Abstract
Despite the availability of efficacious direct-acting antiviral (DAA) therapy, the number of people infected with hepatitis C virus (HCV) continues to rise, and HCV remains a leading cause of liver-related morbidity, liver transplantation, and mortality. We developed and validated machine learning (ML) algorithms to predict DAA treatment failure. Using the HCV-TARGET registry of adults who initiated all-oral DAA treatment, we developed elastic net (EN), random forest (RF), gradient boosting machine (GBM), and feedforward neural network (FNN) ML algorithms. Model performances were compared with multivariable logistic regression (MLR) by assessing C statistics and other prediction evaluation metrics. Among 6525 HCV-infected adults, 308 patients (4.7%) experienced DAA treatment failure. ML models performed similarly in predicting DAA treatment failure (C statistic [95% CI]: EN, 0.74 [0.69–0.79]; RF, 0.74 [0.69–0.80]; GBM, 0.72 [0.67–0.78]; FNN, 0.75 [0.70–0.80]), and all 4 outperformed MLR (C statistic [95% CI]: 0.51 [0.46–0.57]), and EN used the fewest predictors (n = 27). With Youden index, the EN had 58.4% sensitivity and 77.8% specificity, and nine patients were needed to evaluate to identify 1 DAA treatment failure. Over 60% treatment failure were classified in top three risk decile subgroups. EN-identified predictors included male sex, treatment < 8 weeks, treatment discontinuation due to adverse events, albumin level < 3.5 g/dL, total bilirubin level > 1.2 g/dL, advanced liver disease, and use of tobacco, alcohol, or vitamins. Addressing modifiable factors of DAA treatment failure may reduce the burden of retreatment. Machine learning algorithms have the potential to inform public health policies regarding curative treatment of HCV.
Similar content being viewed by others
Introduction
Hepatitis C virus (HCV) is the most common chronic bloodborne infection in the U.S. and a leading cause of liver-related morbidity, liver transplantation, and mortality1,2,3,4. The number of deaths resulting from HCV has exceeded the total number of deaths due to 60 other infectious diseases combined, including HIV, pneumococcal disease, and tuberculosis, and the rate of HCV infection continues to increase1,5. In 2014, HCV treatment greatly improved with the approval of direct-acting antiviral (DAA) therapy, with therapeutic efficacy of 95% or higher6, yet new cases of this preventable disease are still increasing7,8,9,10,11,12. With less than a decade remaining to reach the goal set by the World Health Organization to eliminate viral hepatitis by reducing new hepatitis infections by 90% and to reduce death due to hepatitis infections by 65% by 203013, HCV remains one of the top causes of chronic liver disease worldwide14.
The rate of treatment failures, though small in percentage (< 5%), remains large in number considering that the magnitude of patients with HCV means that a substantial number of first DAA therapy interventions will fail and that more patients will need to be treated in the near future15,16,17. To understand more about patients who are at high risk of treatment failure, a recent study by members of our team used machine learning to identify pretreatment risk factors to help clinicians identify factors that may be modifiable before initiation of DAA treatment18. That study found that an algorithm using a gradient boosting machine (GBM) performed effectively for DAA treatment risk prediction with 41 pretreatment predictors; the top 10 GBM-identified predictors included albumin, liver enzyme, and total bilirubin levels, sex, HCV viral load, sodium level, presence of hepatocellular carcinoma, platelet level and tobacco use18.
However, despite the best performance by the GBM algorithm among the four machine learning algorithms assessed in that study, the C statistic was suboptimal (0.69), suggesting that there may be important predictors not included in the model. We hypothesized here that predictors present during treatment, such as the duration of treatment, adherence to the prescribe medication treatment, and adverse events experienced, may better explain treatment failure when combined with patient characteristics present prior to treatment. Therefore, we developed and validated additional machine learning algorithms to predict DAA treatment failure, this time using predictors both before and during treatment. An overarching goal of the present study was to provide clinicians with a reasonable list of risk factors that may be amendable to modification prior to or during treatment of HCV to reduce the rate of DAA treatment failure.
Methods
Study design and participants
The data for this cohort study were obtained from HCV-TARGET (Hepatitis C Therapeutic Registry and Research Network), a longitudinal, prospective, observational cohort study of the real-world administration of DAA therapy19. The use by HCV-TARGET of a standardized and centralized method to abstract data from medical records combined with a detailed data monitoring system ensures both the quality and integrity of the database. Patients included in the present study were 18 years of age or older, initiated an all-oral DAA HCV treatment regimen between February 2014 and 2018, had virologic outcome data available as of June 2019, and provided written informed consent to participate in HCV-TARGET. The DAA regimens used with or without ribavirin included ledipasvir/sofosbuvir; sofosbuvir plus daclatasvir; ombitasvir/paritaprevir/ritonavir plus dasabuvir; elbasvir/grazoprevir; sofosbuvir/velpatasvir; sofosbuvir/velpatasvir/voxilaprevir; and glecaprevir/pibrentasvir. Patients who completed the assigned HCV treatment or who discontinued treatment early owing to efficacy concerns or adverse effects and who had virologic outcome data available were assigned to the per-protocol population. This report complies with the Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD) guideline (Supplementary Table 1)20. This study was approved by the institutional review board of the University of Florida, Gainesville.
Primary outcome
Sustained virologic response (SVR) was the primary efficacy end point and was defined as plasma HCV RNA levels undetectable or below quantitation 12 or more weeks after completing DAA treatment.
Predictor candidates
Given the results in prior studies21,22,23 as well as previous work by members of our team18, we assessed 359 variables as candidate predictors. The candidates included sociodemographic and clinical characteristics, DAA treatment regimen and duration, and laboratory test results consisting of 242 predictors before therapy initiation and 117 predictors 4 weeks after initiation (Supplementary Table 2).
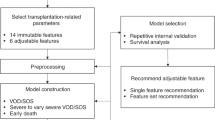
Approaches to machine learning and evaluation of prediction model performance
A full description of the machine learning approach used in the present study was previously described18. In brief, our analyses generated risk prediction scores for DAA treatment failure per individual and then used these risk prediction scores to group individuals into subgroups comprising similar DAA treatment failure risks. Two-thirds of patients were randomly assigned to a training sample for development of a prediction algorithm, which was then validated with the remaining one-third of patients. The prediction results of four commonly used machine learning approaches shown to have the best prediction results, elastic net (EN), random forest (RF), GBM, and feedforward neural network (FNN)24,25, were compared with a multivariable logistic regression algorithm previously generated from HCV-TARGET data, which included as predictors male sex, albumin level, platelet count, total bilirubin level, history of previous treatment, proton pump inhibitor [PPI] use, and HCV genotype subtype26. The Methods in the Supplement describe the details for each of the machine learning approaches used. We assessed the discrimination performance ability of the various models by comparing the DAA treatment failure rates of patients who had been predicted to be high risk of DAA treatment failure vs. the patients who had been predicted to be at low risk. Using the DeLong test, the C statistics (0.7–0.8 considered good; > 0.8, very good) and precision-recall curves for the various models were compared using the validation sample27. Eight metrics of evaluation were also assessed: sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio, negative likelihood ratio, number needed to evaluate (NNE) to identify 1 DAA treatment failure, and estimated positive alert rate. For the EN final model, we report beta coefficients and odds ratios. Because EN regularization does not provide an estimate of precision, 95% CIs are not given herein.
Supplementary Table 3 gives the prediction metrics at numerous sensitivity and specificity levels, including the arbitrary selection of 90% sensitivity as an anchor and the use of the Youden index to obtained a threshold with balanced sensitivity and specificity28. To enable a more granular examination of patients at highest risk of DAA treatment failure, the validation sample was split into subgroups using the decile of the predicted risk score from the training algorithm. The highest decile was further split into three strata: the top first percentile, the second through fifth percentile, and the sixth through tenth percentile. Calibration plots were used to compare the agreement between the observed and predicted risk of DAA treatment failure for each risk subgroup. For potential clinical use, we report the top 25 most important prediction factors. For comparison of the training and validation samples, patient characteristics were analyzed using 2-tailed t tests for continuous variables and chi-square tests for categorical variables. All analyses were performed using SAS, version 9.4 (SAS Institute Inc, Cary, North Carolina) and Python, version 3.6 (Python Software Foundation, Delaware).
Results
Patient characteristics
In total, 6525 patients (4894 in the training sample and 1631 in the validation sample) were included in this study. The sociodemographic (e.g. mean [SD] age, 57 [11] years; 60% male; 23% Black race and ethnicity; and 66% White race and ethnicity) and clinical characteristics (e.g. 36% with cirrhosis) of the training and validation groups were similar (Table 1). Approximately 50% of participants had HCV genotype subtype 1a, 15% had a viral load of at least 6 million IU/mL, 14% had a history of hepatic decompensation, and 8% had undergone a prior liver transplantation. Overall, 65% were treatment naïve and the three most commonly used DAA treatment regimens for the remaining patients were ledipasvir/sofosbuvir (39%), followed by sofosbuvir/velpatasvir (11%), and then glecaprevir/pibrentasvir (9%). At baseline, approximately 28% of patients reported PPI use, 35% reported vitamin use, 60% reported tobacco product use; and 29% reported alcohol use. Overall, 6217 patients (95.3%) achieved an SVR; however, 308 patients (4.7%) experienced DAA treatment failure.
Prediction performance
The ability to predict DAA treatment failure was similar across the four machine learning models, which all performed better than the previously developed multivariable logistic regression model: EN (C statistic = 0.74, 95% CI = 0.69–0.79), FNN (C statistic = 0.75, 95% CI = 0.70–0.80), RF (C statistic = 0.74, 95% CI = 0.69–0.80), GBM (C statistic = 0.72, 95% CI = 0.67–0.78), and multivariable logistic regression (C statistic = 0.51, 95% CI = 0.46–0.57) (Fig. 1A). Of the four machine learning models, the EN required the fewest predictors (EN = 27 vs. GBM = 47, FNN = 359 and RF = 268), and the GBM had slightly better precision-recall performance (Fig. 1B) as assessed by the area under the receiving operating characteristic curves. Supplementary Table 3 presents the prediction performance measures by sensitivity and specificity levels (90–100%). With performance measures balanced for sensitivity and specificity (using the Youden index), the EN approach had 58.4% sensitivity, 77.8% specificity, 11.5% PPV, 97.4% NPV, 9 needed to identify 1 DAA treatment failure, and 24 positive alerts per 100 patients. After setting the sensitivity to 90% to attempt to identify 90% of the observed DAA treatment failure, the EN had 44.3% specificity, 7.4% PPV, 98.9% NPV, 14 needed to identify 1 DAA treatment failure, and 57 positive alerts per 100 patients (Fig. 1C,D; Supplementary Table 3).
Prediction performance of 4 machine learning models vs. a multivariable logistic regression model. FNN feedforward neural network, EN elastic net, GBM gradient boosting machine, MLR multivariable logistic regression, RF random forest, ROC receiver operating characteristic. Data were derived using the validation sample, which comprised 1631 patients: 1554 with direct-acting antiviral treatment success, and 77 with treatment failure. (A), Results include C statistics and 95% CIs. (B), precision is equivalent to the positive predictive value, and recall to sensitivity). Models with curves closer to the upper right corner or above another curve have improved performance. (C), Number needed to evaluate by different cutoff points for sensitivity. (D), Alerts per 100 patients by various sensitivity cutoff points.
Risk stratification by decile risk subgroup
The observed (actual) DAA treatment failure rates for patients by each decile subgroup using the EN model are shown in Fig. 2. The high-risk subgroup (with risk scores in the top decile; 155 patients [9.5%] in the validation sample) had a PPV of 14.8% and needed 7 to identify 1 treatment failure. Of 77 patients with DAA treatment failure, 47 (61%) were assigned to 1 of the top 3 subgroups (decile 1 = 30%, decile 2 = 15.6%, and decile 3 = 15.6%), that is, 7–22 per 100 patients. The DAA treatment failure rate in the first decile subgroup was at least 20-fold as high as that in the lower-risk groups (e.g. first percentile = 22.7% vs. tenth decile = 1.1%). Minimal rates of DAA treatment failure were found in the fourth through tenth decile subgroups (0.5–5 per 100 patients). The top 25 key predictors as identified by the EN model are shown in Fig. 3. Those predictors included male sex, DAA treatment duration < 8 weeks, treatment discontinuation due to adverse events, advanced liver disease (i.e. cirrhosis and hepatocellular carcinoma), albumin level < 3.5 g/dL, total bilirubin level > 1.2 g/dL, alcohol or tobacco use, pain, hyperlipidemia, and use of immunosuppressants, PPI, or vitamins.
Elastic net model identification of 25 key prediction factors associated with direct-acting antiviral treatment failurea. DCC decompensated cirrhosis, HCC hepatocellular carcinoma, LDV/SOF ledipasvir/sofosbuvir, PPI proton pump inhibitor. aPredictors are ordered by factor importance based on odds ratios. Elastic net regularization does not provide an estimate of precision; therefore, 95% CIs are not given.
Discussion
In this cohort study, we used HCV-TARGET registry data to develop and evaluate four machine learning models to predict DAA treatment failure among patients treated for HCV. All four models showed good discrimination performance, outperforming models developed and assessed in a previous study by members of our group18 (C statistics 0.72–0.75 vs. 0.64–0.69) and substantially outperforming the multivariable logistic regression model result (C statistic, 0.51)29. As expected, the PPV was low given the low incidence of DAA treatment failure. However, the EN algorithm effectively subdivided the sample into different risk groups based on predicted risk scores, with 60% of the individuals with DAA treatment failure placed in the top three decile risk subgroups. The EN model was also the preferred and most parsimonious algorithm because it required only 25 predictors (vs. 359 predictors for FNN), reducing computational time. Identifying these risk subgroups as well as risk factors may inform treatment strategies for patients with HCV.
In the previous machine learning study by members of our group using the same dataset as in the present study (HCV-TARGET), only predictor candidates of DAA treatment failure before DAA treatment were assessed. That study found that the factors most strongly associated with treatment failure were albumin, bilirubin and liver enzyme (aspartate aminotransferase, alkaline phosphatase) levels, male sex, HCV RNA level, and the presence of advanced liver disease18. In the present study, we assessed the same pretreatment factors but also included factors associated with HCV treatment. Although low albumin levels, high bilirubin levels, male sex, and presence of advanced liver disease remained significant as predictors of DAA treatment failure, the other two factors (e.g. liver enzymes, HCV RNA level) previously found to be significant predictors did not. The most significant prediction factors in the present study were male sex, treatment duration < 8 weeks, or treatment discontinuation due to adverse effects, suggesting that treatment continuation is a key factor for achieving SVR. Although we do not know why patients discontinued early, further analysis indicated that 44% of patients had treatment durations of < 8 weeks and discontinued treatment due to adverse effects (data not shown). Of those, 38% had ribavirin, which is known to be associated with anemia, nausea, pulmonary, and dermatologic adverse conditions30.
The use of machine learning statistical approaches enabled us to confirm the results of prior studies that found similar baseline predictors of treatment failure, including factors associated with advanced liver disease or with treatment for advanced liver disease (e.g. use of immunosuppressants, diuretics, pain medication, or bile and liver therapies), PPI use, albumin level < 3.5 g/dL, total bilirubin level > 1.2 g/dL, and male sex, and predictors associated with treatment discontinuation21,22. We also suggest that given the significant interaction with PPIs resulting in a reduction in SVR, clinicians should address how best to control patient symptoms during DAA treatment18,26. In contrast to the results of these studies, we did not find a significant association of HCV genotype (e.g. genotype 3 or 1a) with increased risk of DAA treatment failure. The lack of this association may be due to the more common use now of pangenotypic DAA regimens for treating HCV.
Among the top ten predictors of DAA treatment failure, we identified several potentially modifiable risk factors, including tobacco, alcohol, and vitamin use. Several studies using National Health and Nutrition Examination Survey data have reported that individuals with HCV are nearly 3 times as likely to smoke tobacco (62% vs. 23%) and 3 times as likely to consume an average of more than 1 drink per day (36% vs. 14%) than individuals without HCV31,32. More than half of patients with HCV included in the present study smoked cigarettes, and 30% reported alcohol use at baseline, which is well representative of patients with HCV in the U.S. Another study found that 32% of patients with HCV treatment reported alcohol use and that unhealthy alcohol users (adjusted odds ratio, 0.75) among veterans with HCV were less likely to achieve SVR than those who were abstinent or reported low-level alcohol use33. Although the present study results suggested that the vast majority of patients with HCV were cured in the era of available DAA therapy, tobacco and alcohol use may be associated with decreased SVR rate or may serve as markers for patients at risk of treatment failure. It is also important to recognize that continued alcohol and tobacco use even after SVR may put patients at risk for progression of liver disease31,33.
The use of vitamins as a factor associated with DAA treatment failure has not been previously reported, but several studies have demonstrated that deficiency in vitamin A or vitamin D is a risk factor for fibrosis and for interferon/ribavirin treatment failure among patients with HCV infection34,35,36. We postulate that it may not be the use of vitamins themselves that is associated with DAA treatment failure, but that their use may be a proxy measure for the presence of a vitamin deficiency or malnutrition. A recent meta-analysis reported that low vitamin levels are common among patients with HCV infection and are associated with advanced liver fibrosis37,38. In the present study, we also found that patients with vitamin use were more likely to be older (59.7 vs. 56.4 years) and have advanced liver diseases (e.g. cirrhosis 39.5% vs. 34.0%; hepatocellular carcinoma 8.7% vs. 4.3%) [data not shown]. Nonetheless, further research is needed to validate our findings and to determine why multivitamin use may be adversely associated with or interact with DAAs.
Together, the findings of the present study have important implications for clinicians. First, in the high-risk group with many known risk factors, more than 95% of the group achieved SVR, suggesting that despite these risk factors, DAA treatment should be prescribed when indicated. Second, pretreatment risk factors, such as indictors of liver function, while important should not be used as discriminators when making decisions regarding whether to prescribe treatment. Rather, clinicians should continuously encourage treatment adherence and offer alternative ways to address modifiable risk factors (e.g. smoking cessation).
This study has several limitations. First, we did not include data on baseline resistance-associated substitutions (RASs) in NS3 or NS5A proteins. Although RASs have been associated with treatment failure, their contribution appears to be minimal and routine baseline RAS testing is not recommended39,40. Second, although we did not use an external validation data set, the present study expanding on the recent study by members of our group18 found that the factors associated with SVR failure remained similar to those of the previous study. In addition, we used data from the HCV-TARGET registry, one of the largest databases for patients with HCV infection prescribed DAAs in the U.S. Nevertheless, our results should be validated with other data sets. Third, machine learning requires extensive amounts of data and may incur high computational costs. However, by selecting the most parsimonious model (the EN model with 25 predictors), we reduced computational costs while maintaining high prediction validity and accuracy. Fourth, it is important that our results not be interpreted as causal inference between individual predictors and treatment failure but as associations.
In conclusion, the present study demonstrated that machine learning approaches provide a simple algorithm for identifying factors predictive of DAA treatment failure. Given that the number of HCV infection cases is increasing and that the number of patients with the infection still requiring treatment is high, addressing modifiable factors of DAA treatment failure (tobacco, alcohol, vitamin and PPI use) may reduce the burden of retreatment. Machine learning algorithms have the potential to inform public health policies regarding curative treatment of HCV.
Data availability
The data that support the findings of this study are available from HCV-TARGET research consortium, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors (Joy Peter; joy.peter@medicine.ufl.edu) upon reasonable request and with permission of HACV-TARGET research consortium.
Abbreviations
- DAA:
-
Direct-acting antiviral
- EN:
-
Elastic net
- HCV:
-
Hepatitis C virus
- NNE:
-
Number needed to evaluate
- PPI:
-
Proton pump inhibitor
- SVR:
-
Sustained virologic response
References
Centers for Disease Control and Prevnetion (CDC). Hepatitis C kills more Americans than any other infectious disease. Available at: http://www.cdc.gov/media/releases/2016/p0504-hepc-mortality.html. Accessed 10 June 2022.
Ditah, I. et al. The changing epidemiology of hepatitis C virus infection in the United States: National Health and Nutrition Examination Survey 2001 through 2010. J. Hepatol. 60(4), 691–698 (2014).
Denniston, M. M. et al. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann. Intern. Med. 160(5), 293–300 (2014).
Morgan, R. L. et al. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: A meta-analysis of observational studies. Ann. Intern. Med. 158(5 Pt 1), 329–337 (2013).
Ly, K. N. et al. The increasing burden of mortality from viral hepatitis in the United States between 1999 and 2007. Ann. Intern. Med. 156(4), 271–278 (2012).
Falade-Nwulia, O. et al. Oral direct-acting agent therapy for hepatitis C virus infection: A systematic review. Ann. Intern. Med. 166(9), 637–648 (2017).
Ryerson, A. B., Schillie, S., Barker, L. K., Kupronis, B. A. & Wester, C. Vital signs: Newly reported acute and chronic hepatitis C cases—United States, 2009–2018. MMWR Morb. Mortal. Wkly. Rep. 69(14), 399–404 (2020).
Schillie, S., Wester, C., Osborne, M., Wesolowski, L. & Ryerson, A. B. CDC recommendations for hepatitis C screening among adults—United States, 2020. MMWR Recomm. Rep. 69(2), 1–17 (2020).
Smith, B. D. et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945–1965. MMWR Recomm. Rep. 61(RR-4), 1–32 (2012).
Centers for Disease Control and Prevnetion (CDC). Viral Hepatitis Surveillance Report. Available at: https://www.cdc.gov/hepatitis/statistics/2019surveillance/pdfs/2019HepSurveillanceRpt.pdf. Accessed 10 June 2022. (2019).
Ko, J. Y., Haight, S. C., Schillie, S. F., Bohm, M. K. & Dietz, P. M. National trends in hepatitis C infection by opioid use disorder status among pregnant women at delivery hospitalization—United States, 2000–2015. MMWR Morb. Mortal. Wkly. Rep. 68(39), 833–838 (2019).
Liang, T. J. & Ward, J. W. Hepatitis C in injection-drug users—A hidden danger of the opioid epidemic. N. Engl. J. Med. 378(13), 1169–1171 (2018).
World Health Organization (WHO). Hepatitis C. Available at: http://www.who.int/mediacentre/factsheets/fs164/en/. Accessed 10 June 2022.
Paik, J. M., Golabi, P., Younossi, Y., Mishra, A. & Younossi, Z. M. Changes in the global burden of chronic liver diseases from 2012 to 2017: The growing impact of NAFLD. Hepatology 72(5), 1605–1616 (2020).
Centers for Disease Control and Prevnetion (CDC). New estimates reveal declines in hepatitis C treatment in the U.S. between 2015 and 2020. Available at: https://www.cdc.gov/nchhstp/newsroom/2021/2014-2020-hepatitis-c-treatment-estimates.html. Accessed 10 June 2022.
Holmes, J. A., Rutledge, S. M. & Chung, R. T. Direct-acting antiviral treatment for hepatitis C. Lancet 393(10179), 1392–1394 (2019).
Harrington, P. R. et al. Impact of hepatitis C virus polymorphisms on direct-acting antiviral treatment efficacy: Regulatory analyses and perspectives. Hepatology 67(6), 2430–2448 (2018).
Park, H. et al. Machine learning algorithms for predicting direct-acting antiviral treatment failure in chronic hepatitis C: An HCV-TARGET analysis. Hepatology https://doi.org/10.1002/hep.32347 (2022).
Mishra, P. et al. Public-private partnership: Targeting real-world data for hepatitis C direct-acting antivirals. Gastroenterology 153(3), 626–631 (2017).
Bossuyt, P. M. et al. STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. Radiology 277(3), 826–832 (2015).
Benitez-Gutierrez, L. et al. Prevention and management of treatment failure to new oral hepatitis C drugs. Expert Opin. Pharmacother. 17(9), 1215–1223 (2016).
Kondili, L. A. et al. Incidence of DAA failure and the clinical impact of retreatment in real-life patients treated in the advanced stage of liver disease: Interim evaluations from the PITER network. PLoS ONE 12(10), e0185728 (2017).
Su, F., Beste, L. A., Green, P. K., Berry, K. & Ioannou, G. N. Direct-acting antivirals are effective for chronic hepatitis C treatment in elderly patients: A real-world study of 17 487 patients. Eur. J. Gastroenterol. Hepatol. 29(6), 686–693 (2017).
Hastie T. T.R., Friedman J. The Elements of statistical learning: data mining, inference and prediction. New York, NY (2008).
Chu, A. et al. A decision support system to facilitate management of patients with acute gastrointestinal bleeding. Artif. Intell. Med. 42(3), 247–259 (2008).
Terrault, N. A. et al. Effectiveness of ledipasvir-sofosbuvir combination in patients with hepatitis C virus infection and factors associated with sustained virologic response. Gastroenterology 151(6), 1131–1134 (2016).
DeLong, E. R., DeLong, D. M. & Clarke-Pearson, D. L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 44(3), 837–845 (1988).
Fluss, R., Faraggi, D. & Reiser, B. Estimation of the Youden Index and its associated cutoff point. Biom. J. 47(4), 458–472 (2005).
Park, H.L.-C.W. et al. Machine learning algorithms for predicting direct-acting antiviral treatment failure in chronic hepatitis C: An HCV-TARGET analysis. Hepatology https://doi.org/10.1002/hep.32347 (2022).
Sung, H., Chang, M. & Saab, S. Management of hepatitis C antiviral therapy adverse effects. Curr. Hepat. Rep. 10(1), 33–40 (2011).
Kim, R. S. et al. Cigarette smoking in persons living with hepatitis C: The National Health and Nutrition Examination Survey (NHANES), 1999–2014. Am. J. Med. 131(6), 669–675 (2018).
Armstrong, G. L. et al. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann. Intern. Med. 144(10), 705–714 (2006).
Tsui, J. I. et al. Alcohol use and hepatitis C virus treatment outcomes among patients receiving direct antiviral agents. Drug Alcohol Depend. 169, 101–109 (2016).
Gutierrez, J. A., Parikh, N. & Branch, A. D. Classical and emerging roles of vitamin D in hepatitis C virus infection. Semin. Liver Dis. 31(4), 387–398 (2011).
Bitetto, D. et al. Vitamin A deficiency is associated with hepatitis C virus chronic infection and with unresponsiveness to interferon-based antiviral therapy. Hepatology 57(3), 925–933 (2013).
Jin, C. N., Chen, J. D. & Sheng, J. F. Vitamin D deficiency in hepatitis C virus infection: What is old? What is new?. Eur. J. Gastroenterol. Hepatol. 30(7), 741–746 (2018).
Gayam, V. et al. Association between vitamin D levels and treatment response to direct-acting antivirals in chronic hepatitis C: A real-world study. Gastroenterol. Res. 11(4), 309–316 (2018).
Dadabhai, A. S., Saberi, B., Lobner, K., Shinohara, R. T. & Mullin, G. E. Influence of vitamin D on liver fibrosis in chronic hepatitis C: A systematic review and meta-analysis of the pooled clinical trials data. World J. Hepatol. 9(5), 278–287 (2017).
Sarrazin, C. et al. Prevalence of resistance-associated substitutions in HCV NS5A, NS5B, or NS3 and outcomes of treatment with ledipasvir and sofosbuvir. Gastroenterology 151(3), 501–12 e1 (2016).
Lok, A. S. et al. Efficacy of glecaprevir and pibrentasvir in patients with genotype 1 hepatitis C virus infection with treatment failure after NS5A inhibitor plus sofosbuvir therapy. Gastroenterology 157(6), 1506–17 e1 (2019).
Funding
Research reported in this publication was supported by a University of Florida Informatics Institute and Clinical and Translational Science Institute (CTSI) pilot grant and the National Institute on Drug Abuse of the National Institutes of Health under award number K01DA045618 (to HP). MSS is supported in part by the National Institutes of Health Midcareer Investigator Award K24DA034621.
Author information
Authors and Affiliations
Contributions
All authors conceptualized and designed the study. H.P., W.L. and J.H. curated the data and performed the formal analysis. All authors interpreted the data and H.P. wrote the original draft of the manuscript. All authors reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
HP received grant funding from Bristol-Myers Squibb/Pfizer Alliance American Thrombosis Investigator Initiated Research Program (ARISTA-USA). WL received research funding from Merck & Co. DRN received research grant support from AbbVie, Bristol-Myers Squibb, Gilead, Janssen, and Merck & Co; and owns stock in Target Pharma Solutions. All other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, H., Lo-Ciganic, WH., Huang, J. et al. Evaluation of machine learning algorithms for predicting direct-acting antiviral treatment failure among patients with chronic hepatitis C infection. Sci Rep 12, 18094 (2022). https://doi.org/10.1038/s41598-022-22819-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22819-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.