Abstract
The co-occurrence of mental and physical chronic conditions is a growing concern and a largely unaddressed challenge in low-and-middle-income countries. This study aimed to investigate the independent and multiplicative effects of depression and physical chronic conditions on health-related quality of life (HRQoL) in China, and how it varies by age and gender. We used two waves of the China Health and Retirement Longitudinal Study (2011, 2015), including 9227 participants aged ≥ 45 years, 12 physical chronic conditions and depressive symptoms. We used mixed-effects linear regression to assess the effects of depression and physical multimorbidity on HRQoL, which was measured using a proxy measure of Physical Component Scores (PCS) and Mental Component Scores (MCS) of the matched SF-36 measure. We found that each increased number of physical chronic conditions, and the presence of depression were independently associated with lower proxy PCS and MCS scores. There were multiplicative effects of depression and physical chronic conditions on PCS (− 0.83 points, 95% CI − 1.06, − 0.60) and MCS scores (− 0.50 points, 95% CI − 0.73, − 0.27). The results showed that HRQoL decreased markedly with multimorbidity and was exacerbated by the presence of co-existing physical and mental chronic conditions.
Similar content being viewed by others
Introduction
The prevalence of multimorbidity, defined as having two or more co-existing mental or physical chronic conditions, is rising rapidly in low-and middle-income countries (LMICs)1,2. A recent study in China found that the prevalence of physical multimorbidity was 62% among middle-aged and elderly in China in 20153. Findings from the China Mental Health Survey suggested that the prevalence of mental disorders was 9.3% in 2013 among Chinese adults, and most mental disorders have become more common over the past 30 years4. The rising prevalence of physical and mental chronic conditions is expected to pose significant challenges to the health system in China3,5.
Multimorbidity can involve different patterns of physical and mental chronic conditions, combinations, or clusters. To date, evidence suggests that the association between physical and mental chronic conditions can be bi-directional and the link between physical and mental chronic conditions might go in both directions6. A study in Scotland found that the prevalence of multimorbidity was 23.0% for those aged between 45 and 54 years and 76.1% for those aged 75 years above in 2007. However, among patients with multimorbidity, the presence of both physical and mental chronic conditions (i.e. mental-physical multimorbidity) was the most common multimorbidity pattern (approximately 50% of those with multimorbidity) in the non-elderly adult population7. A more recent study in Singapore found that the prevalence of multimorbidity was 39.2% in those aged between 45 and 64 years in 2016, but the prevalence of mental-physical multimorbidity was only 3.3%8. Previous studies have shown that the adverse impact of physical chronic conditions on individuals can be further exacerbated by the co-existence of mental chronic conditions, as the latter raises the complexities of clinical treatment and patient management9,10,11,12,13.
Health-related Quality of Life (HRQoL) is an outcome measure that is commonly used in clinical settings and population health surveys. Several studies have shown that multimorbidity has negative effects on HRQoL14,15,16. However there are limited evidence on the multiplicative (synergistic) effects of mental and physical chronic conditions, and they were all from high-income countries17,18,19,20. There is a paucity of research investigating the independent and multiplicative effects of mental and physical multimorbidity on HRQoL in a LMIC setting, where the prevalence and pattern of multimorbidity, and the ability of its health care system and social support service in mitigating the potential combined impact of physical illness and mental disorder on health outcomes might be different. Furthermore, existing research tends to focus on average HRQoL, ignoring the fact that the impact of multimorbidity may differ for individuals with varying levels of HRQoL.
To fill this critical knowledge gap, in this study, we used nationally representative panel data from China to investigate the independent and multiplicative effects of depression and physical multimorbidity on HRQoL in China, and aim to understand how the multiplicative effects vary by population segments (i.e., across age, by sex, and among people with poorer and better health).
Method
Sample and data
We used data from the China Health and Retirement Longitudinal Study (CHARLS), which collects information on individuals aged 45 years or older in China and their household characteristics. The survey data included measures of physical and psychological health, demographics, and socio-economic status (SES) information21.
We utilised two waves (2011 and 2015) of the CHARLS data that are publicly available. The baseline sample comprised of 17,708 individuals, of which 13,702 also had measurements on blood pressures. There were 10,063 individuals who remained in the 2015 wave, among which, 9657 had HRQoL measured in both waves. After removing individuals with missing values for key independent variables (4.4%), our final sample consisted of 9227 individuals each year, thus a total of 18,454 pooled sample observations in the panel data of two survey waves.
Variables
A total of 12 physical chronic conditions were used to measure physical multimorbidity, including diagnosed hypertension and 11 self-reported diagnosed physical chronic conditions (diabetes, dyslipidaemia, heart disease, stroke, cancer, chronic lung disease, digestive disease, liver disease, kidney disease, arthritis and asthma). Individuals were defined as hypertensive if they had either a systolic blood pressure (SBP) ≥ 140 mmHg, a diastolic blood pressure (DBP) ≥ 90 mmHg, or if they were taking anti-hypertension medicines at the time of the survey22. We counted the number of physical chronic conditions reported for each participant to identify those with physical multimorbidity. We used the presence of depressive symptoms as an indicator of the presence of a mental health condition13,23. Depressive symptoms were identified using a self-reported Center for Epidemiologic Studies Depression 10 items (CES-D10) score, which had been identified as a valid, reliable and useful mental health assessment tool for elderly in China24. An individual with a score greater than ten was identified as having depression25,26. Respondents who had both depressive symptoms and physical chronic conditions were defined as having co-existing depression and physical multimorbidity.
The main HRQoL outcomes included the proxy physical component score (PCS) and mental component score (MCS) from the matched Short Form 36 (SF-36) constructed based on CHARLS questionnaires27,28. Both PCS and MCS range in values from 0 to 100, with 0 score indicating the lowest level of functioning and 100 score indicating the highest possible level of functioning. SF-36 is the most widely used HRQoL measure of studies on multimorbidity and HRQoL14. Standard SF-36 is a 36-question comprehensive health survey that covers eight domains used to define quality of life, including physical functioning, bodily pain, role physical, general health, mental health, social functioning, vitality and role emotional. The CHARLS questionnaire does not include any standard HRQoL instruments but contains a wide range of health indicators that can be used to construct the SF-36 based measure. We used the proxy measure of SF-36 including summarised PCS and MCS constructed by Hao et al27,28. Items and variables used to construct the proxy SF-36 measure are provided in the appendix (Figure S1). Details on the construction of the proxy measure and psychometric assessment has been described elsewhere27,28.
The following variables were included as covariates: year, age, gender, marital status (married and partnered, and otherwise), residency (rural or urban), Hukou (household registration system) status (agricultural or rural Hukou or non-agricultural or urban Hukou), geographical region (four regional classes), education (illiterate, primary school, secondary school, college and above), socio-economic status quartiles (annual per capita household consumption expenditure, Q1 being the poorest and Q4 being the richest), work type (formally employed, farming, self-employed and family business, and unemployed or retired)26 and disability (reported difficulties in activity of daily living)13.
Statistical analyses
We described the prevalence of physical multimorbidity, depression, and co-existing of depression and physical multimorbidity across different population subgroups in two waves. We investigated socio-demographic correlates of multimorbidity using a mixed-effect logistic regression model.
We summarised the mean of outcomes by the number of physical chronic conditions, the presence of depression, and across different population subgroups. We examined the multiplicative effect of depression and physical multimorbidity on HRQoL using a mixed-effects linear regression model. Our null hypothesis was that the effect of having depression and physical chronic conditions on HRQoL was simply additive, no more than the sum of each condition. We tested the hypothesis by including two-way interaction terms between the number of physical chronic conditions and depression in the regression models. A statistically significant and negative coefficient for the interaction terms (negative coefficients in linear regressions of HRQoL) suggests that the combined adverse effect of two conditions was more than the additive effect of each one of them independently.
We examined how the effects of depression and physical multimorbidity on HRQoL vary by population segments through subgroup analysis and quantile analysis. We examined whether the association between physical chronic conditions, depression and HRQoL may be different for people at different levels of quality of life. In this analysis, we ran a series of quantile regression models at the 25th, 50th, 75th percentiles of the HRQoL outcomes. Quantile regression fit a line to minimizes the sum of absolute residuals. The objective is to estimate the median (as well as 25th and 75th percentile) of the outcome variable conditional on independent variables. Quantile regression analysis has been increasingly adopted in health systems research29,30. The method is robust to outliers because it allows for studying the full distribution of the outcome variable and is suitable for modelling outcomes such as HRQoL, which are often skewed or not normally distributed. The coefficients at lower quartile (i.e., the 25th percentiles) present the association between multimorbidity and outcomes on those with low HRQoL, while higher quartile (i.e. the 75th) reflects the association for those with higher HRQoL. We further examined the effect of number of chronic conditions on HRQoL to explore the burden of multimorbidity on HRQoL as an additional analysis. We reported the regression coefficient with 95% confidence intervals (CI). All statistical analyses were conducted using STATA 15.0. All methods were carried out in accordance with the Declaration of Helsinki.
Ethical approval and consent to participate
The Biomedical Ethics Review Committee of Peking University approved the CHARLS study (approval number: IRB00001052–11015). Informed consent was obtained from participants.
Results
Prevalence of depression and physical multimorbidity
We analysed data from 9227 respondents. The median age of the participants was 58 years (inter-quartile range [IQR] 51–64) in 2011 and 62 years (IQR 55–68) in 2015. The majority of the participants were married, lived in a rural area, illiterate, and worked in the agricultural sector (Appendix Table S1). As shown in Table 1, the prevalence of multimorbidity was 55.8% among Chinese aged over 45 years in 2011, which increased to 66.7% to 2015. In 2015, the prevalence of depression and physical multimorbidity was 30.6% and was higher among older ages and females (female vs male: 37.3% and 23.4%).
Table 2 presents the factors associated with depression, any type of multimorbidity and mental-physical multimorbidity. Respondents who were female, not married, having a non-agricultural Hukou, not residing in East China, illiterate, unemployed or worked in the farming sector, and having difficulties in activity of daily living were more likely to have depression, compared to their counterparts. The probability of having any type of multimorbidity was higher among people who were female, living in regions other than East China, having higher household consumption expenditure, unemployed or retired, and having difficulties in activity of daily living. The probability of having depression and physical multimorbidity was higher in respondents aged between 65 and 74 years compared to aged 45 and 54 years (adjusted odds ratio [aOR] 1.32, 95%CI 1.13, 1.54), among female (aOR 2.15, 95% CI 1.91, 2.42), having a rural Hukou (aOR 2.26, 95% CI 1.81, 2.83), unemployed or retired (aOR 1.75, 95%CI 1.45, 2.11) and illiterate compared to their counterparts.
Depression and physical multimorbidity and health-related quality of life
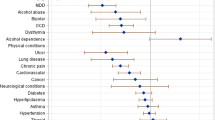
The unadjusted mean of the two HRQoL outcomes by type of multimorbidity and by demographic and socio-economic groups are reported in Table S2. The adjusted effects on physical and mental chronic conditions on HRQoL are presented in Table 3. We found that respondents with more physical conditions had lower PCS and MCS. An increase of one in the number of physical conditions led to a statistically significant reduction of 2.27 (95% CI − 2.44, − 2.11) points in PCS and reduction of 0.38 (95% CI − 0.55, − 0.22) points in MCS, after adjusting for socio-economic and demographic factors. Independently, depression was also significantly associated with lower PCS (a reduction of 6.58, 95% CI − 7.19, − 5.97) and MCS (a reduction of − 25.26, 95% CI − 25.88, − 24.64).
There were significant interaction effects of depression and physical chronic condition on PCS (regression coefficient for interaction term = − 0.83, 95% CI − 1.06, − 0.60) and a lesser extent with MCS (regression coefficient for interaction term = − 0.50, 95% CI − 0.73, − 0.27). The results suggest that the impact of depression and physical multimorbidity was multiplicative rather than a simple additive effect on decreasing HRQoL.
Quantile regression analysis and subgroup analysis
Table 3 also shows the differential impacts of depression and physical multimorbidity on the PCS and MCS at the 25th, 50th and 75th percentiles, after adjusting for covariates. Our findings suggest that the magnitude of the multiplicative effect of depression and physical multimorbidity on PCS and MCS was larger in the lower percentile (i.e. 25th) of the HRQoL distribution compared with the higher percentile (75th) of the HRQoL distribution. The full regression results are reported in Appendix (Tables S3 and S4).
Figure 1 shows the estimated mean PCS and MCS by type of multimorbidity across age and gender. Both PCS and MCS decrease with ages. PCS scores were on average five points lower for females compared to males within the same age group whereas the differences in MCS among males and females were smaller. For example, among those who were between 45 and 54 years, PCS decreased from 83.7 for males and 80.8 for females without any physical chronic conditions and depression to 69.4 for males and 65.1 for females with more than two physical chronic conditions and depression. In the same age group, MCS decreased from 73.5 for males and 72.0 for females without any condition to 46.1 and 44.2 among those who had more than two physical chronic conditions and depression.
Estimated mean proxy Physical Component Scores (PCS) and Mental Component Scores (MCS) scores by age groups and sex. China Health and Retirement Longitudinal Study, 2011–2015. Mixed-effect linear models are used to estimate the association between multimorbidity and PCS and MCS scores. Models were adjusted for age, sex, marital status, residency, Hukou status, geographical region, education, socio-economic status quartiles, work type and disability.
We additionally estimated the mean proxy PCS and MCS by Hukou status and by educational level. Respondents with an agricultural (i.e. rural) Hukou had the lowest PCS and MCS compared to non-agricultural Hukou and migrants. Respondents with low education had lower PCS and MCS than those with high education level. The results are presented in Figure S2. In addition, we examined the effect of number of chronic conditions on HRQoL. An increased number of chronic conditions was associated with lower PCS and MCS scores. The results are reported in Table S5 and Figure S3 in the appendix.
Discussion
Our results showed that in 2015 the prevalence of mental-physical multimorbidity was 30.6% among Chinese aged over 45 years. Increasing numbers of physical chronic conditions and depression were independently associated with lower PCS and MCS. There were significant interactions of depression and physical chronic condition, suggesting the effects on HRQoL was multiplicative rather than simply additive. The negative effects of co-occurring depression and physical multimorbidity on HRQoL were greatest in women and those in poorer health.
Our results from quantile regression analysis revealed a more detailed measure of the association between multimorbidity and HRQoL that was not able to find in existing studies using ordinary least squares regression or generalised linear model. Multimorbidity has significant effect on HRQoL at various point of the distribution, and it remain predictive even for those with high HRQoL.
Our findings align with previous studies in China and the international context, showing that physical chronic conditions and depression impact negatively on HRQoL, independently14,31,32,33,34. Our results further indicated that depression, compared to each increased number of physical chronic conditions, had a greater effect on lowering HRQoL18,20.
More importantly, our result showed that the multiplicative effects of co-existing of depression and physical multimorbidity on quality of life impairment exist in China, whereas previous evidence that from high-income settings (Spain, Singapore and US) found similar effects17,18,19,20. This suggests that the mechanism by which co-existing mental and physical multimorbidity have multiplicative deleterious effects on quality of life may be similar across populations in different settings. This is also in line with published studies showing that mental conditions can increase the level of health care use and medical cost in the presence of physical multimorbidity9,35.
Our study showed that a high proportion of the study population had multimorbidity, with a substantial percentage having both depression and physical conditions. The multiplicative negative effects of mental-physical multimorbidity on HRQoL indicates the challenges and complexity in managing the co-existing conditions. Health care systems that are typically organised around single diseases can no longer effectively address the burden from multimorbidity. It is crucial to priorities the integration of physical and mental health care to improve patients’ outcome. An example of this approach was implemented in the United Kingdom, where recently issued national guidelines provided clinical directives for early assessment and management of patients with multimorbidity36.
The health delivery system in China is still single disease focused, hospital-centred and volume-driven. Renewing the focus on health promotion and management of multimorbidity would require a strong, affordable, and integrated primary health care system. China has made remarkable progress on this front37. However, further strategies should be strengthened to address the multimorbidity challenges, including shifting from secondary care to more integrated primary care, which would allow for better generalist health services38,39. Also, considering that the negative multiplicative effects are more pronounced among people with poorer health, more attention should be given to these groups to deliver targeted and tailored care and prevention services40,41. Efficient management of mental and physical multimorbidity needs an integrated care model and implementation of interventions in different settings, including both clinical settings and community. A recent systematic review found little evidence of an effect of HRQoL interventions for people with multimorbidity in primary care and community settings42,43. The review suggested that future research should consider patient experience of care, optimising medicines management and targeted patient health behaviours such as exercise. More research that addresses the challenges of mental-physical multimorbidity is needed to inform the development of interventions that can be applied to the wider community in China.
We presented the first study that systematically assessed the multiplicative effects of depression and physical multimorbidity on HRQoL and investigated differential impacts on population segments in China using longitudinal data and a quantile regression approach. However, our study has several important caveats. The first relates to the use of the proxy SF-36 based on available survey questions rather than using the standard SF-36 instrument. To the best of our knowledge, there is no public national representative longitudinal dataset that have used a standard HRQoL instrument in China. Despite the possible bias using the constructed instrument, our results are consistent with the literature on the impact of deteriorating physical and mental health using the SF-36 instrument, suggesting the constructed measure has a degree of face validity. Our study estimated HRQoL through PCS and MCS, rather than health utilities44. This was because not all corresponding items required to calculate utilities based on SF-6D45 was available in CHARLS questionnaires. The second relates to the use of self-reported measures in physical chronic conditions. Self-reported measures of physical chronic conditions may underestimate their prevalence, particularly among those from lower SES and educational backgrounds and rural areas due to restricted access to healthcare services. Also, we did not consider different combinations of physical chronic conditions. Third, as CHARLS does not contain other measures on mental health conditions except for depression, our estimated effects of having depression may capture a wider effects of mental health conditions. In addition, depressive symptoms are a part of HRQOL measures, our models included conceptually similar variables on both sides of the equation46. These might explain the very large effects we found of depression on both MCS and PCS. However, it does not alter our conclusion that care for people with depression needs to be prioritised given its substantial impact on not only mental health but also physical health. Future research that considers different combinations of chronic conditions and include more mental conditions can enrich our understanding of the impact of mental and physical multimorbidity on HRQoL. Standard HRQoL instruments should be incorporated in future large-scale population health surveys in China.
In conclusion, the present study has shown that HRQoL decreased markedly with multimorbidity and is exacerbated by the presence of both mental and physical chronic conditions. There is a need to prioritise interventions to health outcomes for patients suffering from co-occurring depression and physical health conditions in China.
Data availability
The data that support the findings of this study are available from the China Health and Retirement Longitudinal Study (CHARLS) study (charls.pku.edu.cn) but restrictions apply to the availability of these data. Data are however available from the authors upon reasonable request and with permission of the CHARLS study team.
Code availability
Stata Code for the analysis is available from the authors upon reasonable request.
References
Academy of Medical Sciences. Multimorbidity: a priority for global research (2018).
Arokiasamy, P. et al. The impact of multimorbidity on adult physical and mental health in low- and middle-income countries: what does the study on global ageing and adult health (SAGE) reveal?. BMC Med. 13, 178. https://doi.org/10.1186/s12916-015-0402-8 (2015).
Zhao, Y. et al. Physical multimorbidity, health service use and catastrophic health expenditure by socio-economic groups in China: A panel data analysis. Lancet Global Health 8, e840–e849 (2020).
Huang, Y. et al. Prevalence of mental disorders in China: A cross-sectional epidemiological study. Lancet Psychiatry 6, 211–224. https://doi.org/10.1016/S2215-0366(18)30511-X (2019).
Que, J., Lu, L. & Shi, L. Development and challenges of mental health in China. General Psychiatry 32, e100053. https://doi.org/10.1136/gpsych-2019-100053 (2019).
Read, J. R., Sharpe, L., Modini, M. & Dear, B. F. Multimorbidity and depression: A systematic review and meta-analysis. J. Affect. Disord. 221, 36–46. https://doi.org/10.1016/j.jad.2017.06.009 (2017).
McLean, G. et al. The influence of socioeconomic deprivation on multimorbidity at different ages: A cross-sectional study. Br. J. General Pract. 64, e440-447 (2014).
Low, L. L. et al. Epidemiologic characteristics of multimorbidity and sociodemographic factors associated with multimorbidity in a rapidly aging Asian Country. JAMA Netw. Open 2, e1915245. https://doi.org/10.1001/jamanetworkopen.2019.15245 (2019).
Payne, R. A., Abel, G. A., Guthrie, B. & Mercer, S. W. The effect of physical multimorbidity, mental health conditions and socioeconomic deprivation on unplanned admissions to hospital: A retrospective cohort study. CMAJ 185, E221-228. https://doi.org/10.1503/cmaj.121349 (2013).
Demyttenaere, K. et al. Comorbid painful physical symptoms and depression: Prevalence, work loss, and help seeking. J. Affect. Disord. 92, 185–193. https://doi.org/10.1016/j.jad.2006.01.007 (2006).
Sheridan, P. E., Mair, C. A. & Quinones, A. R. Associations between prevalent multimorbidity combinations and prospective disability and self-rated health among older adults in Europe. BMC Geriatr. 19, 198. https://doi.org/10.1186/s12877-019-1214-z (2019).
Mercer, S. W., Gunn, J., Bower, P., Wyke, S. & Guthrie, B. Managing patients with mental and physical multimorbidity. BMJ 345, e5559. https://doi.org/10.1136/bmj.e5559 (2012).
Pan, T. et al. The association between mental-physical multimorbidity and disability, work productivity, and social participation in China: A panel data analysis. BMC Public Health 21, 376. https://doi.org/10.1186/s12889-021-10414-7 (2021).
Makovski, T. T., Schmitz, S., Zeegers, M. P., Stranges, S. & van den Akker, M. Multimorbidity and quality of life: Systematic literature review and meta-analysis. Ageing Res. Rev. 53, 100903. https://doi.org/10.1016/j.arr.2019.04.005 (2019).
Fortin, M., Dubois, M. F., Hudon, C., Soubhi, H. & Almirall, J. Multimorbidity and quality of life: a closer look. Health Qual. Life Outcomes 5, 52. https://doi.org/10.1186/1477-7525-5-52 (2007).
Agborsangaya, C. B., Lau, D., Lahtinen, M., Cooke, T. & Johnson, J. A. Health-related quality of life and healthcare utilization in multimorbidity: results of a cross-sectional survey. Qual. Life Res. 22, 791–799. https://doi.org/10.1007/s11136-012-0214-7 (2013).
Lim, L., Jin, A. Z. & Ng, T. P. Anxiety and depression, chronic physical conditions, and quality of life in an urban population sample study. Soc. Psychiatry Psychiatr. Epidemiol. 47, 1047–1053. https://doi.org/10.1007/s00127-011-0420-6 (2012).
Ho, C. et al. Coexisting medical comorbidity and depression: multiplicative effects on health outcomes in older adults. Int. Psychogeriatr. 26, 1221–1229. https://doi.org/10.1017/S1041610214000611 (2014).
Bayliss, M. et al. Health-related quality of life (HRQL) for individuals with self-reported chronic physical and/or mental health conditions: Panel survey of an adult sample in the United States. Health Qual. Life Outcomes 10, 154. https://doi.org/10.1186/1477-7525-10-154 (2012).
Pinto-Meza, A. et al. Impact of mental disorders and chronic physical conditions in health-related quality of life among primary care patients: results from an epidemiological study. Qual. Life Res. 18, 1011–1018. https://doi.org/10.1007/s11136-009-9522-y (2009).
Zhao, Y., Hu, Y., Smith, J. P., Strauss, J. & Yang, G. Cohort profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 43, 61–68. https://doi.org/10.1093/ije/dys203 (2014).
National Health and Family Planning Commission. Chinese citizens nutrition and chronic disease report 2015 (People’s Medical Publishing House, 2015).
Zhao, Y. et al. The impact of mental and physical multimorbidity on healthcare utilization and health spending in China: A nationwide longitudinal population-based study. Int. J. Geriatr. Psychiatry 36, 500–510. https://doi.org/10.1002/gps.5445 (2021).
Boey, K. W. Cross-validation of a short form of the CES-D in Chinese elderly. Int. J. Geriatr. Psychiatry 14, 608–617. https://doi.org/10.1002/(SICI)1099-1166(199908)14:8%3c608::AID-GPS991%3e3.0.CO;2-Z (1999).
Strauss, J. et al. Health Outcomes and Socio-economic Status Among the Elderly in China: Evidence from the CHARLS Pilot. Population Ageing, 111–142 (2010).
Zhao, Y. W. et al. The effect of multimorbidity on functional limitations and depression amongst middle-aged and older population in China: a nationwide longitudinal study. Age Ageing 50, 190–197. https://doi.org/10.1093/ageing/afaa117 (2020).
Hao, X. Evaluating the Effectiveness of health management programs for the elderly in the National Basic Public Health Services on the Health-Related Quality of Life of the elderly in China MPH thesis, Peking Union Medical College, (2019).
Hao, X. Q., Yang, Y. H., Gao, X. T. & Dai, T. Evaluating the effectiveness of the health management program for the elderly on health-related quality of life among elderly people in China: Findings from the China Health and Retirement Longitudinal Study. Int. J. Environ. Res. Public Health 16, 113 (2019).
Anindya, K. et al. Effect of multimorbidity on utilisation and out-of-pocket expenditure in Indonesia: Quantile regression analysis. BMC Health Serv. Res. 21, 427. https://doi.org/10.1186/s12913-021-06446-9 (2021).
Zhao, Y. et al. Medical costs and out-of-pocket expenditures associated with multimorbidity in China: Quantile regression analysis. BMJ Glob. Health 6, e004042. https://doi.org/10.1136/bmjgh-2020-004042 (2021).
She, R. et al. Multimorbidity and health-related quality of life in old age: Role of functional dependence and depressive symptoms. J. Am. Med. Dir. Assoc. 20, 1143–1149. https://doi.org/10.1016/j.jamda.2019.02.024 (2019).
Mujica-Mota, R. E. et al. Common patterns of morbidity and multi-morbidity and their impact on health-related quality of life: Evidence from a national survey. Qual Life Res 24, 909–918 (2015).
Bao, X. Y. et al. The association between multimorbidity and health-related quality of life: A cross-sectional survey among community middle-aged and elderly residents in southern China. Health Qual Life Outcomes https://doi.org/10.1186/s12955-019-1175-0 (2019).
Yang, H. et al. Association of self-rated health with chronic disease, mental health symptom and social relationship in older people. Sci. Rep. 11, 14653. https://doi.org/10.1038/s41598-021-94318-x (2021).
Katon, W. J. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol. Psychiatry 54, 216–226 (2003).
National Institute for Health and Care Excellence. Multimorbidity: clinical assessment and management. (NICE, London).
Meng, Q., Mills, A., Wang, L. & Han, Q. What can we learn from China’s health system reform?. BMJ 365, l2349. https://doi.org/10.1136/bmj.l2349 (2019).
Li, X. et al. The primary health-care system in China. Lancet 390, 2584–2594. https://doi.org/10.1016/S0140-6736(17)33109-4 (2017).
Chen, H., Chen, Y. & Cui, B. The association of multimorbidity with healthcare expenditure among the elderly patients in Beijing, China. Arch. Gerontol. Geriatr. 79, 32–38 (2018).
Zhang, Y. et al. Prevalence, correlates and outcomes of multimorbidity among the middle-aged and elderly: Findings from the China Health and Retirement Longitudinal Study. Arch. Gerontol. Geriatr. 90, 104135. https://doi.org/10.1016/j.archger.2020.104135 (2020).
Zhang, Z. et al. Associations between mental health disorder and management of physical chronic conditions in China: A pooled cross-sectional analysis. Sci. Rep. 11, 5731. https://doi.org/10.1038/s41598-021-85126-4 (2021).
Smith, S. M., Wallace, E., O’Dowd, T. & Fortin, M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev 3, Cd006560. https://doi.org/10.1002/14651858.CD006560.pub3 (2016).
Smith, S. M., Wallace, E., Clyne, B., Boland, F. & Fortin, M. Interventions for improving outcomes in patients with multimorbidity in primary care and community setting: A systematic review. Syst. Rev. 10, 271. https://doi.org/10.1186/s13643-021-01817-z (2021).
Ara, R. & Wailoo, A. J. Estimating health state utility values for joint health conditions: A conceptual review and critique of the current evidence. Med. Decis. Mak. Int. J. Soc. Med. Decis. Mak. 33, 139–153. https://doi.org/10.1177/0272989x12455461 (2013).
Brazier, J., Roberts, J. & Deverill, M. The estimation of a preference-based measure of health from the SF-36. J. Health Econ. 21, 271–292. https://doi.org/10.1016/s0167-6296(01)00130-8 (2002).
Hays, R. D. & Fayers, P. M. Overlap of depressive symptoms with health-related quality-of-life measures. Pharmacoeconomics 39, 627–630. https://doi.org/10.1007/s40273-020-00972-w (2021).
Author information
Authors and Affiliations
Contributions
T.P. and J.T.L. conceived and designed the study. N.D. and S.M. provided important advice on study design. T.P., K.A. and X.H. carried out the initial analysis. N.D., S.M., and B.M. interpreted the data. Y.Z., A.H. and T.P. analysed the literature. T.P. and J.T.L. wrote the first draft of the paper. N.D., S.M., B.M., K.A., A.H., Y.Z. and T.M. provided advice on the first draft and revised the article critically for important intellectual content. All authors reviewed and had final approval of the submitted versions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pan, T., Anindya, K., Devlin, N. et al. The impact of depression and physical multimorbidity on health-related quality of life in China: a national longitudinal quantile regression study. Sci Rep 12, 21620 (2022). https://doi.org/10.1038/s41598-022-25092-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-25092-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.