Abstract
The study investigated the seasonal variations of presenting symptoms and signs of dry eye disease (DED) in Norway. 652 consecutive DED patients examined between August 2012 and May 2015 in Oslo, Norway, were included. Presenting symptoms and signs were related to the season according to when each patient was examined. Weather report data from the examination day were compared with the presenting symptoms and signs. Oslo's mean seasonal temperatures during spring, summer, fall, and winter were 6.4 °C, 15.6 °C, 9.3 °C, and − 2.1 °C, respectively. Dry eye severity level and self-reported symptoms measured by the Ocular surface disease index questionnaire did not differ between seasons. Schirmer I was lower during summer than in other seasons (P < 0.01). The percentage of patients with a pathological tear meniscus height (< 0.2 mm) was higher during fall (P < 0.01) and lower during winter (P < 0.05) compared to the other seasons. Signs and symptoms of DED generally did not correlate with weather report data, although intraocular pressure was weakly associated with mean daily air temperature (r = − 0.22; P < 0.001). Neither dry eye severity level nor dry eye symptoms differ between seasons in Oslo, Norway. However, some parameters for assessing DED show seasonal variations (Schirmer I and tear meniscus height), which are essential to consider when examining patients with DED.
Similar content being viewed by others
Introduction
The hallmark of dry eye disease (DED) is hyperosmolar tears due to tear evaporation1, which initiates ocular surface damage and inflammation. The pathogenesis includes a cascade of events that leads to goblet cell/epithelial cell damage, loss of glycocalyx, and the recruitment of T-lymphocytes1. The prevalence of DED is estimated to range between 5 and 50%, depending on the populations studied and criteria used, and increases with age and female sex2. Dry eye symptoms in terms of burning, dry, gritty, itching, irritated, sandy, and tired eyes are among the most commonly reported complaints in the eye clinic3. The two main forms of DED are the aqueous deficiency and the evaporative type1. Aqueous deficiency can be seen in Sjögren’s syndrome and after radiation therapy to the lacrimal glands. Causes of evaporative DED are either endogenous, i.e., meibomian gland dysfunction (MGD), or external, i.e., environmental factors. Environmental causes of dry eyes consist of low humidity, wind, air pollution, and allergens4,5. It has been proposed that DED patients are susceptible to environmental changes6.
As a range of environmental factors can aggravate DED, it is expected that patients with DED show seasonal variation in their severity of symptoms and signs of dry eyes. In a large multicenter study by Kumar and co-workers that included 3.4 million consultations across the continental United States (US), the prevalence of dry eyes in US veterans was highest during winter/spring and lowest during summer7. The highest monthly prevalence was seen during April. Also, in a study from the Greater Boston Area, U.S., the severity of symptoms of dry eyes was found to be highest during winter8. In Bologna, Italy, symptoms of ocular discomfort were reported to be highest between November and February and between June and August5. Based on Google trend data in the United States, Canada, United Kingdom, and Australia, dry eyes searches on the internet also showed a slight seasonal variation with the highest incidence during summer9. In a multicenter study in Japan, on the other hand, no seasonal variation was found in the prevalence of DED6. A Danish study also reported a lack of variation in the prevalence of dry eyes, as indicated by reduced break-up time and increased lissamine green staining during winter compared to summer10. Thus, there are conflicting reports concerning seasonal variation in DED.
The current study represents the largest single-center study on seasonal variation of DED severity. It includes 652 patients examined at the Norwegian Dry Eye Clinic in Oslo between August 2012 and May 2015. Furthermore, it is the first to investigate if MGD, the most common cause of DED, displays seasonal variation.
Results
Patient demographics
Patient demographics are shown in Table 1.
Seasonal weather data
Weather report data from Oslo are summarized in Table 2.
Correlations between weather report data and clinical tests
Weather report data correlated the strongest with intraocular pressure, which was weakly associated with mean air temperature (C°) (r = − 0.22; P < 0.001), and wind speed (r = − 0.14; P < 0.015) (Table 3). Tear meniscus height correlated weakly with mean air temperature (r = − 0.12; P = 0.004). Dry eye severity level was marginally associated with relative air humidity (%) (r = 0.09; P = 0.032). Symptoms of DED as measured by the self-reported OSDI were not associated with any of the weather report data parameters.
Symptoms and signs of dry eye disease according to season
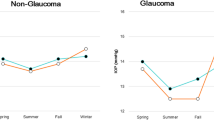
Neither self-reported symptom load (OSDI) nor dry eye severity level (DESL) differed between seasons (Table 4). Schirmer I was lower during summer than during all other seasons (P < 0.01). The percentage of patients with tear meniscus height < 0.2 mm was higher during fall (29%) compared to other seasons (P < 0.001). Intraocular pressure was higher during winter than during summer and fall (P < 0.05).
Discussion
Understanding factors that are associated with DED is important for accurate diagnosis, and optimal treatment, of dry eye. Environmental factors such as high altitude11,12, exposure to wind13, air pollution13,14, and low relative humidity15 have been suggested to impact the DED. The current study was performed to assess whether parameters used in clinical DES diagnosis have a seasonal pattern. We hypothesized that seasonal environmental changes in temperature and humidity affect clinical parameters.
In the current study, DESL did not vary according to season. This is in line with two studies from Japan and Denmark, where no seasonal variation in the prevalence of DED could be found6,10. The lack of a consistent seasonal variation in DED could be related to a geographical impact. In the US, the prevalence of DED appeared higher in the southern regions16. In our study, all patients were examined at a single location. Hence no conclusions on regional effects can be drawn. Although the prevalence of DED was not investigated in our study, an increased prevalence of DED would be expected to be associated with a higher mean DESL. A large multicenter study that included 3.4 million consultations across the continental United States, on the other hand, did show a higher prevalence of dry eyes in US veterans during winter/spring than during summer7. The authors attributed the higher prevalence to be related to allergen exposure. Unfortunately, data on air allergen levels were not available for comparison in the present study. Dry eye severity level was only weakly related to higher specific humidity and was not associated with mean air temperature, average wind speed, or daily hours of sunshine in our study. The lack of associations between DESL, seasons, and weather report data in our study could be partly explained by the fact that the majority of the patients were classified as having DESL 2 (78%, data not shown). DESL is scored using a four-level system, thus, potential minute variations in DED severity may not have been detected with this scoring system.
In our study, self-reported symptoms of dry eyes, as measured by OSDI, did not show significant differences throughout the four seasons or with any single one of the weather report parameters. In the Greater Boston area, symptoms of dry eyes worsened during winter, which the authors speculated was related to more windy conditions, lower humidity, and lower air temperature8. A survey-based study in Sweden demonstrated that 47% of patients suffering from dry eye and/or Sjögren’s syndrome reported that they had the impression that seasonal conditions had a high impact on their DED symptoms, compared to only 15% reporting no presumed seasonal impact17. Wind (71%), followed by sunshine (60%) and heat (42%), were the most common weather conditions to reportedly impact on dry eye symptoms. In addition, cold weather also was suggested to aggravate DED symptoms in 34% of patients. The general lack of moderate/strong associations between symptoms of DED and weather conditions in our study, may, however, indicate that these environmental factors do not affect symptoms of DED to any large extent. Other factors, including allergen exposure and air pollution, were not assessed in this study but could represent relatively more important contributions to DED symptoms.
Signs of DED did not show a uniform variation throughout the various seasons in this study. Schirmer I and tear meniscus height were the only DED signs that were significantly correlated with season or weather report data. Schirmer I was lower during Summer compared to the remaining year. The known induction of tear secretion through the activation of corneal cold thermoreceptors could support this finding18. We also found a more pathological tear meniscus height during fall, a season during which relative air humidity is high in Oslo. Hence, this result is surprising given that tear evaporation is inversely related to relative air humidity19. Thus, there must be other aggravating factors that reduce tear meniscus height during the fall season in Oslo. A reduced ambient temperature during fall could increase meibomian lipid viscosity and inhibit meibomian gland secretion, thereby promoting tear evaporation due to a thinner tear lipid layer.
Intraocular pressure has been shown to increase during winter in normotensive individuals20 and in patients with ocular hypertension21,22. The approximately 2 mmHg increase in IOP during winter compared to summer in the current study is similar to what was shown in other studies on normotensive patients20,23. The mechanism of higher IOP during winter has been hypothesized to be related to the pineal hormone melatonin, as its secretion is inhibited by light and therefore reduced during summer21.
Surprisingly, meibum expressibility was not associated with the current season or air temperature in our study. This was expected since meibomian lipid viscosity, and its expressibility is related to temperature24. Other reports have shown higher meibum secretion following increased eyelid temperature by application of warm compresses. Apparently, warm compresses reduce secrete stagnation by offering a short-term decrease in lipid viscosity. As meibum expression was not reduced during winter, other factors may counteract the effect of temperature on lipid viscosity. Consumption of dietary omega-3 fatty acids has been demonstrated to improve symptoms of MGD25. Proposed mechanisms include the reduction of inflammation and alteration of the meibomian lipid composition25. A study from Belgium demonstrated lower serum levels of omega-3 fatty acids during winter than summer26, which would be expected to exacerbate MGD during winter. To our knowledge, the variation of serum level of omega-3 fatty acids throughout the year in a Norwegian population has not been reported. Finally, the ambient temperature in the offices of the Norwegian Dry Eye Clinic was not measured. However, it is reasonable to assume that it stayed relatively constant throughout the year. Still, the indoor temperature may be somewhat more important than the outdoor temperature regarding meibum expression. The latter may be significant to consider during the colder seasons in Norway, during which people tend to stay indoors.
In conclusion, there was no apparent seasonal variation in the level of dry eye severity or self-reported symptoms of dry eyes in patients being examined in Oslo, Norway. Certain parameters for assessing DED, on the other hand, did show seasonal variations that should be considered when diagnosing DED. Further studies including parameters on the indoor environment, as well as allergens and air pollution, could shed more light on the magnitude of external influences on DED.
Methods
Patients
The study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients. The Regional Committee for Medical & Health Research Ethics, Section C, South East Norway (REC) reviewed the use of the data for the study from the Norwegian Dry Eye Clinic. REC determined that the research project “Evaluation of data from the Norwegian Dry Eye Clinic” is outside the remit of the Act on Medical and Health Research (2008) and therefore can be conducted without its approval. A letter of exemption by REC is provided. The study consecutively included patients with dry eye symptoms that were examined for the first time at the Norwegian Dry Eye Disease Clinic in Oslo, Norway, between August 2012 and May 2015. Patients without symptoms of dry eye were excluded.
Ophthalmological examination
All included subjects were examined by one of two ophthalmologists at the clinic and completed a self-report questionnaire on symptoms of ocular dryness (Ocular Surface Disease Index [OSDI]). The OSDI questionnaire includes 12 items on symptoms of ocular dryness, as reported elsewhere27. All examinations were performed between 9 a.m. and 4 p.m. The ophthalmological examination consisted of measuring tear film break-up time (TFBUT)28,29, ocular staining (lissamine green and fluorescein)30, meibum expressibility31, Schirmer I28, tear meniscus height, and intraocular pressure measured with iCare tonometer. The ocular protection index (OPI)29 and dry eye severity level (DESL) (Table 5)32 were evaluated based on the measurements. In this study, meibomian gland dysfunction was defined as having a pathological score (> 0) on meibum expressibility. Only scores from the right eye of each subject were used for analyses.
Meteorological data
Presenting symptoms and signs in each patient were related to the mean weather report data from Oslo during the season in which the patient had been examined. Spring was defined as March, April, and May, summer as June, July, and August, fall as September, October, and November, and winter as December, January, and February. The weather report data were obtained from the Norwegian Meteorological Institute and included air temperature, relative air humidity, hours of sunshine, and wind speed. In addition, weather report data from the exact day of examination in Oslo were correlated with the presenting symptoms and signs.
Statistical analyses
Data are presented as mean ± standard deviation (SD). One-way analysis of variance with Tukey post hoc test (continuous variables) and chi-square test (dichotomous variables) was used for comparing symptoms and signs of DED during any one season with the rest of the year. Pearson’s correlation coefficient (r) was used for correlating weather report data with symptoms and signs of DED. P < 0.05 was considered significant (SPSS ver. 21.0).
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DED:
-
Dry eye disease
- MGD:
-
Meibomian gland dysfunction
- REC:
-
The Regional Committee for Medical & Health Research Ethics, Section C, South East Norway
- OSDI:
-
Ocular surface disease index
- TFBUT:
-
Tear film break-up time
- OPI:
-
Ocular protection index
- DESL:
-
Dry eye severity level
References
Bron, A. J. et al. TFOS DEWS II pathophysiology report. Ocul. Surf. 15, 438–510. https://doi.org/10.1016/j.jtos.2017.05.011 (2017).
Stapleton, F. et al. TFOS DEWS II epidemiology report. Ocul. Surf. 15, 334–365. https://doi.org/10.1016/j.jtos.2017.05.003 (2017).
O’Brien, P. D. & Collum, L. M. Dry eye: Diagnosis and current treatment strategies. Curr. Allergy Asthma Rep. 4, 314–319 (2004).
McCulley, J. P., Uchiyama, E., Aronowicz, J. D. & Butovich, I. A. Impact of evaporation on aqueous tear loss. Trans. Am. Ophthalmol. Soc. 104, 121–128 (2006).
Versura, P., Profazio, V., Cellini, M., Torreggiani, A. & Caramazza, R. Eye discomfort and air pollution. Ophthalmologica 213, 103–109 (1999).
Hikichi, T. et al. Prevalence of dry eye in Japanese eye centers. Graefes Arch. Clin. Exp. Ophthalmol. 233, 555–558 (1995).
Kumar, N., Feuer, W., Lanza, N. L. & Galor, A. Seasonal variation in dry eye. Ophthalmology 122, 1727–1729. https://doi.org/10.1016/j.ophtha.2015.02.013 (2015).
Davis, J. A. et al. In ARVO, vol. 47 (Investigative Ophthalmology & Visual Science, 2006).
Leffler, C. T., Davenport, B. & Chan, D. Frequency and seasonal variation of ophthalmology-related internet searches. Can. J. Ophthalmol. 45, 274–279. https://doi.org/10.3129/i10-022 (2010).
Franck, C. & Palmvang, I. B. Break-up time and lissamine green epithelial damage in “office eye syndrome”. Six-month and one-year follow-up investigations. Acta Ophthalmol. (Copenh.) 71, 62–64 (1993).
Lu, P. et al. Dry eye syndrome in elderly Tibetans at high altitude: A population-based study in China. Cornea 27, 545–551. https://doi.org/10.1097/ICO.0b013e318165b1b7 (2008).
Willmann, G. et al. Exposure to high altitude alters tear film osmolarity and breakup time. High Alt. Med. Biol. 15, 203–207. https://doi.org/10.1089/ham.2013.1103 (2014).
Sahai, A. & Malik, P. Dry eye: Prevalence and attributable risk factors in a hospital-based population. Indian J. Ophthalmol. 53, 87–91 (2005).
Torricelli, A. A. et al. Correlation between signs and symptoms of ocular surface dysfunction and tear osmolarity with ambient levels of air pollution in a large metropolitan area. Cornea 32, e11-15. https://doi.org/10.1097/ICO.0b013e31825e845d (2013).
Abusharha, A. A. & Pearce, E. I. The effect of low humidity on the human tear film. Cornea 32, 429–434. https://doi.org/10.1097/ICO.0b013e31826671ab (2013).
McCann, P. et al. Prevalence and incidence of dry eye and meibomian gland dysfunction in the United States: A systematic review and meta-analysis. JAMA Ophthalmol. https://doi.org/10.1001/jamaophthalmol.2022.4394 (2022).
van Setten, G., Labetoulle, M., Baudouin, C. & Rolando, M. Evidence of seasonality and effects of psychrometry in dry eye disease. Acta Ophthalmol. https://doi.org/10.1111/aos.12985 (2016).
Parra, A. et al. Ocular surface wetness is regulated by TRPM8-dependent cold thermoreceptors of the cornea. Nat. Med. 16, 1396–1399. https://doi.org/10.1038/nm.2264 (2010).
Uchiyama, E., Aronowicz, J. D., Butovich, I. A. & McCulley, J. P. Increased evaporative rates in laboratory testing conditions simulating airplane cabin relative humidity: An important factor for dry eye syndrome. Eye Contact Lens 33, 174–176. https://doi.org/10.1097/01.icl.0000252881.04636.5e (2007).
Blumenthal, M., Blumenthal, R., Peritz, E. & Best, M. Seasonal variation in intraocular pressure. Am. J. Ophthalmol. 69, 608–610 (1970).
Qureshi, I. A. et al. Seasonal and diurnal variations of ocular pressure in ocular hypertensive subjects in Pakistan. Singap. Med. J. 40, 345–348 (1999).
Gardiner, S. K., Demirel, S., Gordon, M. O., Kass, M. A., Ocular Hypertension Treatment Study, G. Seasonal changes in visual field sensitivity and intraocular pressure in the ocular hypertension treatment study. Ophthalmology 120, 724–730. https://doi.org/10.1016/j.ophtha.2012.09.056 (2013).
Bengtsson, B. Some factors affecting the distribution of intraocular pressures in a population. Acta Ophthalmol. (Copenh.) 50, 33–46 (1972).
Butovich, I. A., Arciniega, J. C. & Wojtowicz, J. C. Meibomian lipid films and the impact of temperature. Investig. Ophthalmol. Vis. Sci. 51, 5508–5518. https://doi.org/10.1167/iovs.10-5419 (2010).
Thode, A. R. & Latkany, R. A. Current and emerging therapeutic strategies for the treatment of meibomian gland dysfunction (MGD). Drugs 75, 1177–1185. https://doi.org/10.1007/s40265-015-0432-8 (2015).
De Vriese, S. R., Christophe, A. B. & Maes, M. In humans, the seasonal variation in poly-unsaturated fatty acids is related to the seasonal variation in violent suicide and serotonergic markers of violent suicide. Prostaglandins Leukot. Essent. Fatty Acids 71, 13–18. https://doi.org/10.1016/j.plefa.2003.12.002 (2004).
Schiffman, R. M., Christianson, M. D., Jacobsen, G., Hirsch, J. D. & Reis, B. L. Reliability and validity of the Ocular Surface Disease Index. Arch. Ophthalmol. 118, 615–621 (2000).
Bron, A. J. Diagnosis of dry eye. Surv. Ophthalmol. 45(Suppl 2), S221-226 (2001).
Ousler, G. W. 3rd., Hagberg, K. W., Schindelar, M., Welch, D. & Abelson, M. B. The ocular protection index. Cornea 27, 509–513. https://doi.org/10.1097/ICO.0b013e31816583f6 (2008).
Bron, A. J., Evans, V. E. & Smith, J. A. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea 22, 640–650 (2003).
Nichols, K. K. et al. The international workshop on meibomian gland dysfunction: Executive summary. Investig. Ophthalmol. Vis. Sci. 52, 1922–1929. https://doi.org/10.1167/iovs.10-6997a (2011).
The Definition and Classification of Dry Eye Disease. Report of the definition and classification subcommittee of the international dry eye workshop (2007). Ocul. Surf. 5, 75–92. https://doi.org/10.1016/s1542-0124(12)70081-2 (2007).
Author information
Authors and Affiliations
Contributions
T.P.U. supervised the project. S.R. examined the patients. J.R.E. analyzed the data. J.R.E., X.C., R.A.B., and T.P.U. wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eidet, J.R., Chen, X., Ræder, S. et al. Seasonal variations in presenting symptoms and signs of dry eye disease in Norway. Sci Rep 12, 21046 (2022). https://doi.org/10.1038/s41598-022-25557-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-25557-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.