Abstract
The aim of our study was to assess whether a well-established federal state-wide Stroke Care Pathway delivering high quality stroke care can cope with the COVID-19 pandemic and associated measures to contain the virus spread. The retrospective analysis is based on a prospective, quality-controlled, population-based registry of all stroke patients in the Tyrol, a federal state of Austria and one of the early hot-spots of COVID-19 in Europe. Patient characteristics, pre-hospital management, intra-hospital management and post-hospital were analysed. All residents of the Tyrol suffering ischemic stroke in 2020 (n = 1160) and four pre-COVID-19 years (n = 4321) were evaluated. In 2020, the annual number of stroke patients was the highest in this population-based registry. When local hospitals were overwhelmed with SARS-CoV-2-patients, stroke subjects were temporarily allocated to the comprehensive stroke centre. Stroke severity, quality metrics of stroke management, serious complications, and post-stroke mortality did not differ between 2020 and the four comparator years. Notably, iv. thrombolysis-rate was similar (19.9% versus 17.4%, P = 0.25) and endovascular stroke treatment even better (5.9% versus 3.9%, P = 0.003) but resources for in-patient rehabilitation were limited (25.8% versus 29.8%, P = 0.009). Concluding, a well-established Stroke Care Pathway was able to maintain high-quality acute stroke care even when challenged by a global pandemic.
Similar content being viewed by others
Introduction
Since the WHO declared the coronavirus disease 2019 (COVID-19) a global pandemic on March 11th 2020, converging evidence suggests that stroke admissions have decreased and disruptions in the delivery of emergency stroke care, such as intravenous (iv.) thrombolysis, occurred1,2,3,4,5,6,7,8. Factors that propagated these changes have predominantly been attributed to efforts aimed to contain the spread of the virus3,9,10,11. Mortality has increased in COVID-19 times, in part because of impaired care of other diseases or, in case of ischemic stroke, due to the substantial reduction of acute stroke therapy12. To get an unbiased view of how COVID-19 affects stroke, reliable population-based data are mandatory. Our aim was to provide data from a federal state of Austria, that collects information of all stroke patients since 2009, and to investigate whether our well-established Tyrolean Stroke Pathway, that defines and continuously improves stroke management in the pre-hospital, intra-hospital, and rehabilitation field13, held up stroke-management-quality against one of the most strenuous crises in recent history.
Methods
The following analyses were performed using data from the Tyrolean Stroke Pathway database, which provided one of the first evidence that Stroke Care Pathways improve patients’ outcome13. In short, the pathway was implemented in 2009, funded by the Tyrolean Government and health insurance carriers and has since been sustained to maintain high quality routine stroke care in the pre-hospital, hospital and post-stroke rehabilitation phase in the entire federal state. All patients that suffer ischemic- or hemorrhagic stroke and are admitted to any of the 8 hospitals in the Tyrol are included in the database. The subjects are identified through stroke discharge codes (International Statistical Classification of Diseases and Related Health Problems 10th Revision [ICD-10]) and digital data entry by a trained and qualified team is mandatory for reimbursement. Information on stroke characteristics (i.e. etiology, baseline National Institute of Health Stroke Scale [NIHSS]), pre-hospital management (i.e. emergency medical services transport modality), acute management timing and strategies (i.e. hospital arrival, acute imaging modalities, iv. thrombolysis and thrombectomy) in-house complications as well as early rehabilitation measures are supplemented by central governmental information about mortality, inter-hospital transfers discharge destinations and in-patient rehabilitation. Data collection and – entry into a three-page form, which is embedded within the electronic file of each stroke subject, was done by stroke teams located at each hospital in the Tyrol. Patients cannot be discharged from the treating hospital if the form is not completed. The database is monitored for completeness (100% complete) and accuracy by the Tyrolean Health Care Fund. The Stroke Care Pathway consists of more than 100 individual items, primarily focused on improving communication between sections (i.e. emergency medical service, hospital personnel, therapists) and organizational processes. Along with the documentation aspects, as previously reported13, the Tyrol Stroke Pathway encompasses the following selected key components: Repeated stroke awareness and information campaigns (especially focused on the general public), prehospital stroke codes, hospital pre-notification, prehospital triage algorithm, algorithms for helicopter and emergency doctor involvement, standardized information transfer, practice guidelines for diagnostic work-up and stroke therapy, thrombolysis administration protocol, early routine mobilization of patients, practice standards for nurses and therapists, assembly of stroke teams, continuous educational activities for all health care professions, obligatory NIHSS training, CT prioritization, obligatory dysphagia testing, standardized assessment of stroke complications, tele-radiology, early state-of-the-art secondary prevention, standardized discharge management, 24/7 access to stroke expertise, competence platform and decision support, web-based stroke pathway, regional rehabilitation transfer agreements, emergency medical service bypass and referral protocols, annual feedback visits, continuous feedback of achievements, standardized electronic documentation of selected quality parameters, education of and educational material for patients and their relatives, follow-up at three months, therapy standards for inpatient rehabilitation, network for quality-controlled outpatient rehabilitation.
Patient recruitment and selection
In all, only patients coded as I63 as a main diagnosis were considered for the analysis. ICD 10 Codes I62, I64 and G46 are not permitted for reimbursement by the Tyrolean Healthcare Fund and source data verification of G45 coded patients are regularly performed by the data management team to ensure delimitability between ischemic stroke and TIA patients. All residents of the Tyrol suffering ischemic stroke treated in any Tyrolean hospital in 2015–2017, 2019 and 2020 were included in the study. 2020 was considered the COVID-19 year whilst all others (2015–2017 and 2019) were pre-COVID-19 comparators14. Based on database maintenance, data input was disabled for 3 months in 2018, therefore 2018 was not considered in the current analysis. The Tyrol has high mountain chains along its borders to Italy and Germany and, accordingly, the proportion of acute stroke patients living within the catchment area but being treated outside the Tyrol was well below 1.0% per year, thus negligible, (data source Documentation and Information Systems for Analyses in Health Care [DIAC]) and the hospitalization rates for stroke was 97.4%13. There was no formal patient involvement plan during the set-up process of the Tyrol Stroke Pathway.
Statistical methodology
Statistical analyses were performed using R, version 4.2.2 (R-Core Team [2021]. R-Foundation for Statistical Computing, Vienna, Austria). Confidence intervals for proportions were obtained by the Clopper-Pearson method. Chi-squared test for categorical and Mann–Whitney-U test for continuous variables examined group differences.
Standard protocol approvals, registration, patient consents
Analyses were approved by the local ethics committee at the Medical University of Innsbruck (EK#1152/2020). Data was collected as part of the governmental quality-assurance dataset of the Tyrolian Stroke Pathway based on the Tyrolean Healthcare Fund law (TGFG §18) and the federal law on health care documentation and the target control health (Art. 15a Bundesverfassungsgesetz–Zielsteuerung Gesundheit). Therefore, individual patient consent was not required. All methods were carried out in accordance with relevant guidelines and regulations. Anonymized data not published within this article will be made available by request from any qualified investigator.
Results
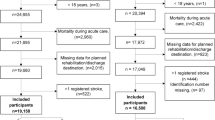
Baseline characteristics of 5481 stroke patients (n = 1160 in COVID-19 and n = 4321 in the four comparator years) are given in Table 1 and Fig. 1.
In 2020, the annual number of stroke patients was the highest in our population-based registry which is active from 2009 onwards. Stroke incidence was 153.1/100.000 compared to 145.5/100.000 in the four comparator years, which was not statistically significant (P = 0.13). There were no differences in stroke severity, relevant quality indices of acute stroke management or post-stroke mortality. In 2020, however, stroke patients were more frequently allocated to the comprehensive stroke center, rate of endovascular thrombectomy increased and post-stroke care in rehabilitation centers decreased. Concerning in-hospital treatment, severe complications were unchanged but urinary tract infections in 2020 were more frequent.
Discussion
Cardiovascular disease is the main cause of death, with stroke being the most frequent, devastating, time-critical vascular emergency and one of the leading causes of disability world-wide13,15. Therefore, even in challenging times, it is indispensable to provide quality care for stroke subjects. Stroke is a serious complication of COVID-19 affecting approximating 1.3% of all cases16. Previous evidence suggested that the COVID-19 pandemic has impacted stroke care around the globe with decreased hospital admissions, especially of minor stroke patients, and a decline in rates of iv. thrombolysis and endovascular thrombectomy1,3,6,7. We report the impact of COVID-19 in a federal state of Austria using a population-based registry of near 100% of all stroke patients in the region. The Tyrol was an early hot-spots of COVID-19 in Europe. Internal and neurological hospitals treating stroke patients were crucially involved in managing severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) patients but stroke units and angiosuites were preserved. The annual number of stroke patients in 2020 was the highest in our population-based registry (active from 2009 onwards). Stroke severity (including minor stroke) and stroke characteristics remained unchanged (Fig. 1). Previous studies have reported a decline in stroke admissions and acute management strategies such as i.v. thrombolysis especially in non-stroke centers (drip-and-ship concept) during COVID-1917,18. The Tyrolean Stroke Pathway recommends the mothership concept for patients with severe stroke symptoms if the thrombectomy center can be reached within 30 min. Accordingly, during the COVID-19 pandemic, hospital allocation of stroke patients has temporarily changed, whenever local hospitals were overwhelmed with SARS-CoV-2 patients and stroke patients were directly transported to the comprehensive stroke center Innsbruck (mothership)17,18. In spite of the measures taken in the whole federal state to prevent intra-hospital COVID-19 spread, the rate of iv. thrombolysis was at least as good as in the four comparator years (Table 1, Fig. 1). Further, time-dependent quality indices of acute stroke management remained unchanged with rates of patients being admitted within 3 h of symptom onset and subjects having initial cerebral imaging within 1 h of hospital admission as well as door-to-needle-time seeing no significant difference (Table 1). The rate of thrombectomy has annually increased since the landmark trials of 2015 (thrombectomy rates 2015, 2016, 2017 and 2019 were 2.7%, 3.6%, 3.9%, and 4.6%) and the up-wards trajectory persists in 2020 (5.3%, P = 0.014)19. This increase might in-part be due to a higher incidence of large vessel occlusions reported in literature during the COVID-19 pandemic20,21. No change emerged concerning serious in-house complications and stroke mortality. Urinary tract infections were more frequent in 2020 compared to previous years, which may be due to increased screening for sources of fever and inflammation in COVID-19 times. This finding is in line with previous reports suggesting higher rates of infections overall in rehabilitation eligible patients unable to be transferred to rehabilitation facilities22. As one of the two stroke rehabilitation centers in Tyrol was partially reassigned to treat SARS-CoV-2 patients in early spring and late autumn in 2020, the share of in-patient post-stroke rehabilitation was impaired (25.9% versus 29.8%) and partly compensated by out-patients rehabilitation. In conclusion, the Tyrol Stroke Pathway, through its network of stake-holders making timely decisions and its continuous stroke awareness campaigns to Tyrolian inhabitants, was able to maintain high-quality stroke care even when challenged by a global pandemic. Therefore, we emphasize on the positive impact that structured treatment pathways have on the functional outcome of ischemic stroke subjects, which could presumably be extrapolated to other time-critical emergencies, such as myocardial infarction. The key strength of our study is the Tyrol Stroke Pathway database being one of the very few population-based registries that covers information on all stroke patients in a federal state irrespective of the treating hospital, which additionally has full data monitoring and no missing data.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Nogueira, R. G. et al. Global impact of COVID-19 on stroke care and IV thrombolysis. Neurology 96, e2824–e2838 (2021).
Richter, D. et al. Analysis of nationwide stroke patient care in times of COVID-19 pandemic in Germany. Stroke https://doi.org/10.1161/STROKEAHA.120.033160 (2020).
Douiri, A. et al. Stroke care in the United Kingdom during the COVID-19 pandemic. Stroke 52, 2125–2133 (2021).
Zhao, J. et al. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke 51, 1996–2001 (2020).
Solomon, M. D. et al. Changes in patterns of hospital visits for acute myocardial infarction or ischemic stroke during COVID-19 surges. JAMA 326, 82–84 (2021).
Bhambhvani, H. P., Rodrigues, A. J., Yu, J. S., Carr, J. B. & Hayden Gephart, M. Hospital volumes of 5 medical emergencies in the COVID-19 pandemic in 2 US medical centers. JAMA Intern. Med. 181, 272–274 (2021).
Altersberger, V. L. et al. Maintenance of acute stroke care service during the COVID-19 pandemic lockdown. Stroke 52, 1693–1701 (2021).
Mariet, A.-S. et al. Hospitalizations for stroke in france during the COVID-19 pandemic before, during, and after the national lockdown. Stroke 52, 1362–1369 (2021).
Diegoli, H. et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke 51, 2315–2321 (2020).
Hsiao, J. et al. Effect of COVID-19 on Emergent stroke care: A regional experience. Stroke 51, e2111–e2114 (2020).
Teo, K.-C. et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke 51, 2228–2231 (2020).
Faust, J. S. et al. All-cause excess mortality and COVID-19-related mortality among US adults aged 25–44 years, March-July 2020. JAMA https://doi.org/10.1001/jama.2020.24243 (2020).
Willeit, J. et al. Thrombolysis and clinical outcome in patients with stroke after implementation of the Tyrol Stroke Pathway: a retrospective observational study. Lancet Neurol. 14, 48–56 (2015).
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria (2021). https://www.R-project.org/.
GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18, 439–458 (2019).
Qureshi, A. I. et al. Acute ischemic stroke and COVID-19: An analysis of 27 676 patients. Stroke 52, 905–912 (2021).
Brunetti, V. et al. Effect of the COVID-19 pandemic and the lockdown measures on the local stroke network. Neurol. Sci. 42, 1237–1245 (2021).
Romoli, M. et al. Stroke network performance during the first COVID-19 pandemic stage: A meta-analysis based on stroke network models. Int. J. Stroke 16, 771–783 (2021).
Goyal, M. et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387, 1723–1731 (2016).
Sacco, S. et al. Reduced admissions for cerebrovascular events during COVID-19 outbreak in Italy. Stroke 51, 3746–3750 (2020).
Richter, D. et al. A full year of the COVID-19 pandemic with two infection waves and its impact on ischemic stroke patient care in Germany. Eur. J. Neurol. 29, 105–113 (2022).
Thau, L. et al. Decline in rehab transfers among rehab-eligible stroke patients during the COVID-19 pandemic. J. Stroke Cerebrovasc. Dis. 30, 105857 (2021).
Author information
Authors and Affiliations
Consortia
Contributions
L.M.-S., M.K. and S.K. conceptualized and designed the study. L.M.-S., At.T., S.P., J.W., E.W., T.G., H.R. were involved in the acquisition of data and data analyses. L.M.-S., H.R. and M.K. interpreted the data. L.M.-S. wrote the manuscript. All authors have approved the submitted manuscript version and are accountable for their contributions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mayer-Suess, L., ter Telgte, A., Praxmarer, S. et al. Stroke Care Pathway ensures high-quality stroke management in the COVID-19 pandemic. Sci Rep 13, 5587 (2023). https://doi.org/10.1038/s41598-023-32586-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-32586-5
This article is cited by
-
Trends in stroke severity at hospital admission and rehabilitation discharge before and during the COVID-19 pandemic in Hesse, Germany: a register-based study
Neurological Research and Practice (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.