61.1%), enrofloxacin (60.1%), tiamulin (60.1%), penicillin G (58.0%) and doxycycline (54.9%). The susceptibility to lincospectin (33.2%), erythromycin (14.7%), tylosin (8.8%), oxytetracycline (8.0%) and lincomycin (5.2%) was lower than 40% (Table 2). Notably, most S. suis isolates showed low susceptibilities (< 10%) to tylosin, oxytetracycline and lincomycin in this study. Since there was no clinical breakpoint of S. suis for tylvalosin, the results were shown as MIC50 and MIC90, which were 256 and 1,024 μg/mL, respectively. The pattern of antibiotic resistance was analyzed according to the resistance of S. suis to different drug classes. Only 14 isolates (14/388, 3.6%) were susceptible to all classes of antimicrobial agents, 112 isolates (112/388, 28.9%) were resistant to 1–3 drug classes, 184 isolates (184/388, 47.4%) were resistant to 4–6 drug classes, 78 isolates (78/388, 20.1%) were resistant to more than seven drug classes, and 8 isolates were resistant to all classes of drugs. The most common antimicrobial resistance pattern was the resistance to tetracyclines, macrolides and lincosamides, which was found in 89.9% (349/388) of the S. suis isolates. (Fig. 1).
Heatmap showing antimicrobial susceptibility profiles of S. suis isolates. Rows represent bacterial isolates and columns represent antibiotics. The blocks indicate antibiotic susceptibility (green: susceptible, yellow: intermediate, red: resistant). The heatmap was generated by using Microsoft Excel 2010.
The relation between the antimicrobial susceptibility and the serotypes indicated that serotype 1 was highly susceptible to penicillin G, amoxicillin, cefazolin, ceftiofur, tiamulin and enrofloxacin. Serotypes 2 and 3 also had high susceptibility to penicillin G, amoxicillin, cefazolin, ceftiofur, enrofloxacin, tiamulin; and were additionally highly susceptible to gentamicin, florfenciol and trimethoprim/sulfamethoxazole. Serotype 7 had better susceptibility only to cefazolin, ceftiofur and trimethoprim/sulfamethoxazole. Serotypes 8 and 9 were highly susceptible to cefazolin, ceftiofur, gentamicin and trimethoprim/sulfamethoxazole (Table S1).
Multilocus sequence typing (MLST)
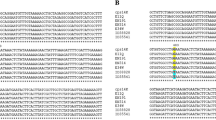
Eighty S. suis clinical isolates in numbers proportional to their serotypes were selected for the MLST, which included serotypes 1 (n = 6), 1/2 (n = 2), 2 (n = 7), 3 (n = 17), 4 (n = 3), 5 (n = 3), 7 (n = 11), 8 (n = 8), 9 (n = 7), 21 (n = 2), and 14 unidentified isolates. Seventeen new alleles were found out of 7 pairs of house-keeping genes, including 5 alleles of aroA gene, 8 alleles of cpn60 gene, 2 alleles of dpr gene, and 1 allele of gki gene and recA gene. New sequences of house-keeping gene were submitted to PubMLST for verification and the allele profiles of the new sequences were then registered to PubMLST to define the 22 new STs discovered in this study. The result of the 80 S. suis isolates showed that aroA, cpn60, gki, dpr, mutS, recA and thrA genes exerted respectively 16, 15, 13, 9, 11, 9 and 12 different alleles, forming 28 different STs. ST27 (12/80, 15.0%), ST94 (13.8%) and ST1831 (13.8%) were the major STs, followed by ST28 (10.0%), ST1832 (8.7%), ST1 (6.3%), ST1833 (3.7%), ST117 (2.5%) and ST1175 (2.5%) (Fig. 2). The 80 S. suis isolates were divided into 4 clusters and 9 singletons. As depicted in the phylogenetic dendrogram and MST, 28 STs were divided into 4 CCs. CC1 was composed of 6 S. suis isolates and 2 STs. CC27 was composed of 23 S. suis isolates and 4 STs, and ST27 was predicted as the ancestral type of this cluster. CC94 was composed of 13 S. suis isolates and 2 STs. CC1832 was composed of 29 S. suis isolates and 11 STs, and ST1832 was predicted as the ancestral type of this cluster (Figs. 2 and 3a).
Phylogenetic dendrogram constructed from the ST profiles of S. suis isolates. PG: Penicillin G, AMO: Amoxicillin, CZ: Cefazolin, CEF: Ceftiofur, GN: Gentamicin, OTC: Oxytetracycline, DO: Doxycycline, ERY: Erythromycin, TY: Tylosin, LN: Lincomycin, LS: Lincospectin, FFC: Florfenicol, TIA: Tiamulin, ENR: Enrofloxacin, SXT: Sulfamethoxazole-trimethoprim. The heatmap was generated by using Microsoft Excel 2010.
The MST graph constructed from the ST profiles of S. suis isolates (n = 80). (a) The relationship between CC and serotypes of S. suis isolates was characterized. The nodes were labeled based on the ST data, and the branch lengths were shown according to the discrepancy of allele profile between connected nodes. (b) The relationship between serotypes and STs.
Further analysis of the association between serotypes and STs among the 80 S. suis isolates revealed that most of the isolates identified as serotypes 1, 2 and 3 belonged to ST1, ST28 and ST27, respectively. Both serotypes 2 and 3 were categorized in CC27. In addition, isolates identified as serotypes 7, 8 and 9 were mostly ST1831 and ST1832, which belonged to CC1832 (Table 3 and Fig. 3b). Taken together, specific STs may be related to serotypes.
Discussion
In this study, S. suis isolates were mostly serotypes 3, 7 and 8, followed by serotypes 1, 2 and 9. In comparison with the serotype distribution in other countries, serotype 2 is the most prevalent in China, Japan, Vietnam, Thailand, Spain, Italy, France, Poland and White Russia20. The second prevalent serotype varies with countries, which are mostly serotypes 3 and 4 in Korea, serotypes 3, 1/2 and 7 in the U.S., serotype 9 in the Netherlands, and serotypes 1 and 14 in Britain21,22. Our result is close to the data reported in the U.S., in which serotypes 3 and 7 are more prevalent. In addition, our results are also in agreement with previous finding that S. suis isolated from diseased pigs was mainly composed of limited serotypes23. In general, the cps genome is the key region of gene recombination, leading to cps transformation between strains24. New cps genomes of S. suis have been found successively in recent years25, which expands the genetic diversity and reduces the quantity of unidentified isolates. In the current study, there are 18.8% of isolates that cannot be identified using cps gene by PCR and RFLP; therefore, evaluation of the virulence potential and the effects of these likely new genomes in the pathogenesis is warranted.
As shown in Table 1, serotype 1 was frequently isolated from brains, cerebrospinal fluid or synovial fluid at the suckling stage (p < 0.01). Furthermore, a very significant association between the stage of suckling pigs and the strains derived from cerebrospinal fluid and synovial fluid was found (p < 0.001, Table S2). The phenomenon that suckling pigs were more prone to brain and joint infections may be attributed to the invasive operations such as ear notching, tail cutting, teeth clipping, castration and drug injection during the lactation stage, leading to exposure of opportunistic bacteria in the environment such as S. suis. In addition, significant association between the strains isolated from respiratory tract and the stages of growing and finishing pigs was identified. S. suis that colonizes in healthy adult pigs rarely causes symptoms; however, suckling pigs may be prone to get infected from the healthy adult S. suis carriers through cross-fostering26.
The antimicrobial susceptibility testing showed that the isolates were highly susceptible to ceftiofur, cefazolin, trimethoprim/sulfamethoxazole and gentamicin, and moderately susceptible to florfenicol, amoxicillin, enrofloxacin, tiamulin, penicillin G and doxycycline. By applying the PK/PD indices that are calculated by the antimicrobial susceptibility data (Fig. S1) in combination with pharmacokinetic parameters of the drugs, effective treatment can be reasonably recommended. For instance, the suckling pigs were prone to be infected with serotype 1 which mainly causes suppurative meningitis or/and arthritis, so amoxicillin, ceftiofur and tiamulin were recommended for treatment. The pigs at the nursing stage were especially susceptible to serotypes 3, 7, 8 and 9, in which the infection in the respiratory system was relatively frequent. Considering the pharmacokinetic characteristics, cefazolin, ceftiofur, or trimethoprim/sulfamethoxazole was recommended for treatment. Among them, β-lactams are time-dependent bactericidal antimicrobial agents. In this study, the MIC90 of S. suis serotype 3, 7, 8 and 9 for ceftiofur were 0.25, 2, 0.5, and 0.25 μg/mL, respectively. After administration of ceftiofur at 5 mg/kg, AUC0-24 h was calculated as approximately 358.84 μg•h/mL27. The index of the AUC/MIC ratio was used to describe the antibacterial activity of time-dependent drugs. An AUC/MIC ratio > 125 h is generally considered good antimicrobial activity28,29. As AUC/MIC90 calculated for serotype 3, 7, 8 and 9 for ceftiofur ranged from 179.42–1435.36 h (> 125 h), indicating that this antimicrobial agent could be recommended for treating these infection of the four S. suis serotypes. Similar in rationale, the S. suis infection of pigs at the growing-finishing stage was mainly serotype 2, which was most likely to be isolated from the respiratory system but may cause systemic infection. The MIC values of penicillin G (MIC90 = 0.5 μg/mL), amoxicillin (MIC90 = 0.5 μg/mL), cefazolin (MIC90 = 0.25 μg/mL) and ceftiofur (MIC90 = 0.25 μg/mL) were obtained. When these data were combined with the pharmacokinetic information, oral administration of amoxicillin at 20 mg/kg or injection of ceftiofur at 5 mg/kg can give rise to AUC/MIC90 ≥ 125 h, and thus could be advised to treat serotype 2 infections. Notably, the parameters might be different for different drugs, organisms or bacteria30. In addition, it should be noted that healthy asymptomatic pigs are the source of human S. suis infection, in which most of the strains are serotype 2 and 90.2% of the cases are in Asia. Therefore, more attention should be paid to S. suis serotype 2 strains persisting in finishing pigs31.
Resistance of S. suis to tetracycline is prevalent worldwide. High proportion of resistance has been reported in the Americas (Canada 80–90%, Brazil 98%)32,33, Asia (China 99%, Korea 98%, Japan 78–100%, Thailand 96%, Vietnam 100%)34,35,36,37,38 and Spain (95%)39. Some of the European countries show a moderate degree of drug resistance (40.3–73.3%), and Sweden shows the lowest degree (7.7%)20. The resistance to erythromycin is higher in Taiwan (87%), South Korea (96%) %), the United States (82%) and Australia (99%), and lower in China (68%) and Japan (55–66%). Although β-lactams have been frequently used in pigs in recent years, most S suis strains are still sensitive to them and maintain a low drug resistance. The resistance rates to penicillin and ampicillin are 0–27% and 0–23%, respectively.
The proportion of S suis resistant to macrolides and lincosamides is rising globally20. According to the results of the drug resistance the results of the drug resistance, it can be seen that 89.9% of S. suis isolates were resistant to three classes of drugs including tetracyclines, macrolides and lincosamides. Li et al. have reported that S. suis resistant to chloramphenicols, macrolides, lincosamides, chloramphenicols, fluoroquinolones, aminoglycosides and hydantoins is the most common drug resistance profile in China40. In addition, S. suis strains become resistant to five classes of antimicrobials including tetracyclines, lincosamides, fluoroquinolones, sulfonamides and hydantoins in Brazil33. The percentage of multi-drug resistance (resistance to more than 3 classes of antimicrobials) of the isolates collected in this study was as high as 93.0%, and 39.4% of the isolates were resistant to more than 6 classes of antimicrobials. Our result is similar to the data from Li et al. (2012) and Soares et al. (2014), which showed the proportion of S. suis isolates resistant to more than 3 classes (98.7%, 99.6%) and 6 classes (35.9%, 85.0%) of antimicrobials in China and Brazil33,40.
Comparing the MLST result with serotypes, it was apparent that the pigs at the suckling stage were mainly infected with S. suis serotype 1, which corresponded to ST1 (n = 5) and CC1. S. suis serotype 2 mainly corresponded to ST28 (n = 6) (Table 3). Goyette-Desjardins et al. found that most of the invasive strains with high virulence belong to CC1, including ST1, ST6, ST7 and ST11, which are usually related to septicemia, meningitis and arthritis21. The current study showed that S. suis isolated from the diseased pigs with central nervous system symptoms and arthritis also belonged to CC1. In contrast, CC27 might be related more to the respiratory tract infections3. S. suis serotype 2 isolated from the growing-finishing pigs was ST28 belonging to CC27 and mostly isolated from the respiratory system. This result is similar to that of China, Japan, and the U.S., but the pathogenicity needs further investigation21,41. S. suis serotype 3 isolated from the pigs at the nursing stage was mainly ST27 of CC27 (n = 12) from respiratory systems (79.7%; 63/79). In comparison, S. suis serotype 8 was prone to be isolated from the pigs at the nursing stage (p < 0.01), and it was mostly isolated from lungs or bronchial lumina (82.2%; 37/45). These isolates were mainly ST1831 of CC1832 (n = 5). These results correspond well to previous findings that serotypes 3 and 8 are mostly restricted to lung infection42. CC94 included ST94 (n = 11) and ST1175 (n = 2), which corresponded to the unidentified S. suis isolates (n = 6), serotypes 4 (n = 3), 7 (n = 2), 3 (n=1) and 5 (n = 1) (Fig. 2). ST94 and CC94 are widely detected in the U.S., and they are the fourth most frequently seen ST and CC in North America. They are related to the pathogenic strains of serotypes 3, 4, 5, 7 and 24, but unrelated to serotypes 1, 2 and 1443. ST94 detected in Europe and Asia is mainly related to serotypes 4, 16 and unidentified strains44. Taken together, different serotypes exerting distinct infectious efficiency might determine the virulence or geographical distribution of S. suis45.
CC1832 is the largest CC in this study. It consisted of ST1831, ST1832, ST1833, ST1836, ST1837, ST1838, ST1840, ST1841 and ST1844, which corresponded mostly to serotypes 7, 8 and 9 (n = 23) and were mostly isolated from the pigs at the nursing stage (n = 23). This CC has a higher proportion of drug resistance to penicillin G, amoxicillin, cefazolin, ceftiofur, tiamulin and enrofloxacin than the other CCs. The pigs at this stage are susceptible to viral infections, such as PRRSV and PCV2, which are likely to cause opportunistic/secondary bacterial respiratory tract infections, e.g., Glaesserella parasuis, Mycoplasma hyorhinis, Bordetella bronchiseptica, and S. suis46,47. The antimicrobial agents are frequently used for pigs at this stage, leading to a relatively high drug resistance to common S. suis serotypes. The S. suis isolated from diseased pigs in this study was mostly from the respiratory system, and most of the isolates showed multi-drug resistance. Therefore, clinical use of antimicrobial agents should be selected with caution based on the characteristics of clinical isolates and the results of antimicrobial drug susceptibility.
Conclusion
S. suis is an important bacterial zoonotic pathogen with a high risk of occupational infection. In this study, aside from newly identified STs of S. suis strains, STs and serotypes were found to exert certain association, which can be further related to the feeding stages of pigs and the antimicrobial drug susceptibility. This is the first study that reports the serotype distribution, bacterial resistance and molecular epidemiological analysis of S. suis isolated from diseased pigs at different feeding stages in Taiwan. The epidemiological investigation contributes to a better understanding of the role of this bacteria and more proper treatment strategies.
Data availability
The datasets generated in the current study are available in the PubMLST, web link [https://pubmlst.org/bigsdb?db=pubmlst_ssuis_isolates&page=query&prov_field1=f_country&prov_value1=Taiwan&submit=1].
References
Gottschalk, M. & Segura, M. Streptococcosis. In: Diseases of swine. 11th ed. (Eds. Zimmerman, J. J. et al.) 934–950 (John Wiley & Sons Ltd, USA, 2019).
Hatrongjit, R., Fittipaldi, N., Gottschalk, M. & Kerdsin, A. Tools for molecular epidemiology of Streptococcus suis. Pathogens 9, 81 (2020).
King, S. J. et al. Development of a multilocus sequence typing scheme for the pig pathogen Streptococcus suis: Identification of virulent clones and potential capsular serotype exchange. J. Clin. Microbiol. 40, 3671–3680 (2002).
Reams, R. Y., Glickman, L. T., Harrington, D. D., Thacker, H. L. & Bowersock, T. L. Streptococcus suis infection in swine: A retrospective study of 256 cases Part. II. Clinical signs, gross and microscopic lesions, and coexisting microorganisms. J. Vet. Diagn. Invest. 6, 326–334 (1994).
Allgaier, A., Goethe, R., Wisselink, H. J., Smith, H. E. & Valentin-Weigand, P. Relatedness of Streptococcus suis isolates of various serotypes and clinical backgrounds as evaluated by macrorestriction analysis and expression of potential virulence traits. J. Clin. Microbiol. 39, 445–453 (2001).
Van Hout, J., Heuvelink, A. & Gonggrijp, M. Monitoring of antimicrobial susceptibility of Streptococcus suis in the Netherlands, 2013–2015. Vet. Microbiol. 194, 5–10 (2016).
Zhang, C. P. et al. Distributions of pathogenic capsular types and in vitro antimicrobial susceptibility of different serotypes of Streptococcus suis isolated from clinically healthy sows from 10 provinces in China. Zhonghua Liu Xing Bing Xue Za Zhi 30, 235–238 (2009).
Soares, T. C. et al. Streptococcus suis in employees and the environment of swine slaughterhouses in São Paulo, Brazil: Occurrence, risk factors, serotype distribution, and antimicrobial susceptibility. Can. J. Vet. Res. 79, 279–284 (2015).
Silva, L. M. et al. Virulence-associated gene profiling of Streptococcus suis isolates by PCR. Vet. Microbiol. 115, 117–127 (2006).
Kerdsin, A. et al. Streptococcus suis serotyping by a new multiplex PCR. J. Med. Microbiol. 63, 824–830 (2014).
Athey, T. B. et al. Determining Streptococcus suis serotype from short-read whole-genome sequencing data. BMC Microbiol. 16, 162 (2016).
Matiasovic, J. et al. Resolution of Streptococcus suis serotypes 1/2 versus 2 and 1 versus 14 by PCR-restriction fragment length polymorphism method. J. Clin. Microbiol. 58, e00480-e520 (2020).
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals, 5th ed. CLSI Supplement VET01S. Clinical and Laboratory Standards Institute: Wayne, PA, USA (2020).
European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters, v10. EUCAST: Basel, Switzerland. http://www.eucast.org (2020).
Food and Drug Administration. Antibacterial susceptibility test interpretive criteria. FDA: Silver Spring, MD, USA. http://www.fda.gov/drugs/development-resources/antibacterial -susceptibility-test-interpretive-criteria (2019).
Lunha, K. et al. Antimicrobial susceptibility of Streptococcus suis isolated from diseased pigs in Thailand, 2018–2020. Antibiotics (Basel) 11, 410 (2022).
Rehm, T. et al. Amplified fragment length polymorphism of Streptococcus suis strains correlates with their profile of virulence-associated genes and clinical background. J. Med. Microbiol. 56, 102–109 (2007).
Jolley, K. A., Bray, J. E. & Maiden, M. C. J. Open-access bacterial population genomics: BIGSdb software, the PubMLST. org website and their applications. Wellcome Open Res. 3, 124 (2018).
Feil, E. J., Li, B. C., Aanensen, D. M., Hanage, W. P. & Spratt, B. G. eBURST: Inferring patterns of evolutionary descent among clusters of related bacterial genotypes from multilocus sequence typing data. J. Bacteriol. 186, 1518–1530 (2004).
Segura, M. et al. Update on Streptococcus suis research and prevention in the era of antimicrobial restriction: 4th international workshop on S suis. Pathogens 9, 374 (2020).
Goyette-Desjardins, G., Auger, J. P., Xu, J., Segura, M. & Gottschalk, M. Streptococcus suis, an important pig pathogen and emerging zoonotic agent-an update on the worldwide distribution based on serotyping and sequence typing. Emerg. Microbes. Infect. 3, e45 (2014).
Bojarska, A. et al. Diversity of serotypes and new cps loci variants among Streptococcus suis isolates from pigs in Poland and Belarus. Vet. Microbiol. 240, 108534 (2020).
Okura, M. et al. Current taxonomical situation of Streptococcus suis. Pathogens 5, 45 (2016).
Mostowy, R. J. et al. Pneumococcal capsule synthesis locus cps as evolutionary hotspot with potential to generate novel serotypes by recombination. Mol. Biol. Evol. 34, 2537–2554 (2017).
Huang, J. et al. Identification of six novel capsular polysaccharide loci (NCL) from Streptococcus suis multidrug resistant non-typeable strains and the pathogenic characteristic of strains carrying new NCLs. Transbound. Emerg. Dis. 66, 995–1003 (2019).
Obradovic, M. R., Segura, M., Segalés, J. & Gottschalk, M. Review of the speculative role of co-infections in Streptococcus suis-associated diseases in pigs. Vet. Res. 52, 49 (2021).
Sun, D. et al. Optimal regimens based on PK/PD cutoff evaluation of ceftiofur against Actinobacillus pleuropneumoniae in swine. BMC Vet. Res. 16, 366 (2020).
Meinen, J. B., Mcclure, J. T. & Rosin, E. Pharmacokinetics of enrofloxacin in clinically Normal dogs and mice and drug pharmacodynamics in neutropenic mice with Escherichia-Coli and staphylococcal infections. Am. J. Vet. Res. 56, 1219–1224 (1995).
Toutain, P. L., Del Castillo, J. R. E. & Bousquet-Melou, A. The pharmacokinetic- pharmacodynamic approach to a rational dosage regimen for antibiotics. Res. Vet. Sci. 73, 105–114 (2002).
Andes, D. & Craig, W. A. Animal model pharmacokinetics and pharmacodynamics: A critical review. Int. J. Antimicrob. Agents 19, 261–268 (2002).
Dutkiewicz, J. et al. Streptococcus suis: A re-emerging pathogen associated with occupational exposure to pigs or pork products. Part I—epidemiology. Ann. Agric. Environ. Med. 24, 683–695 (2017).
Glass-Kaastra, S. K. et al. Surveillance of antimicrobial resistance in clinical isolates of Pasteurella multocida and Streptococcus suis from Ontario swine. Can. J. Vet. Res. 78, 241–249 (2014).
Soares, T. C. et al. Antimicrobial susceptibility of Streptococcus suis isolated from clinically healthy swine in Brazil. Can. J. Vet. Res. 78, 145–149 (2014).
Chen, L. et al. Antimicrobial susceptibility, tetracycline and erythromycin resistance genes, and multilocus sequence typing of Streptococcus suis isolates from diseased pigs in China. J. Vet. Med. Sci. 75, 583–587 (2013).
Ichikawa, T., Oshima, M., Yamagishi, J., Muramatsu, C. & Asai, T. Changes in antimicrobial resistance phenotypes and genotypes in Streptococcus suis strains isolated from pigs in the Tokai area of Japan. J. Vet. Med. Sci. 82, 9–13 (2020).
Lakkitjaroen, N. et al. Prevalence and antimicrobial susceptibility of Streptococcus suis isolated from slaughter pigs in northern Thailand. Kasetsart J. Nat. Sci. 45, 78–83 (2011).
Ngo, T. H. et al. Slaughterhouse pigs are a major reservoir of Streptococcus suis serotype 2 capable of causing human infection in southern Vietnam. PLoS ONE 6, e17943 (2011).
Oh, S. I. et al. Capsular serotypes, virulence-associated genes and antimicrobial susceptibility of Streptococcus suis isolates from pigs in Korea. J. Vet. Med. Sci. 79, 780–787 (2017).
Vela, A. I. et al. Antimicrobial susceptibility of clinical strains of Streptococcus suis isolated from pigs in Spain. Vet. Microbiol. 105, 143–147 (2005).
Li, L. L. et al. Antimicrobial resistance, serotypes, and virulence factors of Streptococcus suis isolates from diseased pigs. Foodborne Pathog. Dis. 9, 583–588 (2012).
Huang, W. et al. Genomic epidemiological investigation of a Streptococcus suis outbreak in Guangxi, China, 2016. Infect. Genet. Evol. 68, 249–252 (2019).
Wei, Z. et al. Characterization of Streptococcus suis isolates from the diseased pigs in China between 2003 and 2007. Vet. Microbiol. 137, 196–201 (2009).
Lacouture, S., Olivera, Y. R., Mariela, S. & Gottschalk, M. Distribution and characterization of Streptococcus suis serotypes isolated from January 2015 to June 2020 from diseased pigs in Québec Canada. Can. J. Vet. Res. 86, 78–82 (2022).
Estrada, A. A. et al. Serotype and genotype (multilocus sequence type) of Streptococcus suis isolates from the United States serve as predictors of pathotype. J. Clin. Microbiol. 57, e00377-e419 (2019).
Berthelot-Hérault, F., Morvan, H., Kéribin, A. M., Gottschalk, M. & Kobisch, M. Production of muraminidase-released protein (MRP), extracellular factor (EF) and suilysin by field isolates of Streptococcus suis capsular types 2, 1/2, 9, 7 and 3 isolated from swine in France. Vet. Res. 31, 473–479 (2000).
Ouyang, T., Zhang, X., Liu, X. & Ren, L. Co-infection of swine with porcine circovirus type 2 and other swine viruses. Viruses 11, 185 (2019).
Saade, G. et al. Coinfections and their molecular consequences in the porcine respiratory tract. Vet. Res. 51, 80 (2020).
Author information
Authors and Affiliations
Contributions
H.C.K. designed research; S.H.C. collected samples; C.F.W., S.H.C., H.C.K. performed research, analyzed data and wrote the draft manuscript. C.F.W., C.C.C, C.M.W., S.W.H. and H.C.K. edited and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, CF., Chen, SH., Chou, CC. et al. Serotype and multilocus sequence typing of Streptococcus suis from diseased pigs in Taiwan. Sci Rep 13, 8263 (2023). https://doi.org/10.1038/s41598-023-33778-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-33778-9
This article is cited by
-
Characterization of pig tonsils as niches for the generation of Streptococcus suis diversity
Veterinary Research (2024)
-
Epidemiology and genetic diversity of Streptococcus suis in smallhold swine farms in the Philippines
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.