Abstract
We compared the outcomes of robotic-assisted partial nephrectomy (RPN) and open partial nephrectomy (OPN) using contemporary data to respond to unmet clinical needs. Data from patients included in the registry who underwent partial nephrectomy between January 01, 2014 and June 30, 2017 within 20 centres of the French Network for Research on Kidney Cancer UroCCR were collected (NCT03293563). Statistical methods included adjusted multivariable analyses. Rates of peri- and post-operative transfusion, and of surgical revision, were lower in the RPN (n = 1434) than the OPN (n = 571) group (2.9% vs. 6.0%, p = 0.0012; 3.8% vs. 11.5%, p < 0.0001; 2.4% vs. 6.7%, p < 0.0001, respectively). In multivariable analyses, RPN was independently associated with fewer early post-operative complications than OPN (overall: odds-ratio [95% confidence interval, CI] = 0.48 [0.35–0.66]; severe: 0.29 [0.16–0.54], p < 0.0001 for both) and shorter hospital stays (34% [30%; 37%], p < 0.0001). RPN was also a significantly associated with a decresedrisk of post-operative acute renal failure, and new-onset chronic kidney disease at 3 and 12 months post-surgery. There were no between-group differences in oncological outcomes. In comparison with OPN, RPN was associated with improved peri- and post-operative morbidity, better functional outcomes, and shorter hospital stays. Our results support the use of RPN, even for large and complex tumours.
Similar content being viewed by others
Introduction
According to the guidelines of the French and European associations of urology, partial nephrectomy (PN) is the standard of care for localised kidney T1a (≤ 4 cm) tumours1,2. When technically possible, PN is also the standard of care in case of imperative surgery (solitary kidney, bilateral disease, and pre-existing renal insufficiency)1, and may be preferred in case of localised T1b and T2 tumours, depending on their complexity1,2. Recent data have shown that PN might also represent a feasible option for large kidney tumours (> 7 cm), with substantial but acceptable morbidity, limited risk of local recurrence, and excellent preservation of renal function3.
The open approach has long been considered the gold standard for PN. Although the laparoscopic route was popularized in the 2000s, technical difficulties (primarily longer arterial clamping times with ischaemia) limited its development4. However, the introduction of robotic assistance bypassed these limitations and led to an increasing proportion of renal cell carcinoma surgery being performed using minimally invasive procedures. In France, Ouzaid et al.5 reported that the annual number of robotic-assisted partial nephrectomy (RPN) procedures continuously increased between 2009 and 2015, whereas the number of laparoscopic partial nephrectomy (LPN) procedures remained stable over this period. Several systematic reviews and meta-analyses have highlighted the benefits of RPN compared to open partial nephrectomy (OPN)6,7,8,9,10,11 and LPN12,13,14. According to Autorino and Porpiglia15, RPN is becoming “the new gold standard for nephron sparing surgery” (NSS). However, the French health care system does not have a specific pricing system for this approach, and therefore does not reimburse the additional costs involved.
Data from the literature are usually based on retrospective series involving single centres and thus few of these data are contemporary and truly representative of French practices. The aim of our study was to use contemporary data, prospectively collected within the French Network for Research on Kidney Cancer UroCCR, to compare short- and mid-term PN outcomes according to the surgical approach. The recent report of the French National Authority for Health (HAS) on robotic-assisted nephrectomy indicated that RPN should be compared to OPN rather than LPN, due to the technical difficulties associated with the LPN approach16. Thus, in this article we report on the comparison between OPN and RPN outcomes.
Methods
Study design and setting
CONTEMPORARI-PN (Comparative analysis of cONtemporary partial nEphrectoMy outcoMes between oPen, laparascOpic and Robotic AppRoaches In France) was a French, retrospective, observational, multicentre, cohort study based on the analysis of prospectively collected data from the UroCCR database (NCT03293563; CNIL DR 2013-206;). Informed consent was obtained from all participants. Collected data included patient and tumour characteristics, as well as surgery-related information. Partial nephrectomy could have been performed through OPN, LPN, or RPN. Thus, two-by-two comparisons were performed using a statistical model integrating these three arms: OPN, LPN, and RPN. However, only the comparisons between RPN and OPN are presented here.
Participants and procedures
All patients iwho underwent PN for kidney cancer and consented to be included in the database between January 01, 2014 and June 30, 2017 within 20 centres belonging to the UroCCR network were included into analyses. The surgical approach was chosen at the surgeon’s discretion. All procedures were performed by experienced surgical teams. RPN was performed using the da Vinci® Surgical System (Intuitive Surgical Sunnyvale, CA, USA).
Outcomes and assessment methods
Primary outcome
The peri-operative morbidity of OPN and RPN was evaluated by measuring the rates of early post-operative surgical complications (overall and severe according to the Clavien-Dindo scale17) and late post-operative complications occurring within 30 days.
Secondary outcomes
The peri-operative morbidity of OPN and RPN was also evaluated by measuring the rates of peri-operative and post-operative transfusion, surgical re-operation, and post-operative death within 30 days.
Oncological outcomes were evaluated by assessing the rates of positive surgical margins, local and contralateral recurrence, metastatic progression, recurrence-free survival, and overall survival.
Functional outcomes were evaluated before surgery and post-operatively on days 1–3 (D1–D3), and at month 3 (M3) and M12 by measuring the following parameters: creatinine, glomerular filtration rate (GFR) calculated according to the modified diet and renal disease (MDRD) formula, new-onset chronic kidney disease (CKD) for patients with pre-operative stage I or II CKD defined by a eGFR < 60 mL/min/1.73 m2, and post-operative acute renal failure rates. We considered an acute renal failure when the eGFR shifted under 60 mL/min/1.73 m2. We also analysed the creatinaemia relative change ((creatinaemia after surgery–creatinaemia before surgery)/creatinaemia before surgery) and GFR relative change ((GFR after surgery–GFR before surgery)/GFR before surgery) that could be more clinically significant than new-onset chronic kidney disease.
Length of hospital stay, and Trifecta achievement according to the Khalifeh criteria18 (defined as negative surgical margins + zero peri-operative complications and a warm ischaemia time ≤ 25 min) were also assessed.
Statistical analyses
Statistical analyses were carried out using SAS software version 9.3 (SAS Institute Inc., NC, USA). Qualitative variables were expressed as numbers and percentages. Quantitative variables were expressed as means and standard deviations. Early and late post-operative surgical complications, qualitative functional outcomes and Trifecta were compared between groups using mixed-effects logistic regression models, with the study centre as a random effect. Local and contralateral recurrence, and metastatic progression were described using the cumulative incidences approach to take into account the competing risk of death occurring before observing these events. Recurrence-free and overall survival were described using the Kaplan–Meier method. Oncological outcomes were compared between groups using stratified (according to study centre) Cox proportional-hazards models. Quantitative functional outcomes and length of hospital stay were compared between groups using mixed linear regression models, with the study centre as a random effect. Model assumptions were systematically verified. Quantitative functional outcomes and length of hospital stay were transformed into natural logarithms to comply with model assumptions. Removal of the random effect (for logistic and linear regression models) and/or use of the Firth’s penalization method (for Cox and logistic models) was proposed when models did not converge. All comparisons were done with and without adjustment for the following prognostic factors: tumour size, imperative NSS indication, age at surgery, American Society of Anesthesiologists (ASA) score, body mass index (BMI) at diagnosis and pre-operative creatininemia for post-operative acute renal failure and new onset CKD only. The RENAL score19 was not included in the model because variations in tumour size had already been taken into account as a prognostic factor. Stratified analyses were performed according to tumour size (≤ 4 cm, [4–7] cm, > 7 cm) and NSS indication. Rates of peri-operative transfusion, surgical re-operation and post-operative deaths within 30 days were compared between groups using the Chi-squared or Fisher exact tests, depending on the event distribution. The type I error rate was set at 5% for all comparisons. No missing data management strategy was used.
Ethics approval and consent to participate
This study was performed in line with the principles of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. In accordance with French law, the processing of personal data was approved by the French data protection agency (Commission Nationale de l'Informatique et des Libertés, CNIL): authorization DR 2013-206 and DR 2014-251. Moreover, the UroCCR project and this particular study (NCT03293563) were IRB-approved (Comité de Protection des Personnes (CPP) Sud-Ouest et Outre mer III, decision DC 2012/108). All patients gave their written consent before inclusion in the UroCCR database, after having received oral and written information about the UroCCR project.
Results
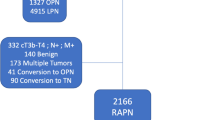
Of the 2097 patients included int the study, who underwent PN for cT1-2N0M0 tumours between January 01, 2014 and June 30, 2017, 1969 (93.9%) underwent either OPN (N = 560) or RPN (N = 1409). Patient and tumour characteristics, as well as surgical outcomes are presented in Table 1.
Peri-operative and post-operative morbidity
Rates of early post-operative complications were lower in patients who underwent RPN than in those that underwent OPN (overall: 17.9% vs. 34.9%; severe: 2.0% vs. 5.5%), whereas no between-group differences were observed for late post-operative complications (4.6% vs. 6.5%). Multivariable analyses showed that RPN was independently associated with a decrease in both overall (odds-ratio [95% confidence interval], OR 95% CI = 0.48 [0.35–0.66], p < 0.0001) and severe (OR 95% CI = 0.29 [0.16–0.54], p < 0.0001) early post-operative complications compared with OPN (Table 2). Stratified analyses did not show any impact of tumour size or NSS indication on this primary outcome (Supplementary Table 1). Rates of peri- and post-operative transfusion, and of re-operation were lower in patients who underwent RPN than in those that underwent OPN (Table 3).
Oncological outcomes
Few patients had positive surgical margins (OPN, N = 29/452, 5.8%; RPN, N = 63/1291, 4.9%), and no significant difference was observed between groups (Table 2). Cumulative incidence curves and Kaplan–Meier curves of oncologic outcomes are shown in Supplementary Fig. 1. Multivariable analyses showed no between-group differences (Table 2).
Functional outcomes
Analyses of functional outcomes are presented in Table 2. Pre-operative/D1-D3 changes in creatininaemia were significantly smaller for the RPN group than for the OPN group. No between-group differences in estimated GFR changes were observed at any time post-surgery. In comparison with OPN, RPN was significantly associated with a lower risk of post-operative acute renal failure, and from new-onset CKD at M3 and M12 post-surgery. Compared with OPN, multivariable analysis revealed a trend towards better fulfilment of Trifecta outcomes with RPN (OR [95% CI] = 0.73 [0.51–1.05], p = 0.0879), and stratified analyses showed that Trifecta outcomes were more likely to be fulfilled with RPN for tumours > 7 cm (Supplementary Table 1).
Finally, RPN was associated with a 34% reduction in the length of hospital stay compared to OPN (Table 2).
Discussion
This analysis of prospectively collected data from almost 2,000 patients who underwent PN over 3.5 years in 20 centres, showed a clear benefit of RPN over OPN in terms of early post-operative complications, peri- and post-operative transfusion rates, re-operation rates, length of hospital stay, pre-operative/D1-D3 creatininaemia changes, post-operative acute renal failure, and new-onset CKD at M3 and M12 post-surgery. No between-group differences were observed for late complication rates, positive surgical margins, and GFR changes. The surgical approach did not have any impact on oncological outcomes.
Our study responds to unmet clinical needs, and addresses the concerns of the HAS surrounding the lack of prospective contemporary studies on RPN16. Indeed, previous prospective studies included few patients and/or did not include patients consecutively, with RPN groups being added a posteriori16. Thus, in such studies, including a previous French study20 in which patients were included over an extensive time period (2006–2014), the observed differences between RPN and OPN groups may not have been uniquely related to the surgery: there may have been differences at several levels of the patient care pathway including anaesthesia, management in the intensive care unit, and other post-operative parameters. Additionally, this previous French study20 included RPN performed by surgeons with various levels of expertise, with most of them still being on the RPN learning curve. This was not the case in our study.
Our contemporary results are in line with those reported by several systematic reviews and/or meta-analyses6,9,10,11,21, except for estimated GFR outcomes, which were reported as better in patients who underwent RPN in two systematic reviews and meta-analyses9,11. Creatininaemia changes, post-operative acute renal failure, and new-onset CKD could not be compared with the literature due to a lack of published data.
Multivariable analyses showed that the benefit of RPN over OPN regarding early post-operative complications (overall or severe), post-operative acute renal failure, and new-onset CKD at M3 and M12 post-surgery was independent of the tumour size, imperative NSS indication, age at surgery, ASA score, and BMI at diagnosis. Interestingly, the superiority of RPN over OPN on Trifecta (which included zero peri-operative complications) was observed for tumours > 7 cm in stratified analyses. RPN therefore had a beneficial impact on these parameters, even for large and complex tumours. The seemingly greater benefit of RPN observed for new-onset CKD at M3 post-surgery for tumours > 7 cm may be related to the higher probability of occurrence of this event in patients with large tumours. The benefits of RPN over OPN for complex tumours have also been highlighted in a systematic review (RENAL score ≥ 7)11 and in a single centre study (RENAL score > 9)22, with reported benefits including reductions in blood loss and length of stay, as well as in intra-operative complications and transfusion rates22, and post-operative complications11,22. In contrast, apart from a shorter hospital stay after RPN versus OPN, Zargar et al. did not identify any between-group differences in their preliminary study focusing on solitary kidney23. To the best of our knowledge, the benefits of RPN for achieving Trifecta for large and complex tumours have not been demonstrated previously.
Several authors concluded their systematic review and meta-analysis on PN by claiming that randomized controlled trials (RCTs) to compare RPN and OPN would be needed to confirm their findings6,9,10,21. However, the implementation of such RCTs is no longer conceivable due to the rapid expansion of RPN, and ethical issues. In France, some centres already only use the robotic approach for PN, convinced of the net benefits of this surgical approach, both for patients and hospitals. Outpatient RPN has even been implemented in Bordeaux for selected patients, supported by a dedicated, nurse-led clinical pathway, and has been shown to provide a high level of patient satisfaction as well as economic optimization of robotic assistance24,25.
Our study had some limitations. Two-by-two comparisons were performed using a statistical model integrating an initial three study arms: OPN, LPN, and RPN. However, the results of the multivariable and stratified analyses remained stable after removal of the LPN arm, enabling us to report only on the clinically relevant comparison between OPN and RPN. The retrospective design of the study might lead to selection biases with more complex tumors and more imperative indications in the OPN arm. Although these differences were tackled with the multivariate analyses, other factors and unmeasured cofounders might affect the results and selection bias remains a concern. The exclusive practice of RPN in some of our study centres may have introduced a bias because no same-centre comparisons of outcomes were possible. However, our study was multicentric and gathered data from 20 centres, all of which were expert centres for both RPN and OPN. Furthermore, the impact of surgeons’ expertise on outcomes also needs to be considered. Although this is a factor that cannot be eliminated, our study, like most previous evaluations of RPN, used data generated by high-volume surgeons with extensive experience. Our findings may not therefore be readily transferable to settings were RPN is conducted by less experienced surgeons. Another question to be addressed is the comparative cost-effectiveness of the two surgical approaches. Our findings demonstrated that patients who underwent RPN had shorter hospital stays, fewer complications and re-operations than those who underwent OPN. Other previously reported advantages of minimally invasive PN over OPN that may also have some impact on costs include lower rates of peri-operative opioid use and fewer days of workplace absenteeism26. These advantages could balance out the cost of robotic assistance. In their meta-analysis, Wu et al.6 found that the overall cost of RPN was not significantly higher than that of OPN, and Bernhard et al.25 recently reported that implementing RPN along with enhanced recovery after surgery and day-case nurse-led protocols may facilitate the economic sustainability of robotic assistance for hospitals where the extra cost is not covered by the healthcare system.
In conclusion, RPN was associated with improved peri- and post-operative morbidity, shorter hospital stays, better functional outcomes for some parameters, and similar oncological outcomes in comparison with OPN in our multicentre contemporary study. Our results support the use of RPN, even for large and complex tumours.
Data availability
Data are available from the corresponding author upon request.
References
Bensalah, K. et al. French ccAFU guidelines—update 2020–2022: Management of kidney cancer. Prog. Urol. 30(12s), S2-s51. https://doi.org/10.1016/s1166-7087(20)30749-1 (2020).
Ljungberg, B. et al. European association of urology guidelines on renal cell carcinoma: The 2019 update. Eur. Urol. 75(5), 799–810. https://doi.org/10.1016/j.eururo.2019.02.011 (2019).
Rouffilange, J. et al. Partial nephrectomy for renal masses > 7 cm: Morbidity, oncological and functional outcomes (UroCCR-7 study). Prog. Urol. 28(12), 588–595. https://doi.org/10.1016/j.purol.2018.06.007 (2018).
Bensalah, K. et al. French ccAFU guidelines—update 2018–2020: Management of kidney cancer. Prog. Urol. 28(Suppl 1), R5-r33. https://doi.org/10.1016/j.purol.2019.01.004 (2018).
Ouzaid, I. et al. Trends in the practice of renal surgery for cancer in France after the introduction of robotic-assisted surgery: Data from the National Health Care System Registry. J. Robot. Surg. 14(5), 799–801. https://doi.org/10.1007/s11701-020-01076-5 (2020).
Wu, Z. et al. Robotic versus open partial nephrectomy: A systematic review and meta-analysis. PLoS ONE 9(4), e94878. https://doi.org/10.1371/journal.pone.0094878 (2014).
Poinas, G., Long, J. A., Rébillard, X. & Descotes, J. L. Place of partial nephrectomy assisted by robot: Review of the literature at the time of a request for a specific nomenclature. Prog. Urol. 28(16), 890–899. https://doi.org/10.1016/j.purol.2018.08.012 (2018).
Grivas, N. et al. Robot-assisted versus open partial nephrectomy: Comparison of outcomes. A systematic review. Minerva Urol. Nefrol. 71(2), 113–120. https://doi.org/10.23736/s0393-2249.19.03391-5 (2019).
Tsai, S. H. et al. Open versus robotic partial nephrectomy: Systematic review and meta-analysis of contemporary studies. Int. J. Med. Robot. 15(1), e1963. https://doi.org/10.1002/rcs.1963 (2019).
Xia, L., Wang, X., Xu, T. & Guzzo, T. J. Systematic review and meta-analysis of comparative studies reporting perioperative outcomes of robot-assisted partial nephrectomy versus open partial nephrectomy. J. Endourol. 31(9), 893–909. https://doi.org/10.1089/end.2016.0351 (2017).
Cacciamani, G. E. et al. Impact of surgical factors on robotic partial nephrectomy outcomes: Comprehensive systematic review and meta-analysis. J. Urol. 200(2), 258–274. https://doi.org/10.1016/j.juro.2017.12.086 (2018).
Zhang, X. et al. Comparison of peri-operative outcomes of robot-assisted vs laparoscopic partial nephrectomy: A meta-analysis. BJU Int. 112(8), 1133–1142. https://doi.org/10.1111/bju.12255 (2013).
Choi, J. E., You, J. H., Kim, D. K., Rha, K. H. & Lee, S. H. Comparison of perioperative outcomes between robotic and laparoscopic partial nephrectomy: A systematic review and meta-analysis. Eur. Urol. 67(5), 891–901. https://doi.org/10.1016/j.eururo.2014.12.028 (2015).
Leow, J. J., Heah, N. H., Chang, S. L., Chong, Y. L. & Png, K. S. Outcomes of robotic versus laparoscopic partial nephrectomy: An updated meta-analysis of 4919 patients. J. Urol. 196(5), 1371–1377. https://doi.org/10.1016/j.juro.2016.06.011 (2016).
Autorino, R. & Porpiglia, F. Robotic-assisted partial nephrectomy: A new era in nephron sparing surgery. World J. Urol. 38(5), 1085–1086. https://doi.org/10.1007/s00345-020-03164-5 (2020).
HAS. Évaluation de la néphrectomie totale ou partielle assistée par robot.2019. Available from: https://www.has-sante.fr/jcms/p_3103989/fr/evaluation-de-la-nephrectomie-totale-ou-partielle-assistee-par-robot.
Dindo, D., Demartines, N. & Clavien, P. A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 240(2), 205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae (2004).
Khalifeh, A. et al. Comparative outcomes and assessment of trifecta in 500 robotic and laparoscopic partial nephrectomy cases: A single surgeon experience. J. Urol. 189, 1236–1242. https://doi.org/10.1016/j.juro.2012.10.021 (2013).
Kutikov, A. & Uzzo, R. G. The R.E.N.A.L. Nephrometry score: A comprehensive standardized system for quantitating renal tumor size, location and depth. J. Urol. 182(3), 844–53. https://doi.org/10.1016/j.juro.2009.05.035 (2009).
Peyronnet, B. et al. Comparison of 1800 robotic and open partial nephrectomies for renal tumors. Ann. Surg. Oncol. 23(13), 4277–4283. https://doi.org/10.1245/s10434-016-5411-0 (2016).
Shen, Z. et al. The comparison of perioperative outcomes of robot-assisted and open partial nephrectomy: A systematic review and meta-analysis. World J. Surg. Oncol. 14(1), 220. https://doi.org/10.1186/s12957-016-0971-9 (2016).
Garisto, J. et al. Robotic versus open partial nephrectomy for highly complex renal masses: Comparison of perioperative, functional, and oncological outcomes. Urol. Oncol. 36(10), 471.e1-471.e9. https://doi.org/10.1016/j.urolonc.2018.06.012 (2018).
Zargar, H. et al. Comparison of perioperative outcomes of robot-assisted partial nephrectomy and open partial nephrectomy in patients with a solitary kidney. J. Endourol. 28(10), 1224–1230. https://doi.org/10.1089/end.2014.0297 (2014).
Bernhard, J. C. et al. Day-case robotic-assisted partial nephrectomy: Feasibility and preliminary results of a prospective evaluation (UroCCR-25 AMBU-REIN study). World J. Urol. https://doi.org/10.1007/s00345-020-03283-z (2020).
Bernhard, J. C. et al. Nurse-led coordinated surgical care pathways for cost optimization of robotic-assisted partial nephrectomy: Medico-economic analysis of the UroCCR-25 AMBU-REIN study. World J. Urol. https://doi.org/10.1007/s00345-022-04066-4 (2022) (Epub ahead of print. PMID: 35727334).
Krimphove, M. J. et al. Recovery from minimally invasive vs. open surgery in kidney cancer patients: Opioid use and workplace absenteeism. Investig. Clin. Urol. https://doi.org/10.4111/icu.20200194 (2020).
Acknowledgements
We would like to acknowledge Laurence Rous, PhD, Emma Pilling, PhD, and Marielle Romet, PhD (Synergy Pharm/Santé Active Edition) for providing medical writing and English editing assistance.
Funding
Sponsorship of this study was provided by Intuitive Surgical.
Author information
Authors and Affiliations
Consortia
Contributions
J.C.B.; data collection: A.I., K.B., J.B.B., P.P., M.R., H.L., F.X.N., F.H., F.B., F.A., C.L., H.B., J.A.L., R.T., T.C., E.X., T.W., C.M., G.M., R.B., P.B., and J.C.B.; data analysis: A.I., J.A., A.B., and J.C.B.; manuscript editing: A.I., C.M., J.A., A.B., and J.C.B.
Corresponding author
Ethics declarations
Competing interests
Dr. Ingels, Prof. Bensalah, Prof. Paparel, Prof. Rouprêt, Prof. Bruyère and Prof. Bernhard declare to be proctors and/or speakers for Intuitive Surgical. The other authors have nothing to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ingels, A., Bensalah, K., Beauval, J.B. et al. Comparison of open and robotic-assisted partial nephrectomy approaches using multicentric data (UroCCR-47 study). Sci Rep 12, 18981 (2022). https://doi.org/10.1038/s41598-022-22912-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22912-8
This article is cited by
-
A prototype variable corresponding to the proportion of ischemia for the comparison between robotic and open partial nephrectomy: a meta-analysis accompanied by sensitivity analysis
Beni-Suef University Journal of Basic and Applied Sciences (2023)
-
Comparison of peri- and intraoperative outcomes of open vs robotic-assisted partial nephrectomy for renal cell carcinoma: a propensity-matched analysis
World Journal of Surgical Oncology (2023)
-
Assessing the safety of minimally invasive partial nephrectomy in octogenarians
Journal of Robotic Surgery (2023)
-
Late complications and 5 years outcomes of robotic partial nephrectomy in France: prospective assessment in the French Kidney Cancer Research Network (UroCCR 10)
World Journal of Urology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.