Abstract
Naïve T cells become effector T cells following stimulation by antigen-loaded dendritic cells (DCs) and sequential cytokine activation. We aimed to develop procedures to efficiently activate T cells with tumor-associated antigens (TAAs) to glioblastoma (GBM) stem cells. To remove antigen presentation outside of the immunosuppressive tumor milieu, three different glioma stem cell (GSC) specific antigen sources to load DCs were compared in their ability to stimulate lymphocytes. An activated T cell (ATC) protocol including cytokine activation and expansion in culture to target GSCs was generated and optimized for a planned phase I clinical trial. We compared three different antigen-loading methods on DCs to effectively activate T cells, which were GBM patient-derived GSC-lysate, acid-eluate of GSCs and synthetic peptides derived from proteins expressed in GSCs. DCs derived from HLA-A2 positive blood sample were loaded with TAAs. Autologous T cells were activated by co-culturing with loaded DCs. Efficiency and cytotoxicity of ATCs were evaluated by targeting TAA-pulsed DCs or T2 cells, GSCs, or autologous PHA-blasts. Characteristics of ATCs were evaluated by Flow Cytometry and ELISpot assay, which showed increased number of ATCs secreting IFN-γ targeting GSCs as compared with non-activated T cells and unloaded target cells. Neither GSC-lysate nor acid-eluate loading showed enhancement in response of ATCs but the synthetic peptide pool showed significantly increased IFN-γ secretion and increased cytotoxicity towards target cells. These results demonstrate that ATCs activated using a TAA synthetic peptide pool efficiently enhance cytotoxicity specifically to target cells including GSC.
Similar content being viewed by others
Introduction
Glioblastoma (GBM) is the most common and lethal brain tumor in the United States and accounted for 14.6% of all primary brain and other central nervous system (CNS) tumors in 20201. Five-year survival rate after diagnosis is as low as 6.8%1. Different approaches have been studied to treat cancers including GBM. In particular, recent efforts in immunotherapy across multiple tumor types have seen tremendous success2,3,4,5. Given the well-known heterogeneity of GBM, immunotherapeutic strategies targeting multiple targets may hold the most promise for addressing this challenging disease.
Antigen specific cellular immune response is required to induce T cell (TC) activation by antigen presenting cells and proliferation in lymph nodes to initiate a T cell response against cancer. Dendritic cells (DCs) are professional antigen presenting cells with the greatest capacity to process and present antigen to T cells. Previously, we vaccinated GBM patients with a DC vaccine to induce a long-lived immune response in patients with GBM6,7,8. The antigen source for these trials included MHC-I acid-eluted peptides6, glioblastoma tumor lysate7,8, and specific epitopes targeting glioma stem cells (GSCs)9,10. The results showed that tumor antigen-loaded DCs can migrate to lymph nodes to induce antigen-specific systemic T cell responses that localize intracranially in glioblastoma9. A placebo-controlled randomized trial of those peptide loaded DCs demonstrated significant improvement in progression free survival in newly diagnosed GBM patients as compared to unloaded DC vaccinations10. The immune response was shown to target GSCs, which were derived from GBM patients. Despite these findings, the T cell responses generated by the vaccine remained limited in number and potency. This blunted response might be due to the lack of helper T lymphocyte (Th) support, which is critical to sustain a long-lived response11,12,13,14. In addition, cytokine support may be lacking in immunosuppressed cancer patients. To overcome these limitations, we sought to keep the potent antigen presentation of DCs supplemented with helper T cells and cytokines to support the effector response in a setting outside of the immunosuppressive mileu of the cancer patient. Immune cells that more directly attack cancer cells need to be highly strengthened in order to eliminate residual tumor and prevent recurrence after surgery, chemotherapy and radiotherapy. Naïve T cells from GBM patients can be activated ex vivo by autologous DCs loaded with cancer cell antigens and expanded to generate sufficient cytotoxic T lymphocytes (CTL), which can specifically target cancer cell antigens of GBM patients. The activation and expansion of T cells ex vivo enabled the increase in potency and numbers of cytotoxic and helper T cells for infusion.
To determine the best source of cancer cell antigens to target glioblastoma cancer stem cells, we compared the specific immunogenicity of antigens obtained from tumor lysate of GSCs, acid-eluted antigens from MHC-I epitopes washed from the surface of GSCs, and pool of specific MHC I and II peptides known to be expressed on GSCs. We sought to compare the generation of activated T cells (ATCs), which could target GSCs of GBM patients. Our goal was to develop a novel adoptive T cell therapy with the highest capacity to induce a specific T cell response against cancer stem cells in GBM, with a minimal risk of side effects.
Results
Characterization of T cells activated by glioma stem cell lysate
Autologous monocytes were differentiated into DCs with Granulocyte–Macrophage Colony Stimulating Factor (GM-CSF) and IL-4, then matured by lipopolysaccharide (LPS) and interferon-gamma (IFN-γ). GSC lysate (final concentration of 100 µg/mL) was loaded onto DCs to so that the mature DC are presenting peptides derived from GSC. Naïve T cells and DCs were then mixed at 10:1 ratio in a G-Rex 100 container for T cell activation and rapid proliferation for 12 days with culture medium containing IL-4, IL-7 and IL-2. Number of T cells expanded in the G-Rex container were counted at day 5, 7, 9 and 12 while IL-2 was added every other day to enhance the growth. Both TNLY (T cells activated by unloaded DCs (DC-NLY)) and TLY (T cells activated by GSC lysate-loaded DCs (DC-LY)) showed increases in cell density at day 12, which was 12 times great than the initial culture density (Fig. 1a). Co-cultured cells were sampled at day 7 and 12 for characterization analysis by flow cytometry to evaluate maturation of T cells. Sub-populations of CD3+ T cells were detected for CD4 and CD8. CD4+ T cells and CD8+ T cells were 82% and 14.2% of TLY12 cells, respectively while 80.7% of CD4+ and 15.0% of CD8+ T cells in TNLY12 were observed (Fig. 1b). There was no significant difference in CD4+:CD8+ ratio between TLY12 and TNLY12. More interestingly, over several days of incubation, CD4+:CD8+ ratio increased dramatically (62.3:29.9 on day 7 vs. 82:14.2 on day 12). Again, no difference was seen between TNLY and TLY groups. All surface markers including CD154, CD69, CD137, HLA-DR and CD45RO for T cell activation were up-regulated in all T cells compared to naïve T cells (T0) (Fig. 1c). To evaluate antigen-specific cytokine secretion as a result of activation, frequency of IFN-γ secreting T cells as effector cells against target cells, which were antigen-pulsed DCs or unpulsed DCs, was measured by ELISpot assay (Fig. 1d). Frequencies of IFN-γ secreting T cells were all up-regulated from T0. T cells at day 12 had more spot counts than ones at day 7 and especially against lysate-pulsed DCs compared to other target types (p < 0.01, data not shown). However, significant difference between TLY and TNLY was not detected in cytokine secretion against lysate-pulsed DCs (Fig. 1d).
T cell activation with DCs loaded with GSC lysate. (a) Cell growth curve of activated T cells. 40 U/mL of IL-2 was added to the medium every other day until day 10. (b) Expression of CD4 and CD8 by CD3+ T cells at day 7 and 12. (c) Surface markers of T cells by flow cytometry. (d) ELISpot assay to measure IFN-γ secretion of T cells against DCs pulsed with or without GSC lysate. T cells without DCs were also measured as comparison. T0: naïve T cells, TNLY12: T cells co-cultured with non-lysate loaded DCs for 12 day, TLY12: T cells co-cultured with lysate-loaded DCs for 12 day. ns, no significant difference.
Characterization of T cells activated by acid-eluted peptides from GSCs
Autologous monocytes were differentiated into DCs with GM-CSF and IL-4, then matured by LPS and IFN-γ. Acid-eluted peptides (100 ng/mL) were loaded to DCs following maturation. Naïve T cells and DCs were then mixed at 10:1 ratio in a G-Rex 100 container for T cell activation and rapid proliferation for 12 days with culture medium containing IL-4, IL-7 and IL-2. The number of T cells expanded in the G-Rex container were counted at day 5, 7, 9 and 12 while IL-2 was added every other day to enhance the growth. Both TNEP (T cells activated by unloaded DCs (DC-NEP)) and TEP (T cells activated by DCs loaded with eluted GSC peptides with acid (DC-EP)) showed increases in cell density at day 12, which was 6 times greater than the initial culture density (Fig. 2a). Co-cultured cells were sampled at day 7 and 12 for characterization analysis by flow cytometry to evaluate maturation of T cells. Sub-populations of CD3+ T cells were detected for CD4 and CD8. CD4+ T cells and CD8+ T cells were about 57.1% and 34.3% in TEP12 samples, respectively (Fig. 2b). On the other hand, CD4+ and CD8+ population of TNEP12 samples were 59.2% and 32.7%, respectively. There was no significant difference in CD4+:CD8+ ratio between TEP12 and TNEP12, or on day 7 versus day 12. All surface markers including CD154, CD69, CD137, HLA-DR and CD45RO for T cell activation were up-regulated in all T cells comparing to T0 (Fig. 2c). To evaluate antigen-specific cytokine production as a result of activation, frequency of IFN-γ secreting T cells as effector cells against antigen-pulsed DCs or unpulsed DCs was measured by ELISpot assay (Fig. 2d). Frequencies of IFN-γ secreting T cells were all up-regulated from T0 but significant difference among different types of T cells was not observed. TNEP7 cells always showed highest frequency.
T cell activation with DCs loaded with GSC-eluted peptides. (a) Cell growth curve of activated T cells. 40 U/mL of IL-2 was added to the medium every other day until day 10. (b) Expression of CD4 and CD8 by CD3+ T cells at day 7 and 12. (c) Surface markers of T cells by flow cytometry. (d) ELISpot assay to measure IFN-γ secretion of T cells against DCs pulsed with or without GSC-eluted peptides. T cells without DCs were also measured as comparison. T0: naïve T cells, TNEP12: T cells co-cultured with non-peptide loaded DCs for 12 day, TEP12: T cells co-cultured with eluted peptides-loaded DCs for 12 day. ns, no significant difference.
Generation of peptide pool as GBM specific antigens
Sequences of 9 CTL peptides and 9 helper T lymphocyte (Th) peptides were determined based on previous studies demonstrating expression on glioblastoma cells and on glioblastoma stem cells (Table 1) and potential cross-reactivities of ATCs activated with those synthetic peptides were analyzed. The Human Protein Atlas (https://www.proteinatlas.org/) was used to confirm the expression of each target protein in human normal tissues. RNA expression profiles in human normal tissues by NCBI Gene (https://www.ncbi.nlm.nih.gov/gene/) was used instead only if there was no data for the target protein in the Human Protein Atlas. According to the Human Protein Atlas, gp100, MAGE-A1, NY-ESO-1, and TRP-2 are uniquely expressed in normal skin, testis, testis and skin, respectively (data not shown). RNA expression of AIM2, EphA2, and IL-13Ra2 is relatively lower across any tissues except 1–2 tissue types such as lymph node, esophagus, and testis. HER2 protein is expressed in many types of normal tissue but it is known to be overexpressed in many types of cancer cells. We also performed homology searches by NCBI Protein BLAST (https://blast.ncbi.nlm.nih.gov/Blast.cgi) to investigate the cross-reactivity of our peptides. The search results showed that all epitopes were highly specific to each target protein except AIM2Intron and gp100209-217-2 M (data not shown). The peptide sequence of AIM2Intron did not match to the original protein sequence because it was designed from the nonspliced transcript containing the retained intron, which is well recognized by T cells15,16. Sequence of gp100209-217-2 M is modified from the original amino acid sequence of gp100209-217 [ITDQVPFSV]. We altered the peptide sequence [IMDQVPFSV] by changing the second amino acid from threonine (T) to methionine (M) as this was reported to increase the affinity for GM-CSF -associated HLA-A2.1, resulting in enhanced induction of T cells against native epitope17,18,19. These unique peptides did not show significant homology to other protein sequences.
Activation of autologous T cells by using GBM-specific-peptide pool
T cells were activated (TPP) by autologous monocyte-derived DCs, which were matured and loaded with synthetic peptide cocktail specific for GBM including 9 CTL epitopes (final concentration 20 µg/mL of each) and 9 Th epitopes (final concentration 20 µg/mL of each). As controls, T cells without incubation (T0) and T cells cocultured with DCs without peptide loading (TNPP) were also prepared. To assess the activation of T cells, TPP and TNPP were harvested at 5 days after co-culturing with DCs and analyzed for T cell surface markers by flow cytometry with T0. The number of T cells expanded in the G-Rex container were counted at day 5, and 19 while IL-2 was added every other day to enhance the growth. Both TNPP (T cells activated by unloaded DCs (DC-NPP)) and TPP (T cells activated by DCs loaded with GBM-specific synthetic peptide pool (DC-PP)) showed increases in cell density at day 19, which was 11 times larger for TNPP and 14 times larger for TPP than an initial culture density (Fig. 3a). Sub-populations of CD4+ and CD8+ in CD3+ TPP19 were 80.1% and 17.3% at day 19, respectively, and slightly increased for CD4+ (74%) and decreased for CD8+ (22.5%) in comparison with TNPP19 group (Fig. 3b). Compared with activation markers in T0, expression of CD69 and CD137 increased in TNPP and TPP, furthermore, CD69 on TPP group was much higher than TNPP, indicating T cells in TNPP and TPP were activated (Fig. 3c). There was no significant difference in expression of CD45RO and CD154 across all T cell types. TNPP and TPP were harvested at day 12 (TNPP12 and TPP12) and compared in ELISpot assay where T cells targeted two types of T2 cells (peptide pool-pulsed T2 (T2-PP) vs. unpulsed T2 (T2-NPP)) and patient-derived GSC lines CSC38b, CSC40b, CSC59 and CSC66, which are all HLA-A2 positive. Frequency of IFN-γ secreting T cells significantly increased when TPP12 was co-cultured with T2-PP and all four tested GSC lines (Figs. 3d and 4e, p < 0.0001). To determine the optimal culture time to obtain sufficient cytokine secretion of ATCs, ELISpot data for T cells co-cultured with DC-PP for 12 days (TPP12) and 19 days (TPP19) were compared against T2-PP and individual GSC line. Our results showed that more antigen specific IFN-γ secreting T cells were detected at day 12 than day 19 when TPP12 was co-cultured against antigen-loaded T2 cells or GSCs (Figs. 3f and 4g, p < 0.0001).
Autologous T cell activation by using GBM-specific peptide pool. (a) Cell growth curve of activated T cells. 40 U/mL of IL-2 was added to the medium every other day until day 19. (b) Expression of CD4 and CD8 by CD3+ T cells at day 4 and 19. (c) Analysis of T cell surface marker to assess activation of T cells at day 5. (d) ELISpot assay to measure IFN-γ secretion of T cells against GBM-specific peptides-pulsed T2 cells (T2-PP) in contrast to unpulsed T2 cells (T2-NPP). (e) IFN-γ secretion of T cells responding to institute-established GBM cancer stem cell lines (all HLA-A2 +) compared to naïve T cells (T0) and T cells activated by no-peptides-loaded DCs (TNPP12). (f) Comparison of IFN-γ secretion between 12 and 19 days of T cell activation by co-culturing ATCs with T2 cells pulsed with peptide pool. (g) Comparison of IFN-γ secretion between 12 and 19 days of T cell activation by co-culturing ATCs with four different GSC lines. *p < 0.05 and ****p < 0.0001. ns, no significant difference.
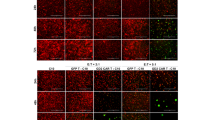
Intracellular cytokine staining. T cells were cultured under various conditions (as indicated) and stained for surface markers and cytokines (described in the materials and methods). The cells were first gated to exclude doublets or groups of cells, the live cells were selected by live/dead dye, followed by selection of CD3+ and CD4+ or CD8+. The cells could be further identified by cytokine expressions (the percentage of gated cells was indicated).
Cytokine production of autologous T cells by intracellular cytokine staining
T cells from various groups: T0: naïve T cells at day 0, TPP12: T cells were expanded with peptide-loaded DCs for 12 days and TNPP12: T cells were expanded with unloaded DCs for 12 days, were in vitro cultured in three different conditions: medium alone (untreated), medium with peptide pool (PP), and medium with T2 cells pulsed with peptide pool (T2-PP). Our data showed that TPP12 had robust responses to T2-PP. Both CD4+ and CD8+ T cells from TPP12 group revealed a strong recall response to T2-PP with high IFN-γ secretion (Fig. 4). More interestingly, both CD4+ and CD8+ T cells presented multifunctionality: secreting both IFN-γ and IL-2. Although TPP12 under peptide pool stimulation also displayed high cytokine production from CD4+ and CD8+ T cells, as well as multifunctionality of T cells, in comparison with untreated group, but they are not as strong as T2-PP group. In addition, our data disclosed that T0 group as well as T cell group expended for 12 day without peptide pool stimulation (TNPP12) had minimal IFN-γ and IL-2 production, even with stimulations from T2-PP or PP alone (Table 2). In summary, our approach to generate tumor-antigen specific T cells demonstrated strong antigen-specific recall responses.
Cytotoxicity assay for glioma stem cells
Our data so far showed that among three various ways to generate antigen specific T cells, cells activated with GBM-specific peptide pool was the most robust generating cytokine. Here we further assessed the killing ability of these ATCs using CSC66 as target cells. As described in Methods, HLA-A2 positive GSC line, CSCC66 was stained with CTV dye, T cells with DC-PP (TPP) or DC-NPP (TNPP) were co-cultured at E:T ratio of 20:1. Single cell suspension was examined by flow cytometry for CTV dye. Mean percentage of dead CSC66 was 16.1% with effector T cells while mean spontaneous lysis of CSC66 was 2%, showing significant increase in killing target cells (Fig. 5a). Longer incubation time was reported to increase cytotoxicity of CTLs while standard 4-h incubation did not result in substantial cell killing20. Therefore, comparison between standard incubation (4 h) and overnight incubation (18 h) were performed to determine the optimal incubation time for cytotoxic killing assay on GSCs with ATCs. The longer incubation did not increase spontaneous cell death (data not shown) but percentage specific lysis increased more than double in 18-h incubation (Fig. 5b). There was no increased killing of HLA-A2 negative cells with any of our T cells (data not shown).
Cytotoxicity analyses with ATCs. (a) Population of dead CSC66 cells analyzed by flow cytometry. Dead GSCs were detected as double-positive for CellTrace Violet (CTV) dye and Fixable Viability eFluor 780 dye (FVD), where CTV stained only GSCs and FVD stained dead cells. The plot shows mean percentages of dead GSCs with or without co-culturing with TPP (activated T cells by synthetic peptide-loaded DCs). (b) Comparison of specific lysis between short incubation (4 h) and long incubation (18 h). (c) In vitro assay for autoimmune effect of ATCs on autologous PHA-blast (BL). PHA-blasts were co-cultured with T0, TNPP and TPP at effector:target (E:T) ratio of 20:1. Population of dead PHA-blasts was also detected as spontaneous lysis by analyzing % parent CTV + /eFluor780 + population. % parent of PHA-blast without any T cells was used to calculate % specific lysis for T0, TNPP and TPP, showing all less than 5% of dead PHA-blasts. (d) Percent specific lysis of floating U87 cells (detached from a culture plate and co-cultured as floating cells) lysed by T cells (T0, TNPP12 or TPP12) at different E:T ratio after co-culturing for 18 h. (e) Percent specific lysis of adherent U87 cells (kept attached on a culture plate and co-cultured as adherent cells) lysed by T cells (T0, TNPP12 or TPP12) at different E:T ratio after co-culturing for 18 h. Those percentages were calculated based on the population of dead U87 cells analyzed by flow cytometry. *p < 0.05.
Autoimmune responses by activated T cells
To assess the potential autoimmune side effect of activated T cells, autologous, phytohemagglutinin-L (PHA) stimulated lymphoblasts were generated from peripheral blood mononuclear cells (PBMCs) from the same donor and co-cultured with T cells at 20:1 (E:T)21. We compared percentage lysis of PHA-blasts among DC-PP activated T cells (TPP), non-activated T cells (TNPP) and spontaneous lysis of blasts measured by Flow cytometry (Fig. 5c). Plot shows that less than 5% of PHA-blasts were killed by any of T cells (T0, TNPP or TPP). There was no significant effect of activated T cells on autologous immune cells.
Cytotoxicity assay using the U87 GBM line
We also demonstrated an antigen specific dose-dependent killing pattern from an E:T ratio of 5:1 through 10:1 to 20:1 using the HLA-A2 positive U87 cell line22. This was consistent when using detached U87 cells (Fig. 5d) as well attached U87 cells (Fig. 5e). The cytotoxicity was over 40% under both conditions at the 20:1 E:T ratio.
Discussion
In this study, we demonstrated the development of autologous activated T cell therapy using three different types of antigen stimulation to pulse DCs ex vivo in order to identify the optimal activation conditions to generate ATCs, which can improve the efficacy of cancer immunotherapy against GSCs. Cancer cell lysate has been used as one of the major antigen sources to load DCs against cancer cells and induce cytotoxicity of T cells7,23,24,25. However, in this study, cell lysate was not the most efficient stimulator to activate T cells specific to epitopes loaded on DCs as targets. T cell activation markers showed that T cells at day 7 were clearly activated when compared to naïve T cells (T0), which was also true for the cells at day 12. However, there was no significant difference between T cells co-cultured with DCs loaded with tumor lysate (TLY7) and T cells co-cultured with unloaded DCs (TNLY7) for 7 days (data not shown), or between TLY12 and TNLY12, which were expanded for 12 days. Using lysate from cancer stem cells may not be an ideal antigen source because cell lysate contains various types of proteins and debris besides relevant fragments of cancer specific target proteins as tumor antigen for DCs to present. Only limited number of DCs could be loaded with a relevant set of TAAs over a large amount of non-TAAs. In addition, the efficacy of lysate-based T cell activation might be limited if the cancer cells do not express sufficient numbers of antigens, suggesting that antigen source needs to be autologous not allogenic when cancer cell lysate is used to pulse DCs. Gonzalez et al.25, further mentioned pulsing DCs with tumor lysate can also induce tolerogenic transformation of DCs by providing immunoregulatory cytokines which may explain the poor activation observed with tumor lysates in our experiments25.
A similar explanation can be applied to the activation efficiency of T cells by acid-eluted GSC peptides. T cell activation markers showed that T cells at day 7 were clearly activated when compared to T0 cells, which was also true for the cells at day 12. All T cell groups showed more IFN-γ secreting cells than T0 cells, but there was no significant difference between DCs with or without the peptides. Although isolated acid-eluted peptides on the surface of GSCs contain less variety of peptides than whole GSC lysate, acid-eluted GSC peptides still may have limited antigen-specific activation of T cells against target cells.
Regardless of whether they are loaded with antigens or not, matured DCs induced activation of autologous naïve T cells (T0) in vitro. Compared to T0 cells, IFN-γ secretion by all ATCs encountering different stimulus was increased dramatically. T cells seemed to react strongly toward DCs loaded with antigen compared to “empty” DCs (no-antigen loaded). But no statistical significance was found in activation with DC-LY or DC-EP, suggesting that no matter how T cells are activated by DCs loaded with GSC-derived antigen (either GSC-lysate or acid-eluted peptides), the activation is not sufficient to produce tumor antigen-specific ATCs. However, in terms of difference between DC-LY and DC-EP, T cells activated by DC-LY showed much stronger responses as shown by the frequencies of IFN-γ secreting T cells following DC-LY than ones activated by DC-EP.
Delluc et al.26 demonstrated the comparison of immunogenic efficacy between two different acid elution methods, which were citrate–phosphate (CP) and trifluoroacetic acid (TFA) buffer, to choose the best elution method for DC-based vaccine therapy in acute myeloid leukemia (AML)26. Their study found that TFA-eluted peptide-loaded DC was more efficient to induce immune response specific to leukemia than CP-eluted peptide-loaded DC, suggesting that even the selection of the acid elution method to isolate cancer cell specific antigen peptides significantly affects to the immunogenic efficacy of generated ATCs. In this study we only used CP buffer to isolate dissociated peptides, as described in our previous Phase I trial6. Using TFA to elute peptides from the membrane surface of GSCs may improve the immunogenicity of ATCs. However, expectation of dramatic improvement is not high because cell lysate loaded DCs induce significantly higher number of IFN-γ secreting T cells than TFA-loaded DCs against an Epstein-Barr virus (EBV)-transformed B-lymphoblastoid cell line27.
To overcome the poor efficiency of both antigen sources (GSC lysate and acid-eluted peptides) in T cell activation, a pool of GBM-specific synthetic peptides was applied as the third stimulation method. Activation of T cells by DC-PP was confirmed by surface marker analysis and there were more IFN-γ secreting cells for antigen specific ATCs towards T2-PP as antigen presenting cells than any other conditions including ATCs with T2 cells without peptide pulsing. Although both T2 cells with or without synthetic peptide pool activated T cells, no significant difference of activation markers was shown between these groups. However, with regard to antigen specific cytokine secretion, there was a significant difference. This may suggest that T cell activation marker expression may not correlate with cytokine production function. More interestingly, our study suggests that T cell expansion with tumor peptide pool stimulation generates antigen-specific multifunctional T cells. Multifunctionality is the ability of T cells to perform several functions, such as the secretion of several cytokines, or other soluble lysis factors at the single cell level. It has been shown as an important parameter to predict the quality of T cell response and immunological control of tumor and infectious disease28,29. More studies are needed to understand the mechanisms to elicit multifunctional T cells in order to enhance tumor specific immunity.
We also investigated how longer incubation times for co-culturing T cells with DCs impacts T cell activation, which helped us to determine if longer culturing time can enhance cytotoxicity of ATCs. However, we found the opposite result with a dramatic decrease in the number of IFN-γ secreting T cells after an additional 7 days of culture. Longer incubation (12 days) induced higher frequency of IFN-γ secreting T cells than shorter incubation (3 days) (data not shown) but cytotoxicity lowered at day 19. These results indicate that cytotoxicity of ATCs becomes significantly high after 12 days of co-culture with DC-PP but excess culture diminishes the activation effect.
To assess the cytotoxicity of ATCs against GSCs in vitro, we performed non-radioactive cytotoxicity assay with of CellTrace Violet (CTV) dye instead of chromium 51 (51Cr) release assay30,31, which has been a traditional method for assessment of cytotoxic effect by CTLs in vitro32,33. Percentage of lysed GSCs dramatically increased by co-culturing with peptide-activated T cells. Autoimmune toxicity against normal cells should be evaluated when immunogenicity is induced because of the potential cytotoxic effect of ATCs against autologous healthy immune cells or normal tissues34,35. One of the major risks of T cell therapy is graft-versus-host (GVH) response when donor T cells are infused to the patient. However, this GVH adverse effect can be avoided if autologous T cells are activated and expanded ex vivo to treat cancer in the same patient. On the other hand, there still remains possible side effects36. Sequences of MHC I and MHC II peptides were carefully selected to enhance cytotoxicity against GSCs and minimize autoimmune reaction in normal cells, which has been reported when normal cells express the same peptides utilized as the antigen source for T cell activation34,35. T cells activated by this method kill less than 5% of autologous PHA-stimulated blast cells, suggesting that our T cells activated by DC-PP do not induce autoimmune toxicity by ATCs against autologous immune cells. Our results showed that the method to generate ATCs by a synthetic peptide pool was feasible and efficient to activate T cells generating antigen-specific immune responses without showing any autoimmune toxicity, supporting the notion that this method can be used as a safe way to propagate GSC-specific ATCs for immunotherapy for GBM.
In conclusion, a pool of cancer-specific synthetic peptides was found that exhibited as a promising source for T cell activation compared to other traditional sources of tumor antigen, which are tumor cell lysate or acid-eluted tumor cell peptides from a GSC line. We have established a potentially safe protocol to develop T cell therapy activated by synthetic peptide-loaded dendritic cells for GBM patients, showing enhanced capability of cytotoxicity against HLA type matched glioma stem cells in vitro without autoimmune risk. After infusion, these activated T cells should have the capacity to generate tumor antigen-specific and cytotoxic immune responses in vivo to facilitate GBM treatment. This method of T cell activation has been implemented into an investigational new drug cleared by the FDA.
Materials and methods
Patient-derived glioma stem cell lines
Patient-derived GSCs were established from tumors of GBM patients as previously described37,38 and cultured in serum-free neurobasal medium at Cedars-Sinai Medical Center. All GSCs were approved by the institutional review board of Cedars-Sinai Medical Center and informed consents were obtained from all patients. All methods were performed in accordance with the Cedars-Sinai Medical Center institutional review board and institutional biosafety committee guidelines and regulations.
Monocytes and T cell preparation
HLA-A2 positive apheresis products were obtained from the Blood Donor Facility at the Cedars-Sinai Medical Center or purchased from HemaCare Corp. (Van Nuys, CA). Using the Elutra Cell Separation System (Terumo BCT), both monocytes and lymphocytes were isolated and red blood cells (RBCs) were removed. By staining the lymphocyte fraction with anti-CD3 antibody (BD Bioscience, Cat.564810) purification of T cells was assessed (T cells > 80%) and cells were frozen and stored in liquid nitrogen tank for later use. The monocyte fraction was stained with anti-CD14-PerCP (BD Bioscience, Cat.340585), anti-CD45-FITC (BD Bioscience, Cat.555482) and anti-CD66-PE (BD Bioscience, Cat.551480) antibodies. In order to generate DCs, more than 60% of the monocyte population needs to be CD14+/CD45+ while CD66+ cells are less than 10%.
Cancer stem cell lysates
Cancer cell lysates of GSC was prepared by harvesting cultured GSCs and cell lysates generated by several freezing and thawing cycles. Briefly, cultured neurospheres were collected and then dissociated by pipetting. Cells were then washed with 1X DPBS and frozen down with freezing medium at − 80 °C. Then cells were thawed at room temperature until completely thawed, followed by freezing the cells at − 80 °C for more than 2 h or in liquid nitrogen for 30 min. The freeze–thaw cycles were repeated three more times for a total of 4 cycles. After the last thawing step, the resulting suspension was centrifuged at 2000 rpm at 4 °C for 10 min. The supernatant was collected, filtered through 0.2 µm syringe filter and stored at − 80 °C until use.
Acid elution of peptides
MHC-I associated peptides were isolated from the cell surface proteins by eluting GSC lysate with acid as previously described6,39. Cultured GSC spheres were collected and dissociated. After several washings with HBSS buffer, about 108 cells were resuspended in 10 mL of citrate–phosphate buffer (pH 3.2) to dissociate peptides from surface MHC-I, gently homogenized until cell disruption and centrifuged at 1000 rpm for 5 min. The supernatant was collected and then concentrated by passing through Sep-Pak C18 cartridge (Waters Corp.), aliquoted and stored at − 80 °C.
Synthetic peptides
Eighteen human GSC-specific peptides including 9 MHC-I peptides (CTL peptides) and 9 MHC-II peptides (Th peptides) were selected based on amino acid sequences previously reported (Table 1)9,13,15,16,17,19,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57. All peptides were synthesized by PolyPeptide Group (Torrance, CA), diluted in dimethyl sulfoxide (DMSO) at 1 mg/mL and stored at − 20 °C until use. All eighteen peptides were pooled as antigen cocktail to stimulate DCs to later activate naïve T cells to become GSC-specific CTLs and Ths.
Generation of dendritic cells
Monocytes were cultured in MACS GMP Cell Differentiation Bags (Miltenyi Biotec, Germany) containing DC culture medium (DC medium, 560 U/mL GM-CSF, 35 µg/mL IL-4, 1% Gentamycin) at 37 °C, 5% CO2 for 4 days. For DC maturation, 2000 U/mL of interferon-gamma (IFN-γ) and 60 U/mL of lipopolysaccharide (LPS) were added into the culture bag and the cells were kept culturing for another 24 h (GSC lysate was added at this step). Antigen source (for synthetic peptide cocktail, each peptide with final concentration of 20 µg/mL) was added into the culture bag on day 5 and the cells were incubated at 37 °C, 5% CO2 overnight (16–20 h). DCs were harvested in HBSS and their phenotype was evaluated by the flow cytometry (CD11c+/CD83+ population > 60%).
ATC generation (Loading DCs with cancer cell specific antigens)
On the same day as matured DCs were harvested, frozen naïve T cells were thawed and allowed to recover in R10 medium (RPMI1640, 10% FBS) for 2 h (Fig. 6). Then 2 × 108 cells of naïve T cells (T0) were co-cultured with 2 × 107 cells of peptide-loaded DCs in the TC:DC ratio of 10:1) in G-Rex100 container (WilsonWolf Manufacturing Corp., P/N 80,500) with 200 mL T cell culture medium (TCM: RPMI1640, 45% Click’s medium, 10% FBS, 10 ng/mL IL-7 (CellGenix, Cat.1010), 400 U/mL (35 µg/mL) IL-4 (CellGenix, Cat.1003), 1% Gentamycin) at 37 °C, 5% CO2 for rapid growth and expansion. After 2 days, 40 U/mL of IL-2 was added into the culture medium and IL-2 was replenished every other day until day 10. IL-4 and IL-7 were replenished with fresh TCM into the culture at day 5 and 10. The cells were harvested at day 12 (TNPP12 and TPP12) according to the manufacturer’s instructions and surface markers were analyzed to confirm success of activation and ELISpot assay performed on final product to measure the IFN-γ secretion towards specific tumor antigen or cancer stem cell lines from which the antigen source was derived12.
Workflow of producing tumor-associated antigens (TAA)-activated T cells. There are four main steps after isolation of monocytes and naïve T cells from donor’s leukapheresis product by elutriation. Isolated naïve T cells were cryopreserved for later use. Immature DCs were differentiated from monocytes and loaded with TAA (GSC lysate, GSC-eluted peptides or GBM-specific peptide pool) at day 4. TAA-loaded mature DCs were co-cultured with thawed naïve T cells to activate T cells specific for TAA (TAA-ATCs), followed by expansion of TAA-ATCs to obtain enough amount. TAA-unspecific ATCs were also generated by co-culturing naïve T cells with TAA-unloaded DCs. ATCs were cryopreserved at day 7 and 12 for comparison.
Characterization of activated T cells and quality control
ATCs were analyzed by flow cytometry for the surface markers including CD69, HLA-DR, CD45RO, CD154 and CD137 at day 5 and 12 in addition to CD3, CD4 and CD8. Early activation markers were noted to be highest on day 5 and maximal T cell growth was noted on day 12. Additionally, sterility testing for endotoxin, mycoplasma, gram stain and environmental culture was performed to ensure quality of the cell products for future clinical trials. Antibodies (BD Bioscience) used were anti-human CD3 (Cat. 564,810), CD4 (Cat. 555,346), CD8 (Cat. 560,662), CD69 (Cat. 562,883), HLA-DR (Cat. 564,231), CD45RO (Cat: 561,136), CD154 (Cat. 557,299) and CD137 (Cat. 561,702). Growth of ATCs was also measured along with the activation marker analysis. Maximal growth of T cells was noted to be at day 12 (data not shown).
Interferon-gamma (IFN-γ) ELISpot assay
To quantify IFN-γ secreting cells as a result of the recognition of antigens on the surface of target cells by activated T cells, autologous DC or T2 cell, which is HLA-A2 positive lymphoblast cell line, was used as antigen presenting target cell. Antigen-pulsed DCs were co-cultured with T cells activated with either tumor-lysate or acid-eluted peptides-loaded DCs. T cells activated with synthetic peptide loaded DCs were co-cultured with antigen-pulsed T2 cells (Bossi, Oncoimmunology, 2013). For preparing T2 cell targeting assay, T2 cells were cultured in IMDM medium (20% FBS, antibiotics) and antigen peptides cocktail (final concentration of 5 µg/mL for each peptide) was pulsed for 2 h. Cryopreserved T cells (pre- and post-activation) were allowed to recover in R10 medium (RPMI1640, 10% FBS, 1% Gentamycin) for 2 h. For GSC targeting assay, four GSC lines were harvested and resuspended in ELISpot medium (RPMI1640, 10% FBS, 1% Gentamycin, 20 ng/mL IL-7). These cells were transferred to ELISpot plate (MabTech, Cat. 3420-4HPT-2) at TC to T2 ratio of 2:1 and TC to GSC ratio of 1:1.5 following the manufacturer’s protocol. Each well contained 1 × 105 T cells with 200 µL medium. Additional wells for negative (medium only) and positive (anti-CD3 antibody) controls were also included. The plate was incubated at 37 °C, 5% CO2 overnight. After centrifuging at 1300 rpm for 3 min, supernatant was discarded, each well was stained according to the manufacturer’s protocol (Mabtech, Cincinnati, OH). Then the plate was sent to ZellNet Consulting (Fort Lee, NJ) for plate reading and quantification using ELISpot reading system (Carl Zeiss, Thornwood, NY). Pre- and post-activated T cells were analyzed for interferon γ-secreting T cells.
Intracellular cytokine staining
T cells from various experiment groups: T0, TNPP12 and TPP12 were cultured in complete RPMI medium, or with T2 cell (pulse with synthetic peptide pool for 2 h on rotator), or with peptide pool for 4 h, followed by adding GolgiPlug (Biolegend, San Diego, CA). To exclude dead cells, samples were stained with Live/Dead dye (Biolegend, San Diego, CA), followed by surface staining (fluorochrome-conjugated antibodies: anti-CD3, anti-CD4, and anti-CD8, Biolegend, San Diego, CA) for 30 min on ice. Cells were then fixed with Fix & Perm Cell Fixation & Permeabilization Kit (ThermoFisher) according to the instruction, stained with fluorochrome-conjugated anti-IFN-γ and anti-IL-2 (Biolegend, San Diego, CA) for 30 min on ice, washed and resuspended in staining buffer with 1% PFA, followed by flow cytometry analysis by BD LSR Fortessa (Beckman Dickinson, Franklin Lakes, NJ.). Flow cytometry data was analyzed by FlowJo (Three Star, Ashland, OR).
Generation of PHA-blasts
Autologous PHA-blasts were generated by stimulating PBMC with 5 µg/mL Phytohemagglutinin-L (PHA-L, Sigma, L2769), followed by culturing in RPMI1640 medium containing 10% FBS and 100 U/mL IL-2 (Gibco, PHC0027) in 24-well plate for about one week12,14,21. At day 3 or 4, cell growth and formation of blasts were assessed by microscopy. After 7 days of culture, PHA-blasts were harvested and frozen down in freezing medium (culture medium + 10% DMSO).
Cytotoxicity assay
HLA-A2 positive GSC line, CSC66 or HLA-A2 negative GSC line, CSC55 were cultured in serum-free neural basal medium and harvested to use in a cytotoxic assay to evaluate efficiency of cell lysis by activated T cells. U87 cell line, which is HLA-A2 positive22, was also used as a target cell in a cytotoxicity assay. Collected cancer cells were stained as target cells with 2.5 μM of CellTrace Violet (CTV) dye (ThermoFisher Scientific, C34557) for flow cytometry analysis. T cells with peptide-loaded DCs (TPP) or non-peptide loaded DCs (TNPP) were cultured for at least 2 h prior to the assay. Those T cells were co-cultured with stained cancer cells in the effector to target cells (E:T) ratio of 5:1, 10:1 and 20:1 in 6-well plate at 37 °C for 4 h or 18 h. U87 cells were split into two groups where one group was trypsinized prior to co-culture (detached), and another group was co-cultured as adherent cells (attached). Cancer cells without T cells were also incubated in the same manner to detect basal cell death for the calculation of specific cell lysis by T cells. After the incubation, cells were stained with eBioscience Fixable Viability Dye (FVD) eFluor 780 (Thermo Fisher Scientific, 65–0865) and fixed with 4% formaldehyde, followed by filtering through 70 μm and 40 μm cell strainers. Single cell suspension was transferred to FACS tube and stored at 4 °C protected from light until use in flow cytometry analysis. Percentages of dead cancer cells (CTV-positive/FVD-positive) were measured by BD LSRFortessa flow cytometry. The percentage of specific lysis was calculated as below58.
Testing for autoimmune responses
Thawed autologous PHA-blasts were cultured in RPMI1640 medium containing 10% FBS and 100 U/mL IL-2 in 24-well plate for 1 to 3 days prior to use in a cytotoxic assay to evaluate autoimmune effect by activated autologous T cells. Collected PHA-blasts were stained as target cells with 2.5 μM of CellTrace Violet (CTV) dye (ThermoFisher Scientific, C34557) for flow cytometry analysis. T cells with peptide-loaded DCs or non-peptide loaded DCs were cultured for at least 2 h prior to the assay. Those T cells were co-cultured with stained PHA-blasts in the effector to target cells (E:T) ratio of 20:1 in 6-well plate at 37 °C for 4 h21. PHA-blasts without T cells were also incubated in the same manner to detect basal cell death for the calculation of specific cell lysis by T cells. After the incubation, cells were stained with eBioscience Fixable Viability Dye (FVD) eFluor 780 (Thermo Fisher Scientific, 65–0865) and fixed with 4% formaldehyde, followed by filtering through 70 μm and 40 μm cell strainers. Single cell suspension was transferred to FACS tube and stored at 4 °C protected from light until use in flow cytometry analysis. Percentages of dead PHA-blast cells (CTV-positive/FVD-positive) were measured by BD LSRFortessa flow cytometry. The percentage of specific lysis was calculated by the same equation used for cytotoxicity assay58.
Comparison of incubation times for cytotoxicity assay
Frozen TPP cells were thawed and cultured for at least 2 h prior to the cytotoxicity assay described above. T cells were co-cultured with stained GSCs in the effector to target cells (E:T) ratio of 20:1 in 6-well plate at 37 °C for 4 h (short incubation) and 18 h (long incubation). GSCs without T cells were also incubated in the same manner to detect basal cell death for the calculation of specific cell lysis by T cells. After the incubation, cells were stained and analyzed by flow cytometry in the same manner as described above. % specific lysis between short incubation and long incubation was compared.
Statistical analysis
ELISpot data were analyzed with two-way ANOVA followed by Tukey’s test to adjust for multiple group comparisons. Cytotoxicity data were analyzed with Student’s t-test. Residuals were inspected to confirm homoscedasticity and normality. Data were considered significant where p < 0.05. Data are presented as means + / − standard deviation (SD). Analysis performed with GraphPad software (v9.1). Each experiment was performed with at least triplicate replicates.
Data availability
All data generated in this study are available from the corresponding author on reasonable request.
References
Ostrom, Q. T. et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2012–2016. Neuro. Oncol. 21, v1–v100. https://doi.org/10.1093/neuonc/noz150 (2019).
Choi, B. D., Maus, M. V., June, C. H. & Sampson, J. H. Immunotherapy for Glioblastoma: Adoptive T-cell Strategies. Clin. Cancer Res. 25, 2042–2048. https://doi.org/10.1158/1078-0432.CCR-18-1625 (2019).
Waldman, A. D., Fritz, J. M. & Lenardo, M. J. A guide to cancer immunotherapy: From T cell basic science to clinical practice. Nat. Rev. Immunol. 20, 651–668. https://doi.org/10.1038/s41577-020-0306-5 (2020).
Hoteit, M. et al. Cancer immunotherapy: A comprehensive appraisal of its modes of application. Oncol. Lett. 22, 655. https://doi.org/10.3892/ol.2021.12916 (2021).
Akkin, S., Varan, G. & Bilensoy, E. A review on cancer immunotherapy and applications of nanotechnology to chemoimmunotherapy of different cancers. Molecules 26, 3382. https://doi.org/10.3390/molecules26113382 (2021).
Yu, J. S. et al. Vaccination of malignant glioma patients with peptide-pulsed dendritic cells elicits systemic cytotoxicity and intracranial T-cell infiltration. Cancer Res. 61, 842–847 (2001).
Yu, J. S. et al. Vaccination with tumor lysate-pulsed dendritic cells elicits antigen-specific, cytotoxic T-cells in patients with malignant glioma. Cancer Res. 64, 4973–4979. https://doi.org/10.1158/0008-5472.CAN-03-3505 (2004).
Wheeler, C. J. et al. Vaccination elicits correlated immune and clinical responses in glioblastoma multiforme patients. Cancer Res. 68, 5955–5964. https://doi.org/10.1158/0008-5472.CAN-07-5973 (2008).
Phuphanich, S. et al. Phase I trial of a multi-epitope-pulsed dendritic cell vaccine for patients with newly diagnosed glioblastoma. Cancer Immunol. Immunother. 62, 125–135. https://doi.org/10.1007/s00262-012-1319-0 (2013).
Wen, P. Y. et al. A randomized double-blind placebo-controlled phase II trial of dendritic cell vaccine ICT-107 in newly diagnosed patients with glioblastoma. Clin. Cancer Res. 25, 5799–5807. https://doi.org/10.1158/1078-0432.CCR-19-0261 (2019).
Borst, J., Ahrends, T., Babala, N., Melief, C. J. M. & Kastenmuller, W. CD4(+) T cell help in cancer immunology and immunotherapy. Nat. Rev. Immunol. 18, 635–647. https://doi.org/10.1038/s41577-018-0044-0 (2018).
Gerdemann, U. et al. Cytotoxic T lymphocytes simultaneously targeting multiple tumor-associated antigens to treat EBV negative lymphoma. Mol. Ther. 19, 2258–2268. https://doi.org/10.1038/mt.2011.167 (2011).
Osen, W. et al. Screening of human tumor antigens for CD4 T cell epitopes by combination of HLA-transgenic mice, recombinant adenovirus and antigen peptide libraries. PLoS One 5, e14137. https://doi.org/10.1371/journal.pone.0014137 (2010).
Gerdemann, U. et al. Rapidly generated multivirus-specific cytotoxic T lymphocytes for the prophylaxis and treatment of viral infections. Mol. Ther. 20, 1622–1632. https://doi.org/10.1038/mt.2012.130 (2012).
Harada, M. et al. Melanoma-reactive CD8+ T cells recognize a novel tumor antigen expressed in a wide variety of tumor types. J. Immunother. 24, 323–333. https://doi.org/10.1097/00002371-200107000-00008 (2001).
Liu, G. et al. AIM-2: A novel tumor antigen is expressed and presented by human glioma cells. J. Immunother. 27, 220–226. https://doi.org/10.1097/00002371-200405000-00006 (2004).
Parkhurst, M. R. et al. Improved induction of melanoma-reactive CTL with peptides from the melanoma antigen gp100 modified at HLA-A*0201-binding residues. J. Immunol. 157, 2539–2548 (1996).
Schaed, S. G. et al. T-cell responses against tyrosinase 368–376(370D) peptide in HLA*A0201+ melanoma patients: Randomized trial comparing incomplete Freund’s adjuvant, granulocyte macrophage colony-stimulating factor, and QS-21 as immunological adjuvants. Clin. Cancer Res. 8, 967–972 (2002).
Akiyama, Y. et al. Alpha-type-1 polarized dendritic cell-based vaccination in recurrent high-grade glioma: A phase I clinical trial. BMC Cancer 12, 623. https://doi.org/10.1186/1471-2407-12-623 (2012).
Nelson, N. et al. A cell-engineered system to assess tumor cell sensitivity to CD8(+) T cell-mediated cytotoxicity. Oncoimmunology 8, 1599635. https://doi.org/10.1080/2162402X.2019.1599635 (2019).
Weber, G. et al. Generation of tumor antigen-specific T cell lines from pediatric patients with acute lymphoblastic leukemia–implications for immunotherapy. Clin. Cancer Res. 19, 5079–5091. https://doi.org/10.1158/1078-0432.CCR-13-0955 (2013).
Wu, A. H., Hall, W. A. & Low, W. C. Identification of HLA a*0201 glioblastoma multiforme cell lines for immunotherapy by PCR-SSP and DNA sequencing. J. Neurooncol. 66, 1–8. https://doi.org/10.1023/b:neon.0000013460.53527.28 (2004).
Rojas-Sepulveda, D. et al. Tumor lysate-based vaccines: on the road to immunotherapy for gallbladder cancer. Cancer Immunol. Immunother. 67, 1897–1910. https://doi.org/10.1007/s00262-018-2157-5 (2018).
Parney, I. F. et al. Novel strategy for manufacturing autologous dendritic cell/allogeneic tumor lysate vaccines for glioblastoma. Neurooncol. Adv. 2, vdaa105. https://doi.org/10.1093/noajnl/vdaa105 (2020).
Gonzalez, F. E. et al. Tumor cell lysates as immunogenic sources for cancer vaccine design. Hum. Vaccin. Immunother. 10, 3261–3269. https://doi.org/10.4161/21645515.2014.982996 (2014).
Delluc, S. et al. DC-based vaccine loaded with acid-eluted peptides in acute myeloid leukemia: The importance of choosing the best elution method. Cancer Immunol. Immunother. 56, 1–12. https://doi.org/10.1007/s00262-006-0170-6 (2007).
Herr, W. et al. Mature dendritic cells pulsed with freeze-thaw cell lysates define an effective in vitro vaccine designed to elicit EBV-specific CD4(+) and CD8(+) T lymphocyte responses. Blood 96, 1857–1864 (2000).
Boyd, A. et al. Pathogen-specific T cell polyfunctionality is a correlate of T cell efficacy and immune protection. PLoS One 10, e0128714. https://doi.org/10.1371/journal.pone.0128714 (2015).
Imai, N., Ikeda, H., Tawara, I. & Shiku, H. Tumor progression inhibits the induction of multifunctionality in adoptively transferred tumor-specific CD8+ T cells. Eur. J. Immunol. 39, 241–253. https://doi.org/10.1002/eji.200838824 (2009).
Quah, B. J., Wijesundara, D. K., Ranasinghe, C. & Parish, C. R. Fluorescent target array killing assay: a multiplex cytotoxic T-cell assay to measure detailed T-cell antigen specificity and avidity in vivo. Cytom. A 81, 679–690. https://doi.org/10.1002/cyto.a.22084 (2012).
Tempany, J. C., Zhou, J. H., Hodgkin, P. D. & Bryant, V. L. Superior properties of Cell Trace Yellow as a division tracking dye for human and murine lymphocytes. Immunol. Cell Biol. 96, 149–159. https://doi.org/10.1111/imcb.1020 (2018).
Wallace, D., Hildesheim, A. & Pinto, L. A. Comparison of benchtop microplate beta counters with the traditional gamma counting method for measurement of chromium-51 release in cytotoxic assays. Clin. Diagn. Lab. Immunol. 11, 255–260. https://doi.org/10.1128/cdli.11.2.255-260.2004 (2004).
Chan, J. K. et al. Enhanced killing of primary ovarian cancer by retargeting autologous cytokine-induced killer cells with bispecific antibodies: A preclinical study. Clin. Cancer Res. 12, 1859–1867. https://doi.org/10.1158/1078-0432.CCR-05-2019 (2006).
Yee, C. et al. Melanocyte destruction after antigen-specific immunotherapy of melanoma: Direct evidence of t cell-mediated vitiligo. J. Exp. Med. 192, 1637–1644. https://doi.org/10.1084/jem.192.11.1637 (2000).
Dudley, M. E. et al. Cancer regression and autoimmunity in patients after clonal repopulation with antitumor lymphocytes. Science 298, 850–854. https://doi.org/10.1126/science.1076514 (2002).
Tey, S. K. Adoptive T-cell therapy: adverse events and safety switches. Clin. Transl. Immunol. 3, e17. https://doi.org/10.1038/cti.2014.11 (2014).
Yuan, X. et al. Isolation of cancer stem cells from adult glioblastoma multiforme. Oncogene 23, 9392–9400. https://doi.org/10.1038/sj.onc.1208311 (2004).
Lee, J. et al. Tumor stem cells derived from glioblastomas cultured in bFGF and EGF more closely mirror the phenotype and genotype of primary tumors than do serum-cultured cell lines. Cancer Cell 9, 391–403. https://doi.org/10.1016/j.ccr.2006.03.030 (2006).
Zitvogel, L. et al. Therapy of murine tumors with tumor peptide-pulsed dendritic cells: dependence on T cells, B7 costimulation, and T helper cell 1-associated cytokines. J. Exp. Med. 183, 87–97. https://doi.org/10.1084/jem.183.1.87 (1996).
Tatsumi, T. et al. Disease stage variation in CD4+ and CD8+ T-cell reactivity to the receptor tyrosine kinase EphA2 in patients with renal cell carcinoma. Cancer Res. 63, 4481–4489 (2003).
Pollack, I. F. et al. Antigen-specific immune responses and clinical outcome after vaccination with glioma-associated antigen peptides and polyinosinic-polycytidylic acid stabilized by lysine and carboxymethylcellulose in children with newly diagonised malignant brainstem and nonbrainstem gliomas. J. Clin. Oncol. 32, 2050–2058. https://doi.org/10.1200/JCO.2013.54.0526 (2014).
Nguyen-Hoai, T. et al. CCL21 (SLC) improves tumor protection by a DNA vaccine in a Her2/neu mouse tumor model. Cancer Gene Ther. 19, 69–76. https://doi.org/10.1038/cgt.2011.69 (2012).
Mintz, A., Gibo, D. M., Slagle-Webb, B., Christensen, N. D. & Debinski, W. IL-13Ralpha2 is a glioma-restricted receptor for interleukin-13. Neoplasia 4, 388–399. https://doi.org/10.1038/sj.neo.7900234 (2002).
Okano, F., Storkus, W. J., Chambers, W. H., Pollack, I. F. & Okada, H. Identification of a novel HLA-A*0201-restricted, cytotoxic T lymphocyte epitope in a human glioma-associated antigen, interleukin 13 receptor alpha2 chain. Clin. Cancer Res. 8, 2851–2855 (2002).
Liu, G. et al. HER-2, gp100, and MAGE-1 are expressed in human glioblastoma and recognized by cytotoxic T cells. Cancer Res. 64, 4980–4986. https://doi.org/10.1158/0008-5472.CAN-03-3504 (2004).
Ottaviani, S., Zhang, Y., Boon, T. & van der Bruggen, P. A MAGE-1 antigenic peptide recognized by human cytolytic T lymphocytes on HLA-A2 tumor cells. Cancer Immunol. Immunother. 54, 1214–1220. https://doi.org/10.1007/s00262-005-0705-2 (2005).
Shraibman, B., Kadosh, D. M., Barnea, E. & Admon, A. Human leukocyte antigen (HLA) peptides derived from tumor antigens induced by inhibition of DNA methylation for development of drug-facilitated immunotherapy. Mol. Cell Proteomics 15, 3058–3070. https://doi.org/10.1074/mcp.M116.060350 (2016).
Wargo, J. A. et al. Recognition of NY-ESO-1+ tumor cells by engineered lymphocytes is enhanced by improved vector design and epigenetic modulation of tumor antigen expression. Cancer Immunol. Immunother. 58, 383–394. https://doi.org/10.1007/s00262-008-0562-x (2009).
Liu, Z. et al. NY-ESO-1- and survivin-specific T-cell responses in the peripheral blood from patients with glioma. Cancer Immunol. Immunother. 67, 237–246. https://doi.org/10.1007/s00262-017-2066-z (2018).
Liu, G. et al. Molecular and functional analysis of tyrosinase-related protein (TRP)-2 as a cytotoxic T lymphocyte target in patients with malignant glioma. J. Immunother. 26, 301–312. https://doi.org/10.1097/00002371-200307000-00002 (2003).
Liu, G. et al. Cytotoxic T cell targeting of TRP-2 sensitizes human malignant glioma to chemotherapy. Oncogene 24, 5226–5234. https://doi.org/10.1038/sj.onc.1208519 (2005).
Kobayashi, H., Lu, J. & Celis, E. Identification of helper T-cell epitopes that encompass or lie proximal to cytotoxic T-cell epitopes in the gp100 melanoma tumor antigen. Cancer Res. 61, 7577–7584 (2001).
Knutson, K. L., Schiffman, K. & Disis, M. L. Immunization with a HER-2/neu helper peptide vaccine generates HER-2/neu CD8 T-cell immunity in cancer patients. J. Clin. Invest. 107, 477–484. https://doi.org/10.1172/JCI11752 (2001).
Davis, I. D., Jefford, M., Parente, P. & Cebon, J. Rational approaches to human cancer immunotherapy. J. Leukoc. Biol. 73, 3–29. https://doi.org/10.1189/jlb.0502261 (2003).
Kobayashi, H., Wood, M., Song, Y., Appella, E. & Celis, E. Defining promiscuous MHC class II helper T-cell epitopes for the HER2/neu tumor antigen. Cancer Res 60, 5228–5236 (2000).
Matsuzaki, J. et al. Recognition of naturally processed and ovarian cancer reactive CD8+ T cell epitopes within a promiscuous HLA class II T-helper region of NY-ESO-1. Cancer Immunol. Immunother. 57, 1185–1195. https://doi.org/10.1007/s00262-008-0450-4 (2008).
Paschen, A. et al. Detection of spontaneous CD4+ T-cell responses in melanoma patients against a tyrosinase-related protein-2-derived epitope identified in HLA-DRB1*0301 transgenic mice. Clin. Cancer Res. 11, 5241–5247. https://doi.org/10.1158/1078-0432.CCR-05-0170 (2005).
Lecoeur, H., Fevrier, M., Garcia, S., Riviere, Y. & Gougeon, M. L. A novel flow cytometric assay for quantitation and multiparametric characterization of cell-mediated cytotoxicity. J. Immunol. Meth. 253, 177–187. https://doi.org/10.1016/s0022-1759(01)00359-3 (2001).
Author information
Authors and Affiliations
Contributions
Conception and design: K.M., H.W., J.S.Y. Development of methodology: K.M., H.W. Acquisition of data: K.M., H.W. Analysis and interpretation of data: K.M., H.W., J.S.Y. Writing, review, and/or revision of the manuscript: K.M., H.W., K.L.B., S.L.S., R.W., J.S.Y. Study supervision: K.L.B., S.L.S., R.W., J.S.Y.
Corresponding author
Ethics declarations
Competing interests
Authors K.L.B. and J.S.Y. have a patent on this technology that was licensed to Kairos Pharma, Ltd. J.S.Y. has stock ownership and is an officer of Kairos Pharma, Ltd. No potential conflicts of interest were disclosed by the other authors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Miyaguchi, K., Wang, H., Black, K.L. et al. Activated T cell therapy targeting glioblastoma cancer stem cells. Sci Rep 13, 196 (2023). https://doi.org/10.1038/s41598-022-27184-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-27184-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.