Abstract
The older population has an increasing burden of non-communicable disease, which can potentially be associated with physical and mental disabilities and shorten life spam. To investigate whether depression, loss of functionality for activities of daily living, and lower social support are associated with all-cause mortality in the older population of Italian descent. This population-based cohort study was conducted in Veranópolis, a country city from southern Brazil, among individuals aged 60 years or older. Interviews were performed in a systematic random sampling regarding demographic, socioeconomic, and psychosocial variables, in addition to depression (Geriatric Depression Scale), activities of daily living (Barthel Index), and social support (Medical Outcomes Study scale). In the follow-up, participants were reinterviewed or, in case of death, the next of kin, and hospital records were revised. Hierarchical analysis was used to determine characteristics independently associated with all-cause mortality, using Poisson regression with robust variance, expressed as relative risk with 95% confidence intervals (RR; 95%CI). A total of 997 participants were enrolled and 882 participants completed the study, after 7.24 ± 2.41 years; with 581 remaining alive. The mean age was 73.12 ± 8.03 years, 4% were nonagenarians or centennials, and 62% were women. Symptoms of depression (RR: 1.04; 1.01–1.06) and functional dependence for ADL (RR: 1.00; 0.99–1.00) were associated with all-cause mortality, even after controlling for confounding factors. Lower social support was not associated with mortality (RR: 1.00; 0.99–1.01). Depression and functional dependence are independent predictors of all-cause mortality in the older population from Italian descent.
Similar content being viewed by others
Introduction
Cardiovascular disease is the main cause of disability and mortality worldwide1, leading to early loss of years of productive life2. Persistent exposures to elevated blood pressure3, hyperglycemia4, and smoking5 increase the risk of death in older adults, while aerobic activity, strength training, or combined exercise seem to reduce this risk6. Whether alcoholic beverage intake is a risk factor7 or affords cardiovascular protection8,9 remains controversial.
Veranópolis, a town located in the highlands of southern Brazil, has become known for the longevity of its population, which has the highest life expectancy in the country. Cohort studies of very old10 and older11 individuals have confirmed associations of cardiovascular risk factors (such as high blood pressure, extremes of sleep duration, and dyslipidemia) with mortality. Studies have also shown that reduced feelings of well-being, lack of purpose in life, hopelessness, and loneliness also increased the risk of mortality12,13. The older population, mostly of Italian descent, seems to share a social cohesion, enhancing the feeling of belonging to the community.
Multimorbidity is highly prevalent in older adults14, and those with effective social interactions seem to be more likely to survive than those with absent or disrupted relationships. The lack of social connections and isolation seem to have an effect comparable to that of traditional risk factors15, which may be even more relevant in older individuals due to the concomitant occurrence of frailty, functional dependence, and depression16,17. Although the mechanisms are not fully established, the effect of these risk factors when unmitigated by full social connections and socioeconomic status compatible with one’s needs should be investigated.
This city was founded by Italian immigrants who came to Brazil during the immigration period. Part of the population are bilingual, speaks Portuguese and an Italian dialect, and maintains traditions of closeness and friendly relationships. Given the dearth of studies on this topic conducted in the older population from middle-income countries, this cohort study was designed to investigate independent associations of depression, functionality for activities of daily living, and lower social support with all-cause mortality in the population into their sixties and beyond.
Methods
Study design
This population-based cohort study included individuals aged 60 years or older living in the town of Veranópolis, southern Brazil, certified as one of the Age-friendly cities and communities by the World Health Organization. Participants were selected through a systematic random sampling of all individuals aged 60 years or older residing in the municipality. The only exclusion criterion would be not residing in the municipality.
During 2009, enrolled participants were interviewed regarding characteristics potentially associated with the decision to have the influenza vaccine, as well as past medical history and demographic, socioeconomic, and psychosocial variables. Participants were selected by systematic random sampling from a record of all individuals aged 60 years or older living in the municipality. During the follow-up visit, participants were assessed between June 2017 and March 2018. Throughout this period, the investigators sought to locate all participants interviewed at baseline through telephone calls, home visits, contacting neighbors or the next of kin informed in the application, and making on-site visits to any secondary or additional addresses which participants might have provided in the hospital record.
Participants were scheduled to undergo an interview, as well as measurements and specimen collection for laboratory tests, at the study headquarters or at home. The next of kin of participants who had died between baseline and follow-up were contacted to obtain information through a verbal autopsy. All experiments were performed in accordance with relevant guidelines and regulations, and that the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines were followed. This study was approved by the Ethics Committee of Hospital de Clinicas de Porto Alegre (GPPG number: 170241), which is accredited by the Office of Human Research Protections as an Institutional Review Board, and registered at Plataforma Brasil. Written informed consent was provided from all participants or their next of kin.
Studied variables
Vital status (dead or alive), determined through death certificates, was the primary clinical outcome. A verbal autopsy with the next of kin, review of hospital records, and interviews with attending physicians were used to outline the events surrounding death. All deaths that occurred between January 1, 2009 and March 31, 2018 were identified.
The exposures of interest included:
-
Depression, investigated through the Geriatric Depression Scale (GDS), which consists of 15 items to measure how the respondent has been feeling18. This quantitative scale, used for screening, has been validated in Brazil; scores ≥ 5 are indicative of moderate depression, 1–4 of mild depression, and < 5 of no depression19.
-
Functionality for basic activities of daily living, determined by the 10 items of the Barthel Index, assessed self-care (feeding, transferring from chair to bed, grooming, toilet use, bathing, dressing, and sphincter control) and mobility (climbing/descending stairs and walking)20. This quantitative scale, ranging from zero to 100, was administered and categorized to identify individuals as totally independent (100 points) or dependent (< 100) for least one ADL.
-
Social support, investigated using the Medical Outcomes Study (MOS) scale21, conceived to measure material social support, involving the provision of practical resources and material help; affective support, relating to demonstrations of love and affection; positive social interactions, i.e., having people to relax with or have fun with; emotional support, encompassing the social network’s ability to satisfy individual needs in relation to emotional problems; and, finally, an information dimension, which measures access to people on whom one can rely for advice, information, or guidance22. Answers were categorized as: never, rarely, sometimes, nearly always, and always, and added together to score from 19 to 95. The 80th percentile (scores > 88) was also used to identify lower social support.
Variables considered potential risk or protection factors were: sex, age (categorized as 60–69, 70–79, 80–102 years), education (years at school; categorized as 0–4, 5–8, and ≥ 9), having a partner (or spouse), retirement, self-reported regular physical activity, smoking status (categorized as never smoker, former smoker, or current smoker), alcohol intake (categorized as abusive consumption if daily intake ≥ 2 units for men or ≥ 1 unit for women, of beer (can), wine (glass), or spirits (dose); social consumption for a daily intake of < 2 or < 1 unit, respectively; abstemious otherwise), participation in group activities (religious group, community association, cultural group, political party, regular meeting with friends, sports team; categorized as present for those who were involved in at least one group), and previous diagnosis of heart disease or cancer.
The research team was composed of health professionals who were trained and supervised during the performance of standardized interviews, using a previously tested questionnaire10, and when administering the study scales.
Sample size calculation and statistical analysis
Sample size calculation was based on the association between Barthel Index and mortality, assuming that functionally dependent older individuals would have a 50% risk of dying during the follow-up period versus 30% in those who were independent, considering an exposed–to-unexposed ratio of 12:9 and a 95% confidence level (95%CI). A sample of 800 participants would be needed to ensure statistical power > 95% (EPIDAT; PAHO, version 3.1).
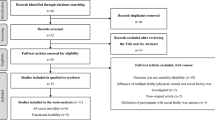
Analysis of associations, with calculation of relative risk (RR) and respective 95% confidence intervals, was performed through Poisson regression with robust variance. A hierarchical analysis23 was used to plan and conduct multivariate analysis, including the variables of interest (depression, functionality for ADL, and social support) and potential confounding factors (age, sex, education, marital status, retirement, regular physical activity, smoking, harmful alcohol use, participation in group activities, physician diagnosis of hypertension, diabetes mellitus, heart disease, and history of cancer). Figure 1 illustrates these sets of variables, starting from those temporally most distal to mortality—demographic (sex and age) and socioeconomic (education, marital status, and retirement)23. In an attempt to obtain a parsimonious model, a univariate analysis of risk factors potentially associated with mortality was carried out in each set, and the most strongly associated variables (P < 0.20) selected. Chi-square test of independence was used to determine if there was a statistically significant association between nominal variables and mortality. Risk factors that remained associated were carried forward into the multivariate analysis as confounding factors for the set itself and of subsequent sets. Depression, functional independence for ADL, and social support were analyzed adjusting for confounding factors within the set at the same level and at hierarchically superior ones23. The selected variables were categorized (to greater applicability of the results) and to allow better model fit on multivariate analysis. All statistical analyses were carried out in IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY). Spearman’s correlation was used to test for correlation between the variables of interest on their original scales.
Results
Among participants potentially eligible at baseline, 10.48% were not found, 1.06% refused to participate, and 0.70% died before they could be interviewed, resulting in 997 participants enrolled (Fig. 2). After 7.24 ± 2.41 years of follow-up, 882 (88.46%) were interviewed and 115 (11.53%) had been lost: 67 were not found, 36 refused to participate, and 12 moved out of town.
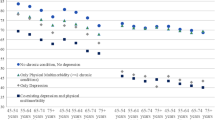
Table 1 shows that participants were aged 73.1 ± 8.0 years on average. The majority were women, with low educational attainment, retired, and living with a partner. Most participants were non-smokers; more than half consumed alcoholic beverages and engaged in physical activity on a daily basis. Regarding previous diagnoses, 56.46% reported hypertension, 14.29% diabetes mellitus, 32.43% heart disease, and 5.82% cancer. Approximately one-third had depression, 83.90% were independent for ADLs and most had some type of social support.
During the follow-up period, 301 (34.13%) participants died, mostly women, with low education level, at a mean age of 78.72 ± 8.14 years. There was an inverse association between educational attainment and mortality, as well as lower risk among individuals who were not retired and lived with a partner (Table 1). Considering lifestyle characteristics, individuals who participated in one or more group activities had lower risk of dying, but reduced social support was not associated with mortality. An increased risk of death was observed among smokers, those who self-reported as abstainers, and those with hypertension, heart disease, or a history of cancer. Depression, present in about one-third of the sample, was directly related to the risk of death; increasing depression severity was associated with higher mortality. A supplementary Table presents the studied sample and participants loose to follow-up.
As shown in Table 2, sex and age were strongly associated with mortality, even after controlling for biological confounding factors. Among socioeconomic characteristics, not having a partner remained as an independent risk factor, but educational attainment and retirement lost statistical significance after controlling for biological and socioeconomic variables. Among lifestyle characteristics, smoking remained associated with mortality even after taking into account traditional risk factors, while consumption of alcoholic beverages and participation in group activities were protective factors. Previous diagnosis of heart disease or cancer was an independent risk factor for mortality, even after controlling for multiple traditional risk factors. On univariate analysis, the risk of mortality increased 8% per additional point on the GDS score, decreasing to 4% in the model adjusted for biological, socioeconomic, lifestyle factors, comorbidity, and loss of functionality. Lower scores on the Barthel Index suggested greater risk of dying, and controlling for other risk factors did not substantially reduce the risk. Lower social support was not associated with mortality.
Table 3 shows correlations between the GDS, the Barthel Index, and the social support scale. All dimensions of social support were found to be negatively correlated with the depression scale. This suggests that the more material, affective, emotional, informational, and social interaction support that older people receive, the lower their score on the GDS. However, there was no statistically significant correlation between the Barthel Index and social support.
Discussion
In this cohort study representative of a population aged 60–102 years, mostly Italian descent, symptoms of depression and loss of functionality for ADL were associated with higher mortality, even after controlling for the effect of traditional risk and protective factors. Older adults with symptoms of depression are subject to decreased implementation of self-care, adherence to medications, systematic medical monitoring, and healthy lifestyle habits, as well as less likely to adopt protective behaviors (such as participation in group activities, moderate intake of alcoholic beverages, and regular physical activity), but to increased time spent sitting or lying down. All-cause mortality can be explained by a set of risk exposures8, insufficiently mitigated by protective factors. However, the independence of the association between mortality and symptoms of depression indicates an increase in overall risk that is not completely mediated by these traditional risk factors or by loss of functionality for ADL.
This finding is corroborated by studies conducted in multiple countries which included broad control of confounding factors24, including one of individuals aged 35 to 70 years, a U.S. study that investigated individuals aged 45 years or older25, and a study conducted in Eastern Europe of individuals aged 45–69 years26. However, in addition to not having been conducted in middle-income countries, these studies included participants with a wider age range, unlike the present study, which enrolled exclusively 60 years-old or older adults, including centenarians. Characteristics associated with loneliness were also related to depression, such as older adults, males, and among those lacking a partner. Although some studies have found controversial results regarding gender and age, the analysis restricted to the elderly was able to detect a higher prevalence of depression in the elderly of a Spanish population27.
The present study also found a low prevalence of dependence for ADL at baseline. Nevertheless, about half of those with functional dependence died during the follow-up. Participants who experience deterioration of physical capacity inevitably need help from a caregiver, greater number of visits to health services, burdening individuals, families, and society. Use of the Barthel Index offers the advantage of allowing early detection of different domains of disability and its progression, in addition to predicting mortality28.
In this study, lower social support was not associated with mortality, in contrast to a previous investigation29. Veranópolis, a town built and largely populated by descendants of Italian immigrants, has several peculiar social characteristics: older adults live predominantly with relatives and interact closely with family, neighbors, and friends. These population-wide characteristics ensure that support networks extend well beyond the nuclear family, precluding the loneliness30. People who live with a partner, relatives, friends, or in communities may have their care needs better met, as may those with a broad-ranging social network. The observed negative correlations between the depression scale and various dimensions of social support, such as material, affective, emotional, information, and social interaction, can potentially be explained by these characteristics. This result has been previously documented31.
Some limitations deserve to be considered in the interpretation of the results. The study being conducted in a country city circumscribed the presence of a large population of Italian immigrants, like the Italians born in Brazil, which favored to detect the maintenance of proximity and healthier behaviors32 than those in the country of adoption. These characteristics were associated with the outcome of interest. Our study provided a glimpse in the centenarians, as this city has one of the highest life expectancy rates in the country. However, as they were outnumbered, limited statistical power prevented comparisons with other population-based studies33.
In conclusion, in the population of older adults observed in this cohort, symptoms of depression and loss of functionality for ADL are independent predictors of higher mortality. In addition to traditional risk factors, these aspects should be considered as part of the assessment and promotion of health in the older population.
Data availability
The data that support the findings of this study are available upon reasonable request from the corresponding author [SCF].
References
Joseph, P. et al. Reducing the global burden of cardiovascular disease, part 1: The epidemiology and risk factors. Circ. Res. 12, 677–694 (2017).
Roth, G. A. et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J. Am. Coll. Cardiol. 70, 1–25 (2017).
Lewington, S. et al. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913 (2002).
Preis, S. R. et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation 119, 1728–1735 (2009).
Taghizadeh, N., Vonk, J. M. & Boezen, H. M. Lifetime smoking history and cause-specific mortality in a cohort study with 43 years of follow-up. PLoS ONE 11, 0153310 (2016).
Zhao, M., Veeranki, S. P., Magnussen, C. G. & Xi, B. Recommended physical activity and all cause and cause specific mortality in US adults: Prospective cohort study. BMJ 370, m2031 (2020).
Fuchs, F. D. & Chambless, L. E. Is the cardioprotective effect of alcohol real?. Alcohol 41, 399–402 (2007).
Ding, D., Rogers, K., Van der Ploeg, H., Stamatakis, E. & Bauman, A. E. Traditional and emerging lifestyle risk behaviors and all-cause mortality in middle-aged and older adults: Evidence from a large population-based australian cohort. PLoS Med. 12, e1001917 (2015).
Da Luz, P. L. et al. Red wine consumption, coronary calcification, and long-term clinical evolution. Braz J Med Biol Res. 51, e7703 (2018).
Werle, M. H. et al. Risk factors for cardiovascular disease in the very elderly: Results of a cohort study in a city in southern Brazil. Eur. J. Cardiovasc. Prev. Rehabil. 18, 369–377 (2011).
Da Silva, A. A. et al. Sleep duration and mortality in the elderly: A systematic review with meta-analysis. BMJ Open 6, e008119 (2016).
Tomioka, K., Kurumatani, N. & Hosoi, H. Relationship of having hobbies and a purpose in life with mortality, activities of daily living, and instrumental activities of daily living among community-dwelling elderly adults. J. Epidemiol. 26, 361–370 (2016).
Rizzuto, D. & Fratiglioni, L. Lifestyle factors related to mortality and survival: A mini-review. Gerontology 60, 327–335 (2014).
Zhao, Y. et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: An analysis of population-based panel data. Lancet Glob. Health 8, e840-849 (2020).
Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T. & Stephenson, D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect. Psychol. Sci. 10, 227–237 (2015).
Brandão, D. J., Fontenelle, L. F., Da Silva, S. A., Menezes, P. R. & Pastor-Valero, M. Depression and excess mortality in the elderly living in low- and middle-income countries: Systematic review and meta-analysis. Int. J. Geriatr. Psychiatry 34, 22–30 (2019).
Zhao, Y. W. et al. The effect of multimorbidity on functional limitations and depression amongst middle-aged and older population in China: A nationwide longitudinal study. Age Ageing. 50, 190–197 (2021).
Yesavage, J. A. et al. Development and validation of a geriatric screening scale. J. Psychiatry Res. 17, 37–49 (1983).
Almeida, O. P. & Almeida, S. A. Reliability of the Brazilian version of the abbreviated form of Geriatric Depression Scale (GDS) short form. Arq. Neuropsiquiatr. 57, 421–426 (1999).
Mahoney, F. I. & Barthel, D. W. Functional evaluation: The Barthel index. Md. State Med. J. 14, 61–65 (1965).
Sherbourne, C. D. & Stewart, A. L. The MOS social support survey. Soc. Sci. Med. 32, 705–714 (1991).
Zanini, D. S. & Peixoto, E. M. Social Support Scale (MOS-SSS): Analysis of the psychometric properties via item response theory. Paidéia 26, 359–368 (2016).
Victora, C. G., Huttly, S. R., Fuchs, S. C. & Olinto, M. T. The role of conceptual frameworks in epidemiological analysis: A hierarchical approach. Int. J. Epidemiol. 26, 224–227 (1997).
Rajan, S. et al. Prospective Urban Rural Epidemiology (PURE) Study Investigators. Association of symptoms of depression with cardiovascular disease and mortality in low-, middle, and high-income countries. JAMA Psychiat. 77, 1052–1063 (2020).
Moise, N. et al. Observational study of the differential impact of time-varying depressive symptoms on all-cause and cause-specific mortality by health status in community-dwelling adults: The REGARDS study. BMJ Open 8, e017385 (2018).
Kozela, M. et al. The association of depressive symptoms with cardiovascular and all-cause mortality in Central and Eastern Europe: Prospective results of the HAPIEE study. Eur. J. Prev. Cardiol. 23, 1839–1847 (2016).
Delgado-Losada, M. L., Bouhaben, J., Arroyo-Pardo, E., Aparicio, A. & López-Parra, A. M. Loneliness, depression, and genetics in the elderly: Prognostic factors of a worse health condition?. Int. J. Environ. Res. Public Health. 19, 15456 (2022).
Wu, L. W. et al. All-cause mortality risk in elderly individuals with disabilities: A retrospective observational study. BMJ Open 6, e011164 (2016).
Hill, T. D., Uchino, B. N., Eckhardt, J. L. & Angel, J. L. Perceived social support trajectories and the all-cause mortality risk of older mexican american women and men. Res Aging. 38, 374–398 (2016).
Hammoud, R. et al. Lonely in a crowd: Investigating the association between overcrowding and loneliness using smartphone technologies. Sci. Rep. 11, 24134 (2021).
Paganini-Hill, A., Kawas, C. H. & Corrada, M. M. Positive mental attitude associated with lower 35-year mortality: The leisure world cohort study. J Aging Res. 2018, 2126368 (2018).
Campostrini, S. et al. Migrant health in Italy: A better health status difficult to maintain-country of origin and assimilation effects studied from the Italian risk factor surveillance data. Popul. Health Metr. 17, 14 (2019).
Leitch, S., Glue, P., Gray, A. R., Greco, P. & Barak, Y. Comparison of psychosocial variables associated with loneliness in centenarian vs elderly populations in New Zealand. JAMA Netw Open. 1, e183880 (2018).
Acknowledgements
We would like to thank to the older population of Veranópolis, who have been cooperative and enthusiastic with research projects; to the research team who undertook the data collection, and to the administrative staff of the International Longevity Centre (ILC-BR).
Funding
This study was partially supported by the National Council for Scientific and Technological Development (CNPq, no. 309023/2015-7) and the Fundo de Incentivo à Pesquisa do Hospital de Clinicas de Porto Alegre (FIPE-GPPG number: 170241) supported with a publication grant.
Author information
Authors and Affiliations
Contributions
E. P. and S. C. F. contributed to the conception. N. M. B , F. C. F. and E. H. M. contributed to the design. E. P. and N. M. B. contributed to the acquisition of the data. E. P. and S. C. F. analyzed and interpreted the data. E. P., F. C. F., and E. H. M. drafted the manuscript. All authors critically revised the manuscript, provided input, gave final approval, and agreed to be accountable for all aspects of work, ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pessin, E., Fuchs, S.C., Bruscato, N.M. et al. Mortality was predicted by depression and functional dependence in a cohort of elderly adults of Italian descent from southern Brazil. Sci Rep 13, 5448 (2023). https://doi.org/10.1038/s41598-023-32617-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-32617-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.