Abstract
Survival rates from colorectal cancer (CRC) are drastically higher if the disease is detected and treated earlier. Current screening guidelines involve stool-based tests and colonoscopies, whose acceptability and uptake remains low. Routinely collected blood-based biomarkers may offer a low-cost alternative or aid for detecting CRC. Here we aimed to evaluate the pre-diagnostic and diagnostic value of a wide-range of multimodal biomarkers in the UK Biobank dataset, including sociodemographic, lifestyle, medical, physical, and blood and urine-based measures in detecting CRC. We performed a Cox proportional hazard and a tree-boosting model alongside feature selection methods to determine optimal combination of biomarkers. In addition to the modifiable lifestyle factors of obesity, alcohol consumption and cardiovascular health, we showed that blood-based biomarkers that capture the immune response, lipid profile, liver and kidney function are associated with CRC risk. Following feature selection, the final Cox and tree-boosting models achieved a C-index of 0.67 and an AUC of 0.76 respectively. We show that blood-based biomarkers collected in routine examinations are sensitive to preclinical and clinical CRC. They may provide an additive value and improve diagnostic accuracy of current screening tools at no additional cost and help reduce burden on the healthcare system.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the fourth most common type of cancer after breast, prostate, and lung cancer in England, constituting 11.4% of all cancer cases1. Despite falling mortality rates over the last decades, CRC remains the second most common cause of cancer-related deaths with an age-standardised overall survival rate of 78% at year 1, subsequently falling to 59% after 5-years2,3. Metastasis is the main cause of mortality, observed in half of the CRC patients, with liver as the most common distant site4. Early detection drastically improves surgery and treatment outcome. Nearly 90% of patients survive at 5-years post-diagnosis, compared to only 10% in advanced-stages5. Further, early detection can reduce treatment costs and save healthcare professionals’ valuable time6. Biomarkers, indicators of a biological state that can be objectively measured and evaluated, can aid early detection. There is an urgent need for biomarkers that are sensitive and specific to early stages of CRC, well-accepted by patients, and scalable to the national level at lower costs.
Current gold standards of early diagnostic tools are faecal immunochemical test (FIT; 79% sensitivity, 94% specificity) in the UK and multitarget stool DNA test in the US (MT-sDNA, Cologuard®; 92% sensitivity, 86.6% specificity)7,8, which are followed up by colonoscopy and polypectomy, if positive. While stool-based tests show good diagnostic performance, are non-invasive, safe and simple to perform, patient acceptability and uptake remains low9. Instead, blood-based biomarkers offer a more acceptable, low-cost alternative to stool-based tests10, are routinely used across hospitals in the UK, and have the potential to be adopted for home-testing. Cancer-specific blood-based markers detect presence of genomic and epigenomic markers, circulating tumour cells, or specific protein markers such as carcinoembryonic antigen (CEA)11. Although these markers show diagnostic potential for CRC, they are not part of routine blood panels.
Numerous biochemical and hematological measures, tested in routine blood panels, show associations with the risk for developing CRC. Some of these biomarkers measure systemic inflammation, which include acute-phase proteins such as C-reactive protein and albumin12 and white blood cells such as lymphocytes and neutrophils13,14. Others include liver enzymes15,16 and lipids17 as well as hematological measures such as hemoglobin and platelets which might indicate rectal bleeding and anemia as a result of CRC13,18. Individually these biomarkers are not highly sensitive or specific to CRC. When combined, however, they might have the potential to detect wider, multifaceted aspects of the molecular changes that occur in CRC. Identifying optimal combinations can be achieved by using statistical or machine learning (ML) models, alongside data-driven feature selection methods.
In this study, using the longitudinal UK Biobank dataset, we investigate the diagnostic potential of a wide range of biomarkers including medical, socioeconomic, and routinely collected blood and urine-based laboratory measures, in detecting preclinical and clinical CRC. Here we adopt a data-driven approach and perform (i) feature selection to identify biomarkers sensitive to CRC; (ii) a survival analysis to determine the optimal combination of pre-diagnostic biomarkers and quantify their contribution to the risk of developing CRC; and lastly (iii) a classification model to determine the combination of diagnostic features that can classify CRC cases from healthy participants with high accuracy. Survival analysis focused on incident cases of CRC and used Cox proportional hazards regression to model multivariate associations. The classification model used the GPBoost algorithm, which combines mixed effects models with tree-boosting, and focused on prevalent cases. With these two methods, we aimed to identify biomarker combinations sensitive to diagnostic and clinical CRC.
Methods
UK Biobank study
UK Biobank is a large scale, population-based cohort aged 40–69 years, recruited between 2006 and 2010 across 22 UK-based assessment centres, and aiming to follow up for 20 years19. The dataset comprises sociodemographic, psychosocial, lifestyle, family history, clinical, physical, cognitive, activity monitoring, biochemical, imaging, health linkage to a wide range of electronic healthcare records, and genomics data from over 500,000 participants.
At the baseline visit, a touchscreen questionnaire and a computer assisted interview were completed. Physical and functional measures, and blood, urine and saliva samples were collected. The baseline assessments were repeated on a smaller subset of the cohort (20,000–25,000 participants). The time lag between visits was approximately 4 years on average (range: 1–10 years).
All participants were registered in the UK National Health Service. Cancer outcomes were taken from electronic healthcare records, hospital episodes statistics, the National Cancer Registry, self-reports validated by the study nurse and death certification data. Outcomes were coded using the International Classification of Diseases 10th revision (ICD-10) system. The UK Biobank study was approved by the North West—Haydock Research Ethics Committee (21/NW/0157), all experiments were performed in accordance with relevant guidelines and regulations. Participants provided informed consent for the storage and use of their data by bona fide researchers undertaking health research for public good.
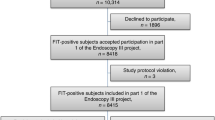
Participants
Initial sample size was 502,411 participants. 387,773 participants (77.2%) were healthy controls (HC), defined as those who have not received a cancer diagnosis before or during the study. To define the CRC group, we used ICD-10 codes for malignant neoplasm of colon including caecum, appendix, ascending colon, hepatic flexure, transverse colon, splenic flexure, descending colon, sigmoid colon, overlapping lesion of colon, and colon unspecified (C18.0–9), rectosigmoid junction (C19) and rectum (C20). There were 2,317 participants with CRC at baseline (0.46%), and 6,237 incident cases (1.24%) on follow-up visits. Among incident cases, 6,116 (98%) were diagnosed after their last study visit.
Measures
We included 72 sociodemographic, physical, medical, lifestyle and biochemical measurements in our analysis. Cancer-related variables were only used to describe the patient population and were not used as predictors in the analyses.
Sociodemographic measures
Age at screening visit, sex, ethnicity, Townsend deprivation index as an index of socioeconomic status, and highest education qualification.
Physical measures
Height, body mass index (BMI), pulse, diastolic and systolic blood pressure (BP), waist-to-hip ratio, trunk-to-leg fat ratio, metabolic rate, impedance, grip strength of the dominant hand, and self-reported sleep duration in hours.
Medical history
Family history of cancer and CRC, disease history for inflammatory bowel disease (IBD), cardiovascular disease (CVD), liver and biliary disease, diabetes, self-reported overall health rating (on a scale of 1 to 4 from Excellent to Poor), and regular aspirin and statin use.
Lifestyle
Smoking and alcohol consumption frequency, intake frequency of oily fish, processed and red meat, summed metabolic equivalent task (MET) minutes per week for all activity based on International Physical Activity Questionnaire.
Full blood count (FBC) and biochemistry
Biochemical measures were assessed in serum and urine. Serum markers consisted of white blood cell (WBC) count, red blood cell (RBC) count, hemoglobin concentration, hematocrit percentage, platelet count, lymphocyte percentage, apolipoprotein A and B, urea, cholesterol, C-reactive protein (CRP), cystatin C, high density lipoprotein, insulin-like growth factor 1 (IGF-1), low density lipoprotein, sex hormone binding globulin (SHBG), testosterone, total protein, triglycerides, vitamin D, mean corpuscular volume, percentages of monocytes, neutrophils, eosinophils, basophils, nucleated RBCs, and reticulocytes, albumin, alkaline phosphatase (ALP), alanine aminotransferase (ALT), aspartate aminotransferase (AST), direct bilirubin, calcium, gamma glutamyltransferase (GGT), glucose, glycated hemoglobin A1C (HbA1C), phosphate, total bilirubin and urate. An additional measure was included in the models as a covariate to indicate whether the participant fasted before the blood draw. Markers assessed in urine were creatinine, potassium, and sodium.
Cancer related variables
Age at cancer diagnosis, cancer site, behaviour of the cancer tumour, distinct diagnoses of cancer, and whether the participant had been previously screened for CRC.
Pre-processing
All preprocessing and data analysis steps (Fig. 1) were carried out with Python 3. Participants whose consent date was not available (N = 2), who withdrew consent (N = 158), who had other primary cancers (N = 105,924) or concurrent cancers (N = 1,458) were excluded. We removed outliers outside the 0.1th and 0.99th percentiles. To simplify interpretation of results, ethnicity was re-coded into white and non-white, and education level as university and non-university. Summed MET minutes was binned into 5 quintiles. To maximise available data in the following analyses, we opted for methods that can handle sparse data when possible, and coded missing data in categorical measures as an ‘unknown’ category. We performed group comparisons on baseline data using two-tailed chi-square tests and between samples t-tests and corrected for multiple comparisons using the false discovery rate. Analysis-specific pre-processing steps are given in respective sections.
Time-to-event analysis
We used Cox regression model to assess the effect of the above biomarkers on the age of diagnosis and associated risk for CRC using the Lifelines package20. In addition to the filtering steps explained in pre-processing, we removed participants who developed any cancer prior to recruitment (N = 6740). All participants were followed until the censoring date, 29th February 2020. We calculated survival based on participant’s age. Covariates used in the model were measures from the initial screening visit. Since Cox regression does not handle missing data, rows with missing values were removed.
A data-driven approach was adopted to find the optimal set of covariates to model in Cox regression. We first split the dataset into 80% training and 20% test sets, stratified by label. We ran a forward feature selection, where each covariate was univariately fitted to the dataset, and any covariates that exceeded P > 0.10 were removed from the list of features. We then tested for multicollinearity in the dataset by calculating variance inflation factors (VIF) and removed any covariate exceeding VIF > 10. Finally, we used backward feature elimination where we initially modelled all the remaining variables, then iteratively removed the variable with highest non-significance at P > 0.05, until all covariates in the model were significant. The final model was then evaluated with the test set. We report the concordance index (C-index) for both training and test sets, as an index of model’s performance.
Classification analysis
We used Python implementation of GPBoost which combines powerful tree-boosting algorithms with mixed effects models—which are commonly used when working with grouped data21,22, to classify CRC vs HC using both baseline and repeat visits (where available). The tree-boosting part utilises LightGBM, a highly efficient type of gradient boosting decision tree, which handles missing values and works with categorical variables23.
Here we used the same feature processing and outlier removal procedures as before. Unlike the survival analysis, we included both prevalent and incident cases, and retained incomplete rows. We assigned a binary label for CRC to each study visit of a participant based on whether they had developed CRC at the time of the visit. We first split the dataset into 80% training and 20% test sets, and then split the training set into 5 cross-validation (CV) folds for feature selection experiments. We evaluated the performance of the final model using Area Under the Receiver Operating Characteristic Curve (AUC-ROC).
To determine the number of features, we implemented Recursive Feature Elimination (RFE)24. RFE is a wrapper type of feature selection algorithm, which recursively prunes the least ‘important’ features until the desired number of features is reached. In order to find a cost-effective biomarker combination, we performed a grid search with a maximum of 5 features, using gain-based feature importance provided by our model. The optimal number of features (Nfeatures) was then selected as the number of features which achieved the highest score in fivefold CV. We also calculated feature importance values for each split, normalised by the total importance, and aggregated by mean across splits. We generated partial dependence plots (PDP) to assess the dependency of predicted CRC probability on each feature.
Results
Sample characteristics at baseline
Group comparison results of sociodemographic, medical history and key lifestyle measures are given in Table 1. Across sociodemographic measures, two groups had significantly different ages and sex. CRC group was significantly older and had a higher percentage of males than the controls. There were no significant differences on ethnicity, education level and socioeconomic status measured by the Townsend Deprivation Index. Most of the participants on both groups were white and had tertiary education as their highest qualification. Both groups had a negative mean score of Townsend Deprivation Index, indicating relative affluence in each group relative to the general population.
Two groups further differed in their disease history. Compared to controls, the CRC group had a significantly greater odds of having a family history for cancer and CRC and disease history of CVD. This effect was especially high for the family history of CRC, where incidence in CRC group was twice the incidence in controls. The CRC group also had a higher proportion of individuals who have been previously screened for CRC. CRC patients rated their health significantly lower on the self-reported health rating compared to controls. Groups did not show any difference in their diet and lifestyle measurements. There was no significant effect of the study centre (X2(21) = 2.824; P = 1.000).
We further explored cancer-related measures in the CRC group. Mean age of diagnosis was 55.9 years (SD = 8.04) with a negatively skewed distribution. Throughout the duration of the cancer registry data, 65.9% of CRC group had one, 25.4% had two and 9% had three or more distinct cancer diagnoses. For almost all (99.8%), the tumour was of malignant type in the primary cancer site. Among CRC patients, 4.79% had also developed breast cancer, 2.11% lung cancer, 1.24% non-Hodgkin’s lymphoma, 1.01% prostate cancer and 0.29% liver cancer.
Finally, we compared the physical and biochemical biomarkers across groups. All continuous biomarkers, except for RBC, nucleated RBC, ALT, diastolic BP, IGF-1, grip strength, vitamin D, haematocrit, apolipoprotein A and B, calcium and haemoglobin were significant at the corrected level (Pcor < 0.05). Detailed results are given in Supplementary Fig. S1.
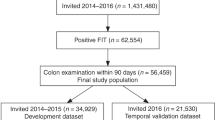
Cox proportional hazard model
In the initial feature selection step, we removed the following features which were above the P < 0.10 threshold: Townsend deprivation score, ethnicity, platelets, apolipoprotein B, low density lipoprotein, total protein, systolic BP, statin use, disease history for CVD, IBD, liver-biliary disease and diabetes, education level, sleep duration, mean corpuscular volume, neutrophils, eosinophils, nucleated RBCs, albumin, ALP, AST, glucose, HbA1C, and phosphate. Figure 2 shows the hazard ratios and the clustering of the features that remained after the feature selection step. Next, we removed intercorrelated variables that showed a VIF > 10. These variables were hematocrit percentage, direct bilirubin, apolipoprotein A, testosterone, impedance, metabolic rate, and height.
Risk profile and relationships between features that remained in the set after the initial forward selection step. Plot on the left shows univariate log hazard ratios and standard error of each variable. Log hazard ratios above 0 indicate an increased risk for CRC. Whereas values below 0 indicate a decreased risk (i.e., protective effect) for CRC. Dendrogram on the right displays the relationships between variables calculated as the Ward distance of the pairwise intercorrelations. The distance reflects the similarity between variables, where smaller the distance more similar the variables are. For instance, direct bilirubin and total bilirubin are very similar and form their own cluster. From top to bottom biomarkers formed the adiposity and cholesterol (red), hepatic and cardiovascular (dark orange), urine (orange), sex and RBC (yellow), cancer promoting factors and cholesterol (green), lifestyle (teal), immune system (blue), renal function (navy), and liver-biliary clusters (purple).
In the final backward elimination step, we removed variables not significantly contributing to the model: RBC count, grip strength, calcium, trunk-to-leg fat ratio, sodium, creatinine and potassium in urine, lymphocytes, cystatin C, urate, self-reported health rating, high density lipoprotein, oily fish and red meat intake, WBC count, monocytes, hemoglobin, total bilirubin, fasting status, diastolic BP, vitamin D, reticulocytes, CRP, MET minutes, GGT, IGF-1, BMI, regular aspirin use, and smoking. With backward elimination, we reduced the partial Akaike information criterion of the model from 39,044.14 to 39,006.05, whereas the C-index only marginally reduced from 0.696 to 0.690.
The final model (Fig. 3A) included the following risk factors as strongest predictors for developing CRC: higher waist-to-hip ratio (491% increase), intake of 5–7 units of alcohol pw (63% increase), being male (32% increase) (Fig. 3B) and having family history of cancer (29% increase) (Table 2). Having higher basophil percentage (10% increase), higher triglycerides (8% increase), higher pulse (1% increase), and higher SHBG (0.3% increase) increased the risk for CRC. Whereas having higher urea (7% decrease), higher total cholesterol (6% decrease), and higher ALT (0.4% decrease) decreased the risk for CRC, suggesting that these might be protective factors against the disease. Younger age at recruitment was associated with a higher risk for CRC, where age at recruitment and at diagnosis showed a high positive correlation (r = 0.90). The final model’s C-indices were 0.690 and 0.681 for the training and test sets respectively. As this final model included serum lipids, we ran the model again by including the fasting status. However, the fasting status was not significant and did not affect the results of other predictors. For completeness and comparison in the Supplementary Table S1 we report the unadjusted hazard ratios when the predictors of the final model were fitted to the data in a univariate fashion.
(A) Results of time-to-event analysis showing log hazard ratios and standard error of each variable included in the final optimal model. Log hazard ratios above 0 indicate an increased risk for CRC. Whereas values below 0 indicate a decreased risk (i.e., protective effect) for CRC. (B) Partial effects plots for the top 3 risk factors given the model, y axis displaying the proportion of participants who did not develop CRC. Note that the rate of decline in proportion of healthy individuals is faster for participants with waist-to-hip ratio of 1.2, those who drink 5–7 units of alcohol per week and males. CI confidence interval, HR hazard ratio, pm per month, pw per week, u units.
Classification analysis
In fivefold CV experiments with RFE, Nfeatures of 5 achieved the highest mean AUC score of 0.744. The mean AUC decreased as the number of selected features decreased (0.742 for Nfeatures = 4, 0.734 for Nfeatures = 3, 0.717 for Nfeatures = 2, and 0.690 for Nfeatures = 1) (Fig. 4B). Feature ranking by gain-based importance for the top 20 features is shown in Fig. 4A for the fivefold CV experiments. On average, age had the highest importance score (M = 0.354; SD = 0.014), followed by self-reported overall health rating (M = 0.094; SD = 0.010), ALP (M = 0.043; SD = 0.007), WBC count (M = 0.041; SD = 0.012), lymphocyte percentage (M = 0.040; SD = 0.017), family history of cancer (M = 0.028; SD = 0.011), urine creatinine (M = 0.023; SD = 0.014), trunk-to-leg ratio (M = 0.022; SD = 0.007), urine potassium (M = 0.018; SD = 0.005), and platelet count (M = 0.016; SD = 0.012). Hence, age, self-reported health rating, ALP, WBC count, and lymphocyte percentage were selected as the final feature set.
Classification results. (A) Feature ranking by gain-based importance obtained from tree-boosting random effects model, showing top 20 features. Feature importance values were calculated for each split of the fivefold cross-validation. For each feature, a boxplot is provided showing distribution of normalised importance across runs. (B) Fivefold cross-validation results in AUC-ROC for tree-boosting model with number of selected features from 1 to 5 using Recursive Feature Elimination (RFE). (C) ROC curve for tree-boosting random effects model on the test set with AUC score.
The ROC curve is provided in Fig. 4C for the final tree-boosting with random effects model refitted on the whole training set, using only the selected combination of features as well as all available features. The model achieved an AUC score of 0.763 and 0.773 respectively on the test set. At the threshold maximizing sensitivity and specificity equally, the model with the selected combination of features achieved a sensitivity of 0.718 and a specificity of 0.690. PDPs showing marginal contribution of each feature on CRC probability are provided in Supplementary Fig. S2.
Discussion
In this study, we opted to take a two-pronged, data-driven approach to identify pre-diagnostic and diagnostic biomarkers for detecting CRC. The principal result of our study is that in addition to modifiable lifestyle factors of obesity, alcohol consumption and cardiovascular health, blood-based biomarkers that capture WBC activity, lipid profile, liver and kidney function are informative of CRC, at both pre-clinical and clinical stages.
Among blood-based biomarkers we found those measuring lipid metabolism, liver function and immune response to be also sensitive to CRC. We showed that a lipid profile of high triglycerides and low cholesterol to be indicative of diagnostic CRC. Elevated triglycerides have been previously linked to CRC25, whereas the exact role of cholesterol in CRC is contested. Some studies report a positive association between serum cholesterol and CRC risk26 and beneficial effect of long-term statin use27. Supporting current findings, others reported that low cholesterol increases the risk17, almost by 2-folds28. This inverse relationship can be due to the high energy demanded by cancer cells for proliferation, which is satisfied by increased uptake of the exogenous cholesterol29, or alternatively by deregulations of its metabolic pathway due to genetic alterations30.
Imbalances in ALT and ALP, markers of liver dysfunction, are often linked to non-cancer factors like liver injury due to statin use, obesity, diet31, high alcohol intake32, and smoking33. However, they also relate to the cancers of digestive organs including CRC33 and liver metastases15,16. Our analysis showed an association between elevated levels of ALP and CRC, particularly above 100 U/L. Although this might imply liver metastasis, only a subset of our CRC cases had liver cancer, suggesting that liver markers may have a diagnostic value in the early stages of CRC. Further, the survival analysis highlighted a reduction in ALT in CRC. Lower ALT is linked to oxidative stress34, having invasive cancer cells35, poorer prognosis and mortality36. Therefore, ALP/ALT ratio can be an informative liver function marker in CRC.
Among the immunity markers, we observed strong associations for basophil and lymphocyte percentage and WBC count. Basophils showed a modest, positive link to CRC risk, which might suggest a diagnostic inflammatory response to cancer37. Lymphocytes play an important role in body’s immune response against cancerous cells and lower levels were found to be associated with greater likelihood of CRC38. However, the negative association we observed for WBC differed from previous findings13,14. This could be explained by chemotherapy-related WBC reduction, previously reported for multiple cancers including CRC39.
Waist-to-hip ratio and alcohol intake were the strongest modifiable lifestyle risk factors, with one unit increase in waist-to-hip ratio increasing the CRC risk by nearly 500%. The association is supported by previous studies40, and retained even when the model was adjusted for BMI, confirming that the association is due to visceral fat but not obesity41. High alcohol intake leads both to higher visceral fat and CRC42. We found that compared to non-drinkers, moderate-to-heavy drinking increased the hazard by 62% in a dose-dependent fashion, such that highest risk was observed for highest consumers. Although not significant, there were a higher percentage of former and moderate-to-heavy drinkers in the CRC group. Concordantly, previous work suggested that while moderate and heavy drinking was associated with increased risk, light consumption was not43. Visceral adiposity and high alcohol intake may promote carcinogenesis via hyperinsulinemia, elevated oxidative stress and inflammation pathways44.
Sex is a prominent determinant in CRC development. Here we report over 30% increased risk in men. There are more men who develop CRC than women, 84.5 versus 56.5 per 100,000, and higher mortality in men in the UK3. This susceptibility may be due to behavioural and biological factors45. Men have a higher red meat intake46, alcohol consumption47, and tendency to deposit visceral fat48, all being significant risk factors. Sex hormones might also contribute to the sex-related differences in risk. We found a modest positive association between CRC risk and SHBG, a glycoprotein responsible for transporting sex hormones estrogen and testosterone. Higher levels of SHBG would lead to lower levels of circulating free testosterone and estrogen which are protective against CRC49.
Finally, we report family history of cancer, higher pulse, lower urea and poor health rating as other significant contributors to CRC risk. History of cancer amplified CRC risk by 29%. CRC group had a higher incidence of family history with CRC (OR = 2.03) and cancer (OR = 1.34). First degree relatives of CRC patients have a higher risk for overall cancer, mainly CRC, thyroid, and stomach50. The risk of getting colon cancer in a first-degree relative was 2.2, which drops to 1.3 and 1.2 in second and third-degree relatives51, suggesting a strong familial genetic component. Whereas pulse and urea had minor contributions to the risk, emphasizing the modest but key role of cardiovascular52 and renal health53 in CRC development53. Finally, self-reported poor health was a strong classifying feature, previously linked to overall cancer risk and all-cause mortality54,55. While these biomarkers may not be necessarily specific to CRC on their own, when combined they can yield a higher specificity.
ML models can detect subtle changes and non-linear relationships in biomarkers, which may not be directly evident to clinicians. However, only a limited number of ML studies have investigated the use of routinely collected, longitudinal clinical data in detecting CRC. There is notable work that extracted blood test results from electronic healthcare records and used ML methods to identify patients at risk of CRC or with CRC56,57. The former study used a predictive algorithm involving an ensemble of random forest and gradient boosting to estimate the risk of developing CRC (AUC = 0.82). The latter evaluated five ML models, including logistic regression, naïve Bayes and support vector machines, alongside feature selection to identify the best model and features for distinguishing CRC from healthy (AUC = 0.85). Similarly, in the current study, we show the utility of ML applications in healthcare, and their potential to improve diagnostics when combined with other powerful statistical methods.
CRC has an immense economic burden on the healthcare system. Direct and indirect costs in the UK constitute £314 m and £1.4bn respectively58. These costs can be drastically reduced with the help of improved diagnostic tools, and increased uptake of screening programmes. Current screening in the UK involves FIT (£4 per kit)59, and a follow-up colonoscopy (£465 pp)60. Reducing the false negative rate of FIT by combining it with blood-based biomarkers sensitive to CRC, may increase its diagnostic accuracy and help reduce the long-term economic burden. Blood-based biomarkers offer key advantages: they are routinely collected laboratory tests, and their results are available at low or no additional cost. This would allow clinicians to interpret the FIT with readily available blood test results, and subsequently stratify and triage patients.
Our study had several strengths and limitations. We have opted to take a two-pronged data-driven approach that used survival analysis to determine the pre-diagnostic variables associated with developing CRC throughout the course of the study, and tree-boosting model to determine the clinical features that can classify CRC. We opted for methods that maximally utilize the available data and tested all available variables in our dataset. In order to find the optimal combination of biomarkers both in the survival analysis and in the GPBoost model, we adopted feature selection methods widely used in ML. The study and analyses were planned retrospectively based on the data and participants available in the UK Biobank study. Due to the large sample size of the study, CRC group was well-represented. However, our analyses were limited by the measurements collected in the study which were not specific to cancer. Biochemistry measures did not include other widely used diagnostic measures of cancer such as CEA and FIT. Therefore, we are not able to quantify the additive value of the blood-based biomarkers we report in this study to other CRC screening tools.
In conclusion, in the current study, we used Cox regression to identify key biomarkers that can predict CRC risk from baseline measurements and thus can be used for early detection of disease, and a tree-boosting classification model to identify biomarkers that can distinguish between healthy and CRC states. We provide novel evidence that blood-based biomarkers collected in routine blood examinations, capturing immune response, lipid profile, liver and kidney function are informative of preclinical and clinical CRC. These blood-based biomarkers can provide an additive value to the current, widely used CRC diagnostic tools, to help improve their diagnostic accuracy, increase uptake, and allow earlier disease detection.
Data availability
Approval for the study and permission to access the data was granted by the UK Biobank Resource. UK Biobank is an open access resource and bona fide researchers can access the UK Biobank dataset by registering and applying at https://www.ukbiobank.ac.uk/enable-your-research/apply-for-access.
Code availability
Code for the analysis will be made available on GitHub at https://github.com/sanometech/ukbiobank-crc/.
References
Caul, S., & Broggio, J. Cancer registration statistics, England: 2017 [Internet]. 2019 Apr [cited 2022 Oct 6]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/cancerregistrationstatisticsengland/2017#:~:text=In%202017%2C%20the%20number%20of,%25)%20and%20females%20(63.3%25).
John, S., & Broggio, J. Cancer survival in England: national estimates for patients followed up to 2017 [Internet]. 2019 Jan [cited 2022 Oct 6]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/cancersurvivalinengland/nationalestimatesforpatientsfollowedupto2017.
Cancer Research UK. Bowel cancer incidence statistics [Internet]. 2021 [cited 2022 Oct 17]. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer/incidence.
Vatandoust, S., Price, T. J. & Karapetis, C. S. Colorectal cancer: Metastases to a single organ. World J. Gastroenterol. 21(41), 11767–11776 (2015).
Kuipers, E. J. et al. Colorectal cancer. Nat. Rev. Dis. Primers. 1(1), 15065 (2015).
Joranger, P. et al. Survival and costs of colorectal cancer treatment and effects of changing treatment strategies: A model approach. Eur. J. Heal. Econ. 21(3), 321–334 (2020).
Lee, J. K., Liles, E. G., Bent, S., Levin, T. R. & Corley, D. A. Accuracy of fecal immunochemical tests for colorectal cancer: Systematic review and meta-analysis. Ann. Intern. Med. 160(3), 171–181 (2014).
Imperiale, T. F. et al. Multitarget stool DNA testing for colorectal-cancer screening. N. Engl. J. Med. 370(14), 1287–1297 (2014).
Delisle, T. G. et al. Faecal immunochemical test for suspected colorectal cancer symptoms: Patient survey of usability and acceptability. BJGP Open. 6(1), 102 (2022).
Liles, E. G. et al. Uptake of a colorectal cancer screening blood test is higher than of a fecal test offered in clinic: A randomized trial. Cancer Treat Res. Commun. 10, 27–31 (2017).
Hauptman, N. & Glavač, D. Colorectal cancer blood-based biomarkers. Gastroent. Res. Pract. 2017, 2195361 (2017).
Tuomisto, A. E., Mäkinen, M. J. & Väyrynen, J. P. Systemic inflammation in colorectal cancer: Underlying factors, effects, and prognostic significance. World J. Gastroenterol. 25(31), 4383–4404 (2019).
Virdee, P. S. et al. The full blood count blood test for colorectal cancer detection: A systematic review, meta-analysis, and critical appraisal. Cancers 12(9), 2348 (2020).
Lee, Y. J., Lee, H. R., Nam, C. M., Hwang, U. K. & Jee, S. H. White blood cell count and the risk of colon cancer. Yonsei Med. J. 47(5), 646–656 (2006).
Saif, M. W., Alexander, D., & Wicox, C. M. Serum alkaline phosphatase level as a prognostic tool in colorectal cancer: A study of 105 patients—PMC. J. Appl. Res. [Internet]. 2005; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2741323/.
Wu, X. Z., Ma, F. & Wang, X. L. Serological diagnostic factors for liver metastasis in patients with colorectal cancer. World J. Gastroenterol. 16(32), 4084–4088 (2010).
van Duijnhoven, F. J. B. et al. Blood lipid and lipoprotein concentrations and colorectal cancer risk in the European Prospective Investigation into Cancer and Nutrition. Gut 60(8), 1094 (2011).
Moullet, M. et al. Pre-diagnostic clinical features and blood tests in patients with colorectal cancer: A retrospective linked data study. Br. J. Gen. Pract. 72(721), 563 (2022).
Sudlow, C. et al. UK Biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. Plos Med. 12(3), e1001779 (2015).
Davidson-Pilon, C. Lifelines: Survival analysis in Python. J. Open Source Softw. 4(40), 1317 (2019).
Sigrist, F. Latent Gaussian model boosting. IEEE T Pattern Anal. 2, 1894–1905 (2022).
Sigrist, F. Gaussian Process Boosting. arXiv [Internet]. 2020; Available from: https://doi.org/10.48550/arXiv.2004.02653.
Ke, G., Meng, Q., Finley, T., Wang, T., Chen, W., Ma, W., et al. LightGBM: A Highly Efficient Gradient Boosting Decision Tree. In: NeurIPS Proceedings [Internet]. 2017 [cited 2022 Sep 14]. Available from: https://papers.nips.cc/paper/2017/hash/6449f44a102fde848669bdd9eb6b76fa-Abstract.html.
Pedregosa, F. et al. Scikit learn: Machine learning in Python. J. Mach. Learn. Res. 1(12), 2825–2830 (2011).
Otake, S. et al. Decreased levels of plasma adiponectin associated with increased risk of colorectal cancer. World J. Gastroenterol. 16(10), 1252–1257 (2010).
Yang, M. H. et al. The association of serum lipids with colorectal adenomas. Am. J. Gastroenterol. 108(5), 833–841 (2013).
Poynter, J. N. et al. Statins and the risk of colorectal cancer. N. Engl. J. Med. 352(21), 2184–2192 (2005).
Mamtani, R. et al. Disentangling the association between statins, cholesterol, and colorectal cancer: A nested case-control study. J. Clin. Oncol. 34(15 suppl), 3609–3609 (2016).
Giacomini, I. et al. Cholesterol metabolic reprogramming in cancer and its pharmacological modulation as therapeutic strategy. Front. Oncol. 11, 682911 (2021).
Silvente-Poirot, S. & Poirot, M. Cholesterol and cancer, in the balance. Science 343(6178), 1445–1446 (2014).
Green, D. M. et al. Serum alanine aminotransferase elevations in survivors of childhood cancer: A report from the St Jude lifetime cohort study. Hepatology 69(1), 94–106 (2019).
Mulder, R. L. et al. Surveillance of hepatic late adverse effects in a large cohort of long-term survivors of childhood cancer: Prevalence and risk factors. Eur. J. Cancer. 49(1), 185–193 (2013).
Kunutsor, S. K., Apekey, T. A., Hemelrijck, M. V., Calori, G. & Perseghin, G. Gamma glutamyltransferase, alanine aminotransferase and risk of cancer: Systematic review and meta-analysis. Int. J. Cancer. 136(5), 1162–1170 (2015).
Zoppini, G. et al. The aspartate aminotransferase-to-alanine aminotransferase ratio predicts all-cause and cardiovascular mortality in patients with type 2 diabetes. Medicine 95(43), e4821 (2016).
Kawamoto, R. et al. Alanine aminotransferase/aspartate aminotransferase ratio is the best surrogate marker for insulin resistance in non-obese Japanese adults. Cardiovasc. Diabetol. 11(1), 117–117 (2012).
Peltz-Sinvani, N. et al. Low ALT Levels independently associated with 22-year all-cause mortality among coronary heart disease patients. J. Gen. Intern. Med. 31(2), 209–214 (2015).
Bax, H. J. et al. Basophils from cancer patients respond to immune stimuli and predict clinical outcome. Cells 9(7), 1631 (2020).
Zhou, W. W., Chu, Y. P. & An, G. Y. Significant difference of neutrophil-lymphocyte ratio between colorectal cancer, adenomatous polyp and healthy people. Eur. Rev. Med. Pharm. 21(23), 5386–5391 (2017).
Wondimneh, B. et al. Comparison of hematological and biochemical profile changes in pre- and post-chemotherapy treatment of cancer patients attended at Ayder comprehensive specialized hospital, Mekelle, Northern Ethiopia 2019: A retrospective cohort study. Cancer Manag. Res. 13, 625–632 (2021).
Larsson, S. C. & Wolk, A. Obesity and colon and rectal cancer risk: A meta-analysis of prospective studies. Am. J. Clin. Nutr. 86(3), 556–565 (2007).
Song, M. et al. Long-term status and change of body fat distribution, and risk of colorectal cancer: a prospective cohort study. Int. J. Epidemiol. 45(3), 871–883 (2016).
Traversy, G. & Chaput, J. P. Alcohol consumption and obesity: An update. Curr. Obes. Rep. 4(1), 122–130 (2015).
Fedirko, V. et al. Alcohol drinking and colorectal cancer risk: An overall and dose–response meta-analysis of published studies. Ann. Oncol. 22(9), 1958–1972 (2011).
Jayasekara, H. et al. Associations of alcohol intake, smoking, physical activity and obesity with survival following colorectal cancer diagnosis by stage, anatomic site and tumor molecular subtype. Int. J. Cancer. 142(2), 238–250 (2018).
White, A. et al. A review of sex-related differences in colorectal cancer incidence, screening uptake, routes to diagnosis, cancer stage and survival in the UK. BMC Cancer 18(1), 906 (2018).
Lombardo, M. et al. Gender differences in taste and foods habits. Nutr. Food Sci. 50(1), 229–239 (2019).
Schutze, M. et al. Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study. BMJ 342, d1584–d1584 (2011).
Tchernof, A. & Després, J. P. Pathophysiology of human visceral obesity: An update. Physiol. Rev. 93(1), 359–404 (2013).
Mørch, L. S., Lidegaard, Ø., Keiding, N., Løkkegaard, E. & Kjær, S. K. The influence of hormone therapies on colon and rectal cancer. Eur. J. Epidemiol. 31(5), 481–489 (2016).
Amundadottir, L. T. et al. Cancer as a complex phenotype: Pattern of cancer distribution within and beyond the nuclear family. Plos Med. 1(3), e65 (2004).
Teerlink, C. C., Albright, F. S., Lins, L. & Cannon-Albright, L. A. A comprehensive survey of cancer risks in extended families. Genet Med. 14(1), 107–114 (2012).
Anker, M. S. et al. Resting heart rate is an independent predictor of death in patients with colorectal, pancreatic, and non-small cell lung cancer: results of a prospective cardiovascular long-term study. Eur. J. Heart Fail. 18(12), 1524–1534 (2016).
Sun, Y. et al. Causal associations between serum urea and cancer: A mendelian randomization study. Genes-Basel. 12(4), 498 (2021).
Cancer Research UK. Bowel cancer statistics [Internet]. 2022 [cited 2022 Oct 10]. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer#heading-One.
Ganna, A. & Ingelsson, E. 5 year mortality predictors in 498 103 UK Biobank participants: A prospective population-based study. Lancet 386(9993), 533–540 (2015).
Kinar, Y. et al. Development and validation of a predictive model for detection of colorectal cancer in primary care by analysis of complete blood counts: A binational retrospective study. J. Am. Med. Inform. Assn. 23(5), 879–890 (2016).
Li, H. et al. Colorectal cancer detected by machine learning models using conventional laboratory test data. Technol. Cancer Res. T. 20, 15330338211058352 (2021).
Henderson, R. H. et al. The economic burden of colorectal cancer across Europe: A population-based cost-of-illness study. Lancet Gastroenterol. Hepatol. 6(9), 709–722 (2021).
Quantitative faecal immunochemical tests to guide referral for colorectal cancer in primary care [Internet]. National Institute for Health and Care Excellence; 2017 Jul [cited 2022 Oct 20]. Available from: https://www.nice.org.uk/guidance/dg30/resources/quantitative-faecal-immunochemical-tests-to-guide-referral-for-colorectal-cancer-in-primary-care-pdf-1053744003781.
Kearsey, C. et al. Cost effectiveness of using Faecal Immunochemical Testing (FIT) as an initial diagnostic investigation for patients with lower gastrointestinal symptoms suggestive of malignancy. BMC Fam. Pract. 22(1), 90 (2021).
Acknowledgements
This research has been conducted using the UK Biobank Resource under application number 87991 for the project titled ‘Validation of an AI-powered online search strategy for finding optimal biomarker combinations’. UK Biobank study was primarily funded by the Wellcome Trust and the Medical Research Council. Authors received no specific funding for this work. We thank the UK Biobank participants and researchers who built the UK Biobank Resource.
Author information
Authors and Affiliations
Contributions
G.T. provided access to the data. G.T. and E.K. jointly performed data preprocessing and data analysis. E.K. performed statistics and survival analysis. G.T. performed the GPBoost analysis. Authors jointly interpreted the findings, wrote, revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tanriver, G., Kocagoncu, E. Additive pre-diagnostic and diagnostic value of routine blood-based biomarkers in the detection of colorectal cancer in the UK Biobank cohort. Sci Rep 13, 1367 (2023). https://doi.org/10.1038/s41598-023-28631-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-28631-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.