Abstract
The impact of the adherence to the adjunctive use criteria (AUC) for intravascular ultrasound (IVUS) guided percutaneous coronary intervention (PCI) and clinical outcomes in low IVUS volume countries are limited. The current study compared the procedural success and complication rates between used and not used IVUS catheter in the patients who were met (C +) and were not met (C−) the AUC for IVUS-guided PCI. From June 2018 through June 2019, a total of 21,066 patients were included in the Thai PCI registry. Among the study population, 15,966 patients (75.8%) have met the IVUS-AUC. The IVUS-guided PCI rates were 14.5% and 11.3% in the C + and C − groups, respectively. After adjusting for covariables by propensity model, IVUS-guided PCI was identified as an independent predictor of the procedural success rate regardless of whether the AUC were met with the relative risk [RR (95% confidence interval (CI)] of 1.033(1.026–1.040) and 1.012(1.002–1.021) in C + and C− groups, respectively. IVUS-guided PCI increased the procedural complication risks in both groups but were not significant with corresponding RRs of 1.171(0.915–1.426) and 1.693(0.959–2.426). Procedural success was achieved with IVUS-guided PCI regardless of whether the AUC were met. IVUS-guided PCI did not lead to an increase in procedural complications.
Similar content being viewed by others
Introduction
Angiography-guided percutaneous coronary intervention (PCI) has been used in clinical practice for many decades. In the modern era, the benefits of intracoronary imaging in reducing cardiac death, target vessel myocardial infarction (MI), and target vessel revascularization have been repeatedly demonstrated in randomized controlled trials1,2 and meta-analyses3,4,5,6. However, the penetrance of intracoronary imaging-guided PCI in real-world practice remains low. The use of intracoronary imaging-guided PCI, especially intravascular ultrasound (IVUS), is most common in Japan (75.0–84.8%)7,8, followed by Korea (27.5–27.9%)9,10 and Germany (16.2%)11, while the USA12,13 and Italy14 have rates of around 5%. Despite the huge disparities in IVUS utilization among countries, associations between IVUS-guided PCI and low rates of long-term mortality8 and repeat revascularization7,10,12,13 have been reported consistently.
A recent expert consensus document from the European Association of Percutaneous Cardiovascular Interventions (EAPCI)15 recommended consideration of the adjunctive use of intravascular imaging for PCI guidance in patients with long lesions, chronic total occlusion (CTO), acute coronary syndrome (ACS), left main disease, two-stent bifurcation, implantation of bioresorbable scaffolds, or renal dysfunction. The consensus was derived from the published data that prespecified the used of IVUS-guided PCI in complex lesions10,16,17,18 or patients with complex clinical setting such as renal dysfunction or ACS19,20,21. In addition, some IVUS-guided PCI trials had pre-defined criteria for stent optimization in IVUS-guided PCI arm22,23. Recently, patients-level analysis from 2 randomized trials6 (IVUS-XPL [Impact of Intravascular Ultrasound Guidance on the Outcomes of Xience Prime Stents in Long Lesions]17 and ULTIMATE [Intravascular Ultrasound Guided Drug Eluting Stents Implantation in All-Comers Coronary Lesions])1 showed that IVUS-guided PCI in patients with long lesions with stent length ≥ 28 mm improved 3-year patients cardiac survival6. However, the impact of the adherence to the adjunctive use criteria (AUC) for IVUS on PCI guidance and clinical outcomes remains controversial. The present study was performed to investigate the IVUS procedural success and complication rates according to adherence to the AUC of IVUS in real-world clinical practice.
Methods
Study population
The Thai PCI Registry is a prospective, multi-centre study initiative project of the Cardiac Intervention Association of Thailand. The study design and protocol of the Thai PCI registry were described previously24,25. Briefly, the study was conducted at 39 centres in Thailand. All consecutive patients undergoing PCI who were aged 18 years or older were enrolled. Written informed consent was obtained from all patients. The details regarding the patient characteristics, procedural information, equipment, and outcomes of PCI were prospectively collected in each participating centre and recorded in electronic case record forms.
The Thai PCI registry was conducted in accordance with the Declaration of Helsinki and the Ethical Guidelines for Human Study. The protocol was approved by the Central Research Ethics Committee of Thailand (approval no. COA-CREC 006/2018) and the local ethics committee if required.
Adjunctive use of IVUS criteria
The adjunctive use of IVUS criteria were modified from the EAPCI expert consensus document15 as follows: long lesions (lesion length > 30 mm), CTO, left main disease, true bifurcation lesion with Medina classification 1,1,1/ 0,1,1/ 1,0,1 and number of stent use of 2 or more, in-stent restenosis, stent thrombosis, renal dysfunction (glomerular filtration rate [GFR] < 60 ml/min), and ACS receiving PCI within 1 week after onset. Patients treated with balloon angioplasty or receiving PCI under optical coherence tomography (OCT) guidance were excluded from the analysis.
Patients who did and did not meet at least one of the adjunctive use criteria for IVUS were classified into the C + and C − groups, respectively. The patients in each group were further divided into the IVUS-guided PCI (I +) and angio-guided PCI (I-) groups according to the actual utilization of IVUS during the procedure. In patients with multi-vessel PCI, the lesion treated under IVUS guidance was selected as the representative lesion. In cases in which IVUS-guided PCI was performed in more than one lesion, the representative lesions were prioritized as follows: left main, CTO, bifurcation, long lesion, in-stent restenosis, and stent thrombosis.
Study endpoints
The primary endpoint was the procedural success rate, defined as achievement of < 30% residual stenosis of the target lesion as assessed by visual estimation and without in-hospital major adverse cardiac events (death, MI, target lesion revascularization, or stent thrombosis). The secondary endpoints were the procedural complication rate and 1-year all-cause mortality rate. Clinical follow-up was performed via hospital visits or telephone calls at 6 and 12 months.
Statistical analysis
All continuous variables are presented as the mean ± standard deviation (SD) or median and interquartile range as appropriate. The categorical variables are reported as frequencies and percentages. In the primary analysis, IVUS-guided (I +) or angio-guided PCI(I−) was evaluated according to the C+ or C− group. Clinical and procedural characteristics are summarized according to whether the adjunctive use criteria were met. Comparisons between groups were performed using the χ2 test or Fisher’s exact test for categorical variables and Student’s t test for continuous variables. A univariate and multivariate logistics regression were performed to evaluate the factor associated with procedural success, procedural complication, in-hospital mortality, and 1-year mortality rates in patients who met and unmet criteria.
Effect of IVUS guided-PCI on clinical outcomes was assessed using a propensity analysis by an inverse probability weighting and regression adjustment (IPWRA) stratify by C + /C− groups as follows: First, a propensity model was constructed applying a logit equation by fitting IVUS on variables might be associated with IVUS application and also the clinical outcome of interests26,27 including demographic data [i.e., age, sex, body mass index (BMI)], Clinical presentations (i.e., ST-elevation myocardial infarction, non ST-elevation myocardial infarction, chronic coronary syndrome), chronic total occlusion, previously treated lesions, co-morbidities (i.e., hypertension, diabetes, dyslipidemia, peripheral artery disease, prior-myocardial infarction, prior coronary artery bypass graft surgery, known coronary artery disease, chronic kidney disease, cerebrovascular disease), femoral access site, lesion complexity, total volume contrast, plaque modification, and bifurcation. Only significant variables were kept in the final propensity model. Balancing of these significant variables between IVUS and non-IVUS groups was checked. The propensity model was well specified if absolute weighted standardized mean differences of these significant variables did not exceed 0.228. Second, the outcome model was constructed weighted by propensity score estimated from the first step. A potential outcome mean (i.e., a risk) of outcome occurrence was estimated by IVUS groups. Average treatment effect or risk difference (RD) was then estimated by subtracting risks between IVUS-guided and angio-guided groups. Furthermore, relative risk (RR) was finally estimated by diving risk in IVUS-guided and angio-guided group.
All reported P-values are two-sided, and P < 0.05 was taken to indicate statistical significance. Statistical analyses were performed using STATA version 17 (Stata Corp., College Station, TX, USA).
Results
Baseline characteristics
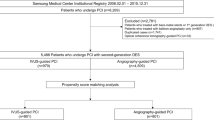
A total of 22,741 patients were enrolled in the Thai PCI registry with mean age of 64.2 years and percent male was 64.0%. Of these patients, 1,675 who were treated with balloon angioplasty or OCT for PCI guidance were excluded from the analysis (mean age of 64.7 years, male 66.4%). Finally, 21,066 patients were included in the study, of whom 15,966 (75.8%) met at least one adjunctive use criteria for IVUS (C + group), and 5,100 (24.2%) did not meet any of these criteria (C − group). IVUS-guided PCI (I + group) and angio-guided PCI (I- group) were performed in 14.5% and 85.6% of patients in the C + group and in 11.3% and 88.7% in the C − group, respectively. The study flow chart is presented in Fig. 1.
The baseline characteristics are shown in Table 1. The rates of hypertension, hyperlipidaemia, peripheral artery disease, and prior history of revascularization with either PCI or coronary artery bypass graft surgery were significantly higher in the patients group C + /I + than the group C + /I−. Conversely, patients presenting with ACS or cardiogenic shock were more likely to be treated with angio-guided PCI than IVUS-guided PCI. Potent P2Y12 inhibitors, such as prasugrel and ticagrelor, were prescribed at discharge more commonly in patients treated with IVUS-guided PCI.
The underlying medical conditions were comparable between the IVUS-guided and angio-guided PCI groups within the C − group, except for histories of prior PCI and MI, both of which had higher rates in the IVUS-guided group. Again, we found that potent P2Y12 inhibitors were used more frequently in patients treated with IVUS-guided PCI within the C − group.
Lesion and procedural characteristics
Table 2 summarizes the lesion and procedural characteristics of the patients according to the adjunctive use criteria for IVUS. The proportion of lesion class B2 or C was significantly higher in the IVUS-guided PCI group than in the angio-guided PCI group regardless of whether the AUC were met (C + /I + 88.8% vs. C + /I- 80.8%, P < 0.001; C − /I + : 79.9% vs. C–/I– 67.5%, P < 0.001). Of those patients who met the AUC, the percentage of each adjunctive use criterion is shown in Fig. 2. The top three most common lesion and clinical criteria were ACS (53.8%), renal dysfunction (42.4%), and long lesion (31.6%) (Fig. 2).
Distribution of the adjunctive use criteria for intravascular ultrasound among the patients who have met the criteria (C + group, n = 15,966). Abbreviations: ACS, acute coronary syndrome; IC, intravascular ultrasound adjunctive use criteria; PCI, percutaneous coronary intervention. Bifurcation lesions that were included in the C + group were true bifurcation lesion with Medina classification 1,1,1/ 0,1,1/ 1,0,1 and number of stent use of 2 or more.
Regardless of the presence of the AUC, femoral access was used more frequently during IVUS-guided PCI than angio-guided PCI. It was also noted that the frequency of using plaque modification procedures, either rotational atherectomy or cutting balloon, was significantly higher under IVUS guidance. IVUS-guided PCI was also related to greater contrast volume and longer fluoroscopic time compared with angio-guided PCI, these findings were observed in both C + and C− group.
Procedural success and complication rates
The procedural success and complication rates are summarized in Table 3. Procedural success rates were significantly higher in patients who met criteria and treated under IVUS-guided PCI than the angio-guided PCI (C + /I + : 98.1% vs. C + /I– 95.6%, P < 0.001). In contrast, procedural success rates in patients who did not meet criteria were comparable irrespective of the usage of imaging catheter (C − /I + : 98.6% vs. C–/I– 97.6%, P = 0.127). The procedures performed under IVUS guidance, versus angiography guidance, have led to a higher rate of procedural complications regardless of whether the AUC were met (C + /I + 6.4% vs. C + /I– 5.3%, P = 0.036; C-/I + 6.6% vs. C–/I– 2.7%, respectively, P < 0.001) (Table 3). The occurrence of coronary perforation was numerically higher in patients in the C + group who were treated with IVUS-guided PCI than with angio-guided PCI, but the difference was not statistically significant (0.6% vs. 0.4%, respectively, P = 0.079). In contrast, the rate of coronary perforation was significantly higher in patients in the C − group who were treated with IVUS-guided PCI than with angio-guided PCI (1.0% vs. 0.2%, respectively, P < 0.001). Residual dissection and infection were noted at significant rates in patients treated with IVUS-guided PCI regardless of whether the adjunctive use criteria were met. The rate of the no-reflow phenomenon was significantly higher in patients in the C − group who were treated with IVUS-guided PCI than with angio-guided PCI (1.0% vs. 0.2%, respectively, P < 0.001). In the C + group, the in-hospital mortality rate was significantly higher in patients who were treated with angio-guided PCI than with IVUS-guided PCI (3.2% vs. 2.3%, respectively, P = 0.016). Similarly, the 1-year mortality rate was significantly higher in patients in the C + group who were treated with angio-guided PCI than with IVUS-guided PCI (12.0% vs. 10.2%, respectively, P = 0.013). However, the in-hospital mortality and 1-year mortality rates in the C − group were comparable between patients treated with angio-guided PCI and IVUS-guided PCI.
The details of the univariate and multivariate analyses for each outcome model are presented in Supplementary Tables S1–S8. After adjusting for covariables, IVUS-guided PCI was identified as an independent predictor of the procedural success rate regardless of whether the criteria were met (OR 4.7, 95% CI 3.4–6.6, P < 0.001) or were not met (OR 2.7, 95% CI 1.3–5.7, P = 0.009). In addition, the IVUS-guided PCI was associated with a higher procedural complication rate in the C − group (adjusted OR 2.1, 95% CI 1.4–3.0, P < 0.001), but not in the C + group (adjusted OR 1.0, 95% CI 0.8–1.3, P = 0.74). IVUS-guided PCI was not related to the in-hospital mortality rate or 1-year mortality rate in either the C + or C − group.
The propensity score-adjusted
A propensity model was constructed to balance confounders between IVUS-guided PCI (I +) and angio-guided PCI (I−). The absolute standardized mean differences ranged from 0.058 to 0.594 and 0.260 to 0.637 in C + and C− groups, see Table S9. After weighting by propensity score, the absolute standardized weight mean differences of these corresponding groups ranged from 0.005 to 0.040 and 0.009 to 0.128 indicating well balance of these confounders between IVUS-guided PCI groups. In addition, density plots also indicated that distributions of each covariate were well balanced between I + and I− groups, see Fig. S1a,b. Furthermore, a positivity assumption was checked by overlapping plots, indicating the probabilities of I + and I− were very much overlapped, see Fig. S2a,b.
Risks, risk difference (RD), and relative risk (RR) along with 95% confidence intervals (CIs) of the primary and secondary endpoints were estimated based on propensity models in the C + and C − groups (Table 4 and Fig. 3). After adjusting for covariables by propensity model, IVUS-guided PCI was identified as an independent predictor of the procedural success rate regardless of whether the criteria were met and were not met with RRs (95% CI) of 1.033 (1.026, 1.040) and 1.012 (1.002, 1.021), respectively. IVUS-guided PCI was associated with procedural complication in both the C + /C− groups but none of them was significant with the RRs (95% CI) of 1.171 (0.915, 1.426) and 1.693 (0.959, 2.426), respectively. In addition, IVUS-guided PCI was related to lowering risks of the in-hospital mortality rate and 1-year mortality rate the C + with the RRs (95% CI) of 0.887 (0.598, 1.176) and 0.894 (0.750, 1.039), but none was significant. Conversely, IVUS-guided PCI in group C− was associated with higher risk of in-hospital death with the RR of 1.074 (0.001, 2.897), although this was not significant. Effects of IVUS-guided PCI on primary and secondary endpoints in patients who met and unmet criteria are summarized in the Fig. 4.
Discussion
The present study was performed to investigate the procedural success, complication, in-hospital mortality, and 1-year mortality rates when the adjunctive use criteria were applied for IVUS-guided PCI in real-world data. The main findings of the present study were as follows: despite no ceiling for IVUS catheter reimbursement in Thailand, the penetrance of IVUS catheters was low, as only 14.5% of patients who fulfilled the AUC were treated with IVUS-guided PCI. After propensity score adjustment, procedural success was achieved at a significantly high rate for IVUS-guided PCI regardless of whether the criteria were met. IVUS-guided PCI trended to increase procedural complication rates in patients who did and did not meet the AUC but both were not significant. IVUS-guided PCI seemed to lower the risk of short- or medium-term mortality rates if the criteria were met, but this did not reach statistical significance.
The present study demonstrated that the IVUS-guided PCI was around 10% of the overall population. The adoption rates of IVUS-guided PCI in the current study were slightly higher than those in previous reports from the United Kingdom and USA, where IVUS was used in 4.3%29 and 5.6%12 of cases, respectively. On the one hand, significant variation in IVUS use was noted according to the data from Japan, where IVUS was used in 84.8% of cases7. According to the practice survey by the EAPCI and the Japanese Association of Cardiovascular Interventions and Therapeutics in 2018, a high cost and prolonged procedure were the common reasons for limiting the use of intracoronary imaging in clinical practice30. The present study showed that IVUS-guided PCI had extended fluoroscopic time of around 10.9 and 12.3 min in patients who met and unmet the adjunct use criteria, respectively. Another possible reason for the low rates of IVUS-guided PCI in Thailand may be explained by the operators' familiarity with IVUS image interpretation. About 52% of the interventional cardiology fellows in the United States reported no or rudimentary education in IVUS31. In contrast, data from UK showed that the operators who graduated after year 2000 were almost 15-fold higher than the operator graduated before 1990 for using IVUS-guided PCI29. The findings reflected that adequate IVUS training would lead to an improvement in adoption of IVUS-guided PCI. Unfortunately, the Thailand PCI registry did not collect the data regarding operators’ experience, therefore, we could not demonstrate the association between the operator generation and the use of IVUS- guided PCI.
In view of procedural complication, the current study showed that IVUS-guided PCI increased the procedural complication risks in both groups but were not significant from propensity analysis. Previously, data from Japan showed that IVUS has reduced the risk of flow impairing severe coronary dissection7 confined to elective procedures, but not among urgent/emergent PCIs. In contrast, the higher rate of coronary dissection in the Thai PCI registry was noted when compared with the data from the Japanese registry. It might be explained by the study protocol of Thai PCI registry that documented all visible dissection flaps from coronary angiography whereas the Japanese registry documented only flow-impairing dissection. In addition, there are also differences in operator skill in IVUS imaging between Japan and Thailand. In Japan, IVUS-guided PCI was used in over 90% of elective PCI procedures and in over 80% of the overall procedures7, whereas the rate of IVUS use in Thailand is approximately 10%. Therefore, the rate of coronary dissection could be higher due to the lack of familiarity of the operators with the IVUS image sizing algorithm. In the OPUS-CLASS (OCT Compared With IVUS in a Coronary Lesion Assessment) study32, measurement of the lumen diameter and lumen area of a phantom model were compared between IVUS and OCT. The lumen area measured by OCT was equivalent to the actual lumen area of the phantom model, whereas the measurement by IVUS was significantly greater, by 8%, than the value measured by OCT32. If the operators were not aware of this overestimation, coronary dissection could occur from stent or balloon oversizing leading to intramural haematoma in less diseased reference segments33. Previously, a nationwide inpatient database in the USA reported that IVUS-guided PCI was used in only 10.4% of PCI procedures for calcified coronary lesions34, and the IVUS-assisted procedure increased the overall cardiac complication rate (OR 1.25, CI 1.03–1.53, P = 0.025). Similar findings were also reported in the nationwide inpatient database in the USA for PCI in ST-segment elevation MI (OR 4.26, 95% CI 2.34–7.7, P < 0.01)35. The difference in IVUS usage may explain the different complication rates between high-volume (Japan) and low-volume (Thailand and USA) countries.
In the present study, IVUS-guided PCI did not improve short- or medium-term mortality rates after adjusting for covariables by propensity model and irrespective of whether the criteria were met. Our results contrasted with the pooled analysis of IVUS-XPL and ULTIMATE trials6, which showed a reduction of cardiac death in patients who were treated with IVUS-guided PCI compared with angio-guided PCI. However, it should be noted that the pooled analysis was an ad-hoc analysis in 2577 patients, including only patients with long lesions whereas the current study stratified the patients according to the AUC. In addition, pooled analysis reported cardiac mortality at 3-year follow-up6 while in contrast, the present analysis had clinical follow-up for 1 year. Regarding the real-world data of IVUS-guided PCI on the mortality, our study results were in line with previous reports that there was no improvement of mortality29,36 and MACE29 rates with IVUS-guided PCI.
Patients who did not meet the adjunct use criteria(C-) in the present study could be assumed as the representative for the case with non-complex lesions. The current analysis showed that IVUS-guided PCI in patients who did not meet the criteria (C− /I + group) had numerically higher procedural complication rate than that of patients who did not meet the criteria and underwent angio-guided PCI (C−/I−). A possible explanation for this might be the ad-hoc use of IVUS catheters after unfavourable angiographic findings, such as no-reflow phenomenon, coronary perforation, and coronary dissection, as demonstrated in Table 3.
Limitations
The present study had several limitations. First, the Thai PCI registry was an observational study. The criteria were applied retrospectively to the study population. The decision to use IVUS-guided PCI was made at the operator’s discretion. Second, IVUS was not available in all participating centres. Thus, there would have been variations in IVUS skill among centres. In addition, centres with IVUS facilities tend to perform more complex procedures than those without such facilities. It is unclear whether IVUS use was a marker of more complex procedures or supported/altered the operator strategy, as the study protocol did not document the pre-procedural SYNTAX score. Third, a detailed analysis of the IVUS findings, such as plaque characteristics, minimal stent area, and stent expansion, was not included in the study protocol. Finally, other long-term outcomes, such as recurrent MI and urgent revascularization, were not available in the present study.
Conclusion
The penetrance of IVUS-guided PCI was low despite clinical indications for IVUS usage in real-world data. Significant procedural success was achieved with IVUS-guided PCI regardless of whether the AUC were met. The procedural complication did not escalate when IVUS-guided PCI. IVUS-guided PCI seemed to reduce the mortality rates if the AUC were met, but this did not reach statistical significance.
Data availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Change history
02 February 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41598-023-29201-y
Abbreviations
- ACS:
-
Acute coronary syndrome
- AUC:
-
Adjunctive use criteria
- CTO:
-
Chronic total occlusion
- IVUS:
-
Intravascular ultrasound
- OCT:
-
Optical coherence tomography
- PCI:
-
Percutaneous coronary intervention
- MI:
-
Myocardial infarction
References
Zhang, J. et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: The ULTIMATE trial. J. Am. Coll. Cardiol. 72, 3126–3137. https://doi.org/10.1016/j.jacc.2018.09.013 (2018).
Hong, S. J. et al. Effect of intravascular ultrasound-guided drug-eluting stent implantation: 5-year follow-up of the IVUS-XPL randomized trial. JACC Cardiovasc. Interv. 13, 62–71. https://doi.org/10.1016/j.jcin.2019.09.033 (2020).
di Mario, C., Koskinas, K. C. & Raber, L. Clinical benefit of IVUS guidance for coronary stenting: The ULTIMATE step toward definitive evidence?. J. Am. Coll. Cardiol. 72, 3138–3141. https://doi.org/10.1016/j.jacc.2018.10.029 (2018).
Nerlekar, N. et al. Intravascular ultrasound guidance improves clinical outcomes during implantation of both first- and second-generation drug-eluting stents: A meta-analysis. EuroIntervention 12, 1632–1642. https://doi.org/10.4244/EIJ-D-16-00769 (2017).
Darmoch, F. et al. Intravascular Ultrasound Imaging-Guided Versus Coronary Angiography-Guided Percutaneous Coronary Intervention: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 9, e013678, https://doi.org/10.1161/JAHA.119.013678 (2020).
Hong, S. J. et al. Improved 3-year cardiac survival after IVUS-guided long DES implantation: A patient-level analysis from 2 randomized trials. JACC Cardiovasc. Interv. 15, 208–216. https://doi.org/10.1016/j.jcin.2021.10.020 (2022).
Kuno, T. et al. Real-world use of intravascular ultrasound in Japan: A report from contemporary multicenter PCI registry. Heart Vessels 34, 1728–1739. https://doi.org/10.1007/s00380-019-01427-9 (2019).
Okura, H. et al. Frequency and prognostic impact of intravascular imaging-guided urgent percutaneous coronary intervention in patients with acute myocardial infarction: results from J-MINUET. Heart Vessels 34, 564–571. https://doi.org/10.1007/s00380-018-1285-3 (2019).
Shin, D. H. et al. The current status of percutaneous coronary intervention in Korea: Based on year 2014 & 2016 cohort of korean percutaneous coronary intervention (K-PCI) registry. Korean Circ. J. 49, 1136–1151. https://doi.org/10.4070/kcj.2018.0413 (2019).
Choi, K. H. et al. Impact of intravascular ultrasound-guided percutaneous coronary intervention on long-term clinical outcomes in patients undergoing complex procedures. JACC Cardiovasc. Interv. 12, 607–620. https://doi.org/10.1016/j.jcin.2019.01.227 (2019).
Ankle Brachial Index, C. et al. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA 300, 197–208, https://doi.org/10.1001/jama.300.2.197 (2008).
Mentias, A. et al. Long-term outcomes of coronary stenting with and without use of intravascular ultrasound. JACC Cardiovasc. Interv. 13, 1880–1890. https://doi.org/10.1016/j.jcin.2020.04.052 (2020).
Smilowitz, N. R., Mohananey, D., Razzouk, L., Weisz, G. & Slater, J. N. Impact and trends of intravascular imaging in diagnostic coronary angiography and percutaneous coronary intervention in inpatients in the United States. Catheter Cardiovasc. Interv. 92, E410–E415. https://doi.org/10.1002/ccd.27673 (2018).
Biondi-Zoccai, G. et al. Is intravascular ultrasound beneficial for percutaneous coronary intervention of bifurcation lesions? Evidence from a 4314-patient registry. Clin. Res. Cardiol. 100, 1021–1028. https://doi.org/10.1007/s00392-011-0336-x (2011).
Raber, L. et al. Clinical use of intracoronary imaging. Part 1: guidance and optimization of coronary interventions. An expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. Eur. Heart J. 39, 3281–3300, https://doi.org/10.1093/eurheartj/ehy285 (2018).
Elgendy, I. Y., Mahmoud, A. N., Elgendy, A. Y. & Bavry, A. A. Outcomes With Intravascular Ultrasound-Guided Stent Implantation: A Meta-Analysis of Randomized Trials in the Era of Drug-Eluting Stents. Circ. Cardiovasc. Interv. 9, e003700, https://doi.org/10.1161/CIRCINTERVENTIONS.116.003700 (2016).
Hong, S. J. et al. Effect of intravascular ultrasound-guided vs angiography-guided everolimus-eluting stent implantation: The IVUS-XPL randomized clinical trial. JAMA 314, 2155–2163. https://doi.org/10.1001/jama.2015.15454 (2015).
Shin, D. H. et al. Effects of intravascular ultrasound-guided versus angiography-guided new-generation drug-eluting stent implantation: Meta-analysis with individual patient-level data from 2345 randomized patients. JACC Cardiovasc. Interv. 9, 2232–2239. https://doi.org/10.1016/j.jcin.2016.07.021 (2016).
Groenland, F. T. W. et al. Intravascular ultrasound-guided versus coronary angiography-guided percutaneous coronary intervention in patients with acute myocardial infarction: A systematic review and meta-analysis. Int. J. Cardiol. 353, 35–42. https://doi.org/10.1016/j.ijcard.2022.01.021 (2022).
Choi, I. J. et al. Impact of intravascular ultrasound on long-term clinical outcomes in patients with acute myocardial infarction. JACC Cardiovasc. Interv. 14, 2431–2443. https://doi.org/10.1016/j.jcin.2021.08.021 (2021).
Kim, Y. et al. Role of Intravascular Ultrasound-Guided Percutaneous Coronary Intervention in Optimizing Outcomes in Acute Myocardial Infarction. J. Am. Heart Assoc. 11, e023481, https://doi.org/10.1161/JAHA.121.023481 (2022).
Gao, X. F. et al. 3-Year outcomes of the ULTIMATE trial comparing intravascular ultrasound versus angiography-guided drug-eluting stent implantation. JACC Cardiovasc. Interv. 14, 247–257. https://doi.org/10.1016/j.jcin.2020.10.001 (2021).
Ali, Z. A. et al. Outcomes of optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation: one-year results from the ILUMIEN III: OPTIMIZE PCI trial. EuroIntervention 16, 1085–1091. https://doi.org/10.4244/EIJ-D-20-00498 (2021).
N, S. et al. Multi-Center, Prospective, Nation-Wide Coronary Angioplasty Registry in Thailand (Thai PCI Registry): Registry Design and Rationale. J. Med. Assoc. Thai. 104, 1678–1685, https://doi.org/10.35755/jmedassocthai.2021.10.13066 (2021).
Sansanayudh, N. et al. Patient characteristics, procedural details, and outcomes of contemporary percutaneous coronary intervention in real-world practice: Insights from nationwide Thai PCI registry. J. Interv. Cardiol. 2022, 5839834. https://doi.org/10.1155/2022/5839834 (2022).
Austin, P. C., Grootendorst, P. & Anderson, G. M. A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: A Monte Carlo study. Stat. Med. 26, 734–753. https://doi.org/10.1002/sim.2580 (2007).
Austin, P. C. Propensity-score matching in the cardiovascular surgery literature from 2004 to 2006: A systematic review and suggestions for improvement. J. Thorac. Cardiovasc. Surg. 134, 1128–1135. https://doi.org/10.1016/j.jtcvs.2007.07.021 (2007).
Austin, P. C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 28, 3083–3107. https://doi.org/10.1002/sim.3697 (2009).
Tindale, A. & Panoulas, V. Real-world intravascular ultrasound (IVUS) use in percutaneous intervention-naive patients is determined predominantly by operator, patient, and lesion characteristics. Front. Cardiovasc. Med. 9, 974161, https://doi.org/10.3389/fcvm.2022.974161 (2022).
Koskinas, K. C. et al. Current use of intracoronary imaging in interventional practice - Results of a European Association of Percutaneous Cardiovascular Interventions (EAPCI) and Japanese Association of Cardiovascular Interventions and Therapeutics (CVIT) Clinical Practice Survey. EuroIntervention 14, e475–e484. https://doi.org/10.4244/EIJY18M03_01 (2018).
Mintz, G. S. Intravascular imaging, stent implantation, and the elephant in the room. JACC Cardiovasc. Interv. 10, 2499–2501. https://doi.org/10.1016/j.jcin.2017.09.024 (2017).
Kubo, T. et al. OCT compared with IVUS in a coronary lesion assessment: the OPUS-CLASS study. JACC Cardiovasc. Imag. 6, 1095–1104. https://doi.org/10.1016/j.jcmg.2013.04.014 (2013).
Liu, X. et al. Intravascular ultrasound assessment of the incidence and predictors of edge dissections after drug-eluting stent implantation. JACC Cardiovasc. Interv. 2, 997–1004. https://doi.org/10.1016/j.jcin.2009.07.012 (2009).
Desai, R. et al. Modern-day nationwide utilization of intravascular ultrasound and its impact on the outcomes of percutaneous coronary intervention with coronary atherectomy in the united states. J. Ultrasound Med. 38, 2295–2304. https://doi.org/10.1002/jum.14922 (2019).
Khalid, M. et al. In-hospital outcomes of angiography versus intravascular ultrasound-guided percutaneous coronary intervention in ST-elevation myocardial infarction patients. J. Commun. Hosp. Intern. Med. Perspect 10, 436–442. https://doi.org/10.1080/20009666.2020.1800970 (2020).
Ng, A. K., Ng, P. Y., Ip, A., Lam, L. T. & Siu, C. W. Survivals of angiography-guided percutaneous coronary intervention and proportion of intracoronary imaging at population level: the imaging Paradox. Front. Cardiovasc. Med. 9, 792837, https://doi.org/10.3389/fcvm.2022.792837 (2022).
Acknowledgements
The authors wish to express their appreciation to all the investigators and cardiac catheterization laboratories participating in the Thai PCI registry. We also thank all staff of the Department of Clinical Epidemiology and Biostatistics, Faculty of Medicine, Mahidol University, for their statistical support.
Funding
This project received a research grant from the Health System Research Institute, the Ministry of Public Health of Thailand, in March 2017. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
P.S. contributed to the conception, data interpretation, drafting, and revising of the manuscript. P.C. and N.S. contributed to the conception and drafting of the manuscript. A.T. performed the statistical analysis, interpreted the data, drafted and revised the manuscript. W.R., A.T., A.W., M.M., A.K., M.C., S.K., and S.S. contributed to the data collection, data interpretation, and drafting of the manuscript. All authors approved publication of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in the spelling of the author Ammarin Thakkinstian which was incorrectly given as Ammarin Thakkinstain.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Suwannasom, P., Chichareon, P., Roongsangmanoon, W. et al. Impact of the adjunctive use criteria for intravascular ultrasound-guided percutaneous coronary intervention and clinical outcomes. Sci Rep 13, 711 (2023). https://doi.org/10.1038/s41598-022-27250-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-27250-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.